Key Points
Question
What is the association between risk-adjusted 30-day readmission rate for myocardial infarction (MI) and in-hospital process of care measures and 1-year clinical outcomes?
Findings
In this analysis of hospitalized patients with MI in centers subject to the first cycle of the Hospital Readmissions Reduction Program, 30-day risk-adjusted readmission rates for MI were not associated with adherence to MI performance of measures or clinical outcomes occurring after the first 30 days after discharge.
Meaning
The performance metric for risk-standardized 30-day readmission rates for MI is not associated with quality of care, long-term mortality risk, or long-term readmission risk beyond the first 30 days following discharge.
Abstract
Importance
The US Centers for Medicare and Medicaid Services Hospital Readmissions Reduction Program penalizes hospitals with higher-than-expected risk-adjusted 30-day readmission rates (excess readmission ratio [ERR] > 1) after acute myocardial infarction (MI). However, the association of ERR with MI care processes and outcomes are not well established.
Objective
To evaluate the association between ERR for MI with in-hospital process of care measures and 1-year clinical outcomes.
Design, Setting, and Participants
Observational analysis of hospitalized patients with MI from National Cardiovascular Data Registry/Acute Coronary Treatment and Intervention Outcomes Network Registry–Get With the Guidelines centers subject to the first cycle of the Hospital Readmissions Reduction Program between July 1, 2008, and June 30, 2011.
Exposures
The ERR for MI (MI-ERR) in 2011.
Main Outcomes and Measures
Adherence to process of care measures during index hospitalization in the overall study population and risk of the composite outcome of mortality or all-cause readmission within 1 year of discharge and its individual components among participants with available Centers for Medicare and Medicaid Services–linked data.
Results
The median ages of patients in the MI-ERR greater than 1 and tertiles 1, 2, and 3 of the MI-ERR greater than 1 groups were 64, 63, 64, and 63 years, respectively. Among 380 hospitals that treated a total of 176 644 patients with MI during the study period, 43% had MI-ERR greater than 1. The proportions of patients of black race, those with heart failure signs at admission, and bleeding complications increased with higher MI-ERR. There was no significant association between adherence to MI performance measures and MI-ERR (adjusted odds ratio, 0.94; 95% CI, 0.81-1.08, per 0.1-unit increase in MI-ERR for overall defect-free care). Among the 51 453 patients with 1-year outcomes data available, higher MI-ERR was associated with higher adjusted risk of the composite outcome and all-cause readmission within 1 year of discharge. This association was largely driven by readmissions early after discharge and was not significant in landmark analyses beginning 30 days after discharge. The MI-ERR was not associated with risk for mortality within 1 year of discharge in the overall and 30-day landmark analyses.
Conclusions and Relevance
During the first cycle of the Hospital Readmissions Reduction Program, participating hospitals’ risk-adjusted 30-day readmission rates following MI were not associated with in-hospital quality of MI care or clinical outcomes occurring after the first 30 days after discharge.
This analysis evaluates the association between excess readmission ratio for myocardial infarction with in-hospital process of care measures and 1-year clinical outcomes during the first cycle of the Centers for Medicare and Medicaid Services Hospital Readmissions Reduction Program.
Introduction
Unplanned hospital readmissions are common and associated with significant clinical and financial burden. As a result, reducing readmission rates has been a central focus of recent payment reforms introduced by the US Centers for Medicare and Medicaid Services (CMS), which aim to improve quality and clinical outcomes as well as reduce costs. The Centers for Medicare and Medicaid Services implemented the Hospital Readmission Reduction Program (HRRP) in 2012 to provide financial incentives for reducing readmission. Under this program, US hospitals with higher-than-expected risk-standardized 30-day readmission rates for heart failure (HF), myocardial infarction (MI), and pneumonia receive financial penalties; in 2013, the first year of the program, the maximum penalty was 1% of 2013 Medicare base payments.
The use of risk-standardized 30-day readmission rates as a metric to promote quality of care across hospitals has been heavily scrutinized. Previous studies performed among patients with acute MI have demonstrated variable associations between in-hospital care quality, as determined by adherence to process of care measures, and short-term clinical outcomes, such as in-hospital mortality. However, data on relationships between the CMS-determined 30-day readmission performance metric and objective measures of care quality and long-term clinical outcomes for MI are lacking.
Accordingly, we evaluated the association between risk-standardized 30-day MI readmission rates and (1) measures of inpatient care quality and (2) 1-year clinical outcomes including both readmission and mortality among National Cardiovascular Data Registry (NCDR)/Acute Coronary Treatment and Intervention Outcomes Network (ACTION) Registry–Get With the Guidelines (GWTG) centers that participated in the first cycle of HRRP (fiscal year 2013).
Methods
Data Source
The NCDR ACTION Registry–GWTG is a voluntary national registry for outcomes-based quality improvement that includes consecutive patients presenting with MI at participating hospitals in the United States. The design of this registry has been previously described and is detailed in the eAppendix in the Supplement. This registry was either approved by an institutional review board or considered quality improvement data and not subject to institutional review board approval based on individual site determinations. The need for informed consent was also waived because all data were collected retrospectively and anonymously without unique patient identifiers. The Duke Clinical Research Institute institutional review board approved this present study, and the institute served as the data analysis center.
Data on postdischarge outcomes were obtained in a subgroup of ACTION Registry–GWTG participants 65 years and older and with fee-for-service Medicare coverage by linking with the Medicare denominator file and inpatient administrative claims using combinations of indirect identifiers (date of birth, sex, hospital identification, date of admission, and date of discharge). The strategy for probabilistic matching of patients to CMS claims files has been previously described.
Study Cohort
For the primary analysis, consecutive patients admitted with MI at NDCR ACTION Registry–GWTG sites participating in the first cycle of HRRP were eligible for inclusion (N = 229 252 from 519 sites). The study period corresponded to the time that was used to calculate readmission penalties for the first HRRP cycle (July 1, 2008, to June 30, 2011). Exclusion criteria included use of the short version of the data collection form, admission to participating hospitals with fewer than 25 cases of MI during the study period, transfer out of presenting hospital for further treatment, treatment at centers without percutaneous coronary intervention capability, and missing zip code information. The final study population included 176 644 participants from 380 sites (eFigure in the Supplement).
One-year outcome analysis was conducted in the subset of study participants with available CMS-linked follow-up data who were discharged alive from the index hospitalization (n = 51 453 from 377 sites).
Primary Exposure Variable
The excess readmission ratio (ERR) for MI (MI-ERR) for each participating center in the first cycle of HRRP (fiscal year 2013) was obtained from the publicly available CMS-HRRP supplemental data file. The details about calculation of MI-ERR have been previously described. Briefly, a hospital’s MI-ERR is the ratio between predicted and expected 30-day readmission rates during the study period. Rates are risk-adjusted based on age, comorbidities, and patient case mix using a previously reported risk-standardization protocol endorsed by the National Quality Forum. The HRRP penalty amount is calculated by comparing the dollars spent on excess readmissions for the target conditions with the total dollars spent on admissions at any given hospital. Therefore, if a center’s condition-specific ERR is less than 1 (indicating lower-than-expected readmission rates), it does not contribute to the overall readmission penalty.
Study Outcomes
The process of care outcomes of interest included adherence to individual MI acute and discharge performance measures listed in eTable 1 in the Supplement as well as the composite defect-free care metric, determined as the percentage of eligible patients with MI without contraindications who received all the recommended care during the index hospitalization (eTable 1 in the Supplement). The clinical outcomes assessed in the CMS-linked cohort were days from discharge to the composite of all-cause mortality or all-cause readmission within 1 year of discharge, and days to the individual components of 1-year mortality and 1-year all-cause readmission.
Statistical Analysis
The NCDR ACTION Registry-GWTG–participating centers included in this study were stratified into categories based on the MI-ERR determined by CMS for fiscal year 2013. Hospital-level characteristics were compared across groups with MI-ERR less than or equal to 1 and MI-ERR greater than 1. Differences in categorical variables between the 2 groups were assessed by χ2 tests. Differences in continuous variables were assessed by Wilcoxon rank-sum tests. Patient-level baseline characteristics and outcomes were compared across 4 MI-ERR–based hospital groups: MI-ERR less than or equal to 1 and tertiles of centers with MI-ERR greater than 1. Socioeconomic status was determined based on the median income of the patient’s residence zip code as previously reported; details are provided in the eAppendix in the Supplement.
Proportional adherence to individual acute and discharge MI process of care measures and use of overall defect-free care across the 4 MI-ERR–based hospital groups was compared using an unadjusted random-effect model, with a random intercept for hospital and fixed effects for 4 ordinal MI-ERR groups. Unadjusted and adjusted associations between continuous measures of MI-ERR and overall defect-free care were also assessed using generalized linear mixed models with a logit link, with a random intercept for hospital and fixed effects for MI-ERR and patient characteristics. The assumption of linearity of relationship between MI-ERR and defect-free care in this model was tested and determined to have been met. Flexible splines of other continuous variables were used to fit the models. The models were adjusted for demographic characteristics, medical history, clinical presentation characteristics, home medications, and number of defect-free care opportunities per patient as detailed in the eAppendix in the Supplement.
Unadjusted incidence of all-cause mortality and all-cause readmission at 1 year were presented as cumulative incidence curves. Mortality was accounted as a competing risk in the cumulative incidence curve for all-cause readmission. Random-effect Cox proportional hazard models were constructed to assess the association between continuous measures of MI-ERR and 1-year outcomes (1-year mortality and 1-year all cause readmission), accounting for hospital clustering. The association between MI-ERR (a 30-day measure) and risk of outcomes beyond the first 30 days after discharge was also evaluated by performing a landmark analysis of these outcomes at 30 days after discharge. In this analysis, patients with an event within the first 30 days after discharge were excluded and time to event was evaluated starting at the 31-day mark.
The proportional hazards assumption was met for time to composite outcome event (all-cause readmission or mortality) and time to mortality within 1 year. Although the outcome of time to all-cause readmission within 1 year did not meet the proportional hazards assumption, the hazard estimates for all-cause readmission within the first 30 days and 31 to 365 days were similar (data not shown), and thus, the results were reported similarly to the other end points, as full 1-year follow-up and landmark analyses beginning at day 31.
The covariates in the adjusted models included patient demographic characteristics, presentation signs and symptoms, laboratory results, medical history, and discharge medication as detailed in the eAppendix in the Supplement. The linearity of relationship between MI-ERR and the 1-year clinical outcomes in this model was tested and found to be nonlinear. The linear spline knot for MI-ERR was chosen at 1 to approximate the nonlinearity. Flexible splines of the other continuous variables were used to fit the models. For both overall defect-free care and clinical outcomes models, missing covariate data were less than 2% for all variables, so missing continuous variables were imputed to sex and MI subtype (ie, ST-elevation MI vs non–ST-elevation MI) median values, and missing categorical variables were imputed to the mode.
Results
Baseline hospital- and patient-level characteristics of ACTION Registry centers included vs excluded in our study are compared in eTable 2 and eTable 3 in the Supplement. Among hospital-level characteristics, centers included in the study were larger, more commonly academic hospitals, and were more likely to have cardiac surgery available. There were no major differences in the patient-level characteristics among centers included vs excluded from the study.
In our study, 42.9% of participating hospitals had higher-than-expected 30-day readmission rates for MI (MI-ERR > 1). Compared with centers with MI-ERR less than or equal to 1, the proportion of black patients was higher among hospital groups with MI-ERR greater than 1 (7.6% vs 4.5%; P = .01; Table 1). Participant-level characteristics across MI-ERR–based hospital groups are compared in Table 2. There were minimal differences in the age and proportion of women across the MI-ERR groups. The proportion of black patients and those with decompensated HF at presentation, severely depressed ejection fraction, and major bleeding events increased across rising MI-ERR categories.
Table 1. Hospital Characteristics Across MI-ERR–Based Groups in the Study Population.
| Hospital Characteristic | No. (%) | P Value | |
|---|---|---|---|
| MI-ERR ≤ 1 (n = 217) |
MI-ERR > 1 (n = 163) |
||
| Geographical region | |||
| West | 42 (19.4) | 7 (4.3) | .001 |
| Northeast | 17 (7.8) | 9 (5.5) | |
| Midwest | 60 (27.7) | 59 (36.2) | |
| South | 98 (45.2) | 88 (54.0) | |
| CABG facility | 180 (83.0) | 140 (85.9) | .44 |
| Academic | 45 (20.7) | 31 (19.0) | .68 |
| Hospital size, median (IQR) | 307 (221 to 425) | 338 (211 to 466) | .40 |
| Black patients, median (IQR) | 4.5 (1.5 to 14.1) | 7.6 (1.9 to 17.7) | .01 |
| SES score, mean (IQR) | −0.03 (−1.1 to 1.1) | −0.07 (−1.2 to 1.3) | .94 |
| Rural | 27 (12.4) | 11 (6.8) | .07 |
Abbreviations: CABG, coronary artery bypass graft; IQR, interquartile range; MI-ERR, excess readmission ratio for acute myocardial infarction; SES, Socioeconomic Status Scale.
Table 2. Patient Characteristics Among Centers Stratified by MI-ERR.
| Characteristic | No. (%) | |||
|---|---|---|---|---|
| MI-ERR ≤ 1 (n = 105 680) |
MI-ERR > 1 Tertile 1 (1.0003-1.0406) (n = 23 539) |
MI-ERR > 1 Tertile 2 (1.0408-1.0953) (n = 25 852) |
MI-ERR > 1 Tertile 3 (1.0959-1.2362) (n = 21 573) |
|
| Baseline characteristics | ||||
| Age, median (IQR), y | 64 (54-76) | 63 (53-74) | 64 (54-76) | 63 (53-74) |
| Women | 36 520 (34.6) | 8212 (34.9) | 9248 (35.8) | 7661 (35.5) |
| Black patients | 8384 (7.9) | 3042 (12.9) | 2892 (11.2) | 3457 (16.0) |
| Insurance status | ||||
| Medicare | 26 776 (25.3) | 6044 (25.7) | 6902 (26.7) | 5933 (27.5) |
| HMO/private | 60 668 (57.4) | 12 980 (55.1) | 14 651 (56.7) | 11 495 (53.3) |
| SES score, median (IQR) | −0.1 (−1.6 to 1.5) | −0.8 (−2.2 to 0.8) | −0.3 (−1.8 to 1.6) | −0.3 (−2.0 to 1.6) |
| History | ||||
| Diabetes | 32 050 (30.3) | 7302 (31.0) | 8240 (31.9) | 7034 (32.6) |
| MI | 25 806 (24.4) | 6013 (25.5) | 6937 (26.8) | 5648 (26.2) |
| Revascularization | 32 410 (30.7) | 7631 (32.4) | 8140 (31.5) | 6799 (31.5) |
| CHF | 12 000 (11.4) | 2748 (11.7) | 3804 (14.7) | 3164 (14.7) |
| Smoking | 37 443 (35.4) | 9221 (39.2) | 9222 (35.7) | 8201 (38.0) |
| Clinical characteristics at presentation | ||||
| STEMI presentation | 42 978 (40.7) | 9754 (41.4) | 9635 (37.3) | 9042 (41.9) |
| Signs of CHF | 15 013 (14.2) | 3375 (14.3) | 4358 (16.9) | 3906 (18.1) |
| Shock | 4725 (4.5) | 970 (4.1) | 1133 (4.4) | 1152 (5.3) |
| Systolic BP, median (IQR) mm Hg | 144 (123-164) | 145 (124-166) | 143 (123-164) | 143 (122-164) |
| Cocaine use with version 2 or higher of Data Collection Form | 860 (0.8) | 274 (1.2) | 180 (0.7) | 348 (1.6) |
| In-hospital management and events | ||||
| Medical management only for NSTEMI | 11 647 (18.6) | 2536 (18.4) | 3147 (19.4) | 2348 (18.7) |
| PCI for NSTEMI | 30 400 (48.5) | 6450 (46.8) | 7263 (44.8) | 5853 (46.7) |
| Severe depressed EF among patients with LVEF evaluated | 4780 (4.9) | 1214 (5.5) | 1214 (5.0) | 1185 (5.9) |
| Major bleeding | 9666 (9.2) | 2170 (9.2) | 2414 (9.3) | 2546 (11.8) |
| CHF | 6067 (5.7) | 1547 (6.6) | 1808 (7.0) | 1431 (6.6) |
| Length of stay, median (IQR), d | 3 (2-5) | 3 (2-6) | 3 (2-6) | 3 (2-6) |
Abbreviations: BP, blood pressure; CHF, congestive heart failure; EF, ejection fraction; HMO, health maintenance organization; IQR, interquartile range; LVEF, left ventricular ejection fraction; MI-ERR, excess readmission ratio for acute myocardial infarction; NSTEMI, non–ST-elevation myocardial infarction; PCI, percutaneous coronary intervention; SES, Socioeconomic Status Scale; STEMI, ST-elevation myocardial infarction.
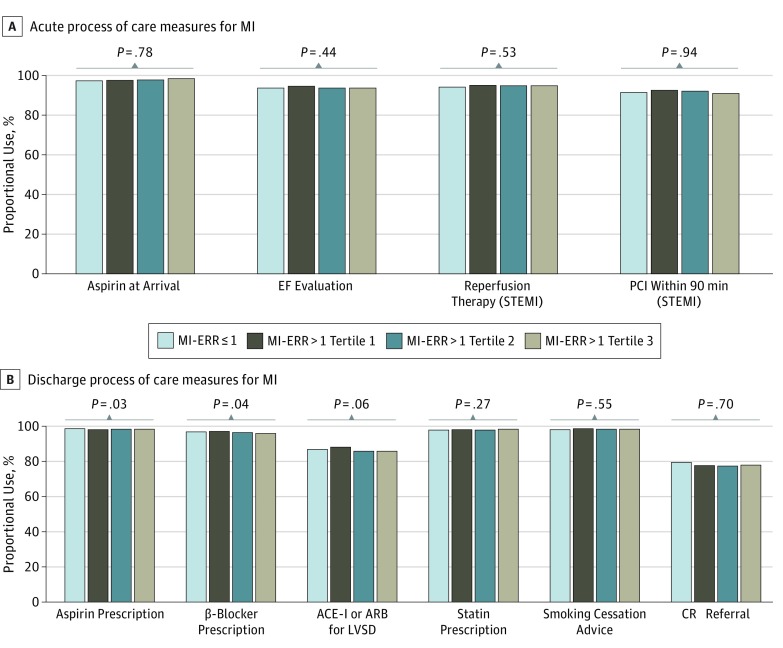
Adherence to MI process of care measures across MI-ERR categories are shown in Figure 1. The overall adherence to acute and discharge MI process of care measures was high in our study population. In unadjusted comparison, no significant difference in adherence to MI acute process of care measures was observed across MI-ERR–based hospital groups (Figure 1A). For discharge MI process of care measures, there was a statistically significant lower rate of use of aspirin and β-blockers at discharge among centers with higher MI-ERR. However, the absolute differences in adherence to these measures were modest. No significant differences were observed in adherence to other discharge MI process of care measures (Figure 1B). Overall defect-free care was also not significantly associated with continuous measures of MI-ERR in either unadjusted (odds ratio, 0.92; 95% CI. 0.80-1.06, per 0.1-unit increase in ERR) or adjusted (odds ratio, 0.94; 95% CI, 0.81-1.08, per 0.1-unit increase in ERR) analysis.
Figure 1. Adherence to Process of Care Measures for Myocardial Infarction (MI) Across Different Hospital Groups Based on the Excess Readmission Ratio for Acute MI (MI-ERR) in 2013.
ACE-I indicates angiotensin-converting enzyme inhibitor; ARB, angiotensin receptor blocker; CR, cardiac rehabilitation; EF, ejection fraction; LVSD, left ventricular systolic dysfunction; PCI, percutaneous coronary intervention; and STEMI, ST-elevation MI.
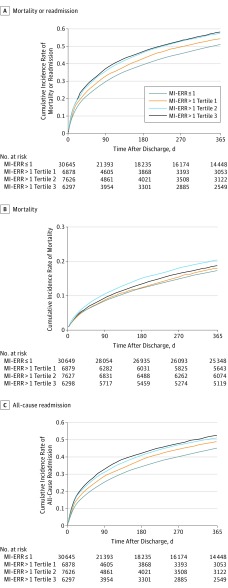
Figure 2 shows the cumulative incidence of 1-year clinical outcomes across the MI-ERR groups. The adjusted associations between continuous measures of MI-ERR and risk for clinical outcomes within 1-year are shown in Table 3. In adjusted analysis, the risk for the composite outcome of mortality or all-cause readmission within 1 year was higher with increasing MI-ERR. The risk for mortality or all-cause readmission was 9% higher per 0.1-unit increase in MI-ERR up to 1. Above this threshold, the risk increased by 6% per 0.1-unit increase in MI-ERR (Table 3). However, in the landmark analysis beginning 30 days after discharge from the index hospitalization, MI-ERR was not associated with long-term risk for composite outcomes after adjustment for potential confounders (Table 3).
Figure 2. Unadjusted Cumulative Incidence Rates.
The graphs show the unadjusted cumulative incidence rates for the composite outcome of all-cause readmission or mortality within 1-year (A); 1-year mortality (B); and 1-year all-cause readmission rates (C) across different hospital groups based on the excess readmission ratio for myocardial infarction (MI-ERR) in 2013.
Table 3. Adjusted Association Between Continuous Measures of MI-ERR and 1-Year Clinical Outcomes.
| Outcomea | Overall Population (Risk Between 1-365 d After Index Hospitalization) | Landmarked Cohort Event-Free at 30 d (Risk Between 31-365 d After Index Hospitalization)b | ||
|---|---|---|---|---|
| Adjusted HR (95% CI)c | P Value | Adjusted, HR (95% CI)c | P Value | |
| Composite outcomed | ||||
| MI-ERR per 0.1-unit increase up to 1 | 1.09 (1.06-1.11) | <.001 | 1.01 (0.93-1.09) | .88 |
| MI-ERR per 0.1-unit increase above 1 | 1.06 (1.03-1.09) | <.001 | 1.00 (0.91-1.10) | .93 |
| 1-y Mortality | ||||
| MI-ERR per 0.1-unit increase up to 1 | 1.00 (0.97-1.04) | .80 | 1.01 (0.96-1.05) | .81 |
| MI-ERR per 0.1-unit increase above 1 | 1.00 (0.95-1.05) | .92 | 1.00 (0.95-1.06) | .93 |
| 1-y All-cause readmission | ||||
| MI-ERR per 0.1-unit increase up to 1 | 1.06 (1.03-1.08) | <.001 | 1.01 (0.98-1.04) | .36 |
| MI-ERR per 0.1-unit increase above 1 | 1.04 (1.01-1.07) | .02 | 1.01 (0.97-1.05) | .67 |
Abbreviations: HR, hazard ratio; MI-ERR, excess readmission ratio for myocardial infarction.
Nonlinear relationship was observed between MI-ERR and 1-year outcomes and the linear spline knot for MI-ERR was chosen at 1 to approximate the nonlinearity.
For landmark analysis of mortality, we additionally excluded patients who died within the first 30 days (n = 2530). For landmark analysis of all-cause readmission, we additionally excluded patients who died (n = 1800) or had readmission (n = 8364) within the first 30 days and those with missing time to follow-up appointment (n = 7).
Separate models were created for the overall population and the landmarked cohorts. Models were adjusted for patients’ demographic characteristics, presentation signs and symptoms, laboratory results, medical history, and discharge medications as covariates (see the Methods section).
Composite of all-cause readmission or mortality.
When individual clinical outcomes were analyzed separately, MI-ERR was not associated with mortality risk after adjustment for potential confounders in the overall analysis (1-365 days after discharge) and landmark analysis (31-365 days after discharge) (Table 3). For the outcome of all-cause readmission, MI-ERR was associated with risk for readmission within 1 year of discharge in adjusted analysis. The risk for all-cause readmission within 1 year was 6% higher per 0.1-unit increase in MI-ERR up to 1. Above this threshold, the risk was 4% higher per 0.1-unit increase in MI-ERR (Table 3). However, in the landmark analysis starting 30 days after discharge, the association between MI-ERR and risk for readmission within 1 year of discharge was not significant (Table 3).
Discussion
To our knowledge, this is the first study to evaluate the association between 30-day risk-adjusted readmission rates and long-term clinical outcomes among US hospitals participating in the CMS HRRP. We found no significant association between MI-ERR and measures of care quality for MI during the index hospitalization. In addition, MI-ERR was not significantly associated with mortality risk at 1-year follow-up after adjustment for potential confounders. Finally, higher MI-ERR was significantly associated with greater risk for 1-year all-cause readmission. However, this association was driven by readmissions that occurred soon after hospitalization and was not significant for readmissions beyond the first 30 days.
Characteristics of Centers With Low vs High Risk-Adjusted Readmission Rates
We observed higher proportions of black patients in hospitals with higher MI-ERR. This is consistent with previous studies and suggests that hospitals serving more socioeconomically vulnerable patient populations, such as safety-net hospitals, are more likely to be penalized for higher readmission rates. We also observed differences in disease severity across MI-ERR–based hospital groups. Patients admitted to hospitals with higher MI-ERR had more prevalent HF symptoms, lower ejection fraction, and more bleeding events. Previous studies from other cohorts have also identified disease severity and comorbidity burden as significant predictors of short-term readmission among patients with MI.
Our findings are particularly relevant in the context of the strategy used by CMS for risk adjustment of the 30-day readmission rates. The Centers for Medicare and Medicaid Services adjusts for hospital-level differences in certain patient characteristics, such as age, comorbidity burden, and certain measures of disease severity, in the calculation of condition-specific ERR. However, they do not account for other relevant factors, such as race/ethnicity, or any measures of symptoms or ejection fraction. Because MI-ERR does not associate with indices of quality of care or 1-year mortality or readmissions between 31 and 365 days, our findings raise questions of whether CMS readmissions penalties are equitably and justly applied for hospitals with a high prevalence of socially and/or medically complex patients.
Risk-Adjusted 30-Day Readmission Rates and Quality of Care
Previous studies among patients with HF have failed to demonstrate a strong association between in-hospital quality of care and 30-day readmission rates. The findings from the present study extend these observations to patients with MI and suggest that the readmission performance metric used by CMS may not differentiate centers based on their in-hospital quality of care. Several factors may underlie the observed lack of association between MI-ERR and quality of care. First, the overall adherence to process of care measures among NCDR ACTION Registry-GWTG–participating hospitals is very high. Thus, there could be a “ceiling effect” limiting our ability to identify an association between MI-ERR and quality of care metrics. Second, the association between hospital-level quality of care and readmission risk is stronger over the first few days after discharge and declines significantly by 30 days. Third, 30-day readmissions may be related to care processes not captured by the metrics collected or related to nonmodifiable factors unrelated to the index hospitalization such as the socioeconomic and demographic profiles of the hospital’s patient population, the hospital’s resource availability, patient social support, or mental health issues. Finally, while measures of care quality are MI specific, most 30-day readmissions after MI, particularly in an older population, are related to noncardiovascular indications.
Risk-Adjusted 30-Day Readmission Rates and 1-Year Outcomes
Previous studies have evaluated the relationship between 30-day readmission and 30-day mortality in patients with HF and MI, with some studies reporting no correlation while others demonstrate an inverse association. In a recent study among GWTG-HF–participating centers, we observed that 30-day risk-adjusted readmission was not associated with 1-year all-cause mortality or readmission among patients with HF. To our knowledge, our study is the first to evaluate the association between the CMS 30-day readmission performance metric and long-term clinical outcomes in patients with MI. The association between MI-ERR and all-cause readmission or mortality within 1 year was largely driven by early events and was completely attenuated after excluding events that occurred within the first month after discharge. Taken together, findings from our study suggest that MI-ERR is not associated with clinical outcomes observed beyond the initial 30-day follow-up.
Health Policy Implications
Our study findings have important health policy implications. The Hospital Readmissions Reduction Program is intended to provide financial incentives to improve quality of care and clinical outcomes and to lower cost of care among hospitalized patients. While recent studies have demonstrated that implementation of HRRP has been associated with an overall reduction in readmission rates for conditions targeted by the program, the present results suggest that this strategy may not in and of itself lead to improvements in quality of care, long-term mortality, or even long-term readmission rates. For policies to drive broader innovation, incentive policies may need to reflect more diverse measures of care quality and patient-centered outcomes that are directly attributable to the care provided in the hospital setting. Large prospective cluster-randomized trials are needed to test novel hospital- and patient-level interventions aimed at improving these outcomes.
Our findings also highlight the inequitable burden of readmission among hospitals serving patient populations with higher levels of social disadvantage and higher illness acuity. For example, despite comparable care quality and clinical outcomes, we found that these hospitals had higher 30-day readmission rates, suggesting either nonmodifiable factors leading to readmission or incomplete risk adjustment. Thus, hospitals that treat a greater proportion of black or other disadvantaged patients may be unfairly penalized, which could deplete resources from the hospitals that need them most. This finding argues for the need to consider updating the readmission metric calculations with adjustments for race/ethnicity and better measures of disease severity. Another strategy would be to compare readmission rates of hospitals within peer groups that have similar patient populations to allow for fair comparison of hospital readmission performance, which is a strategy included in the recently passed 21st Century Cures Act.
Limitations
Our study has limitations that may impact interpretation of these results. First, the study population was limited to patients admitted to NCDR ACTION Registry–GWTG centers that participated in the first cycle of HRRP (fiscal year 2013). Consequently, study results may not be generalizable to all hospitals. Second, the observation period of our study corresponded to the time duration used by CMS to determine the first year of readmission penalties (2008-2011) and our findings may not be applicable to the quality of care and outcomes in following years (2012 onwards). Third, the data on process of care measures at participating centers were collected by medical record review and may be prone to inaccuracies. To the extent these are random errors, they should bias toward the null; in addition, audits of NCDR data have shown a high level of accuracy compared with medical records. Fourth, the strategy used for NCDR ACTION Registry–CMS probabilistic linkage is imperfect, with a success rate of 81% that is consistent with other studies linking national registries with CMS data. Fifth, there may be some degree of misclassification in 1-year outcomes determined from an administrative database, which may have attenuated some of the observed associations. However, the use of CMS administrative data to assess readmission and mortality outcomes is well established and previously validated. Finally, we did not consider rates of emergency department visits or observation status admissions on follow-up. Thus, we would have missed hospital visits on follow-up that were treated under “observation status” by the participating hospitals.
Conclusions
Among NCDR ACTION Registry–GWTG hospitals that were subject to the first year of the HRRP, the CMS metric for risk-standardized 30-day readmission rates for MI is not associated with quality of care, long-term mortality risk, or long-term readmission risk beyond the first 30 days following discharge. Additionally, there are concerning racial/ethnic inequities in MI-ERR–related hospital penalties. Future studies are needed to determine whether 30-day readmission rates are associated with any other meaningful quality measures and the impact of penalties associated with readmission rates on hospital performance and patient outcomes over time.
eAppendix. Supplemental Methods.
eTable 1. Acute and Discharge Process of Care Measures for Myocardial Infarction Evaluated in the Study.
eTable 2. Comparison of Characteristics of Hospitals Included vs Excluded in the Study.
eTable 3. Comparison of Baseline Characteristics of Patients Included vs Excluded in the Study.
eFigure. Cohort Derivation for the Study Population.
References
- 1.Fingar K, Washington R. Trends in Hospital Readmissions for Four High-Volume Conditions, 2009-2013: Statistical Brief No. 196: Healthcare Cost and Utilization Project (HCUP). Rockville, MD: Agency for Healthcare Research and Quality; 2006. [PubMed] [Google Scholar]
- 2.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418-1428. [DOI] [PubMed] [Google Scholar]
- 3.Hospital Readmissions Reduction Programs (HRRP). 76 Fed Reg 51660. August 18, 2011.
- 4.Centers for Medicare and Medicaid Services (CMS), HHS Medicare program; hospital inpatient prospective payment systems for acute care hospitals and the long-term care hospital prospective payment system and Fiscal Year 2014 rates; quality reporting requirements for specific providers; hospital conditions of participation; payment policies related to patient status: final rules. Fed Regist. 2013;78(160):50495-51040. [PubMed] [Google Scholar]
- 5.DeVore AD, Hammill BG, Hardy NC, Eapen ZJ, Peterson ED, Hernandez AF. Has public reporting of hospital readmission rates affected patient outcomes? analysis of Medicare claims data. J Am Coll Cardiol. 2016;67(8):963-972. [DOI] [PubMed] [Google Scholar]
- 6.Joynt KE, Jha AK. Thirty-day readmissions: truth and consequences. N Engl J Med. 2012;366(15):1366-1369. [DOI] [PubMed] [Google Scholar]
- 7.Joynt KE, Jha AK. A path forward on Medicare readmissions. N Engl J Med. 2013;368(13):1175-1177. [DOI] [PubMed] [Google Scholar]
- 8.Bradley EH, Herrin J, Elbel B, et al. Hospital quality for acute myocardial infarction: correlation among process measures and relationship with short-term mortality. JAMA. 2006;296(1):72-78. [DOI] [PubMed] [Google Scholar]
- 9.Granger CB, Steg PG, Peterson E, et al. ; GRACE Investigators . Medication performance measures and mortality following acute coronary syndromes. Am J Med. 2005;118(8):858-865. [DOI] [PubMed] [Google Scholar]
- 10.Peterson ED, Roe MT, Mulgund J, et al. Association between hospital process performance and outcomes among patients with acute coronary syndromes. JAMA. 2006;295(16):1912-1920. [DOI] [PubMed] [Google Scholar]
- 11.Peterson ED, Roe MT, Rumsfeld JS, et al. A call to ACTION (Acute Coronary Treatment and Intervention Outcomes Network): a national effort to promote timely clinical feedback and support continuous quality improvement for acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2009;2(5):491-499. [DOI] [PubMed] [Google Scholar]
- 12.Hammill BG, Hernandez AF, Peterson ED, Fonarow GC, Schulman KA, Curtis LH. Linking inpatient clinical registry data to Medicare claims data using indirect identifiers. Am Heart J. 2009;157(6):995-1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goyal A, de Lemos JA, Peng SA, et al. Association of patient enrollment in Medicare Part D with outcomes after acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2015;8(6):567-575. [DOI] [PubMed] [Google Scholar]
- 14.Centers for Medicare and Medicaid Services Readmissions Reduction Program (HRRP). https://www.cms.gov/medicare/medicare-fee-for-service-payment/acuteinpatientpps/readmissions-reduction-program.html. Accessed May 16, 2016.
- 15.Gilman M, Hockenberry JM, Adams EK, Milstein AS, Wilson IB, Becker ER. The financial effect of value-based purchasing and the hospital readmissions reduction program on safety-net hospitals in 2014: a cohort study. Ann Intern Med. 2015;163(6):427-436. [DOI] [PubMed] [Google Scholar]
- 16.QualityNet. Measure methodology reports: readmission measures. https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier4&cid=1219069855841. Accessed May 16, 2016.
- 17.Subherwal S, Patel MR, Tang F, et al. Socioeconomic disparities in the use of cardioprotective medications among patients with peripheral artery disease: an analysis of the American College of Cardiology’s NCDR PINNACLE Registry. J Am Coll Cardiol. 2013;62(1):51-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA. 2011;305(7):675-681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hess CN, Wang TY, McCoy LA, et al. Unplanned inpatient and observation rehospitalizations after acute myocardial infarction: insights from the Treatment With Adenosine Diphosphate Receptor Inhibitors: Longitudinal Assessment of Treatment Patterns and Events After Acute Coronary Syndrome (TRANSLATE-ACS) Study. Circulation. 2016;133(5):493-501. [DOI] [PubMed] [Google Scholar]
- 20.Tisminetzky M, McManus DD, Erskine N, et al. Thirty-day hospital readmissions in patients with non-ST-segment elevation acute myocardial infarction. Am J Med. 2015;128(7):760-765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fischer C, Steyerberg EW, Fonarow GC, Ganiats TG, Lingsma HF. A systematic review and meta-analysis on the association between quality of hospital care and readmission rates in patients with heart failure. Am Heart J. 2015;170(5):1005-1017.e2. [DOI] [PubMed] [Google Scholar]
- 22.Mathews R, Fonarow GC, Li S, et al. ; National Cardiovascular Data Registry . Comparison of performance on Hospital Compare process measures and patient outcomes between hospitals that do and do not participate in Acute Coronary Treatment and Intervention Outcomes Network Registry–Get With The Guidelines. Am Heart J. 2016;175:1-8. [DOI] [PubMed] [Google Scholar]
- 23.Chin DL, Bang H, Manickam RN, Romano PS. Rethinking thirty-day hospital readmissions: shorter intervals might be better indicators of quality of care. Health Aff (Millwood). 2016;35(10):1867-1875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dharmarajan K, Krumholz HM. Strategies to reduce 30-day readmissions in older patients hospitalized with heart failure and acute myocardial infarction. Curr Geriatr Rep. 2014;3(4):306-315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gorodeski EZ, Starling RC, Blackstone EH. Are all readmissions bad readmissions? N Engl J Med. 2010;363(3):297-298. [DOI] [PubMed] [Google Scholar]
- 26.Krumholz HM, Lin Z, Keenan PS, et al. Relationship between hospital readmission and mortality rates for patients hospitalized with acute myocardial infarction, heart failure, or pneumonia. JAMA. 2013;309(6):587-593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Press MJ, Scanlon DP, Ryan AM, et al. Limits of readmission rates in measuring hospital quality suggest the need for added metrics. Health Aff (Millwood). 2013;32(6):1083-1091. [DOI] [PubMed] [Google Scholar]
- 28.Pandey A, Golwala H, Xu H, et al. Association of 30-day readmission metric for heart failure under the hospital readmissions reduction program with quality of care and outcomes. JACC Heart Fail. 2016;4(12):935-946. [DOI] [PubMed] [Google Scholar]
- 29.Desai NR, Ross JS, Kwon JY, et al. Association between hospital penalty status under the hospital readmission reduction program and readmission rates for target and nontarget conditions. JAMA. 2016;316(24):2647-2656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, Epstein AM. Readmissions, observation, and the hospital readmissions reduction program. N Engl J Med. 2016;374(16):1543-1551. [DOI] [PubMed] [Google Scholar]
- 31.Pub L No. 114–255. 21st Century Cures Act.
- 32.Messenger JC, Ho KK, Young CH, et al. ; NCDR Science and Quality Oversight Committee Data Quality Workgroup . The National Cardiovascular Data Registry (NCDR) Data Quality Brief: the NCDR Data Quality Program in 2012. J Am Coll Cardiol. 2012;60(16):1484-1488. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. Supplemental Methods.
eTable 1. Acute and Discharge Process of Care Measures for Myocardial Infarction Evaluated in the Study.
eTable 2. Comparison of Characteristics of Hospitals Included vs Excluded in the Study.
eTable 3. Comparison of Baseline Characteristics of Patients Included vs Excluded in the Study.
eFigure. Cohort Derivation for the Study Population.