Key Points
Question
Is electroacupuncture involving the lumbosacral region effective in reducing urine leakage for women with stress urinary incontinence?
Findings
In this randomized clinical trial that included 504 women, the mean decrease in urine leakage, measured by the 1-hour pad test from baseline to week 6, was 9.9 g with electroacupuncture vs 2.6 g with sham electroacupuncture, a significant difference.
Meaning
Among women with stress urinary incontinence, treatment with electroacupuncture involving the lumbosacral region, compared with sham electroacupuncture, resulted in less urine leakage after 6 weeks.
Abstract
Importance
Electroacupuncture involving the lumbosacral region may be effective for women with stress urinary incontinence (SUI), but evidence is limited.
Objective
To assess the effect of electroacupuncture vs sham electroacupuncture for women with SUI.
Design, Setting, and Participants
Multicenter, randomized clinical trial conducted at 12 hospitals in China and enrolling 504 women with SUI between October 2013 and May 2015, with data collection completed in December 2015.
Interventions
Participants were randomly assigned (1:1) to receive 18 sessions (over 6 weeks) of electroacupuncture involving the lumbosacral region (n = 252) or sham electroacupuncture (n = 252) with no skin penetration on sham acupoints.
Main Outcomes and Measures
The primary outcome was change from baseline to week 6 in the amount of urine leakage, measured by the 1-hour pad test. Secondary outcomes included mean 72-hour urinary incontinence episodes measured by a 72-hour bladder diary (72-hour incontinence episodes).
Results
Among the 504 randomized participants (mean [SD] age, 55.3 [8.4] years), 482 completed the study. Mean urine leakage at baseline was 18.4 g for the electroacupuncture group and 19.1 g for the sham electroacupuncture group. Mean 72-hour incontinence episodes were 7.9 for the electroacupuncture group and 7.7 for the sham electroacupuncture group. At week 6, the electroacupuncture group had greater decrease in mean urine leakage (−9.9 g) than the sham electroacupuncture group (−2.6 g) with a mean difference of 7.4 g (95% CI, 4.8 to 10.0; P < .001). During some time periods, the change in the mean 72-hour incontinence episodes from baseline was greater with electroacupuncture than sham electroacupuncture with between-group differences of 1.0 episode in weeks 1 to 6 (95% CI, 0.2-1.7; P = .01), 2.0 episodes in weeks 15 to 18 (95% CI, 1.3-2.7; P < .001), and 2.1 episodes in weeks 27 to 30 (95% CI, 1.3-2.8; P < .001). The incidence of treatment-related adverse events was 1.6% in the electroacupuncture group and 2.0% in the sham electroacupuncture group, and all events were classified as mild.
Conclusions and Relevance
Among women with stress urinary incontinence, treatment with electroacupuncture involving the lumbosacral region, compared with sham electroacupuncture, resulted in less urine leakage after 6 weeks. Further research is needed to understand long-term efficacy and the mechanism of action of this intervention.
Trial Registration
clinicaltrials.gov Identifier: NCT01784172.
This randomized clinical trial compares the effects of electroacupuncture vs sham electroacupuncture on urinary leakage among women with stress urinary incontinence.
Introduction
Stress urinary incontinence (SUI) is defined by the International Continence Society as an involuntary loss of urine on physical exertion, sneezing, or coughing. The prevalence of stress urinary incontinence is as high as 49% and varies according to the population studied and the definition of stress urinary incontinence. SUI causes psychological burden, affects relationships, lowers physical productivity, and decreases quality of life in women. Yet, few effective therapies are available for treating SUI.
Acupuncture may be an effective treatment option for SUI. Electroacupuncture has been found to decrease urine leakage. However, effects of acupuncture on SUI remain uncertain because of the small sample size, poor study design, and high risks of bias in previous clinical trials.
The main objective of this study was to assess the effect of electroacupuncture involving the lumbosacral region, compared with sham electroacupuncture, in reducing urine leakage in women with SUI.
Methods
Study Design
This multicenter, randomized, participant-blinded, sham electroacupuncture–controlled clinical study was conducted at 12 hospitals in China. The institutional review board at each site approved the study protocol (Supplement 1). Written informed consent was obtained from all participants.
Participants
Women with SUI were recruited from hospitals and communities via poster and newspaper advertisements. Participants were eligible if they were 40 to 75 years old; reported involuntary urine leakage on effort, exertion, sneezing or coughing (that ceased when the stress ended); and had incontinence pad weight gain greater than 1 g in the 1-hour pad test. The main exclusion criteria were urge, mixed, or other types of urinary incontinence (Supplement 1). Participants were not compensated for study participation. Participants' self-reported ethnicity information was routinely collected without ethnic discrimination.
Randomization and Masking
Eligible participants were randomly assigned to receive either electroacupuncture or sham electroacupuncture via a central randomization system for clinical research using a 1:1 ratio. Randomization was stratified by enrollment site in a block size of 6. The participants, outcome assessors, and statisticians were blinded to treatment allocation.
To help maximize blinding of participants, a pragmatic placebo needle was used (similar to the Streitberger design) and sham electroacupuncture design was used. In this trial, adhesive pads were used in both groups; thus, the blunt-tipped placebo needle provided participant-blinding effects with a similar appearance to conventional needles but no skin penetration. The sham electroacupuncture design included a connecting cord with a broken inner wire with no actual current output. To test the participant-blinding effects, 2 hospitals were randomly selected from the study sites. All participants from the 2 selected hospitals were asked to guess whether they had received electroacupuncture or sham electroacupuncture within 5 minutes after one of the treatment sessions in weeks 3 and 6.
Interventions
Hwato brand disposable acupuncture needles (size 0.30 × 75 mm), pragmatic placebo needles (size 0.30 × 25 mm), and SDZ-V electroacupuncture apparatuses were used.
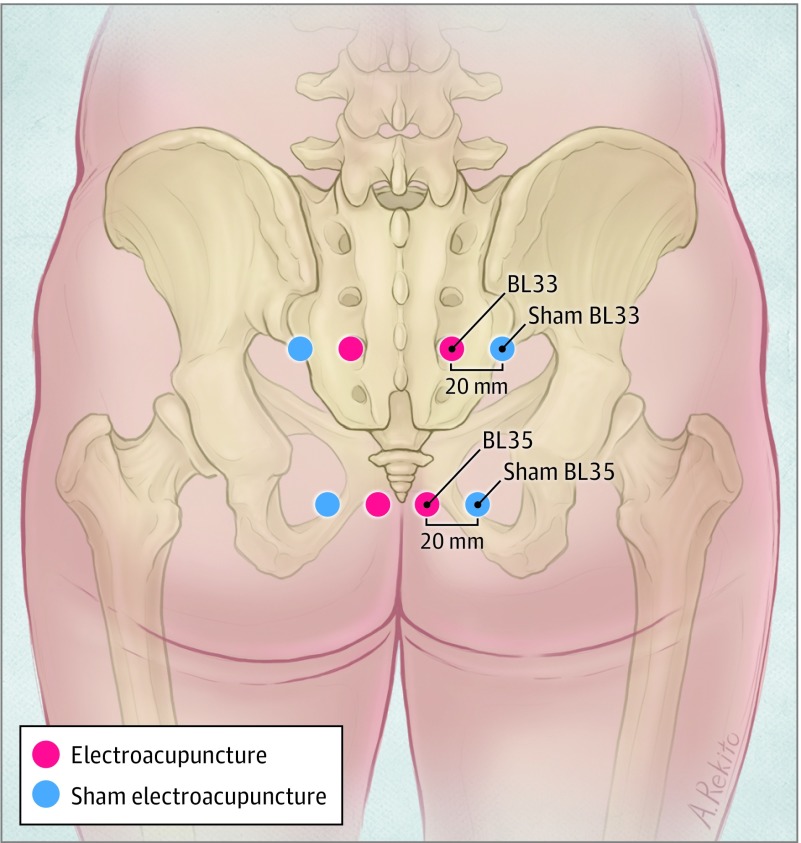
Participants in the electroacupuncture group received acupuncture at bilateral Zhongliao (BL33, located in the third sacral foramen) and Huiyang (BL35, located 0.5 cun [≈10 mm] lateral to the extremity of the coccyx) (Figure 1). After skin disinfection, sterile adhesive pads were placed on bilateral BL33 and BL35, and acupuncture needles were inserted through the adhesive pads approximately 50 to 60 mm into the skin. Needle insertion followed an angle of 30° to 45° in an inferomedial direction for BL33 and a slightly superolateral direction for BL35. Following needle insertion, small, equal manipulations of twirling, lifting, and thrusting were performed on all needles to reach de qi (a composite of sensations including soreness, numbness, distention, heaviness, and other sensations), which is believed to be an essential component for acupuncture efficacy. Paired electrodes from the electroacupuncture apparatus were attached transversely to the needle handles at bilateral BL33 and BL35. The electroacupuncture stimulation lasted for 30 minutes with a continuous wave of 50 Hz and a current intensity of 1 to 5 mA (preferably with the skin around the acupoints shivering mildly without pain). Participants received 3 treatment sessions per week (ideally every other day) for 6 consecutive weeks, 18 sessions in total.
Figure 1. Location of Acupoints for the Electroacupuncture and Sham Electroacupuncture Groups.
Participants in the sham electroacupuncture group received sham electroacupuncture with a pragmatic placebo needle on sham acupoints. The sham BL33 point was 1 cun (≈20 mm) lateral to BL 33 and the sham BL35 point was 1 cun (≈20 mm) horizontal to BL 35 (Figure 1). Procedures, electrode placements, and other treatment settings were the same as in the electroacupuncture group but with no skin penetration, electricity output, or needle manipulation for de qi.
Throughout the trial, the participants were treated separately to prevent communication and were discouraged from receiving any antiincontinence treatments, and participants receiving such treatments were asked to document them.
Outcomes
The primary outcome was the change from baseline in the amount of urine leakage measured by the 1-hour pad test at week 6. A preplanned subgroup analysis according to the SUI severity per baseline amount of urine leakage (mild, 1.1-9.9 g; moderate, 10-49.9 g; severe, ≥50 g) was performed for the primary outcome. The 1-hour pad test was performed according to the International Continence Society instructions at baseline and at weeks 2 and 6 (eAppendix 1 in Supplement 2). In brief, participants wore a preweighed pad, drank 500 mL water in 15 minutes, and then performed various strenuous activities including going up and down stairs, coughing, running, and others. Afterwards, the pad was reweighed to measure the amount of urinary leakage.
Although no clinically meaningful difference has been established, the 1-hour pad test is the only pad test with a standardized procedure for urinary incontinence. With a specificity of 65% to 89%, the 1-hour pad test has a high adherence rate. Its results demonstrated a positive relationship with urine leakage symptoms and significantly correlated with the quality-of-life questionnaire scores. Nonetheless, conflicting results exist in the literature regarding the reproducibility of both 1-hour and 24-hour pad tests. Considering the wide variation of repeated 1-hour pad tests (mean, 10 g [range, −44 to 66 g), the reproducibility of the 1-hour pad test may not be as good as the 24-hour test, which has a repeatability of 0.72 (Lin concordance correlation coefficient).
Secondary outcomes included the change from baseline in the amount of urine leakage at week 2; the mean 72-hour urinary incontinence episodes measured by a 72-hour bladder diary (72-hour incontinence episodes) during weeks 1 to 6, 15 to 18, and 27 to 30; the proportion of participants with at least 50% decrease from baseline in the amount of urine leakage measured by pad at week 6 and in the mean 72-hour incontinence episodes during weeks 1 to 6, 15 to 18, and 27 to 30; the participant-reported severity of SUI (mild, leaking several drops; moderate, soaking the underwear; severe, soaking the outerwear) during weeks 1 to 6, 15 to 18, and 27 to 30; the change from baseline in the validated Chinese version International Consultation on Incontinence Questionnaire-Short Form scores (range, 0 [best]-21 [worst] outcomes, and 2.52 as minimal clinically important differences); and the participants’ self-evaluation of therapeutic effects (no help, little help, medium help, great help) at weeks 6, 18, and 30; the number of urine pads used; and use of other treatments for SUI during weeks 1 to 6, 7 to 18, and 19 to 30.
Data for the 72-hour incontinence episodes and participant-reported SUI severity were extracted from a 3-day bladder diary completed by participants at baseline and at weeks 2, 4, 6, 15 to 18, and 27 to 30. In the diary, participants documented urinary incontinence episodes and activities at the time of occurrence, fluid intake, and the severity of incontinence over 3 consecutive days. For weeks 1 to 6, 15 to 18, and 27 to 30, the mean72-hour incontinence episode values were calculated as the weekly average, and the worst participant-reported degree of urine incontinence was used as the severity of SUI. The International Consultation on Incontinence Questionnaire-Short Form assesses the influence of urinary incontinence on quality of life during the previous 4 weeks. It measures frequency and amount of leakage, overall effects on quality of life, and the type of incontinence.
Adverse events were documented throughout the trial. Based on their potential association with the acupuncture needling procedure, adverse events were categorized by acupuncturists and related specialists as treatment-related or non–treatment-related within 24 hours of occurrence.
Statistical Analysis
Based on the results of a previous electroacupuncture study, a sample size of 144 participants per group was estimated to provide 90% power to detect a between-group difference of 1 g of urine leakage measured by the 1-hour pad test, assuming a standard deviation of 2.61 and a 2-sided significance level of 5%. To compensate for a 20% loss to follow-up and the prespecified subgroup analysis, the sample size was increased to 250 participants in each group.
The primary outcome was analyzed according to the intention-to-treat principle. The change from baseline in the amount of urine leakage at week 6 was analyzed by fitting a mixed-effect model using baseline value as a covariate, treatment as a fixed effect, and site and interaction between site and treatment as random effects accounting for center differences.
The same approach was used for the change from baseline in the amount of urine leakage at week 2. The changes from baseline in mean 72-hour incontinence episodes and International Consultation on Incontinence Questionnaire-Short Form scores were analyzed using a mixed-effect model with repeated-measures approach using baseline as a covariate; treatment, visit, and treatment × visit interaction as a fixed effect; and site and interaction between site and treatment as random effects. The analyses of participants with at least 50% reduction from baseline in the amount of urine leakage and mean 72-hour incontinence episodes were performed using a generalized linear model. For other continuous variables, comparisons between treatment groups were assessed using the t test or Wilcoxon rank-sum test as appropriate. Categorical variables were compared using the Fisher exact test or Wilcoxon rank-sum test as appropriate. Kappa analysis was used to determine whether participants correctly guessed their group assignment at a higher rate than would be expected by chance.
Missing data on the primary outcome were imputed using the multiple imputation method under the missing-at-random assumption (eAppendix 2 and eTable 1 in Supplement 2). Four sensitivity analyses were conducted for the primary outcome. The preplanned analysis used a control-based pattern model to evaluate sensitivity to missing data departure from the assumption, and 3 posthoc analyses evaluated whether the analyses could have diluted the estimates of treatment effect (eAppendix 3 in Supplement 2). The posthoc subgroup analysis was conducted by adding an interaction between the baseline amount of urine leakage and treatment into the mixed-effect model.
All statistical analyses were performed using SAS version 9.4 (SAS Institute Inc) with a 2-sided P value of less than .05 considered significant. No adjustment was made for multiple comparisons; therefore, secondary outcomes should be interpreted as exploratory.
Results
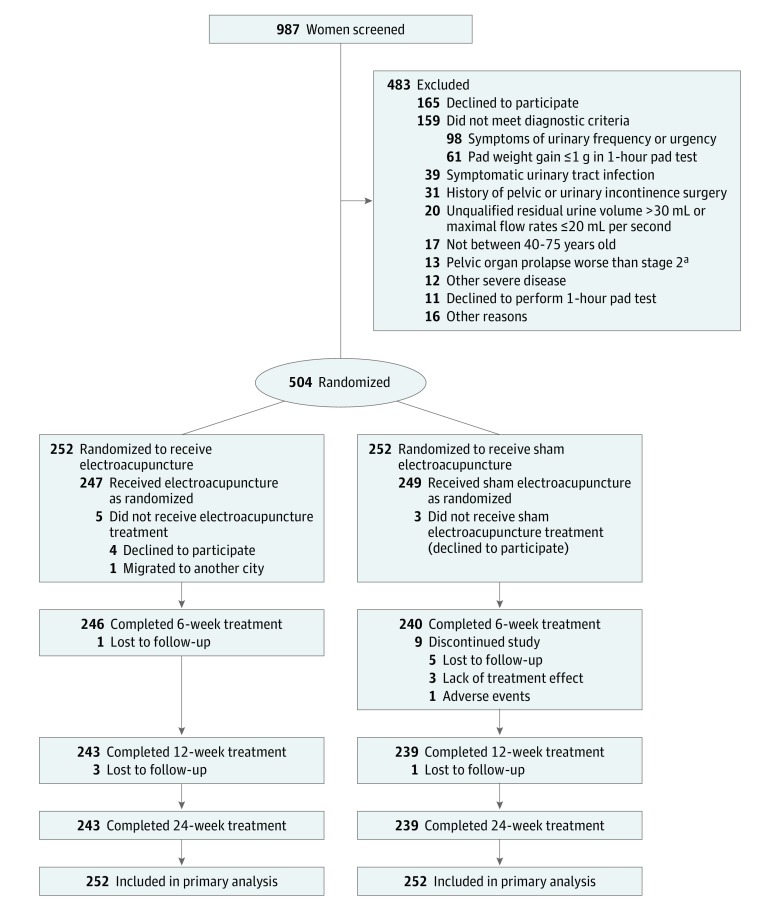
Between October 8, 2013, and May 15, 2015, we screened 987 participants for eligibility, of whom 504 (mean [SD] age, 55.3 [8.4] years) were randomly assigned to receive either electroacupuncture (n = 252) or sham electroacupuncture (n = 252). Among the randomized participants, 482 (95.6%) completed the study (Figure 2). Multiple imputation was used for the missing data in 18 participants (6 in the electroacupuncture group and 12 in the sham electroacupuncture group). Baseline characteristics were similar between groups except for age (Table 1).
Figure 2. Flow of Participants Randomized to Receive Electroacupuncture or Sham Electroacupuncture.
aStages of pelvic organ prolapse range from 0 (no prolapse, apex can descend within 2 cm of hymen) to 4 (complete eversion, leading edge >2 cm of total vaginal length).
Table 1. Participant Baseline Characteristicsa.
| Characteristics | Electroacupuncture (n = 252) |
Sham Electroacupuncture (n = 252) |
|---|---|---|
| Age, mean (SD), yb | 54.5 (8.3) | 56.2 (8.4) |
| Race | ||
| Han | 242 (96.0) | 247 (98.4) |
| Minorities | 10 (4.0) | 4 (1.6) |
| Educational level | ||
| Primary education or less | 91 (36.1) | 91 (36.1) |
| Secondary education | 148 (58.7) | 142 (56.3) |
| Tertiary education | 13 (5.2) | 19 (7.5) |
| Manner of child deliveryc | ||
| Vaginal delivery | 231 (91.7) | 228 (91.6) |
| Cesarean section | 19 (7.5) | 19 (7.6) |
| Both | 2 (0.8) | 2 (0.8) |
| Menopause | 169 (67.1) | 180 (71.4) |
| BMI, mean (SD)d | 23.9 (2.8) | 23.8 (2.6) |
| SUI duration, median (IQR), mo | 60 (31.5-117.5) | 62.5 (36-120) |
| Comorbidities | ||
| Cardiovascular and cerebrovascular diseases | 11 (4.4) | 17 (6.7) |
| Osteoarthritis | 9 (3.6) | 4 (1.6) |
| Respiratory diseases | 5 (2.0) | 7 (2.8) |
| Metabolic disorders | 0 | 3 (1.2) |
| Other | 11 (4.4) | 7 (2.8) |
| Severity of SUIe | ||
| Mild, 1.1-9.9 g | 129 (51.2) | 132 (52.4) |
| Moderate, 10-49.9 g | 99 (39.3) | 96 (38.1) |
| Severe, ≥50 g | 24 (9.5) | 24 (9.5) |
| Amount of urine leakage measured by the 1-h pad test, g | ||
| Mean (SD) | 18.4 (23.6) | 19.1 (28.5) |
| Median (IQR) | 9.8 (3.1-22.6) | 9.3 (3.0-20.9) |
| 72-h Incontinence episodesf | ||
| Mean (SD) | 7.9 (9.1) | 7.7 (7.3) |
| Median (IQR) | 5.0 (2.0-10.0) | 5.0 (3.0-10.0) |
| ICIQ-SF score, mean (SD)g | 9.9 (3.3) | 9.8 (3.2) |
| Severity of SUIh | ||
| None | 7 (2.8) | 3 (1.2) |
| Mild | 116 (46.0) | 127 (50.6) |
| Moderate | 103 (40.9) | 104 (41.4) |
| Severe | 26 (10.3) | 17 (6.8) |
| 24-h Volume of liquid intake, median (IQR), mL | 1092 (800-1460) | 1017 (700-1500) |
| Participants using urine pads | 119 (47.4) | 107 (43.2) |
| Weekly mean No. of urine pads used (1 wk before treatment), median (IQR)i | 7.0 (3.0-9.0) | 6.0 (3.0-9.0) |
| Previous treatments for SUI within 2 wkj | 14 (5.6) | 15 (6.0) |
Abbreviations: BMI, body mass index; ICIQ-SF, International Consultation on Incontinence Questionnaire-Short Form; IQR, interquartile range; SUI, stress urinary incontinence.
Values are reported as No. (%) unless otherwise indicated.
Three participants, aged 39 years, were included by mistake.
Three participants in the sham electroacupuncture group had no history of childbirth.
Calculated as weight in kilograms divided by height in meters squared.
Severity of SUI (objectively based) was rated by the amount of urine leakage measured by the 1-h pad test (minimal/continent, ≤1 g).
One participant in the sham electroacupuncture group had no baseline record of 72-h incontinence episodes.
Scoring of the ICIQ-SF was additive (0 [better]-21 [worse] outcomes).
Severity of stress urinary incontinence (subjectively based) was rated by participants in the 72-hour bladder diary (none; mild, leaking several drops; moderate, soaking the underwear; severe, soaking the outerwear).
The weekly consumption of urine pads was assessed in participants who used urine pads.
Previous treatment for stress urinary incontinence mainly included pelvic floor muscle training (electroacupuncture group, n = 7; sham electroacupuncture group, n = 3), medicine and acupuncture (electroacupuncture group, n = 7; sham electroacupuncture group, n = 10),lifestyle intervention (sham electroacupuncture group, n = 2).
For the primary outcome, the mean amount of urine leakage measured by the 1-hour pad test was 18.4 g (95% CI, 15.5-21.4 g) at baseline and 8.2 g (95% CI, 6.3-10.0 g) at week 6 in the electroacupuncture group, and 19.1 g (95% CI, 15.6-22.7 g) at baseline and 16.8 g (95% CI, 13.5-20.1 g) at week 6 in the sham electroacupuncture group. The reduction in the amount of urine leakage at week 6 was greater in the electroacupuncture group (mean, −9.9) than in the sham electroacupuncture group (−2.6 g) with a mean difference of 7.4 g (95% CI, 4.8-10.0 g; P < .001). Similar results were observed at week 2 (Table 2), in the sensitivity analyses (eTables 2-5 in Supplement 2), and across subgroups except for the subgroup with mild SUI symptoms (eFigure 1 in Supplement 2). A higher proportion of participants in the electroacupuncture group compared with the sham electroacupuncture group had a decrease of at least 50% in the amount of urine leakage at week 6 (between-group difference, 43.0% [95% CI, 35.0%-50.9%]; P < .001) (Table 2).
Table 2. Primary and Secondary Outcomes.
| Variable | Electroacupuncture (n = 252) |
Sham Electroacupuncture (n = 252) |
Difference (95% CI) |
P Valuea |
|---|---|---|---|---|
| Primary Outcome | ||||
| Urine leakage at wk 6, mean (95% CI), gb,c | 8.2 (6.3 to 10.0) | 16.8 (13.5 to 20.1) | ||
| Change at wk 6, adjusted mean (95% CI)d | −9.9 (−12.5 to −7.3) | −2.6 (−5.2 to 0) | 7.4 (4.8 to 10.0) | <.001 |
| Secondary Outcomese | ||||
| Change in mean No. of 72-h incontinence episodes, adjusted mean (95% CI), wkf | ||||
| 1-6 | −2.9 (−3.6 to −2.2) | −2.0 (−2.7 to −1.2) | 1.0 (0.2 to 1.7) | .01 |
| 15-18 | −4.7 (−5.4 to −4.0) | −2.7 (−3.4 to −2.0) | 2.0 (1.3 to 2.7) | <.001 |
| 27-30 | −5.0 (−5.8 to −4.3) | −3.0 (−3.7 to −2.2) | 2.1 (1.3 to 2.8) | <.001 |
| Change at wk 2, urine leakage, adjusted mean (95% CI), gb | −5.8 (−8.3 to −3.2) | −2.0 (−4.6 to 0.5) | 3.7 (1.5 to 6.0) | <.001g |
| Reduction ≥50% at wk 6, urine leakage from baselineb | 159/246 (64.6) | 52/240 (21.7) | −43.0 (−50.9 to −35.0) | <.001h |
| Reduction ≥50% in mean 72-h incontinence episodes from baselineh | ||||
| Weeks 1-6 | 91/239 (38.1) | 56/243 (23.1) | −15.0 (−23.2 to −6.9) | <.001 |
| Weeks 15-18 | 152/237 (64.1) | 91/236 (38.6) | −25.6 (−34.3 to −16.9) | <.001 |
| Weeks 27-30 | 160/237 (67.5) | 99/236 (42.0) | −25.6 (−34.2 to −16.9) | <.001 |
| Change, ICIQ-SF score, adjusted mean (95% CI)i | ||||
| Week 6 | −2.4 (−3.1 to −1.8) | −0.9 (−1.6 to −0.2) | 1.5 (0.7 to 2.3) | <.001 |
| Week 18 | −3.6 (−4.3 to −2.9) | −1.3 (−2.0 to −0.6) | 2.3 (1.4 to 3.2) | <.001 |
| Week 30 | −4.1 (−4.8 to −3.4) | −1.6 (−2.4 to −0.9) | 2.5 (1.5 to 3.4) | <.001 |
| Volume of liquid intake at 24 h, median (range), mLj | ||||
| Weeks 1-6 | 1077.7 (755.6 to 1400.0) | 999.4 (766.7 to 1438.9) | NA | .74 |
| Weeks 15-18 | 1025.0 (799.2 to 1360.0) | 975.0 (745.8 to 1412.5) | NA | .74 |
| Weeks 27-30 | 975.0 (775.0 to 1316.7) | 937.5 (725.0 to 1370.8) | NA | .47 |
| Participants using urine padsh | ||||
| Weeks 1-6 | 115/245 (46.9) | 111/245 (45.3) | −1.6 (−10.5 to 7.2) | .72 |
| Weeks 7-18 | 72/242 (29.8) | 89/237 (37.6) | 7.8 (−0.6 to 16.2) | .07 |
| Weeks 19-30 | 75/242 (31.0) | 93/237 (39.2) | 8.3 (−0.3 to 16.8) | .06 |
| Weekly mean use of urine pads, median (IQR)k | ||||
| Weeks 1-6 | 3.0 (1.7 to 6.0) | 3.7 (1.7 to 7.0) | NA | .12 |
| Weeks 7-18 | 3.1 (1.5 to 5.9) | 3.3 (1.3 to 7.0) | NA | .75 |
| Weeks 19-30 | 3.0 (1.0 to 6.0) | 3.8 (2.0 to 7.0) | NA | .02 |
| Use of other treatment for stress urinary incontinence | ||||
| Weeks 1-6l | 1/245 (0.4) | 0 | NA | >.99 |
| Weeks 7-18l | 1/242 (0.4) | 0 | NA | >.99 |
| Weeks 19-30 | 0 | 0 | NA | NA |
Abbreviations: ICIQ-SF, International Consultation on Incontinence Questionnaire-Short Form; IQR, interquartile range; NA, not applicable.
All tests were 2-sided. P value of less than .05 was considered significant.
Measured using the 1-hour pad test.
Number of participants: 240, sham electroacupuncture group and 246, electroacupuncture group.
Number of participants with imputed data: 12 (4.8%), sham electroacupuncture group and 6 (2.4%), electroacupuncture group (from mixed-effects model–adjusted baseline values).
Missing data not imputed for secondary outcomes analyses.
Number of participants: 243, electroacupuncture group and 239, sham electroacupuncture group (from repeated-measures mixed-effects model–adjusted baseline values).
Calculated using a mixed-effects model with baseline adjustment.
Calculated using a generalized linear model.
Scoring was additive (0 [better]-21 [worse] outcomes). Minimally clinically important difference: 2.52. Repeated-measures mixed-effects model–adjusted baseline values were used (243, electroacupuncture group; 239, sham electroacupuncture group).
Calculated using the Wilcoxon rank-sum test (participants [electroacupuncture group: 246, wk 1-6; 243, wk 15-18; 243, wk 27-30 and for the sham electroacupuncture group: 246, wk 1-6; 239, wk 15-18; 238, wk 27-30]).
Weekly use assessed among participants who used urine pads by the Wilcoxon rank-sum test. Between-group differences were not provided.
One participant used pelvic floor muscle training. P value was calculated using the Fisher exact test.
At baseline, there were 7.9 72-hour incontinence episodes among participants in the electroacupuncture group and 7.7 in the sham electroacupuncture group. Change in mean number of 72-hour incontinence episodes from baseline was greater in the electroacupuncture group than the sham electroacupuncture group with between-group differences of 1.0 episode (95% CI, 0.2-1.7 episodes; P = .01) during weeks 1 to 6, 2.0 episodes (95% CI, 1.3-2.7 episodes; P < .001) during weeks 15 to 18, and 2.1 episodes (95% CI, 1.3-2.8 episodes; P < .001) during weeks 27 to 30. A higher proportion of participants in the electroacupuncture group compared with the sham electroacupuncture group showed at least 50% reduction in mean number of 72-hour incontinence episodes with between-group differences of 15.0% (95% CI, 6.9% to 23.2%; P < .001) during weeks 1-6, 25.6% (95% CI, 16.9% to 34.3%; P < .001) during weeks 15 to 18, and 25.6% (95% CI, 16.9% to 34.2%; P < .001) during weeks 27 to 30.
Compared with the sham electroacupuncture group, the electroacupuncture group had a greater decrease from baseline in the total International Consultation on Incontinence Questionnaire-Short Form score with between-group differences of 1.5 points (95% CI, 0.7-2.3 points; P < .001) at week 6, 2.3 points (95% CI, 1.4-3.2 points; P < .001) at week 18, and 2.5 points (95% CI, 1.5-3.4 points; P < .001) at week 30 (Table 2). The electroacupuncture group had higher improvement in participant-reported SUI severity and better self-evaluation of therapeutic effects (Table 3). No differences were found between the 2 groups in weekly mean number of urine pads used (except weeks 19-30), the number of participants using urine pads, or other treatments (Table 2).
Table 3. Participant-Reported Symptom Severity and Participant Self-Evaluation of Therapeutic Effectsa.
| Week 6 | Week 18 | Weeks 30 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Electro- acupuncture (n = 252) |
Sham Electro- acupuncture (n = 252) |
P Valueb | Electro- acupuncture (n = 252) |
Sham Electro- acupuncture (n = 252) |
P Valueb | Electro- acupuncture (n = 252) |
Sham Electro- acupuncture (n = 252) |
P Valueb | |
| Severity of Stress Urinary Incontinencec | |||||||||
| None | 13 (5.3) | 6 (2.4) | .03 | 40 (16.5) | 17 (7.1) | <.001 | 51 (21.1) | 24 (10.0) | <.001 |
| Mild | 138 (56.1) | 121 (49.2) | 166 (68.6) | 134 (56.1) | 147 (60.7) | 140 (58.6) | |||
| Medium | 88 (35.8) | 102 (41.5) | 30 (12.4) | 75 (31.4) | 39 (16.1) | 66 (27.6) | |||
| Severe | 7 (2.8) | 17 (6.9) | 6 (2.5) | 13 (5.4) | 5 (2.1) | 9 (3.8) | |||
| Missing | 6 | 6 | 10 | 13 | 10 | 13 | |||
| Participant Self-evaluation of Therapeutic Effects | |||||||||
| No help | 2 (0.8) | 75 (30.5) | <.001 | 8 (3.3) | 76 (31.8) | <.001 | 15 (6.2) | 82 (34.3) | <.001 |
| Little help | 34 (13.8) | 96 (39.0) | 50 (20.6) | 97 (40.6) | 45 (18.5) | 89 (37.2) | |||
| Medium help | 119 (48.4) | 47 (19.1) | 104 (42.8) | 35 (14.6) | 95 (39.1) | 40 (16.7) | |||
| Great help | 91 (37.0) | 28 (11.4) | 81 (33.3) | 31 (13.0) | 88 (36.2) | 28 (11.7) | |||
| Missing | 6 | 6 | 9 | 13 | 9 | 13 | |||
There were 252 participants for each group and time period.
Calculated using the Wilcoxon rank-sum test.
Rated using the 72-hour bladder diary by participants ( mild, leaking several drops; moderate, soaking the underwear; severe, soaking the outerwear). The worst degree of urine incontinence during weeks 1 to 6, 15 to 18 and 27 to 30 was used as the severity of stress urinary incontinence for each corresponding time period.
Treatment-related adverse events, including hematoma and fatigue occurred among 1.6% of participants in the electroacupuncture group and 2.0% in the sham electroacupuncture group (Table 4). Non–treatment-related adverse events occurred infrequently (eTable 6 in Supplement 2).
Table 4. Adverse Events Related to Treatmenta.
| Adverse Event | Participant, No. (%) | |
|---|---|---|
| Electroacupuncture (n = 247)b |
Sham Electroacupuncture (n = 249)b |
|
| Overall | 4 (1.6) | 5 (2.0) |
| Severe adverse events | 0 | 0 |
| Subcutaneous hematoma | 0 | 4 (1.6) |
| Fatigue | 2 (0.8) | 1 (0.4) |
| Sharp pain | 1 (0.4) | 0 |
| Palpitation | 1 (0.4) | 0 |
Adverse events were analyzed in all participants who received treatment. Adverse events were counted by type rather than frequency in the same participant. Adverse events with different types occurring in a single participant were defined as independent adverse events. An adverse event with multiple occurrences in a single participant was defined as 1 adverse event.
Five participants in the electroacupuncture group and 3 in the sham electroacupuncture group did not receive treatment.
At week 3, 31 of 41 participants in the electroacupuncture group vs 29/42 participants in sham electroacupuncture group guessed their treatment to be electroacupuncture (κ coefficient = 0.07, 95% CI, (−0.13 to 0.26); P = .63); at week 6, the numbers were 32/42 participants in the electroacupuncture group vs 25/39 participants in sham electroacupuncture group (kappa coefficient = 0.14, 95% CI, (−0.06 to 0.34); P = .22) (eTable 7 in Supplement 2).
Discussion
Over a 6-week treatment period, electroacupuncture involving the lumbosacral region showed a greater reduction in the amount of urine leakage than sham electroacupuncture. The effects persisted 24 weeks after treatment. The incidence of adverse events was low.
Objective and quantitative assessments of urinary incontinence provide direct evidence for the therapeutic assessment of an intervention. Similar to a previous electroacupuncture study, electroacupuncture involving the lumbosacral region decreased the amount of urine leakage measured by the 1-hour pad test. In this study, the decrease in the amount of urine leakage in the electroacupuncture group was 9.9 g after treatment, while previous trials reported a decrease of 5.1 g after 8 weeks of pelvic floor muscle training and 8.9 g after 12 weeks of pelvic floor muscle training. A 50% or more decrease in the amount of urine leakage was considered to be a clinical improvement. In this study, 64.6% of participants in the electroacupuncture group had a decrease of at least 50% in the amount of urine leakage after treatment. Thus, results of this study demonstrated that electroacupuncture had a clinically meaningful benefit in decreasing urine leakage in women with SUI.
Urinary incontinence frequency during daily life is another important assessment for SUI. In this trial, the decreases in the 72-hour incontinence episodes in the electroacupuncture group were consistent with the previous findings of electroacupuncture treatment and were similar to the effects of pelvic floor muscle training and duloxetine. The proportion of participants with at least a 50% reduction in the mean 72-hour incontinence episodes (clinically meaningful) in the electroacupuncture group was 67.5% during weeks 27 to 30 and is similar to 69.8% after pelvic floor muscle training.
In this trial, 85.4% of participants reported at least medium help from electroacupuncture at week 6; this was similar to the participants’ satisfaction rate (84.8%) with pelvic floor muscle training. The decreases from baseline in the International Consultation on Incontinence Questionnaire-Short Form score following electroacupuncture at week 18 and week 30 were clinically significant and comparable to a pelvic floor muscle training regimen.
The mechanisms of acupuncture for SUI remain unclear. Intrinsic urethral sphincter deficiency and urethral hypermobility caused by weak pelvic floor muscles have been proposed as the main pathophysiologies. Pelvic floor electric stimulation could increase the maximum urethral closure pressure. Electroacupuncture involving the lumbosacral region could cause muscle contraction and simulate pelvic floor muscle training. Both techniques were found effective in treating SUI. Results of this trial are consistent with these previous findings. Additionally, denervation of the pelvic floor has also been linked with SUI. Electroacupuncture may stimulate S3 via BL33 and the pudendal nerve via BL35 at the lumbosacral region. Thus, electroacupuncture may facilitate the reinnervation and strengthening of pelvic floor muscles, improving symptoms of SUI. These potential relationships may also account for the delayed effects of electroacupuncture after treatment in this study.
This study has some limitations. First, no clinically meaningful difference was defined for the 1-hour pad test. Second, the amount of urine leakage was not assessed during the 24-week follow-up. Third, the participant blinding assessment was only performed in 2 of the 12 centers. Fourth, the use of fixed block randomization could not prevent bias from the prediction of treatment allocation in participants. Fifth, no adjustment was made for multiple comparisons for secondary outcomes. Sixth, the 18 sessions of electroacupuncture treatment over 6 weeks may be burdensome. Seventh, electroacupuncture procedures in the study can be technically challenging.
Conclusions
Among women with stress urinary incontinence, treatment with electroacupuncture involving the lumbosacral region compared with sham electroacupuncture resulted in less urine leakage after 6 weeks. Further research is needed to understand long term efficacy and the mechanism of action of this intervention.
Trial Protocol
eAppendix 1. Procedure for 1-Hour Pad Test According to International Continence Society Instructions
eAppendix 2. Multiple Imputation
eTable 1. Missing Data Patterns
eAppendix 3. Details for Results of Primary Analysis
eTable 2. Different Analysis Model Accounting for Center Effects
eTable 3. Multiple Imputation Under Departures From the Missing at Random Assumption
eTable 4. Estimated Values With Age Adjustment for Change in Amount of Urine Leakage Measured by the 1-Hour Pad Test
eTable 5. Estimated Values With Using Mixed-Effect Model With Repeated Measures
eTable 6. Adverse Events Unrelated to Treatment
eTable 7. Participant-Binding Assessment Results
eFigure. A Forest Plot of Subgroup Analysis per Stress Urinary Incontinence Severity at Baseline
eReferences.
References
- 1.Abrams P, Cardozo L, Fall M, et al. ; Standardisation Sub-Committee of the International Continence Society . The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology. 2003;61(1):37-49. [DOI] [PubMed] [Google Scholar]
- 2.Kobashi KC, Albo ME, Dmochowski RR, et al. Surgical Treatment of Female Stress Urinary Incontinence (SUI): AUA/SUFU Guideline. 2017. http://www.auanet.org/guidelines/stress-urinary-incontinence-(sui)-new-(aua/sufu-guideline-2017). Accessed May 20, 2017.
- 3.Sinclair AJ, Ramsay IN. The psychosocial impact of urinary incontinence in women. The Obstetrician & Gynaecologist. 2011;13(3):143-148. doi: 10.1576/toag.13.3.143.27665 [DOI] [Google Scholar]
- 4.Mo Q, Ma X, Liu Z. Curative effect observation on the treatment of female stress urinary incontinence with electro-acupuncture [Article in Chinese]. Beijing Journal of Traditional Chinese Medicine. 2013;32(6):434-436. [Google Scholar]
- 5.Wang Y, Zhishun L, Peng W, Zhao J, Liu B. Acupuncture for stress urinary incontinence in adults. Cochrane Database Syst Rev. 2013;7(7):CD009408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liu Z, Xu H, Chen Y, et al. The efficacy and safety of electroacupuncture for women with pure stress urinary incontinence: study protocol for a multicenter randomized controlled trial. Trials. 2013;14:315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abrams P, Khoury S, Cardozo L, Wein A. Incontinence, 5th International Consultation on Incontinence, Paris February, 2012. Arnhem, Netherlands: ICUD-EAU; 2013. [Google Scholar]
- 8.Streitberger K, Kleinhenz J. Introducing a placebo needle into acupuncture research. Lancet. 1998;352(9125):364-365. [DOI] [PubMed] [Google Scholar]
- 9.Liu B, Xu H, Ma R, Mo Q, Yan S, Liu Z. Effect of blinding with a new pragmatic placebo needle: a randomized controlled crossover study. Medicine (Baltimore). 2014;93(27):e200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhou K, Fang J, Wang X, et al. Characterization of de qi with electroacupuncture at acupoints with different properties. J Altern Complement Med. 2011;17(11):1007-1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smither AR, Guralnick ML, Davis NB, See WA. Quantifying the natural history of post-radical prostatectomy incontinence using objective pad test data. BMC Urol. 2007;7:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abrams P, Blaivas JG, Stanton SL, Andersen JT; The International Continence Society Committee on Standardisation of Terminology . The standardisation of terminology of lower urinary tract function. Scand J Urol Nephrol Suppl. 1988;114:5-19. [PubMed] [Google Scholar]
- 13.Krhut J, Zachoval R, Smith PP, et al. Pad weight testing in the evaluation of urinary incontinence. Neurourol Urodyn. 2014;33(5):507-510. [DOI] [PubMed] [Google Scholar]
- 14.Costantini E, Lazzeri M, Bini V, Giannantoni A, Mearini L, Porena M. Sensitivity and specificity of one-hour pad test as a predictive value for female urinary incontinence. Urol Int. 2008;81(2):153-159. [DOI] [PubMed] [Google Scholar]
- 15.Punter J, Townsend J, Dasgupta J, et al. Compliance with pad tests: 24 hour pad test compared to the 1 hour pad test. International Continence Society. https://www.ics.org/Abstracts/Publish/42/000751.pdf. Accessed May 10, 2017.
- 16.Matharu GS, Assassa RP, Williams KS, et al. Objective assessment of urinary incontinence in women: comparison of the one-hour and 24-hour pad tests. Eur Urol. 2004;45(2):208-212. [DOI] [PubMed] [Google Scholar]
- 17.Liebergall-Wischnitzer M, Paltiel O, Hochner-Celnikier D, Lavy Y, Shveiky D, Manor O. Concordance between one-hour pad test and subjective assessment of stress incontinence. Urology. 2010;76(6):1364-1368. [DOI] [PubMed] [Google Scholar]
- 18.Simons AM, Yoong WC, Buckland S, Moore KH. Inadequate repeatability of the one-hour pad test: the need for a new incontinence outcome measure. BJOG. 2001;108(3):315-319. [DOI] [PubMed] [Google Scholar]
- 19.Lose G, Rosenkilde P, Gammelgaard J, Schroeder T. Pad-weighing test performed with standardized bladder volume. Urology. 1988;32(1):78-80. [DOI] [PubMed] [Google Scholar]
- 20.Groutz A, Blaivas JG, Chaikin DC, et al. Noninvasive outcome measures of urinary incontinence and lower urinary tract symptoms: a multicenter study of micturition diary and pad tests. J Urol. 2000;164(3 pt 1):698-701. [DOI] [PubMed] [Google Scholar]
- 21.Lose G, Jørgensen L, Thunedborg P. 24-hour home pad weighing test versus 1-hour ward test in the assessment of mild stress incontinence. Acta Obstet Gynecol Scand. 1989;68(3):211-215. [DOI] [PubMed] [Google Scholar]
- 22.Karantanis E, Fynes M, Moore KH, Stanton SL. Comparison of the ICIQ-SF and 24-hour pad test with other measures for evaluating the severity of urodynamic stress incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2004;15(2):111-116. [DOI] [PubMed] [Google Scholar]
- 23.Huang L, Zhang SW, Wu SL, Ma L, Deng XH. The Chinese version of ICIQ: a useful tool in clinical practice and research on urinary incontinence. Neurourol Urodyn. 2008;27(6):522-524. [DOI] [PubMed] [Google Scholar]
- 24.Nyström E, Sjöström M, Stenlund H, Samuelsson E. ICIQ symptom and quality of life instruments measure clinically relevant improvements in women with stress urinary incontinence. Neurourol Urodyn. 2015;34(8):747-751. [DOI] [PubMed] [Google Scholar]
- 25.Xu H, Liu B, Wu J, et al. A pilot randomized placebo controlled trial of electroacupuncture for women with pure stress urinary incontinence. PLoS One. 2016;11(3):e0150821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sar D, Khorshid L. The effects of pelvic floor muscle training on stress and mixed urinary incontinence and quality of life. J Wound Ostomy Continence Nurs. 2009;36(4):429-435. [DOI] [PubMed] [Google Scholar]
- 27.Liebergall-Wischnitzer M, Hochner-Celnikier D, Lavy Y, Manor O, Shveiky D, Paltiel O. Randomized trial of circular muscle versus pelvic floor training for stress urinary incontinence in women. J Womens Health (Larchmt). 2009;18(3):377-385. [DOI] [PubMed] [Google Scholar]
- 28.Aksac B, Aki S, Karan A, Yalcin O, Isikoglu M, Eskiyurt N. Biofeedback and pelvic floor exercises for the rehabilitation of urinary stress incontinence. Gynecol Obstet Invest. 2003;56(1):23-27. [DOI] [PubMed] [Google Scholar]
- 29.Sjöström M, Umefjord G, Stenlund H, Carlbring P, Andersson G, Samuelsson E. Internet-based treatment of stress urinary incontinence: a randomised controlled study with focus on pelvic floor muscle training. BJU Int. 2013;112(3):362-372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lin AT, Sun MJ, Tai HL, et al. Duloxetine versus placebo for the treatment of women with stress predominant urinary incontinence in Taiwan: a double-blind, randomized, placebo-controlled trial. BMC Urol. 2008;8:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yalcin I, Peng G, Viktrup L, Bump RC. Reductions in stress urinary incontinence episodes: what is clinically important for women? Neurourol Urodyn. 2010;29(3):344-347. [DOI] [PubMed] [Google Scholar]
- 32.Yoshimura N, Miyazato M. Neurophysiology and therapeutic receptor targets for stress urinary incontinence. Int J Urol. 2012;19(6):524-537. [DOI] [PubMed] [Google Scholar]
- 33.Yamanishi T, Yasuda K, Sakakibara R, Hattori T, Ito H, Murakami S. Pelvic floor electrical stimulation in the treatment of stress incontinence: an investigational study and a placebo controlled double-blind trial. J Urol. 1997;158(6):2127-2131. [DOI] [PubMed] [Google Scholar]
- 34.Wang S, Zhang S. Simultaneous perineal ultrasound and vaginal pressure measurement prove the action of electrical pudendal nerve stimulation in treating female stress incontinence. BJU Int. 2012;110(9):1338-1343. [DOI] [PubMed] [Google Scholar]
- 35.Smith AR, Hosker GL, Warrell DW. The role of partial denervation of the pelvic floor in the aetiology of genitourinary prolapse and stress incontinence of urine: a neurophysiological study. Br J Obstet Gynaecol. 1989;96(1):24-28. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol
eAppendix 1. Procedure for 1-Hour Pad Test According to International Continence Society Instructions
eAppendix 2. Multiple Imputation
eTable 1. Missing Data Patterns
eAppendix 3. Details for Results of Primary Analysis
eTable 2. Different Analysis Model Accounting for Center Effects
eTable 3. Multiple Imputation Under Departures From the Missing at Random Assumption
eTable 4. Estimated Values With Age Adjustment for Change in Amount of Urine Leakage Measured by the 1-Hour Pad Test
eTable 5. Estimated Values With Using Mixed-Effect Model With Repeated Measures
eTable 6. Adverse Events Unrelated to Treatment
eTable 7. Participant-Binding Assessment Results
eFigure. A Forest Plot of Subgroup Analysis per Stress Urinary Incontinence Severity at Baseline
eReferences.