This study describes the reconstruction of the philtrum in the cross-lip flap transfer using nasolabial muscle tension line group reconstruction.
Key Points
Question
Can a philtrum be completely reconstructed on a partial-thickness cross-lip flap transfer using nasolabial muscle tension line group reconstruction?
Findings
A stable philtrum with philtral ridge and philtral dimple was reconstructed on flaps in 5 of 6 patients. The shape of the philtrum was natural according to the 3-dimensional scan measurement.
Meaning
A complete philtrum structure can be reconstructed by applying muscle tension on the flap.
Abstract
Importance
The blood supply pattern of the partial-thickness musculomucosal pedicle flaps is different from the traditional Abbe flap. The arterial blood supply and venous drainage are highly reliable during clinical practice.
Objective
To describe the reconstruction of the philtrum in the cross-lip flap transfer using nasolabial muscle tension line group reconstruction.
Design, Setting, and Participants
From January 1, 2014, through June 31, 2015, a total of 6 patients with upper lip defect were treated with philtrum reconstruction in the same stage of the split cross-lip flap transfer at the Plastic Surgery Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China. These patients underwent reconstruction of the philtrum by nasolabial muscle tension line group reconstruction. The patients were compared with a randomly chosen group of 5 individuals without upper lip defects by measuring the 3-dimensional scans.
Interventions
In the patient group, the split flap was elevated from the posterior portion of the oris orbicularis muscle after the inferior labial arteries were divided. Then the partial-thickness flap was rotated 180° horizontally and inverted 180° upward to the upper lip defect. The philtrum was reconstructed using the nasolabial muscle tension line group reconstruction.
Main Outcomes and Measures
Three-dimensional scans were performed from the 2-month to 28-month revisits.
Results
A total of 11 individuals were included in the study: 6 in the patient group (mean [SD] age, 17.0 [4.8] years; 2 [33.3%] female and 4 [66.7%] male) and 5 in the control group (mean [SD] age, 15.2 [6.0] years; 2 [40.0%] female and 3 [60.0%] male). In the patient group, 5 of 6 musculomucosal pedicle flaps were viable. A stable philtrum with philtral ridge and philtral dimple was reconstructed on the 5 flaps. The shape of the philtrum was natural according to the 3-dimensional scan measurement. One flap partially necrosed, and the scar retraction was severe postoperatively.
Conclusions and Relevance
The blood supply of the partial-thickness cross-lip flap was from the small vascular network of the lower lip. It is reliable to reconstruct a philtrum in this stage of flap transfer. A complete philtrum structure can be reconstructed by applying muscle tension on the flap.
Level of Evidence
4.
Introduction
Previous reports have detailed an innovative split cross-lip flap technique with a musculomucosal pedicle. The flap is supplied by the vascular network in the submucosal and subcutaneous tissue, which is derived mainly from the horizontal labiomental artery and/or the vertical labiomental artery. This technique was used for 69 patients with upper lip defects from January 1, 2012, through June 31, 2015. Because the flap provided more flexibility and plasticity, favorable results were also achieved in these cases.
The blood supply of the split cross-lip flap was different from that of the traditional inferior labial artery flap. However, arterial blood supply and venous drainage were highly reliable because of the 3-dimensional (3D) architecture of the labiomental vessels. The first reconstruction of the philtrum structure on the partial-thickness cross-lip flap in the same stage of the flap transfer was completed in 2014. A stable philtrum, including philtral ridge and philtral dimple, was reconstructed using nasolabial muscle tension line group reconstruction. Since then, 6 procedures have been performed.
On the basis of the anatomical and biomechanical research of the nasolabial muscles, the concept of the nasolabial muscle tension line group has been proposed in recent years. The muscles involved in the formation of the upper lip include the oris orbicularis, the depressor septi nasi, the alar part of the nasalis, and the levator labii superioris alaeque nasi. The connected muscle fibers in bundles are called tension lines. The tension lines in decussation and progression are called the tension line group. Overall, there are 3 tension line groups: main tension line group, first auxiliary tension line group, and second auxiliary tension line group. These tension line groups are kept in equilibrium to maintain the specific shape and aesthetics of the upper lip and the nose. The shape of the philtrum mainly relies on the second auxiliary tension line group. A previous study reconstructed the philtrum in the repair of microform cleft lip, bilateral cleft lip, and secondary cleft lip.
We combined the techniques of using labiomental artery–supplied cross-lip flap and secondary auxiliary tension line group reconstruction to repair the upper lip defect. The philtrum was simultaneously reconstructed on the split cross-lip flap. Five cases of cross-lip flap with a musculomucosal pedicle were viable. The shape of the philtrum was natural and stable. One case of flap partial necrosis occurred. Because of scar contracture, the scar retraction was severe postoperatively. This article describes the reconstruction of the philtrum in the cross-lip flap transfer using nasolabial muscle tension line group reconstruction.
Methods
From January 1, 2014, through June 31, 2015, a total of 6 patients with midline upper lip defects were treated with split cross-lip flap transfer and philtrum reconstruction at the Plastic Surgery Hospital, Chinese Academy of Medical Science and Peking Union Medical College, Beijing, China. These patients were considered the patient group. In this group, nasolabial muscle tension was applied to the flap to reconstruct the philtrum. Three-dimensional scans were performed on the last revisit from 2 months to 28 months. One case of flap partial necrosis occurred. Because of scar contracture, the philtrum structure was completely destroyed; therefore, it could not be measured. The data from this patient were excluded. To compare the philtrum formation, we randomly chose 5 individuals as the control group by measurement of the 3D scan. The participants in the control group were chosen by random number table method in the 3D scan database from the Plastic Surgery Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China. The patients with upper lip deformities were excluded. The patient group information is listed in eTable 1 in Supplement. The lesions involved mainly the superficial layer, including skin with or without muscle. Mucosa was normal or partially involved. All patients provided written informed consent, and data were deidentified. The study was approved by the Ethical Institutional Committee of the Plastic Surgery Hospital, Chinese Academy of Medical Sciences.
Operative Procedures
The procedure was divided into 2 stages. Cross-lip flap transfer and philtrum reconstruction were generally completed with the patient under local anesthesia in the first stage. After 10 to 12 days, the pedicle was severed with the patient under local anesthesia in the second stage.
Preparation of the Upper Lip Recipient Site
The anatomical landmarks and excision area were marked. The aberrant tissue of the upper lip was excised, including the skin scar and the subcutaneous tissue. Superficial degenerative orbicularis oris muscle was excised if necessary, but the deep layer muscle, submucosa, and mucosa were retained.
Elevation and Transfer of the Partial-Thickness Cross-Lip Flap From the Lower Lip
The split flap was elevated from the deep portion of the oris orbicularis muscle. The flap consisted of skin, subcutaneous tissue, and most of the oris orbicularis muscle. The musculomucosal pedicle consisted of mucosa, submucosa, and a thin layer of muscles. Consequently, the vascular networks were well preserved in the submucosal and subcutaneous tissue. These vascular networks derived from the horizontal labiomental artery and/or the vertical labiomental artery. The incision ended at or slightly below the margin of the wet and dry vermilion mucosa. Bilateral inferior labial arteries and the small branches around them were cut off after electrocoagulation. The cross-lip flap should also be elevated beneath the level of the inferior labial artery. The axial artery was conserved in the pedicle. The partial-thickness flap was then rotated 180° horizontally and inverted 180° upward to the upper lip defect (Video).
Video.
Elevation and transfer of the partial-thickness cross-lip flap from the lower lip.
Philtrum Reconstruction by Reconstruction of the Secondary Auxiliary Tension Line Groups
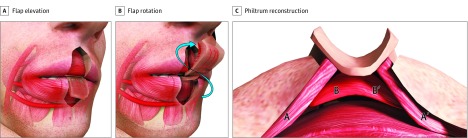
The lateral orbicularis oris muscle flaps A and A′ were dissected from the skin and the mucosa. The medial orbicularis oris muscle flaps B and B′ in the cross-lip flap were dissected from the skin, whereas the skin and muscle kept its connection in the midline. The width of the connection was usually not less than 2 mm, which would preserve the original connection of the skin and the muscle in the philtral dimple. Then the deep layer of the lateral orbicularis oris muscle A and A′ were sutured with the ventral end of the medial orbicularis oris muscle flaps B and B′. The superficial layer of the lateral orbicularis oris muscle A and A′ was sutured to the deep dermis of the philtrum to form a philtral dimple and philtral ridge. As a result, the secondary auxiliary tension line groups were reconstructed in this step (Figure 1 and Figure 2). The skin was sutured in a layer.
Figure 1. Intraoperative Views of the Flap Rotation and Philtrum Construction.
Figure 2. Diagram of the Philtrum Reconstruction by Reconstruction of the Secondary Auxiliary Tension Line Groups.
A and A’ indicate the lateral orbicularis oris muscle flaps; B and B’, the medial orbicularis oris muscle flaps.
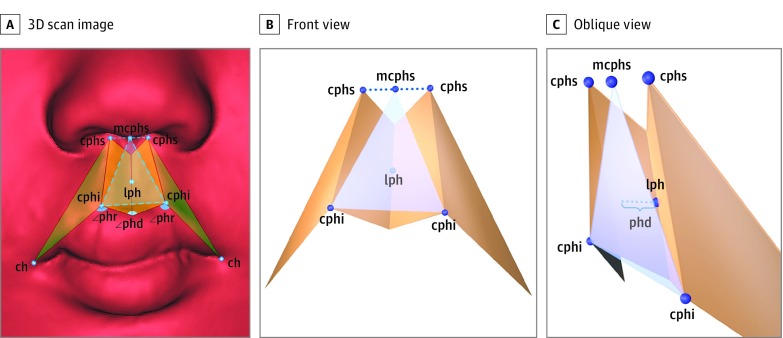
Three-Dimensional Measurement of the Philtrum
The details of the philtrum were measured from 2-month to 28-month follow-up visits by a 3D laser scanner (EVA-S 3D scanner, Artec Europe). We established a method to measure the philtrum on the 3D image. The 3D images were measured using MIMICS software, version 17.0 (Materialise NV) (Figure 3). All statistical analyses were conducted with SPSS statistical software, version 20.0 (IBM Inc). Descriptive statistics included means (SDs) in the individual groups. The independent-sample group 2-tailed, unpaired t test was used to compare means between the patient and control groups. The level of statistical significance was set at P < .05 (2-sided).
Figure 3. Measurements of 3-Dimensional (3D) Scan Image.
Measurements on the 3D scan image (A) and diagrams of the front view (B) and the 45° oblique view (C). cphs-cphi-ch indicates lateral plane of philtrum; cphs-cphi-lph, medial plane of philtrum; lph, lowest point of philtrum; mcphs, midpoint between right cphs and left cphs; mcphs-cphi-cphi, front plane of philtrum; ∠phr, angle of philtrum ridge; ∠phd, angle of philtral dimple; and phd, philtral depth and vertical distance between lph and mcphs-cphi-cphi.
Results
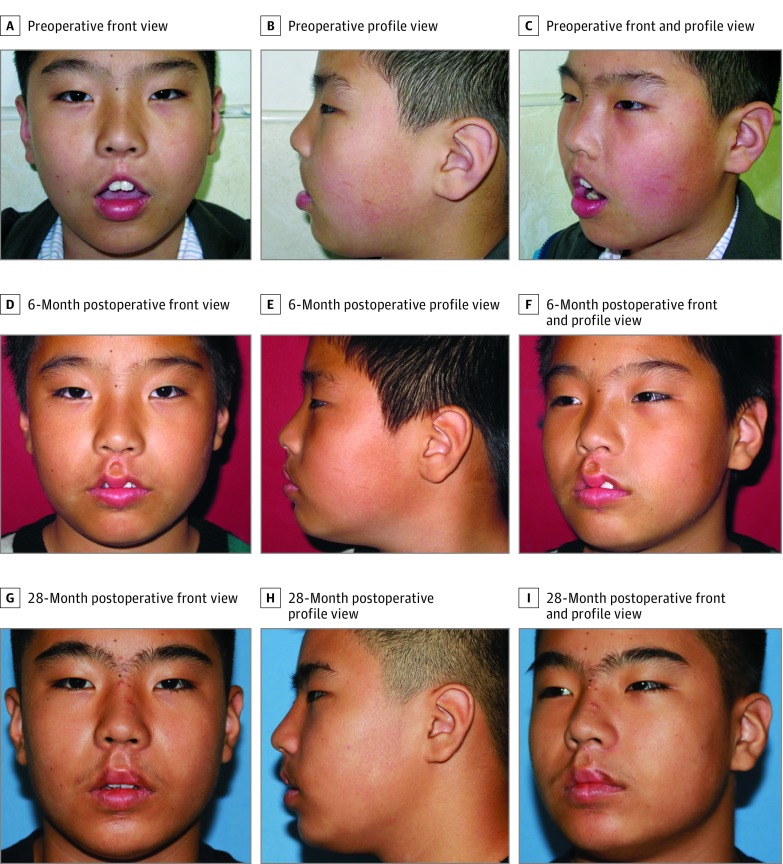
A total of 11 individuals were included in the study: 6 in the patient group (mean [SD] age, 17.0 [4.8] years; 2 [33.3%] female and 4 [66.7%] male) and 5 in the control group (mean [SD] age, 15.2 [6.0] years; 2 [40.0%] female and 3 [60.0%] male). After the first stage, 5 cases of split cross-lip flaps were viable, and 1 flap partially necrosed. In these 5 cases, philtrum structures were constructed completely, including the philtral ridge and the philtral dimple. Patients were satisfied with their appearance. The follow-up period ranged from 2 to 28 months. The shape of the philtrum was natural and stable (Figure 4). The philtrum measurements are given in the Table. No significant difference was found in philtral depth, philtral height, angle of philtral ridge, angle of philtral dimple, and upper prolabial width between the patient and control groups. Therefore, the shape of the philtrum was natural. The inferior point of column to labial fissure was shorter and the lower prolabial width was longer in the patient group, which means the lower part of the flap was wide. The reason for this occurrence might be that the peak of the Cupid’s bow was marked laterally to excise the scar. In addition, 1 case of flap partial necrosis occurred. The patient had a tendency to scar badly; therefore, the scar contraction was severe (eFigure 1 in the Supplement).
Figure 4. A Patient With Upper Lip Defect After Hemangioma Treatment.
Preoperative (A-C) and 6-month postoperative images (D-F) show a stable philtrum structure; a minor revision of the vermillion was performed. G-I, 28-month postoperative images show a natural upper lip.
Table. Philtrum Measurements in the Patient and Control Groups.
| Feature | Measurement | Mean (SD) Philtrum Size, mm | P Value | |
|---|---|---|---|---|
| Control Group | Patient Group | |||
| Philtral depth | phd | 0.93 (0.56) | 1.03 (0.98) | .85 |
| Philtral height (right) | cphi-cphs (right) | 12.70 (2.14) | 12.49 (1.82) | .87 |
| Philtral height (left) | cphi-cphs (left) | 12.91 (2.30) | 12.38 (1.91) | .71 |
| Angle of philtral ridge (right) | ∠phr (right) | 130.44 (8.88) | 127.21 (14.47) | .68 |
| Angle of philtral ridge (left) | ∠phr (left) | 128.57 (10.09) | 125.98 (11.97) | .72 |
| Angle of philtral dimple | ∠phd | 161.31 (12.73) | 161.76 (15.67) | .96 |
| Inferior point of column to labial fissure (right) | ch-cphi (right) | 27.86 (2.20) | 19.33 (2.24) | <.001 |
| Inferior point of column to labial fissure (left) | ch-cphi (left) | 26.41 (2.58) | 18.64 (1.20) | <.001 |
| Lower prolabial width | cphi-cphi | 12.30 (1.65) | 14.85 (1.80) | .048 |
| Upper prolabial width | cphs-cphs | 11.53 (2.05) | 11.25 (1.56) | .82 |
Abbreviations: ch, chelion; cphi, crista philtri inferior; cphs, crista philtri superior; phd, philtral depth; ∠phd, angle of philtral dimple; ∠phr, angle of philtral ridge.
Discussion
Upper lip defects are usually repaired by using adjacent tissue, such as Abbe-Sabattini flap, Estlander flap, Karapandzic flap, and Gillies flap. Procedure selection depends on the location and extent of the defect. If the lesion involves the mucocutaneous junction (white line) and the vermillion, the best donor site is the lower lip. The unique structures cannot be replaced by the other tissue. Therefore, cross-lip flap is the first choice for the defect, involving half to two-thirds of the upper lip. If the defect does not include the commissure, the Abbe-Sabattini flap can be used; if the commissure is involved, the Estlander flap can be used. Tissue that borrows from the opposite lip, well known as the Abbe cross-lip flap, was first described by Sabattini in 1838. The traditional Abbe flap is a full-thickness flap vascularized by the inferior labial arteries. Although various improvements have been made over the years, the supply artery has not changed. Surgeons have attempted to increase the flexibility of the flap so the pedicle around the inferior labial artery would be thinner. However, a thinner pedicle results in venous congestion because a minute venous network surrounds the artery in the submucosa. It is hard to obtain a balance between getting more flexibility and getting better venous drainage.
In 2010, we proposed an innovative partial-thickness cross-lip flap with a musculomucosal pedicle. First, the major difference was the supply arteries. Instead of the inferior labial arteries, the flap was supplied by the vascular network from the horizontal labiomental arteries and/or vertical labiomental arteries. The small arteries and minute arteries formed a 3D vascular network that provided a consistent and sufficient vascular supply to the flap. Second, the venous network in the submucosal layer was maximally conserved in this wide musculomucosal pedicle. The venous drainage was better than that in other methods. The flap rotation was in the axial direction without folding the pedicle, which provided a smooth blood flow. Therefore, the arterial supply and venous drainage were reliable. In some cases, the flap would experience a transient pale period, which usually lasted 2 to 6 hours. The reasons may be that it would take time for the blood flow to change directions and construct a new blood supply pattern after the bilateral inferior labial arteries were cut off.
From an aesthetic aspect, the upper lip had some unique anatomical characteristics, such as the philtrum, curve of the Cupid’s bow, and vermilion tubercle. The preferred result for the upper lip defect repair is filling the gap and reconstructing these fine structures. In some cases, the lower lip has the similar Cupid’s bow and vermilion tubercle; thus, these structures could be imitated. However, the complete philtrum structure, including the philtral dimple and the philtral ridge, are difficult to reconstruct.
Previously, philtrum reconstruction mostly relied on the muscle volume accumulation, such as coronal muscle splitting technique and palmaris longus tendon grafts. We explored the philtrum muscles by examining microscopic anatomic features, reviewing microcomputed tomographic scans, and using the finite element method. We found that the shape of the lip, including the philtrum, depended on balanced muscle tension on both sides instead of muscle volume. The mechanical structure that determined the shape of the philtrum was named the secondary auxiliary tension line group.
Specifically, a branch of the pars peripheralis originated from one side of the modiolus, ran upward and medially, crossed the midline, and inserted into the skin of the philtrum and its lateral areas. Moreover, a branch of levator labii superioris alaeque nasi entered the upper lip from the lateral and top direction, moved inward, and inserted into the dermis inside of the ipsilateral philtral ridge. In the axial plane of the upper lip, the pars peripheralis branch and the levator labii superioris alaeque nasi branch cross each other directionally, and their muscle fibers interact with each other; this region is known as the second auxiliary tension line group. Because the strength of the muscle fibers of the pars peripheralis branch and the levator labii superioris alaeque nasi branch pulled the skin on both sides of the philtral ridge in opposite directions, the bevels perpendicular to the direction of the muscle fibers on both sides were formed, which constituted the contour of the philtral ridge (eFigure 2 in the Supplement).
Therefore, in our procedure, we reconstructed the outline of the philtrum by reconstructing the continuity of the secondary auxiliary tension line group. The orbicularis oris muscle on the lateral side of the defect was divided into 2 layers. The muscle fibers of the deep layer were sutured obliquely to the muscle fibers of the cross-lip flap to simulate the muscle strength of the pars peripheralis branch. The muscle fibers of the superficial layer were sutured obliquely to the subcutaneous tissue of the cross-lip flap to simulate the strength of the levator labii superioris alaeque nasi branch. Then the orbicularis oris muscle on both sides of the philtral ridge formed a cross structure in the 3D space. Under the influence of the strength of the cross structure, the philtral ridge and the philtral dimple were formed.
Philtrum reconstruction by second auxiliary tension line group restoration had achieved good results in primary and secondary repair of cleft lip. With this method, muscle layer is dissected, and tension is added to the skin and muscle; thus, maintaining blood supply in the flap is challenging. The arterial blood supply and venous drainage of the partial-thickness cross-lip flap were reliable during our clinical practice. Even if muscle tension was applied to the flap, the flap might survive. This is the first report, to our knowledge, about philtrum reconstruction on the cross-lip flap.
However, 1 case of flap partial necrosis occurred in a patient with secondary labial defects of bilateral cleft lip. This patient had a tendency to scar badly; thus, the scar retraction was severe postoperatively. The main reason for the severe scar retraction might be that too much muscle tension was added to the flap. To preserve the original connection of the skin and muscle in the philtral dimple, the width of the connection in the midline was usually 2 mm. Because of this case, we recommend that less muscle tension be added to the flap and that the connection is not narrower than 3 mm.
Limitations
This study has some limitations. The case numbers are small, the scar history of the patient should be discussed comprehensively before operation, and the muscle tension added to the flap and the connection conserved should be clarified in a future study.
Conclusions
The partial-thickness cross-lip flap has a completely different blood supply pattern, which is reliable. The philtrum could be reconstructed by secondary auxiliary tension line group reconstruction in the same stage of the flap transfer. This new technique broadened the application of the cross-lip flap and improved the final result of upper lip repair. To achieve the favorable outcome, we should pay close attention to the blood supply of the flap and ensure that proper muscle tension is added to the flap.
eTable. Information of the Patient Group
eFigure 1. A Patient With Secondary Labial Defects of Bilateral Cleft Lip Underwent the Complication of the Necrotic Flap
eFigure 2. Secondary Auxiliary Tension Line Group
References
- 1.Wu D, Song T, Li H, Ma H, Yin N. An innovative cross-lip flap with a musculomucosal pedicle based on the vascular network of the lower lip. Plast Reconstr Surg. 2013;131(2):265-269. [DOI] [PubMed] [Google Scholar]
- 2.Wu D, Wang Y, Song T, et al. Aesthetic reconstruction of the upper lip with novel split musculomucosal-pedicle cross-lip flap. Ann Plast Surg. 2014;73(suppl 1):S88-S91. [DOI] [PubMed] [Google Scholar]
- 3.Yin N, Wu J, Chen B, et al. Muscle tension line concept in nasolabial muscle complex—based on 3-dimensional reconstruction of nasolabial muscle fibers. J Craniofac Surg. 2015;26(2):469-472. [DOI] [PubMed] [Google Scholar]
- 4.Wu J, Yin N. Detailed anatomy of the nasolabial muscle in human fetuses as determined by micro-CT combined with iodine staining. Ann Plast Surg. 2016;76(1):111-116. [DOI] [PubMed] [Google Scholar]
- 5.Wu J, Yin N. Anatomy research of nasolabial muscle structure in fetus with cleft lip: an iodine staining technique based on microcomputed tomography. J Craniofac Surg. 2014;25(3):1056-1061. [DOI] [PubMed] [Google Scholar]
- 6.Bo C, Ningbei Y. Reconstruction of upper lip muscle system by anatomy, magnetic resonance imaging, and serial histological sections. J Craniofac Surg. 2014;25(1):48-54. [DOI] [PubMed] [Google Scholar]
- 7.Yin N, Song T, Wu J, et al. Unilateral microform cleft lip repair: application of muscle tension line group theory. J Craniofac Surg. 2015;26(2):343-346. [DOI] [PubMed] [Google Scholar]
- 8.Coppit GL, Lin DT, Burkey BB. Current concepts in lip reconstruction. Curr Opin Otolaryngol Head Neck Surg. 2004;12(4):281-287. [DOI] [PubMed] [Google Scholar]
- 9.Sabattini P. Rinoplastica e Cheiliplastica operate sopra un solo individuo. Bull Sci Med (Bologna). 1838;10:387. [Google Scholar]
- 10.Hu H, Song R, Sun G. One-stage inferior labial flap and its pertinent anatomic study. Plast Reconstr Surg. 1993;91(4):618-623. [DOI] [PubMed] [Google Scholar]
- 11.Millard DR Jr, McLaughlin CA. Abbe flap on mucosal pedicle. Ann Plast Surg. 1979;3(6):544-548. [DOI] [PubMed] [Google Scholar]
- 12.Kim S, Kwon J, Kwon GY, Choi TH. Dynamic reconstruction of the philtrum using coronal muscle splitting technique in microform cleft lip. J Craniofac Surg. 2014;25(3):742-745. [DOI] [PubMed] [Google Scholar]
- 13.Lim AA, Allam KA, Taneja R, Kawamoto HK. Constructing the philtral column in the secondary cleft lip deformity: utilizing the palmaris longus graft. Ann Plast Surg. 2013;70(3):296-300. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Information of the Patient Group
eFigure 1. A Patient With Secondary Labial Defects of Bilateral Cleft Lip Underwent the Complication of the Necrotic Flap
eFigure 2. Secondary Auxiliary Tension Line Group