Abstract
Importance
Recent studies have observed an increase in the rate of pulmonary artery catheter (PAC) use in heart failure admissions. Little is known about the national trends in other previously common indications for PAC placement, PAC use overall, or outcomes associated with PAC placement.
Objective
To determine national trends in PAC use overall as well as across sociodemographic groups and key clinical conditions, including acute myocardial infarction, heart failure, and respiratory failure.
Design, Setting, and Participants
Centers for Medicare and Medicaid Services inpatient claims data and International Classification of Diseases, Ninth Revision, Clinical Modification codes were used to conduct a serial cross-sectional cohort study between January 1, 1999, and December 31, 2013, identifying hospitalizations during which a PAC was placed. Data analysis was conducted from September 25, 2015, to April 10, 2017.
Main Outcomes and Measures
Rate of use of a PAC per 1000 admissions, 30-day mortality, and length of stay.
Results
Among the 68 374 904 unique Medicare beneficiaries in the study, there were 469 582 hospitalizations among 457 193 patients (204 232 women and 252 961 men; mean [SD] age, 76.3 [6.9] years) during which a PAC was placed. There was a 67.8% relative decrease in PAC use (6.28 per 1000 admissions in 1999 to 2.02 per 1000 admissions in 2013; P < .001), with 2 distinct trends: significant year-on-year decreases from 1999 to 2011, followed by stable use through 2013. There was variation in rates of PAC use across race/ethnicity, age, and sex, but use decreased across all subgroups. Although there were sustained decreases in PAC use for acute myocardial infarction (20.0 PACs placed per 1000 admissions in 1999 to 5.2 in 2013 [74.0% reduction]; P < .001 for trend) and respiratory failure (29.9 PACs placed per 1000 admission in 1999 to 2.3 in 2013 [92.3% reduction]; P < .001 for trend) during the study period, there was an initial decrease in PAC use in heart failure, with a nadir in 2009 followed by a subsequent increase (9.1 PACs placed per 1000 admissions in 1999 to 4.0 in 2009 to 5.8 in 2013). In-hospital mortality, 30-day mortality, and length of stay decreased during the study period.
Conclusions and Relevance
In the wake of mounting evidence suggesting a lack of benefit to the routine use of PACs, there has been a de-adoption of PAC use overall and across sociodemographic groups but heterogeneity in patterns of use across clinical conditions. The clinical outcomes of patients with PACs have significantly improved. These findings raise important questions about the optimal use of PACs and the drivers of the observed trends.
This cohort study of Medicare beneficiaries examines national trends in pulmonary artery catheter use overall as well as across sociodemographic groups and key clinical conditions, including acute myocardial infarction, heart failure, and respiratory failure.
Key Points
Question
What are the national trends in overall use of pulmonary artery catheters (PACs) and in previously common indications for PAC placement?
Findings
In this cohort study of Medicare beneficiaries, rates of PAC use decreased 67.8% from 1999 to 2013, while the rate of PAC use in heart failure admissions decreased from 1999 to 2009, followed by a subsequent increase. Use of PACs in admissions for myocardial infarction and respiratory failure decreased during the study period.
Meaning
Overall use of PACs has decreased, and disparate trends have emerged in admissions for heart failure, respiratory failure, and myocardial infarction, raising questions about the drivers of these trends.
Introduction
The benefit of routine pulmonary artery catheterization for critically ill patients was called into question in 1996 by the Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments investigators, and subsequent prospective, randomized clinical trials failed to demonstrate clinical benefit in an array of populations. In response to these data, many professional societies updated their guidelines; the American College of Cardiology and American Heart Association (ACC/AHA) now recommend against the use of pulmonary artery catheters (PACs) in routine admissions for heart failure (HF), and the Society of Critical Care Medicine recommends against the routine use of PACs for patients with sepsis-related acute respiratory distress syndrome. The ACC/AHA HF guidelines also contain class I recommendations for PAC use “in patients who have respiratory distress or clinical evidence of impaired perfusion in whom the adequacy of or excess of intracardiac filling pressures cannot be determined from clinical assessment.”(p167)
Recent studies have shown an increase in PAC use in admissions for HF, which raise questions about the rates of use of PACs overall and in other previously common indications for PAC placement. In an effort to evaluate these trends and given that rates of PAC use have been highest in Americans older than 65 years of age, we analyzed data on PAC use among Medicare fee-for-service beneficiaries between 1999 and 2013. We also evaluated the outcomes of in-hospital mortality, length of stay, 30-day mortality, 30-day readmission, and 1-year mortality. We also sought to examine trends in PAC use across age, race/ethnicity, and sex to identify any disparities across sociodemographic groups.
Methods
Using Medicare inpatient claims data from the Centers for Medicare and Medicaid Services, we identified all inpatient admissions of fee-for-service beneficiaries 65 years of age or older from January 1, 1999, to December 31, 2013. We used International Classification of Diseases, Ninth Revision, Clinical Modification codes to identify hospital stays in which pulmonary artery catheterization was performed (codes 89.63 [pulmonary artery pressure monitoring], 89.64 [pulmonary artery wedge monitoring], 89.66 [measurement of mixed venous blood gases], 89.67 [monitoring of cardiac output by oxygen consumption technique (Fick method)], and 89.68 [monitoring of cardiac output by other technique (thermodilution indicator)]). Institutional review board approval for this study was obtained through the Yale University Human Investigation Committee, who waived the need for informed patient consent.
We examined the demographic and clinical characteristics of patients who underwent pulmonary artery catheterization. For each year, we calculated the rate of PAC placement per all-cause 1000 admissions, an approach consistent with prior studies. The numerator included all hospitalizations in which a PAC was placed in a given year. Among patients with a hospitalization involving PAC placement, we determined the annual rates of in-hospital, 30-day, 6-month, and 1-year all-cause mortality. We used the date of admission as time zero for all mortality measures. In addition, we examined trends in hospital length of stay, defined as the difference between the discharge and admission dates. We also examined use of PACs across several diagnoses of interest: acute myocardial infarction (AMI), HF, and respiratory failure. We used the Mantel-Haenszel χ2 test to determine the statistical significance of temporal changes in observed outcomes and patient characteristics. Analyses were performed from September 25, 2015, to April 10, 2017, using SAS, version 9.4 (SAS Institute Inc). Statistical tests were 2-sided, with P < .05 considered statistically significant.
Results
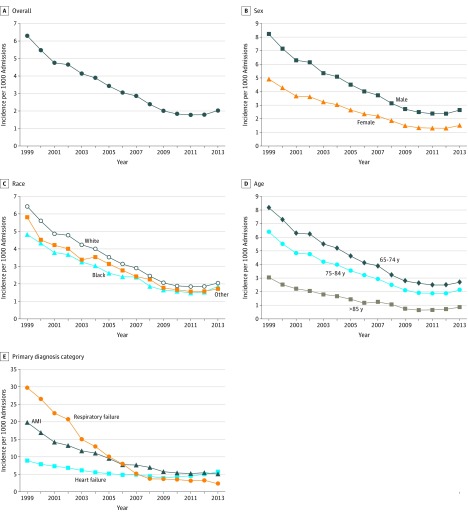
Our study sample included 68 374 904 unique Medicare beneficiaries, representing 420 390 283 beneficiary-years between January 1, 1999, and December 31, 2013. During the study period, there were 469 582 hospitalizations in which PACs were used for 457 193 patients (204 232 women and 252 961 men; mean [SD] age, 76.3 [6.9] years) (Table 1). There was a significant 67.8% relative decrease in PAC use from 6.28 per 1000 all-cause admissions in 1999 to 2.02 per 1000 all-cause admissions in 2013 (P < .001) (Figure, A). There were 2 distinct trends: significant year-on-year decreases from 1999 to 2011 (6.28 per 1000 admissions in 1999 to 1.79 per 1000 admissions in 2011), followed by stable use through 2013.
Table 1. Characteristics of Patients With Pulmonary Artery Catheter Placement From 1999 to 2013.
| Characteristic | Patients, No. (%) | |||||||
|---|---|---|---|---|---|---|---|---|
| 1999-2000 (n = 105 955) |
2001-2002 (n = 89 550) |
2003-2004 (n = 77 580) |
2005-2006 (n = 60 978) |
2007-2008 (n = 46 081) |
2009-2010 (n = 32 325) |
2011-2012 (n = 29 386) |
2013 (n = 15 338) |
|
| Age, mean (SD), y | 76.6 (6.8) | 76.5 (6.7) | 76.3 (6.8) | 76.3 (6.8) | 76.3 (7.1) | 75.7 (6.9) | 75.8 (7.0) | 75.9 (7.2) |
| Female sex | 48 451 (45.7) | 40 322 (45.0) | 35 077 (45.2) | 27 181 (44.6) | 20 575 (44.6) | 13 667 (42.3) | 12 457 (42.4) | 6502 (42.4) |
| Race/ethnicity | ||||||||
| White | 94 232 (88.9) | 79 065 (88.3) | 68 318 (88.1) | 53 507 (87.7) | 40 383 (87.6) | 28 184 (87.2) | 25 604 (87.1) | 13 224 (86.2) |
| Black | 7603 (7.2) | 6673 (7.5) | 5771 (7.4) | 4558 (7.5) | 3573 (7.8) | 2655 (8.2) | 2394 (8.1) | 1377 (9.0) |
| Other | 4120 (3.9) | 3812 (4.3) | 3491 (4.5) | 2913 (4.8) | 2125 (4.6) | 1486 (4.6) | 1388 (4.7) | 737 (4.8) |
| Comorbidities | ||||||||
| Heart failure | 27 205 (25.7) | 23 001 (25.7) | 19 213 (24.8) | 14 971 (24.6) | 11 142 (24.2) | 8497 (26.3) | 8784 (29.9) | 4823 (31.4) |
| Myocardial infarction | 7013 (6.6) | 5851 (6.5) | 4684 (6.0) | 3297 (5.4) | 2516 (5.5) | 1918 (5.9) | 1837 (6.3) | 936 (6.1) |
| Atherosclerotic disease | 49 664 (46.9) | 42 195 (47.1) | 36 393 (46.9) | 28 616 (46.9) | 22 137 (48.0) | 16 214 (50.2) | 15 546 (52.9) | 7858 (51.2) |
| Respiratory failure | 6020 (5.7) | 5117 (5.7) | 4272 (5.5) | 3691 (6.1) | 3512 (7.6) | 2812 (8.7) | 3197 (10.9) | 1807 (11.8) |
| Hypertension | 49 466 (46.7) | 45 093 (50.4) | 41 438 (53.4) | 33 594 (55.1) | 28 089 (61.0) | 20 003 (61.9) | 19 416 (66.1) | 9744 (63.5) |
| Renal failure | 8170 (7.7) | 8077 (9.0) | 7693 (9.9) | 7676 (12.6) | 7457 (16.2) | 6072 (18.8) | 6566 (22.3) | 3626 (23.6) |
| Diabetes | 29 873 (28.2) | 25 948 (29.0) | 22 743 (29.3) | 18 394 (30.2) | 14 010 (30.4) | 10 151 (31.4) | 10 121 (34.4) | 5427 (35.4) |
| Cancer | 11 469 (10.8) | 9380 (10.5) | 7362 (9.5) | 5288 (8.7) | 3751 (8.1) | 2448 (7.6) | 2191 (7.5) | 1225 (8.0) |
| COPD | 33 631 (31.7) | 28 810 (32.2) | 24 340 (31.4) | 18 620 (30.5) | 12 332 (26.8) | 7552 (23.4) | 7152 (24.3) | 3813 (24.9) |
| Pneumonia | 19 266 (18.2) | 16 423 (18.3) | 13 494 (17.4) | 10 096 (16.6) | 7515 (16.3) | 5616 (17.4) | 5246 (17.9) | 2698 (17.6) |
| Stroke | 2338 (2.2) | 1916 (2.1) | 1572 (2.0) | 1313 (2.2) | 872 (1.9) | 571 (1.8) | 537 (1.8) | 278 (1.8) |
| Liver disease | 2105 (2.0) | 1801 (2.0) | 1465 (1.9) | 1075 (1.8) | 745 (1.6) | 587 (1.8) | 620 (2.1) | 359 (2.3) |
Abbreviation: COPD, chronic obstructive pulmonary disease.
Figure. Pulmonary Artery Catheter (PAC) Use Rate per 1000 Admissions Between 1999 and 2013.
A, PAC use rate per 1000 admissions overall. B, PAC use rate per 1000 admissions across sex subgroups. C, PAC use rate per 1000 admissions across race/ethnicity subgroups. D, PAC use rate per 1000 admissions across age subgroups. E, PAC use rate per 1000 admissions across admissions for acute myocardial infarction (AMI), heart failure, and respiratory failure.
Significant reductions in PAC use but persistent variation were observed across demographic subgroups including sex, race/ethnicity, and age (Figure, B-D). Annual trends in PAC placement in hospitalizations for HF, respiratory failure, and AMI are shown in Figure, E. There was a significant and sustained reduction in the rate of PACs placed in hospitalizations for respiratory failure and AMI (20.0 PACs placed per 1000 admissions in 1999 to 5.2 in 2013 [74.0% reduction]; P < .001 for trend) and respiratory failure (29.9 PACs placed per 1000 admission in 1999 to 2.3 in 2013 [92.3% reduction]; Figure, E). In contrast, for HF admissions, there was an initial reduction from 1999 to 2009, followed by an increase in the rate of PAC placement (9.1 PACs placed per 1000 admissions in 1999 to 4.0 in 2009 and 5.8 in 2013). Between 1999 and 2013, in-hospital mortality among patients with PAC decreased significantly from 30.1% (n = 16 918) in 1999 to 8.6% (n = 1321) in 2013 (P < .001), with 30-day mortality decreasing from 33.8% (n = 19 028) to 13.4% (n = 2053) (P < .001; Table 2). The mean (SD) length of stay decreased from 9.1 (9.4) days in 1999 to 6.4 (6.0) days in 2013 (P < .001).
Table 2. Outcomes Associated With Pulmonary Artery Catheter Placement From 1999 to 2013.
| Outcome | Patients, No. (%) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | |
| Mortality | |||||||||||||||
| In hospital | 16 918 (30.1) |
14 968 (30.1) |
13 193 (29.4) |
11 958 (26.8) |
9555 (24.0) |
8113 (21.5) |
6158 (18.6) |
4506 (16.1) |
3278 (13.0) |
2522 (12.1) |
1994 (11.8) |
1765 (11.5) |
1481 (10.1) |
1410 (9.6) |
1321 (8.6) |
| 30 d | 19 028 (33.8) |
16 811 (33.8) |
14 826 (33.0) |
13 596 (30.4) |
11 047 (27.7) |
9520 (25.2) |
7429 (22.5) |
5501 (19.7) |
4226 (16.7) |
3311 (15.9) |
2619 (15.5) |
2387 (15.5) |
1955 (13.3) |
2079 (14.2) |
2053 (13.4) |
| 6 mo | 24 265 (43.1) |
21 515 (43.3) |
19 157 (42.7) |
17 764 (39.8) |
14 688 (36.9) |
12 812 (34.0) |
10 287 (31.1) |
7884 (28.2) |
6404 (25.3) |
5076 (24.4) |
4061 (24.0) |
3700 (24.0) |
3236 (22.0) |
3448 (23.5) |
3513 (22.9) |
| 1 y | 25 702 (45.7) |
22 710 (45.7) |
20 339 (45.3) |
18 828 (42.1) |
15 637 (39.2) |
13 678 (36.3) |
11 118 (33.7) |
8561 (30.6) |
7021 (27.8) |
5583 (26.9) |
4490 (26.5) |
4094 (26.6) |
3624 (24.6) |
3871 (26.4) |
3946 (25.7) |
| Disposition | |||||||||||||||
| Home | 17 131 (30.4) |
15 054 (30.3) |
13 948 (31.1) |
14 147 (31.7) |
12 793 (32.1) |
12 023 (31.9) |
11 234 (34.0) |
9785 (35.0) |
9464 (37.4) |
7538 (36.3) |
6119 (36.2) |
5400 (35.1) |
5152 (35.0) |
5203 (35.5) |
5321 (34.7) |
| Home with services | 6977 (12.4) |
6335 (12.7) |
5396 (12.0) |
5769 (12.9) |
5899 (14.8) |
6378 (16.9) |
5930 (18.0) |
5626 (20.1) |
5194 (20.5) |
4668 (22.5) |
3983 (23.5) |
3940 (25.6) |
3744 (25.4) |
3595 (24.5) |
3965 (25.9) |
| Skilled nursing facility | 9127 (16.2) |
7718 (15.5) |
6839 (15.2) |
6695 (15.0) |
6045 (15.2) |
5824 (15.4) |
5123 (15.5) |
4338 (15.5) |
3984 (15.7) |
3406 (16.4) |
2562 (15.1) |
2193 (14.2) |
2253 (15.3) |
2388 (16.3) |
2475 (16.1) |
| Hospice | 76 (0.1) |
104 (0.2) |
165 (0.4) |
312 (0.7) |
374 (0.9) |
520 (1.4) |
519 (1.6) |
446 (1.6) |
430 (1.7) |
343 (1.7) |
291 (1.7) |
307 (2.0) |
323 (2.2) |
332 (2.3) |
407 (2.7) |
| Transfer | 2561 (4.6) |
2207 (4.4) |
1921 (4.3) |
1911 (4.3) |
1403 (3.5) |
1269 (3.4) |
1077 (3.3) |
863 (3.1) |
761 (3.0) |
575 (2.8) |
452 (2.7) |
459 (3.0) |
449 (3.0) |
459 (3.1) |
471 (3.1) |
| Length of stay, mean (SD), d | 9.1 (9.4) |
9.0 (9.2) |
9.0 (9.6) |
8.7 (9.4) |
8.3 (8.6) |
8.2 (8.6) |
7.7 (8.3) |
7.2 (7.2) |
6.9 (7.2) |
6.8 (6.7) |
6.8 (6.6) |
6.7 (6.6) |
6.7 (6.6) |
6.5 (6.1) |
6.4 (6.0) |
Discussion
Our national study demonstrates a 67.8% decrease in the use of PACs from 1999 to 2013. Despite variation in PAC use across sociodemographic groups, there were significant reductions in use across age, sex, and race/ethnicity. In addition, we report heterogeneity in trends of PAC use across admissions for AMI, HF, and respiratory failure, with substantial and sustained decreases in PAC use for AMI and respiratory failure and a more modest initial decrease for HF with an increase in use more recently.
Our findings build on and extend the prior literature, providing the most expansive collection of national data to date on PAC use, as well as assessing length of stay and risk-adjusted clinical outcomes. Although there were significant reductions in PAC use overall and across sociodemographic groups, patterns of use across conditions were varied. Consistent with recent analyses from the National Inpatient Sample, we report a modest decrease in PAC use among patients with HF from 1999 to 2009, followed by a slight increase through 2013. One potential explanation for this increase in the rate of PAC use in admissions for HF is that the number of admissions for HF decreased from 2009 to 2013 (392 917 admissions in 2009 to 349 823 admissions in 2013), resulting in an increase in clinical severity and acuity, as has been described elsewhere. This finding notwithstanding, there has been an increase in the absolute number of PACs placed among patients hospitalized with HF (from 1581 in 2009 to 2012 in 2013). These findings are consistent with several potential explanations, including that the clinical profile of patients being admitted with HF has changed during the study period, that clinicians question the results and applicability of previous clinical trials, or that there are other clinical factors driving the use of PACs (eg, the need for invasive hemodynamic evaluation prior to consideration for advanced HF therapies, including mechanical circulatory support or transplantation). These results do not offer any insight into the appropriateness of PAC use, which remains a point of considerable controversy. Although the ACC/AHA guidelines along with the Society of Critical Care Medicine guidelines recommend against the routine use of PACs, the former endorses PAC use for patients when cardiac performance and filling pressures remain difficult to determine from clinical evaluation. The lack of detailed clinical and laboratory data limit our ability to adjudicate the appropriateness of PAC use and provide additional insights into the recent increase in PAC use observed among patients with HF. For instance, we observed a 3-fold increase in the prevalence of renal failure. Not only can a PAC provide definitive assessment of intravascular volume status, but patients with severe renal disease were excluded from prior clinical trials of PACs. Beyond these results for HF, we extend prior work by analyzing trends in PAC use among patients with AMI or respiratory failure. In fact, PAC use among both patients with AMI and patients with respiratory failure was significantly higher than use among patients with HF in 1999 and markedly decreased during the study interval.
Another key finding from our analysis is that, despite patients with PACs having increasing numbers of comorbidities, we observed significant decreases in in-hospital and 30-day mortality. This finding is likely the effect of a selection bias for critically ill patients, a population that has seen similar reductions in mortality, but improved patient selection for PAC placement may play a role as well.
Strengths and Limitations
The validity of our findings are supported by consistent results across several subgroups. More important, similar trends in PAC use described in other studies provide external validity. Our study should be interpreted in the context of the following limitations. First, we studied only fee-for-service Medicare beneficiaries, and findings may not be generalizable to patients who are younger or uninsured. Second, our study relies exclusively on administrative claims data. Our data do not provide the indication for PAC placement or information on the type of unit or hospital, which limits our ability to interpret these trends. Similarly, information on concomitant shock, acute renal failure, and subsequent left ventricular assist device or transplant and outpatient data on inotrope therapies could have provided additional insights into patterns of PAC use, but they were not available. Third, there remains the possibility of a systematic undercoding of PAC use because there are a limited number of fields to document procedure codes, and PAC placement may be “crowded out” in long hospitalizations. However, it is unlikely that this effect significantly changed over time.
Conclusions
In the wake of mounting evidence suggesting a lack of benefit to the routine use of PACs, there has been de-adoption of PAC use overall and across sociodemographic groups but heterogeneity in patterns of use across clinical conditions. These findings raise important questions about their optimal use and the drivers of the observed trends.
References
- 1.Connors AF Jr, Speroff T, Dawson NV, et al. ; SUPPORT Investigators . The effectiveness of right heart catheterization in the initial care of critically ill patients. JAMA. 1996;276(11):889-897. [DOI] [PubMed] [Google Scholar]
- 2.Rajaram SS, Desai NK, Kalra A, et al. . Pulmonary artery catheters for adult patients in intensive care. Cochrane Database Syst Rev. 2013;(2):CD003408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yancy CW, Jessup M, Bozkurt B, et al. ; American College of Cardiology Foundation; American Heart Association Task Force on Practice Guidelines . 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62(16):e147-e239. [DOI] [PubMed] [Google Scholar]
- 4.Dellinger RP, Levy MM, Rhodes A, et al. ; Surviving Sepsis Campaign Guidelines Committee including The Pediatric Subgroup . Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med. 2013;39(2):165-228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pandey A, Khera R, Kumar N, Golwala H, Girotra S, Fonarow GC. Use of pulmonary artery catheterization in US patients with heart failure, 2001-2012. JAMA Intern Med. 2016;176(1):129-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khera R, Pandey A, Kumar N, et al. . Variation in hospital use and outcomes associated with pulmonary artery catheterization in heart failure in the United States. Circ Heart Fail. 2016;9(11):e003226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wiener RS, Welch HG. Trends in the use of the pulmonary artery catheter in the United States, 1993-2004. JAMA. 2007;298(4):423-429. [DOI] [PubMed] [Google Scholar]
- 8.Wong CY, Chaudhry SI, Desai MM, Krumholz HM. Trends in comorbidity, disability, and polypharmacy in heart failure. Am J Med. 2011;124(2):136-143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Angus DC. Ongoing use of pulmonary artery catheters despite negative trial findings. JAMA Intern Med. 2016;176(1):133-134. [DOI] [PubMed] [Google Scholar]
- 10.Binanay C, Califf RM, Hasselblad V, et al. ; ESCAPE Investigators and ESCAPE Study Coordinators . Evaluation study of congestive heart failure and pulmonary artery catheterization effectiveness: the ESCAPE trial. JAMA. 2005;294(13):1625-1633. [DOI] [PubMed] [Google Scholar]
- 11.Wheeler AP, Bernard GR, Thompson BT, et al. ; National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network . Pulmonary-artery versus central venous catheter to guide treatment of acute lung injury. N Engl J Med. 2006;354(21):2213-2224. [DOI] [PubMed] [Google Scholar]
- 12.Kaukonen KM, Bailey M, Suzuki S, Pilcher D, Bellomo R. Mortality related to severe sepsis and septic shock among critically ill patients in Australia and New Zealand, 2000-2012. JAMA. 2014;311(13):1308-1316. [DOI] [PubMed] [Google Scholar]