Abstract
Importance
Headache can be a functional indication for ptosis repair and blepharoplasty.
Objective
To evaluate the changes in headache-related quality of life in patients who underwent upper eyelid ptosis repair or blepharoplasty.
Design, Setting, and Participants
A prospective cohort study was conducted among 108 patients who underwent standard upper eyelid blepharoplasty and 44 patients who underwent ptosis repair (levator resection, Müller muscle resection, or frontalis suspension) for obscuration of the superior visual field at an ophthalmology clinic’s oculoplastic department from September 1, 2014, to September 1, 2015. A validated headache-related quality-of-life survey, the Headache Impact Test-6 (HIT), was administered preoperatively and postoperatively to patients who had tension-type headache. The minimum time interval after the operation was 3 months (mean, 13.5 weeks; range, 12-17 weeks).
Main Outcomes and Measures
Postoperative HIT scores, decline in HIT scores, and marginal reflex distance test 1 scores.
Results
Of the 108 patients (66 women and 42 men; mean [SD] age, 49.8 [10.7] years) who underwent blepharoplasty and the 44 patients (26 women and 18 men; mean [SD] age, 45.6 [17.8] years) who underwent ptosis repair, 38 (35.2%) and 28 (63.6%), respectively, had symptoms of tension-type headaches. In both groups, the mean (SD) postoperative HIT scores were statistically significantly better than the preoperative HIT scores (blepharoplasty group: preoperative score, 55.9 [6.6] vs postoperative score, 46.4 [9.0]; ptosis repair group: preoperative score, 60.0 [7.2] vs postoperative score, 42.3 [9.3]; P = .001). In the patients who underwent ptosis repair, the mean (SD) preoperative HIT score was significantly higher than in those who underwent blepharoplasty (60.0 [7.2] vs 55.9 [6.6]; P = .007) and the postoperative HIT score was significantly lower than those who underwent blepharoplasty (42.3 [9.3] vs 46.4 [9.0]; P = .03). The mean (SD) decline in the HIT score was significantly higher in patients who underwent ptosis repair than in those who underwent blepharoplasty (17.8 [9.9] vs 9.5 [8.6]; P = .002). For patients who underwent ptosis repair, there was a statistically significant negative correlation between the results on the marginal reflex distance test 1 (median, 1.82; minimum, 1.0; maximum, 3.5) and change in the HIT score (median, 18; minimum, 0; maximum, 30) (P = .005; r = –0.645). In patients who underwent ptosis repair, the mean (SD) difference between the preoperative and postoperative HIT scores was significantly higher for the patients who underwent levator resection (3.1 [0.3]) than for those who underwent Müller muscle resection (1.5 [0.7]) and frontalis suspension procedures (1.9 [0.7]) (P = .001).
Conclusions and Relevance
The operations for ptosis and blepharoptosis provide significant relief for tension-type headache and result in improved headache-related quality of life. As a result, tension-type headache can be a functional indication for upper eyelid blepharoplasty and ptosis repair, especially for patients with lower results on the marginal reflex distance test 1.
Level of Evidence
3.
This cohort study evaluates the changes in headache-related quality of life in patients who underwent upper eyelid ptosis repair or blepharoplasty.
Key Points
Question
Can ptosis repair or blepharoplasty lead to an improvement in headache-related quality of life?
Findings
In this cohort study, postoperative Headache Impact Test-6 scores were significantly better than preoperative scores in patients who underwent ptosis repair and those who underwent blepharoplasty. The Headache Impact Test-6 score decline ratio was significantly higher in patients who underwent ptosis repair than in those who underwent blepharoplasty.
Meaning
Tension-type headache can be a functional indication for upper eyelid ptosis repair and blepharoplasty.
Introduction
The levator aponeurosis and the underlying Müller muscle retract the eyelid to open the eye. In contrast, contraction of the occipitofrontalis muscle raises the eyebrow and can assist in lifting the eyelid through the orbicularis fascia.
In aponeurotic blepharoptosis, the levator aponeurosis and the underlying Müller muscle are disinserted from the tarsus and are attenuated and elongated. Matsuo et al reported that, because of slippage between the levator aponeurosis and the tarsus, stretching of the mechanoreceptors in the Müller muscle is increased even in primary gaze and induces phasic and tonic reflex contraction of the occipitofrontalis muscles.
Dermatochalasis, or excess upper eyelid skin, may interfere with the superior visual field. Droopiness of the eyelids can lead to reflex contraction of the occipitofrontalis muscles as it does in patients with ptosis. As a result of tonic reflex contraction of the occipitofrontalis muscle, dermatochalasis may also induce tension-type headache. Tension-type headache is the most common form of primary headache, with a mean lifetime prevalence of 46%. The chronic form of a tension-type headache is a serious disease causing a marked decrease in quality of life and significant disability. However, its etiologic factors are uncertain, although activation of peripheral afferent neurons from the head and neck muscles may play a role. Injection of botulinum toxin and excision of the corrugator superciliaris muscle are the treatment options in the oculofacial literature for patients with tension-type headache.
This study prospectively examines patients who have undergone ptosis repair and blepharoplasty. Their changes in headache-related quality of life were evaluated by using a validated headache-related quality-of-life survey, the Headache Impact Test-6 (HIT), to determine whether any change occurs in the HIT scores following these surgical procedures.
Methods
The patient population was prospectively selected from an ophthalmology clinic oculoplastic department. All patients who underwent standard upper eyelid blepharoplasty or ptosis repair (levator resection, Müller muscle resection, or frontalis suspension) by 1 oculoplastic surgeon (I.B.S.) from September 1, 2014, to September 1, 2015, were included. The patients who underwent blepharoplasty are group 1; those who underwent ptosis repair are group 2. All participants provided verbal informed consent. The study was conducted in compliance with the principles of the Declaration of Helsinki. The Biruni University Hospital Institutional Review Board approved this study.
Patients were asked if they had any headache before the operation. Those who did were asked if they had been diagnosed with tension-type, migraine, or any other type of headache by their neurologist or primary care physician according to the criteria of the International Headache Society. The HIT was administered preoperatively and postoperatively to patients who had tension-type headache. Patient information was collected from clinical visits, clinical medical records, and telephone interviews. The minimum time interval after the operation was 3 months (mean, 13.5 weeks; range, 12-17 weeks).
Patients were excluded if they had known orbital, corneal, or intracranial pathologic conditions; a history of trauma; had received botulinum toxin; a change in headache medications; or headache other than tension-type headache. Patients who did not agree to participate were excluded from the study.
Statistical analysis was performed with SPSS for Windows, version 22.0 (IBM Corp). Measurable data are presented as mean (SD). The range of the variable data was measured using a Kolmogorov-Smirnov test. Quantitative data were analyzed with independent samples using a 2-tailed t test and a Mann-Whitney test. Qualitative data were analyzed using a χ2 test. Repetitive data were analyzed using a Wilcoxon test. P < .05 was considered statistically significant.
Results
A total of 152 patients met the inclusion criteria. Group 1 included 108 patients undergoing bilateral blepharoplasty; group 2 comprised 44 patients undergoing ptosis repair (17 [38.6%] underwent levator resection, 22 [50.0%] underwent Müller muscle resection, and 5 [11.4%] underwent frontalis suspension operations) (Table 1). There was no statistically significant difference between the groups in mean (SD) age (group 1, 49.8 [10.7] years; group 2, 45.6 [17.8] years; P = .07) and sex (group 1, 66 women [61.1%] and 42 men [38.9%]; group 2, 26 women [59.1%] and 18 men [40.9%]; P = .82).
Table 1. Patient Demographic Characteristics.
| Characteristic | Group, Valuea | P Valueb | |
|---|---|---|---|
| Blepharoplasty (n = 108) |
Ptosis Repair (n = 44) |
||
| Age, y | |||
| Mean (SD) | 49.8 (10.7) | 45.6 (17.8) | .07 |
| Median (range) | 49 (28-73) | 42 (20-80) | |
| Sex | |||
| Female | 66 (61.1) | 26 (59.1) | .82 |
| Male | 42 (38.9) | 18 (40.9) | |
| Headache | |||
| Yes | 38 (35.2) | 28 (63.6) | .001 |
| No | 70 (64.8) | 16 (36.4) | |
| Ptosis repair type | |||
| Müller muscle resection | NA | 22 (50.0) | NA |
| Frontalis suspension | NA | 5 (11.4) | NA |
| Levator resection | NA | 17 (38.6) | NA |
Abbreviation: NA, not applicable.
Data are presented as number (percentage) of patients unless otherwise indicated.
t Test for age; χ2 test for sex.
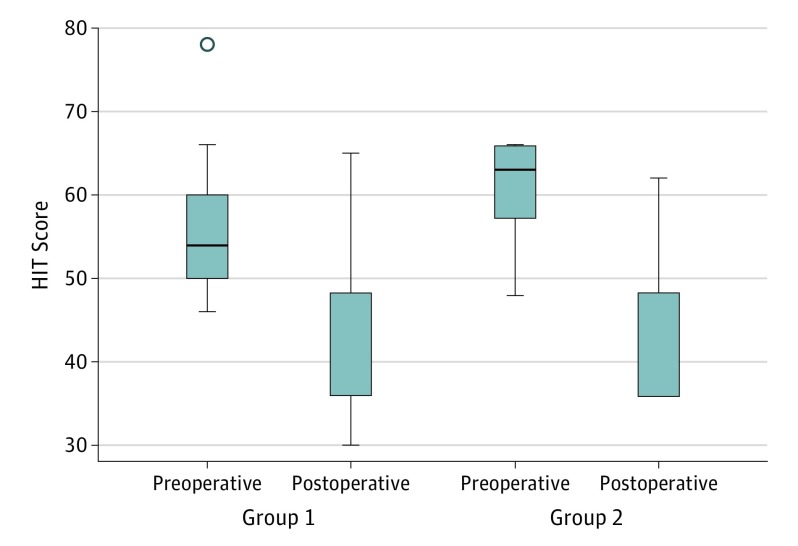
Thirty-eight patients (35.2%) in group 1 and 28 patients (63.6%) in group 2 had tension-type headache (P = .001). In both groups, the mean (SD) postoperative HIT scores were statistically significantly better than the preoperative HIT scores (group 1: preoperative score, 55.9 [6.6], and postoperative score, 46.4 [9.0]; group 2: preoperative score, 60.0 [7.2], and postoperative score, 42.3 [9.3]; P = .001). In group 2, the mean (SD) preoperative HIT score was significantly higher than in group 1 (60.0 [7.2] vs 55.9 [6.6]; P = .007) and the postoperative HIT score was significantly lower than in group 1 (42.3 [9.3] vs 46.4 [9.0]; P = .03). In addition, the mean (SD) difference between the preoperative and postoperative HIT score was significantly higher in group 2 (17.8 [9.9]) than in group 1 (9.5 [8.6]; P = .002) (Table 2 and Figure 1).
Table 2. Preoperative and Postoperative HIT Scores.
| HIT Score | Blepharoplasty | Ptosis Repair | P Value | ||
|---|---|---|---|---|---|
| Mean (SD) | Median (Range) | Mean (SD) | Median (Range) | ||
| Preoperative | 55.9 (6.6) | 54 (46-78) | 60.0 (7.2) | 63 (48-66) | .007 |
| Postoperative | 46.4 (9.0) | 48 (30-65) | 42.3 (9.3) | 36 (36-62) | .03 |
| Difference between preoperative and postoperative score | 9.5 (8.6) | 12 (8-36) | 17.8 (9.9) | 18 (0-30) | .002 |
Abbreviation: HIT, Headache Impact Test-6.
Figure 1. Preoperative and Postoperative Headache Impact Test-6 (HIT) Scores .
Group 1 includes patients who underwent blepharoplasty. Group 2 includes patients who underwent ptosis repair. Boxes indicate medians; error bars, upper and lower limits; and circle, outliers.
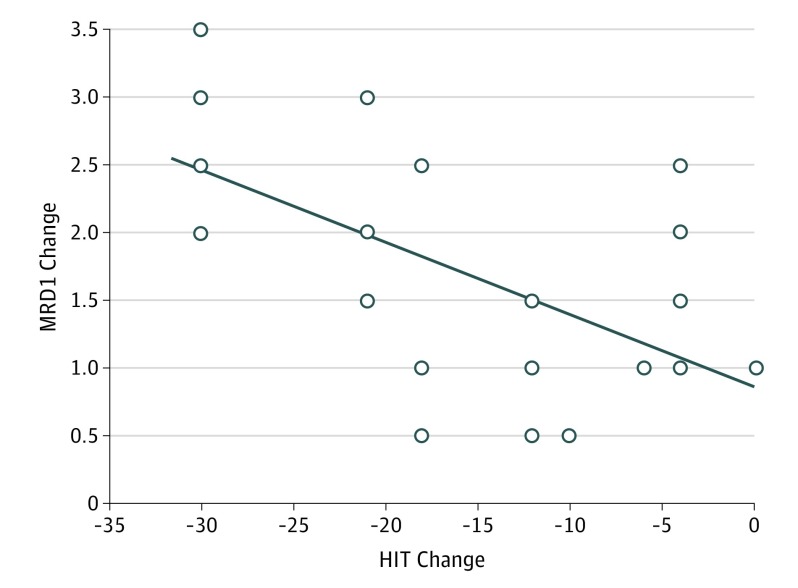
In group 2, there was no significant difference between patients undergoing the Müller muscle resection, frontalis suspension, or levator resection in the mean (SD) preoperative (59.3 [8.4], 58.6 [5.1], and 66.0 [0.0], respectively; P = .054) and postoperative (40.6 [7.4], 48.8 [11.9], and 36.0 [0.0], respectively; P = .08) HIT scores. In addition, the mean (SD) difference between the preoperative and postoperative HIT score was statistically significant for patients undergoing the Müller muscle resection (1.5 [0.7]; P = .001), frontalis suspension (1.9 [0.7]; P = .02), and levator resection (3.1 [0.3]; P = .046). The mean (SD) difference between the preoperative and postoperative HIT score was significantly higher in patients undergoing levator resection (3.1 [0.3]) than in those undergoing Müller muscle resection (1.5 [0.7]) or frontalis suspension (1.9 [0.7]; P = .005). The mean (SD) difference between the preoperative and postoperative HIT score in patients undergoing Müller muscle resection (1.5 [0.7]; P = .001) and frontalis suspension (1.9 [0.7]; P = .02) was statistically significant (Table 3). In addition, for group 2, there was a statistically significant negative correlation between the results on the marginal reflex distance test 1 (MRD1) (median, 1.82; minimum, 1.0; maximum, 3.5) and change in HIT score (median, 18; minimum, 0; maximum, 30) (P = .005; r = –0.645) (Figure 2).
Table 3. Preoperative and Postoperative HIT Scores for Patients Undergoing Müller Muscle Resection, Frontalis Suspension, and Levator Resection .
| HIT Score | Mean (SD) [Median] | P Valuea | ||
|---|---|---|---|---|
| Müller Muscle Resection | Frontalis Suspension | Levator Resection | ||
| Preoperative | 59.3 (8.4) [66.0] | 58.6 (5.1) [59.5] | 66.0 (0.0) [66.0] | .054 |
| Postoperative | 40.6 (7.4) [36.0] | 48.8 (11.9) [51.0] | 36.0 (0.0) [36.0] | .08 |
| Difference between preoperative and postoperative score | 18.6 (7.9) [18.0] | 9.9 (9.3) [4.0] | 30.0 (0.0) [30.0] | .005 |
| P valueb | .001 | .02 | .046 | |
Abbreviation: HIT, Headache Impact Test-6.
Mann-Whitney test.
Kruskal-Wallis test.
Figure 2. Preoperative and Postoperative Headache Impact Test-6 (HIT) Scores and Marginal Reflex Distance Test 1 (MRD1) Changes Among Patients Undergoing Ptosis Repair.
There was a statistically significant negative correlation between the results on the MRD1 and change in HIT score in group 2 (P = .005; r = –0.645).
Discussion
Surgery to correct upper eyelid ptosis and dermatochalasis has been performed for both cosmetic and functional indications. Surgical indications currently in common use include impaired visual acuity, decreased peripheral vision, a compensatory chin-up backward head tilt, difficulty reading, eye strain, and fatigue. This study found that after ptosis repair and blepharoplasty, HIT scores are significantly better, so tension-type headache may be another indication for these surgeries.
A tension-type headache is the most common form of primary headache. Injection of botulinum toxin and excision of the corrugator superciliaris muscle are the treatment alternatives for patients with chronic, recurrent tension type-headaches. Bearden and Anderson reported that corrugator excision is an effective surgical treatment of tension-type headaches. Of the 7 patients in their study with tension-type headache, 4 (57%) had complete resolution of their symptoms after corrugator excision. They speculated that their technique is an option for patients undergoing blepharoplasty who have chronic, recurrent, and debilitating tension-type headache. Ptosis repair and blepharoplasty indications for headache are concerned with eye strain and fatigue. In a report by the American Academy of Ophthalmology, Cahill et al evaluated the functional indications for upper eyelid ptosis repair and blepharoplasty. Literature searches of the PubMed and Cochrane Library databases produced 13 studies that reported the functional effects or treatment results; the authors concluded that the repair of ptosis and upper eyelid dermatochalasis provides significant improvement in vision, peripheral vision, and quality-of-life activities.
A study by Olson and Putterman found that 43% of 88 eyelids with ptosis had a vertical palpebral fissure height of zero in downgaze when the brows were relaxed. Thirty percent of their patients had subjective symptoms of an inability to read or work in the downgaze position for long periods, brow ache, fatigue, or having to manually elevate their eyelids to see in the downgaze position. Olson and Putterman reported that after ptosis repair there was a significant widening of the vertical palpebral fissure height in the downgaze position. The patients also reported relief of their brow ache, fatigue, and inability to read or work in the downgaze position.
In a study by Mokhtarzadeh et al, patients undergoing upper eyelid surgery to repair obscuration of the superior visual field, who also reported headache symptoms for greater than 1 year, completed the HIT before and after surgery (study group). A cohort of patients undergoing other oculoplastic procedures with all type of headaches also completed the questionnaire before and after surgery (control group). Mokhtarzadeh et al compared the answers to the HIT survey questions between the control and the study group preoperatively. The answers to all HIT questions on the postoperative survey were significantly better in the study group compared with the control group. They reported that correction of visually significant upper eyelid position may improve symptoms of chronic headache, similar to the results of the present study.
Different from the results found by Mokhtarzadeh et al, the present study selected only patients with tension-type headache. In addition, in the group undergoing ptosis repair, statistical analysis was performed specifically for the preoperative and postoperative change in MRD1 and HIT score difference. The results showed that there is a negative correlation between the changes in the MRD1 and HIT score.
Federici et al reported that surgical repair of blepharoptosis results in marked improvement in several aspects of patients’ subjective visual function and health-related quality of life. They showed a mean 30-point increase in functional index score after ptosis repair. Battu et al also reported that surgical repair of acquired involutional blepharoptosis resulted in significant improvement in several aspects of patients’ subjective visual function and health-related quality of life. Patipa showed that ptosis surgery improved patients’ visual field. However, none of these studies specifically targeted tension-type headache.
Studies by Matsuo et al showed that, in patients with ptosis, to maintain an appropriate visual field, mechanoreceptors in the Müller muscle stimulate a tonic reflex, contracting the occipitofrontalis muscle and inducing chronic tension-type headache associated with occipitofrontalis tenderness. Therefore, surgical desensitization of the mechanoreceptors in the Müller muscle appears to relieve chronic tension-type headache. They demonstrated their hypothesis in the electromyographic activity of the frontalis muscle of patients with and without chronic tension-type headache. The results of the present study are correlated with the results seen by Matsuo et al, as the preoperative HIT scores of the patients undergoing ptosis repair were higher than those of the patients undergoing blepharoplasty. In addition, the difference between the preoperative and postoperative HIT score was significantly higher in patients undergoing ptosis repair than those undergoing blepharoplasty. When only the type of ptosis repair is taken into consideration, the difference between the preoperative and postoperative HIT score was significantly higher for patients undergoing levator resection.
Limitations
This study has some limitations. First, the sample size was small for the patients undergoing ptosis repair. In this small group, statistical analysis was performed to see if the 3 types of operations were correlated with changes in the HIT score. Second, although the HIT score depends heavily on the patients and may be considered subjective, it is an objective test and one of the major methods to evaluate headache severity and its effect on patients’ daily lives; it is not possible to objectively evaluate headache severity.
Conclusions
This study has shown that repair of ptosis and upper eyelid dermatochalasis provides significant improvement in HIT scores for patients who have tension-type headache. This type of headache can be another functional indication for ptosis repair and blepharoplasty. Especially for the ptosis patients with lower results on the MRD1, correction of ptosis improves symptoms of chronic headache.
References
- 1.Siegel R. Surgical anatomy of the upper eyelid fascia. Ann Plast Surg. 1984;13(4):263-273. [DOI] [PubMed] [Google Scholar]
- 2.Matsuo K, Osada Y, Ban R. Electrical stimulation to the trigeminal proprioceptive fibres that innervate the mechanoreceptors in Müller’s muscle induces involuntary reflex contraction of the frontalis muscles. J Plast Surg Hand Surg. 2013;47(1):14-20. [DOI] [PubMed] [Google Scholar]
- 3.Matsuo K, Ban R. Surgical desensitisation of the mechanoreceptors in Müller’s muscle relieves chronic tension-type headache caused by tonic reflexive contraction of the occipitofrontalis muscle in patients with aponeurotic blepharoptosis. J Plast Surg Hand Surg. 2013;47(1):21-29. [DOI] [PubMed] [Google Scholar]
- 4.Bearden WH, Anderson RL. Corrugator superciliaris muscle excision for tension and migraine headaches. Ophthal Plast Reconstr Surg. 2005;21(6):418-422. [DOI] [PubMed] [Google Scholar]
- 5.Mokhtarzadeh A, McClelland C, Lee MS, Smith S, Harrison AR. The bleph and the brain: the effect of upper eyelid surgery on chronic headaches [published online March 24, 2016]. Ophthal Plast Reconstr Surg. doi: 10.1097/IOP.0000000000000686 [DOI] [PubMed] [Google Scholar]
- 6.Headache Classification Subcommittee of the International Headache Society The International Classification of Headache Disorders: 2nd edition. Cephalalgia. 2004;24(suppl 1):9-160. [DOI] [PubMed] [Google Scholar]
- 7.Vaughn R, Pall ML, Haynes SN. Frontalis EMG response to stress in subjects with frequent muscle-contraction headaches. Headache. 1977;16(6):313-317. [DOI] [PubMed] [Google Scholar]
- 8.Waldie KE, Buckley J, Bull PN, Poulton R. Tension-type headache: a life-course review. J Headache Pain Manage. 2015;1(2):1-9. [Google Scholar]
- 9.Guyuron B, Varghai A, Michelow BJ, Thomas T, Davis J. Corrugator supercilii muscle resection and migraine headaches. Plast Reconstr Surg. 2000;106(2):429-434. [DOI] [PubMed] [Google Scholar]
- 10.Guyuron B, Tucker T, Davis J. Surgical treatment of migraine headaches. Plast Reconstr Surg. 2002;109(7):2183-2189. [DOI] [PubMed] [Google Scholar]
- 11.Dirnberger F, Becker K. Surgical treatment of migraine headaches by corrugator muscle resection. Plast Reconstr Surg. 2004;114(3):652-657. [DOI] [PubMed] [Google Scholar]
- 12.Barbanti P, Egeo G, Fofi L, Aurilia C, Piroso S. Rationale for use of onabotulinum toxin A (Botox) in chronic migraine. Neurol Sci. 2015;36(suppl 1):29-32. [DOI] [PubMed] [Google Scholar]
- 13.Schulte-Mattler WJ, Wieser T, Zierz S. Treatment of tension-type headache with botulinum toxin: a pilot study. Eur J Med Res. 1999;4(5):183-186. [PubMed] [Google Scholar]
- 14.Blumenfeld AM, Binder W, Silberstein SD, Blitzer A. Procedures for administering botulinum toxin type A for migraine and tension-type headache. Headache. 2003;43(8):884-891. [DOI] [PubMed] [Google Scholar]
- 15.Janis JE, Dhanik A, Howard JH. Validation of the peripheral trigger point theory of migraine headaches: single-surgeon experience using botulinum toxin and surgical decompression. Plast Reconstr Surg. 2011;128(1):123-131. [DOI] [PubMed] [Google Scholar]
- 16.Kosinski M, Bayliss MS, Bjorner JB, et al. . A six-item short-form survey for measuring headache impact: the HIT-6. Qual Life Res. 2003;12(8):963-974. [DOI] [PubMed] [Google Scholar]
- 17.World Medical Association World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191-2194. [DOI] [PubMed] [Google Scholar]
- 18.Cahill KV, Bradley EA, Meyer DR, et al. . Functional indications for upper eyelid ptosis and blepharoplasty surgery: a report by the American Academy of Ophthalmology. Ophthalmology. 2011;118(12):2510-2517. [DOI] [PubMed] [Google Scholar]
- 19.Olson JJ, Putterman A. Loss of vertical palpebral fissure height on downgaze in acquired blepharoptosis. Arch Ophthalmol. 1995;113(10):1293-1297. [DOI] [PubMed] [Google Scholar]
- 20.Federici TJ, Meyer DR, Lininger LL. Correlation of the vision-related functional impairment associated with blepharoptosis and the impact of blepharoptosis surgery. Ophthalmology. 1999;106(9):1705-1712. [DOI] [PubMed] [Google Scholar]
- 21.Battu VK, Meyer DR, Wobig JL. Improvement in subjective visual function and quality of life outcome measures after blepharoptosis surgery. Am J Ophthalmol. 1996;121(6):677-686. [DOI] [PubMed] [Google Scholar]
- 22.Patipa M. Visual field loss in primary gaze and reading gaze due to acquired blepharoptosis and visual field improvement following ptosis surgery. Arch Ophthalmol. 1992;110(1):63-67. [DOI] [PubMed] [Google Scholar]