Abstract
Stress plays a central role in the development and persistence of psychosis. Network analysis may help to reveal mechanisms at the level of the micro-dynamic effects between stress, other daily experiences and symptomatology. This is the first study to examine time-lagged networks of the relations between minor daily stress, momentary affect/thoughts, psychotic experiences, and other potentially relevant daily life contexts in individuals varying in risk for psychosis. Intensive longitudinal data were obtained through 6 studies. The combined sample consisted of 654 individuals varying in risk for psychosis: healthy control subjects (n = 244), first-degree relatives of psychotic patients (n = 165), and psychotic patients (n = 245). Using multilevel models combined with permutation testing, group-specific time-lagged network connections between daily experiences were compared between groups. Specifically, the role of stress was examined. Risk for psychosis was related to a higher number of significant network connections. In all populations, stress had a central position in the network and showed direct and significant connections with subsequent psychotic experiences. Furthermore, the higher the risk for psychosis, the more variables “loss of control” and “suspicious” were susceptible to influences by other network nodes. These findings support the idea that minor daily stress may play an important role in inducing a cascade of effects that may lead to psychotic experiences.
Keywords: network analysis, minor daily stress, psychosis, experience sampling method, first-degree relative
Introduction
Minor Daily Stress and Psychosis
Stress plays a central role in the development and persistence of psychosis.1–5 Recently, studies have focused on minor stressors in the realm of daily life and their dynamic associations with affect and psychotic experiences,6 using ecological assessment strategies such as the Experience Sampling Method (ESM).7 These ESM studies found minor daily stress to be associated with an increase in both negative affect and momentary psychotic experiences in patients with psychosis, and in individuals with a familial or psychometric risk for developing a psychosis.8–10 Increased sensitivity to minor daily stress has been proposed to be a vulnerability marker for the development of psychotic symptoms.11 To date, it has remained relatively unclear, if stress acts directly upon experiences or if the association relies on more complex dynamics. According to the “affective pathway” theory, minor daily stress possibly impacts on psychosis through altered affective responses.11 Indeed, increases in anxiety have been found to precede the increase of paranoia,12 and such dynamic interplay of momentary affect and paranoia was also found to be associated with the development and course of psychotic experiences.13 Furthermore, Reininghaus and colleagues found elevated emotional reactivity to minor stress to be associated with more intense psychotic experiences in daily life.14 Overall, it is apparent that the interplay between minor daily stress, affect, and psychosis is complex and dynamic and requires analytic strategies that move beyond a classic predictor-response approach.
The Network Approach
Recently, a network approach to psychopathology has been proposed as a valuable alternative to the more traditional latent construct perspective.15–18 It posits that mental disorders are best understood as dynamic networks of smaller entities (eg, symptoms or affective states displayed as nodes) that cluster together and interact with each other over time.19,20
Applying the network approach to fine-grained ESM data may provide a better understanding of dynamic interrelations between momentary affective states (eg, feeling anxious or cheerful). A number of recent studies have visualized the dynamic associations between momentary affective states,20–22 suggesting that the activation of one affective state can simultaneously activate other affective states. Furthermore, individuals with a mental disorder showed more direct connections between momentary affective states compared to healthy controls.22,23 It can be speculated that when affective states repeatedly reinforce each other over time, vicious cycles may ensue, from which it gets increasingly difficult to escape.23,24 Experiences of minor daily stress are hypothesized to put in motion or maintain such vicious cycles. From a network point of view, a stressor may be able to trigger a whole cascade of other experiences or behavioral changes15,24 relevant to the eventual development of psychotic experiences by activating one of the strongly connected nodes in the network.
In order to examine these relationships, we first require temporal data to estimate networks in which we can visualize which experiences precede other experiences over time. ESM data are very suitable for this purpose. Second, to examine whether the proposed micro-level dynamics play a role in psychosis, comparisons need to be made between groups with different levels of risk for psychosis. Third, as stress and other relevant contextual factors may play an important role in these dynamics, we need to create networks incorporating not only affective and psychotic experiences, but also incorporate measurements representing stress, current thoughts, as well as various situational characteristics.
In the current study, we aim to examine the dynamic interplay between minor daily stress, momentary affect/thoughts, psychotic experiences, and other potentially relevant daily life contexts. For this purpose, we created dynamic networks using combined data from 6 ESM studies in controls, first-degree relatives of patients with psychotic disorder, and patients with psychotic disorder. Permutation testing procedures (comparable to the Network Comparison Test [Van Borkulo CD, Woldorp LJ, Boschloo L, et al. Comparing network structures on three aspects: a permutation test (in preparation).]) were then used to test for differences in the network connections between these 3 groups.
Methods
Samples
We used data from 6 different studies10,25–28 (see supplementary table S1 for inclusion and exclusion criteria of these studies) that used a similar ESM protocol. Participants were classified either as (1) “healthy” control individuals (ie, neither a personal diagnosis nor a family history of psychotic disorder/symptoms), (2) first-degree relatives of individuals with a psychotic disorder, or (3) individuals with a psychotic disorder.
All studies included in this paper were approved by the local medical ethics committee. All further procedures and analyses were performed according to the ethical standards formulated by this committee.
Experience Sampling Method
In all studies, ESM (a structured diary technique) was used to study minor stress in everyday life (table 1). Individuals received a diary and a wristwatch which was programmed to beep 10 times a day (between 7:30 AM and 10:30 PM) for 5 (Aripiprazol study26) or 6 days (remaining studies) at semi-random intervals (random within 90-min time frames). Thus, the time lag between the measurements was, on average, approximately 90 minutes. Information on the ESM can be found elsewhere.29,30
Table 1.
ESM Procedurea and Measures of Stress, Affect, Psychotic Experiences, and Context
| Variable Name | ESM Measures | Rating | |
|---|---|---|---|
| Minor daily stress | Stress | “Think about the most important event since the last beep. This event was…” | Rated on a 7-point bipolar scale (−3 “very unpleasant,” 0 “neutral,” 3 “very pleasant”). Positive scores indicated the absence of an unpleasant event since the last beep, which means that there was no stressor present. Therefore these scores (0, 1, 2, and 3) were coded as 0 “neutral”. Negative scores implicated the presence of an unpleasant event, which means that there was a stressor present. To let high scores reflect more stress, these negative scores were recoded (−3 = 3, −2 = 2, −1 = 1). |
| Affect | Cheerful | “I am cheerful” | Rated on a 7-point Likert scale ranging from 1 (“not at all”) to 7 (“very”). |
| Relaxed | “I feel relaxed” | ||
| Insecure | “I feel insecure” | ||
| Anxious | “I feel anxious” | ||
| Irritated | “I feel irritated” | ||
| Down | “I feel down” | ||
| Psychotic experiences | Suspicious | “I feel suspicious” | Rated on a 7-point Likert scale ranging from 1 (“not at all”) to 7 (“very”). |
| Loss of control | “I am afraid to lose control” | ||
| Cognitive, physical, and contextual aspects | Pleasant thoughts | “I have pleasant thoughts” | Rated on a 7-point Likert scale ranging from 1 (“not at all”) to 7 (“very”). |
| Tired | “I am tired” | ||
| Active | “I am currently doing […]. I am actively engaged in this activity” | Choice of different of activities that is followed by a question on how actively engaged the individual is in this particular activity. This item is rated on a 7-point Likert scale ranging from 1 (“not at all”) to 7 (“very”). Only the rating of engagement was included in the current analyses. | |
| Alone | Alone | “Who am I with” | Choice of different categories for social company (eg, with partner, with friend, etc.). Based on answer, dichotomous variable “alone” was generated with 0 “not alone” and 1 “alone”. |
Note: aESM procedure: Individuals received a diary and a wristwatch which was programmed to beep 10 times (from 7:30 AM to 10:30 PM) a day for 5 (Aripiprazol study26) or 6 days (remaining studies) at semi-random intervals (random within 90-min time blocks). At each prompt, participants were asked to stop their activity and to fill in a short questionnaire including the above items. Prior to the assessment period, participants were provided with detailed instructions during a short training session. The ESM assessment period started on any day of the week, usually 1 day after the training session. Participants were at least contacted once during the assessment period, to assess instruction adherence, identify concerns or problems with the method and in order to maximize the number of observations. Participants had to provide valid responses to at least one-third of the beep signals to be included in the analyses of the current study.
ESM Measures
We selected 13 ESM items for our analyses based on the following criteria: (1) all variables had to be assessed in all 6 ESM studies, (2) the selected variables needed to capture different aspects relevant to psychosis, and (3) the variables had to have a considerable within-person variability over measuring points. This resulted in the following variables: “minor daily stress” (hereafter called “stress”), “cheerful,” “relaxed,” “insecure,” “anxious,” “irritated,” “down,” “suspicious,” “loss of control,” “pleasant thoughts,” “tired,” “active,” and “alone”. “Stress” was assessed with the item “Think about the most important event since the last beep. This event was…” This item was rated on a 7-point bipolar scale (−3 “very unpleasant,” 0 “neutral,” 3 “very pleasant”). Positive scores (0, 1, 2 and 3) were coded as 0 “neutral” and all negative scores were recoded (−3 = 3, −2 = 2, −1 = 1) so that high scores reflect stress. This item has been used widely to assess minor daily stress31–33 and its convergent validity31 as well as its association with physiological stress response has been reported previously.34 More information on the included variables is presented in table 1.
Range of Variables.
To make model coefficients more directly comparable, all variables (with the exception of “alone”) were transformed to range between 0 and 1 before the analyses (with , where is the jth observation of the ith individual and and are the theoretically lowest and highest possible scores on the variable, so that 0 corresponding to the lowest possible score on the variable and 1 corresponding to the highest possible score). Since “alone” was assessed on a dichotomous scale, a transformation of this variable was not necessary.
Analyses
Given the hierarchical structure of ESM data (with multiple observations nested within individuals), multi-level (mixed-effects) regression models were used. In line with previous work, we used VAR-specified multilevel models to obtain regression coefficients that would serve as estimates for network connection strengths between nodes (eg, momentary experiences).21 This means that for each group of participants, 13 models were fitted, where each variable once served as the dependent variable in turn. The time-lagged values of all 13 variables (eg, lag one, at one beep earlier) served as covariates/predictors in the model, so that each variable at time t was predicted by all 13 variables at t−1 simultaneously.21 The lags in the current study had an average distance of 90 minutes. The predictor variables were person-mean centered prior to the analyses. Since we were interested in the temporal relationships of the variables within a day, the first beep on each day was excluded from the analyses. To account for any time trends in the outcome variables, time was included as a covariate. All analyses were controlled for age and gender.
To allow observations from the same individual to be correlated, random intercepts at the individual level were included. Moreover, time trends in ESM data are assumed to differ systematically per individual, and we therefore allowed slopes of the time variable to differ randomly across individuals (with random intercepts and slopes allowed to be correlated). For reasons to be outlined further below, we did not model random slopes for the remaining predictors.
Since “alone” was assessed dichotomously, we used logistic mixed-effects regression models when this variable served as the outcome variable. For the 12 remaining variables, we used standard linear mixed-effects models. The analyses were carried out using R, version 3.2.1 using the nlme35 and lme436 packages for the standard and logistic mixed-effects models, respectively.
Significant Network Connections.
Group networks were generated based on significant regression coefficients (fixed effects with a corresponding 2-side P-value < .05).37 Since the associations between predictors and outcomes are likely to differ across individuals, it would have been preferable to add random effects for all regression coefficients. Since this would result in models that are too complex for our dataset, we opted for models with random intercepts and random slopes only for the time variable. While regression coefficients themselves are then still unbiased estimates, the standard errors of the coefficients (and hence P-values) from the models are not trustworthy. To obtain accurate P-values and thus identify significant network connections, we used a permutation procedure38 with 10 000 iterations to conduct the tests of the coefficients (supplementary text S1).
Variable “alone”.
Using logistic regression multilevel models for the outcome variable “alone” would result in networks containing coefficients which are not directly comparable in magnitude. Since linear models for this outcome yielded similar P-values (and identical conclusions) as the logistic models, the linear coefficients from these models were the ones used in the computation of network measures.
Comparison of Group Networks
Specific Paths Differences.
Significant differences in magnitude (P < .05) of specific paths (eg, regression coefficients) between groups (supplementary materials) were tested with a permutation procedure.
Differences in Average Network Connectivity.
The average whole network connectivity was computed based on all absolute network connection strengths in a network. Network connectivity represents the ease with which the activation of nodes triggers the activation of other nodes in the network. A higher average whole network connectivity means that in the first network activation of nodes is more easily spread throughout the network producing a cascade of changes in the activity of all the network nodes. Furthermore, we also split the measure of whole network connectivity in average internode connectivity and average self-loop strength. The first measure is based on all connection strengths that run between different nodes in the network. The second measure is based on all connection strengths that are present within each node. The latter connections are also called “self-loops” or “autocorrelations”.21,39
Network Centrality.
Centrality characteristics are based on all network connections and were computed using the “qgraph” package.37Inward and outward strength were calculated by adding the absolute weights of all the respectively incoming and outgoing connections (not including self-loops) per node in the network. The higher the outward strength, the stronger the influence the node exerts directly on other nodes in the network. Therefore, hypothetically, alterations in the activity of a node with a high outward strength can thus easily lead to changes in the activity of the other nodes as well. The inward strength of a node gives insight into the extent that a node is influenced directly by other nodes. Finally, nodes with a high betweenness centrality are situated on a high number of shortest paths between other nodes. For example, it can be imagined that the shortest path for stress to influence a node representing a psychotic experience, is by first activating nodes of negative affective states. If many shortest paths run through the latter nodes then these are said to have a high betweenness centrality. In our particular case, connections with higher weights are shorter. Shortest paths are therefore determined by taking the inverse of absolute connection weights.
Results
Basic Sample Characteristics
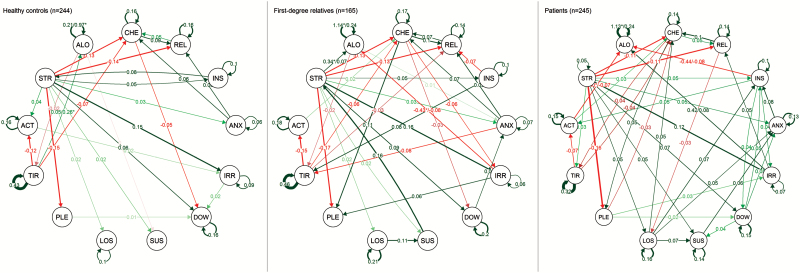
Demographic information and mean levels of ESM items are presented in table 2. Patients differed significantly in their means from controls and relatives on all ESM measures (all P < .05), except for “pleasant thoughts” and “active”. Controls and relatives did not show significant differences on ESM measures. Figure 1 shows network visualizations for controls, first-degree relatives, and patients.
Table 2.
Sample Characteristics per Group
| Controls | First-Degree Relatives | Patients With Psychosis | |
|---|---|---|---|
| N | 244 | 165 | 245 |
| Mean age (SD) | 36.5 (12.3) | 36.8 (12.6) | 35.3 (10.8) |
| Age range | 16–64 | 16–63 | 17–64 |
| Gender | |||
| Male (%) | 111 (44) | 68 (41) | 111 (46) |
| Female (%) | 132 (56) | 97 (59) | 132 (54) |
| Mean (SD) level of ESM measures | |||
| Stress | 0.21 (0.21) | 0.21 (0.21) | 0.27 (0.35) |
| Cheerful | 5.10 (0.76) | 5.08 (0.91) | 4.28 (1.11) |
| Anxious | 1.15 (0.29) | 1.20 (0.50) | 1.70 (0.91) |
| Irritated | 1.49 (0.49) | 1.51 (0.52) | 1.91 (0.95) |
| Relaxed | 5.23 (0.73) | 5.17 (0.86) | 4.56 (1.05) |
| Insecure | 1.30 (0.44) | 1.38 (0.63) | 1.99 (0.99) |
| Down | 1.30 (0.47) | 1.35 (0.64) | 1.94 (1.02) |
| Suspicious | 1.08 (0.19) | 1.07 (0.31) | 1.65 (1.05) |
| Loss of control | 1.06 (0.22) | 1.05 (0.20) | 1.56 (1.06) |
| Tired | 2.51 (0.95) | 2.51 (1.05) | 2.86 (1.13) |
| Pleasant thoughts | 4.30 (0.68) | 4.42 (0.72) | 4.36 (0.91) |
| Active | 3.65 (1.07) | 3.66 (1.05) | 3.58 (1.20) |
| Alone | 0.35 (0.17) | 0.37 (0.18) | 0.45 (0.24) |
Note: ESM, Experiences Sampling Method. Patients differed significantly in their means from healthy controls and relatives on all ESM measures (all P < .05), except for “pleasant thoughts” and “active”. Healthy controls and relatives did not show significant differences on ESM measures.
Fig. 1.
Graphic display of significant connections for healthy controls, first-degree relatives and patients. Arrows represent the strength of the connections between any 2 pairs of ESM measures (one measure at time t−1 and the other at time t, equal to a distance of approx. 90 min.). Darker lines represent stronger connections, the more faded the edges the weaker the connection. Connections marked with an asterisk (*) represent log-odd coefficients (corresponding linear coefficient is presented in line). CHE, cheerful; REL, relaxed; INS, insecure; ANX, anxious; IRR, irritated; DOW, down; SUS, suspicious; LOS, loss of control; PLE, pleasant thoughts; TIR, tired; ACT, active; STR, stress; ALO, alone.
Specific Path Differences
Minor Daily Stress.
Compared to relatives and controls, patients showed a stronger connection from “stress” to feelings of “suspiciousness” and “loss of control” (table 3). Relatives also showed a stronger connection than controls from “suspicious” to “stress”. Controls showed a stronger connection from “stress” to “active” than both patients and relatives. For them, when feeling more “stress” one moment they are more “active” the next. In contrast, in patients and relatives “stress” at t−1 was associated with being less “active” at t.
Table 3.
Significant Path Differences Between Controls and First-Degree Relatives, Controls and Patients, and First-Degree Relatives and Patients
| Differences | Coefficients | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Path | Controls vs First-Degree Relatives | Controls vs Patients | First-Degree Relatives vs Patients | Healthy Controls | First-Degree Relatives | Patients | ||||||
| Difference | P | Difference | P | Difference | P | B | P | B | P | B | P | |
| Stresst−1 → activet | 0.057 | .025 | 0.060 | .009 | 0.003 | .933 | 0.040 | .020 | −0.018 | .398 | −0.020 | .206 |
| Stresst−1 → loss of controlt | 0.002 | .899 | −0.037 | .006 | −0.035 | .018 | 0.017 | .000 | 0.017 | .000 | 0.053 | .000 |
| Stresst−1 → suspicioust | 0.004 | .801 | −0.028 | .031 | −0.032 | .026 | 0.023 | .004 | 0.019 | .000 | 0.051 | .000 |
| Tiredt−1 → activet | 0.032 | .305 | −0.052 | .062 | −0.084 | .007 | −0.121 | .000 | −0.153 | .000 | −0.069 | .000 |
| Tiredt−1 → tiredt | −0.032 | .372 | 0.103 | .001 | 0.136 | .000 | 0.426 | .000 | 0.458 | .000 | 0.322 | .000 |
| Irritatedt−1 → alonet | 0.405 | .152 | −0.446 | .077 | −0.851 | .002 | −0.029 | .882 | −0.435 | .031 | 0.416 | .011 |
| Relaxedt−1 → cheerfult | −0.022 | .430 | −0.050 | .039 | −0.028 | .285 | 0.046 | .001 | 0.068 | .000 | 0.096 | .000 |
| Relaxedt−1 → downt | 0.019 | .327 | 0.035 | .041 | 0.016 | .393 | 0.008 | .417 | −0.011 | .412 | −0.027 | .074 |
| Relaxedt−1 → loss of controlt | −0.016 | .254 | 0.026 | .031 | 0.041 | .003 | −0.004 | .253 | 0.011 | .076 | −0.029 | .006 |
| Insecuret−1 → downt | −0.031 | .275 | −0.054 | .033 | −0.024 | .400 | −0.013 | .425 | 0.017 | .433 | 0.041 | .021 |
| Loss of controlt−1 → irritatedt | −0.140 | .040 | −0.058 | .369 | 0.082 | .228 | −0.083 | .070 | 0.057 | .349 | −0.025 | .349 |
| Loss of controlt−1 → tiredt | −0.130 | .034 | −0.033 | .547 | 0.096 | .126 | −0.053 | .343 | 0.077 | .277 | −0.019 | .483 |
| Loss of controlt−1 → stresst | −0.151 | .040 | −0.039 | .566 | 0.112 | .124 | −0.053 | .425 | 0.099 | .281 | −0.014 | .789 |
| Suspicioust−1 → stresst | −0.188 | .008 | −0.057 | .371 | 0.131 | .068 | −0.032 | .498 | 0.156 | .048 | 0.025 | .466 |
| Alonet−1 → suspicioust | −0.007 | .055 | −0.008 | .018 | 0.000 | .893 | −0.005 | .008 | 0.003 | .126 | 0.004 | .376 |
Note: Representation of significant (P < .05) path differences between controls and first-degree relatives, controls and patients, and first-degree relatives and patients. Significant differences are presented in bold. Corresponding coefficients for paths on the left are displayed on the right hand side of the table.
Negative Experiences and Symptomatology.
Patients differed significantly from relatives in their connection from irritated to alone. Relatives were less often alone, whereas patients were more often alone the moment following feeling irritated. Patients showed a stronger positive connection from “insecure” to “down” than both controls and relatives. Furthermore, patients showed a significantly stronger negative association than controls in their connection from “relaxed” to “down” and from “relaxed” to “loss of control”. Also, in controls feelings of “loss of control” were followed by increases in feeling “irritated,” “stress,” “tired” the next moment, which was not the case in relatives.
Positive Experiences.
In patients feeling relaxed was more strongly followed by feeling cheerful than in controls. Patients also had a stronger negative connection from tired to active than relatives. Feeling more tired one moment was associated with being less active the next moment. All 3 groups, however, showed similar self-loops of “cheerful” and “relaxed” as well as comparable connections from “active” to “cheerful” (figure 1).
Centrality Measures
The number of significant connections increased with higher risk for psychosis. The network of patients showed 49, the network of relatives 41, and the network of healthy controls 34 significant connections.
However, we did not find significant differences in average whole network connectivity (controls vs relatives: difference = 0.007, P = .106; controls vs patients: difference = 0.002, P = .457; relatives vs patients: difference = 0.005, P = .349). Also, the networks did not differ significantly in average internode connectivity (controls vs relatives: difference = 0.007, P = .158; controls vs patients: difference = 0.001, P = .564; relatives vs patients: difference = 0.005, P = .383), nor did they differ in average self-loop strength (controls vs relatives: difference = 0.018, P = .223; controls vs patients: difference = 0.010, P = .471; relatives vs patients: difference = 0.008, P = .567).
Minor Daily Stress.
In all 3 networks, “stress” was the most central node in terms of outstrength when compared to the remaining nodes of the network, with an outstrength at least twice as large (table 4). In controls and relatives “stress” had the highest betweenness centrality. The outstrength of “stress” exceeded the instrength in all 3 groups. The total outstrength of “stress” was similar for all 3 groups, while the instrength was highest in relatives.
Table 4.
Centrality Measures for Each Group
| Stress | Cheerful | Relaxed | Insecure | Anxious | Irritated | Down | Suspicious | Loss of Control | Pleasant | Tired | Active | Alone | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Controls | |||||||||||||
| Instrength | 0.33 | 0.45 | 0.46 | 0.26 | 0.15 | 0.4 | 0.26 | 0.12 | 0.07 | 0.41 | 0.21 | 0.47 | 0.32 |
| Outstrength | 0.83 | 0.37 | 0.15 | 0.27 | 0.44 | 0.16 | 0.27 | 0.28 | 0.57 | 0.12 | 0.30 | 0.08 | 0.06 |
| Betweenness | 48 | 45 | 0 | 7 | 1 | 5 | 19 | 0 | 0 | 0 | 11 | 0 | 1 |
| Self-loop | 0 | 0.16 | 0.16 | 0.1 | 0.06 | 0.09 | 0.16 | 0.06 | 0.1 | 0.01 | 0.43 | 0.16 | 0.21 |
| First-degree relatives | |||||||||||||
| Instrength | 0.42 | 0.47 | 0.51 | 0.23 | 0.22 | 0.38 | 0.30 | 0.17 | 0.12 | 0.58 | 0.49 | 0.42 | 0.62 |
| Outstrength | 0.90 | 0.51 | 0.26 | 0.30 | 0.42 | 0.28 | 0.36 | 0.73 | 0.46 | 0.12 | 0.36 | 0.14 | 0.08 |
| Betweenness | 52 | 29 | 3 | 0 | 4 | 1 | 11 | 2 | 1 | 0 | 20 | 0 | 10 |
| Self-loop | 0.02 | 0.17 | 0.14 | 0.1 | 0.07 | 0.06 | 0.2 | 0.06 | 0.21 | 0.01 | 0.46 | 0.18 | 0.24 |
| Patients | |||||||||||||
| Instrength | 0.18 | 0.44 | 0.38 | 0.34 | 0.29 | 0.33 | 0.30 | 0.25 | 0.20 | 0.43 | 0.16 | 0.25 | 0.62 |
| Outstrength | 0.84 | 0.30 | 0.32 | 0.31 | 0.35 | 0.26 | 0.36 | 0.36 | 0.39 | 0.14 | 0.27 | 0.17 | 0.05 |
| Betweenness | 24 | 40 | 13 | 7 | 1 | 3 | 4 | 1 | 2 | 0 | 11 | 0 | 0 |
| Self-loop | 0.05 | 0.14 | 0.14 | 0.1 | 0.13 | 0.07 | 0.15 | 0.14 | 0.16 | −0.01 | 0.32 | 0.15 | 0.24 |
Negative Experiences and Symptomatology.
In controls and relatives, “loss of control” showed overall high levels of outstrength in comparison to other nodes. There was a positive dose-response association of risk for psychosis and instrength of “anxious,” “suspicious” and “loss of control”. “Down” was the most central node in terms of betweenness centrality in controls and relatives, but not in patients. In relatives and patients “alone” showed a much higher instrength than in controls.
Positive Experiences.
In all 3 groups, “cheerful,” “relaxed,” and “pleasant thoughts” showed high levels of instrength. Also, the level of instrength of these items exceeded the level of outstrength. There was a dose response association of increasing risk for psychosis with a lower instrength on “active”. “Cheerful” was among the nodes with the highest betweenness centrality in all 3 groups.
Discussion
This is the first study to use a dynamic network approach to examine the differences in moment-to-moment time-lagged associations between minor daily stress, momentary affect/thoughts, psychotic experiences, and other potentially relevant daily life contexts in individuals belonging to 3 samples with varying risk for psychosis.
We found that groups with a higher risk for psychosis had networks in which more nodes were strongly connected with each other, as can be concluded from the number of significant network connections in these 3 groups. We further found that experiencing higher levels of minor daily stress led to a stronger increase in feeling “suspicious” and “loss of control” in patients compared to controls and relatives. Finally, the higher the risk for psychosis the more variables “anxious,” “suspicious” and “loss of control” were likely to be activated by other network nodes.
Affective Pathway to Psychosis
The current findings provide further insight into the complex link between minor daily stress, affect, and psychotic experiences. Based on previous findings, showing that a higher risk for psychosis is associated with alterations in affect,10 increased stress-sensitivity,13 and affective dysregulation, an “affective pathway” to psychosis had been postulated.11 The dynamic networks in the current study support this theory as the findings suggest that minor daily stress and psychotic experiences may be linked through a multitude of temporal network connections that pass through nodes representing common, frequently experienced, affective states. We observed that in all 3 groups daily stress has a central position and connects directly to many other mental states and contextual factors. Due to this position, changes in minor daily stress may go hand in hand with changes in the transfer between numerous other mental states. The 3 networks showed similar numbers of direct connections of minor daily stress with other mental states. However, the actual impact of minor daily stress on other nodes, including psychotic experiences, may be stronger in people with risk for psychosis as a higher number of connections may spread the impact of stress in the network further.
The theory regarding the affective pathway to psychosis suggests that minor daily stress impacts on psychotic experiences via feelings of anxiety12 and negative affect.13,40 In the network of patients, connections suggested that the negative affect item “down” had an intermediary position between minor daily stress, psychotic experiences, and other mental states (such as “insecure” and “anxious”). Anxiety was not directly connected to psychotic experiences but based on the reported network connections that link anxiety with other negative affective experiences we can hypothesize that anxiety may be connected to psychotic experiences through moods such as “down” and “insecure”.
This suggests that subclinical psychotic experiences may be activated by changes in affective states and that this may happen much more easily in some individuals than in others, depending on differences in network structure. It also generates the hypothesis that stress may not only directly influence psychotic experiences, but that stress-induced alterations in other nodes—such as affect states—may play a crucial role in propagating the impact of stress to psychotic experiences in those people at risk.
Network Connectivity and Risk
The finding that the number of significant network connections increased with risk for psychosis is in line with theories on the relationship between network connectivity and risk in the field of psychiatry. It may support the notion that the complex dynamical system theory can be applied to mental disorders. In complex dynamical system theory, networks with a large number of inter-node connections are hypothesized to be rather rigid and less resilient to effects of stressors.41,42 This makes sense as in such a strongly connected network a single trigger (stressor) that activates a first node of the network will easily cause a cascade of changes in the system as the initial impact is easily transferred to other nodes in the network.20 Recent empirical studies add to this hypothesis22,43 by showing that higher levels of mental state network connectivity were indeed associated with higher levels of (risk for) psychopathology.
Our findings may therefore be compatible with the idea that vulnerability arises because mental states “infect” each other and to a stronger extent in individuals at risk for psychosis. However, we did not find a significant difference in the strength of the overall network connections between the 3 groups; only in the number.
Methodological Issues
First, differing group variances in network nodes could create a problem when comparing the network connectivity between groups. As expected, means did not differ between relatives and controls. It therefore seems unlikely that differences in connection strengths between these latter groups could be attributed to differences in variances. Some means, though, were higher in the patient group than in the other groups. This was unavoidable as patients score, of course, higher on certain symptom measures.
Permutation procedures were necessary to obtain reliable coefficients in these complex analyses. However, CIs are not provided in the current article as it is computationally extremely demanding to obtain those when using permutation procedures. Also, results should be interpreted with caution as we cannot exclude the presence of type I or II errors.
While it is an important strength that the current study used data from a large pooled dataset with ESM measurements of a total of 654 participants (total of 28 466 filled in time points), combining data from 6 different studies may also come with possible disadvantages. First, the above described variable selection only allowed for 2 psychosis items to be included in the current study. Second, medication status was not available for all included studies, and therefore, we cannot exclude the possibility that use of anti-psychotics obscured some of the network dynamics of patients. This would have likely resulted in a too conservative estimation of total network connectivity in the patient group.
Last, the current study used group average estimates. A natural progression of this work is to use the data to create personalized networks based on data of individual patients. This requires datasets with even more measurements per individual. Such personalized networks are an opportunity to derive personalized precision that may help in targeting specific individual needs.
Conclusion
Evidence that psychopathology can be described as a complex network of interacting nodes is accumulating. The current study provides novel support for this idea since we found a dose-response association between the number of significant network connections and risk for psychosis. Clinical interventions able to specifically target mental state cascades and reduce connection strengths in the network may prove valuable.
Supplementary Material
Supplementary data are available at Schizophrenia Bulletin online.
Funding
This work was supported by a supported by a VENI Grant to U.R. (NWO; no. 451-13-022), by an ERC Consolidator Grant (ERC-2012-StG, project 309767—INTERACT) to I.M-G., and by an Aspasia Grant (NWO) and ERC Consolidator Grant (ERC-2015-CoG, Project 681466—TRANS-ID) to M.W.
Supplementary Material
Acknowledgments
Members of MERGE (alphabetical order): D. Collip, Ph. Delespaul, C. Henquet, M. Janssens, M. Lardinois, J. Lataster, M. Van Nierop, M. Oorschot, C. Simons, and V. Thewissen. The authors have declared that there are no conflicts of interest in relation to the subject of this study.
References
- 1. Lardinois M, Lataster T, Mengelers R, Van Os J, Myin-Germeys I. Childhood trauma and increased stress sensitivity in psychosis. Acta Psychiatr Scand. 2011;123:28–35. [DOI] [PubMed] [Google Scholar]
- 2. Read J, van Os J, Morrison AP, Ross CA. Childhood trauma, psychosis and schizophrenia: a literature review with theoretical and clinical implications. Acta Psychiatr Scand. 2005;112:330–350. [DOI] [PubMed] [Google Scholar]
- 3. van Os J, Linscott RJ, Myin-Germeys I, Delespaul P, Krabbendam L. A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychol Med. 2009;39:179–195. [DOI] [PubMed] [Google Scholar]
- 4. Walker E, Mittal V, Tessner K. Stress and the hypothalamic pituitary adrenal axis in the developmental course of schizophrenia. Annu Rev Clin Psychol. 2008;4:189–216. [DOI] [PubMed] [Google Scholar]
- 5. Zubin J, Spring B. Vulnerability–a new view of schizophrenia. J Abnorm Psychol. 1977;86:103–126. [DOI] [PubMed] [Google Scholar]
- 6. Myin-Germeys I, Oorschot M, Collip D, Lataster J, Delespaul P, van Os J. Experience sampling research in psychopathology: opening the black box of daily life. Psychol Med. 2009;39:1533–1547. [DOI] [PubMed] [Google Scholar]
- 7. Csikszentmihalyi M, Larson R. Validity and reliability of the experience-sampling method. In: Csikszentmihalyi M, ed. Flow and the Foundations of Positive Psychology. Claremont, CA: Springer; 2014:35–54. [Google Scholar]
- 8. Lataster T, Wichers M, Jacobs N, et al. Does reactivity to stress cosegregate with subclinical psychosis? A general population twin study. Acta Psychiatr Scand. 2009;119:45–53. [DOI] [PubMed] [Google Scholar]
- 9. Myin-Germeys I, Delespaul P, van Os J. Behavioural sensitization to daily life stress in psychosis. Psychol Med. 2005;35:733–741. [DOI] [PubMed] [Google Scholar]
- 10. Myin-Germeys I, van Os J, Schwartz JE, Stone AA, Delespaul PA. Emotional reactivity to daily life stress in psychosis. Arch Gen Psychiatry. 2001;58:1137–1144. [DOI] [PubMed] [Google Scholar]
- 11. Myin-Germeys I, van Os J. Stress-reactivity in psychosis: evidence for an affective pathway to psychosis. Clin Psychol Rev. 2007;27:409–424. [DOI] [PubMed] [Google Scholar]
- 12. Thewissen V, Bentall RP, Oorschot M, et al. Emotions, self-esteem, and paranoid episodes: an experience sampling study. Br J Health Psychol. 2011;50:178–195. [DOI] [PubMed] [Google Scholar]
- 13. Kramer I, Simons CJ, Wigman JT, et al. Time-lagged moment-to-moment interplay between negative affect and paranoia: new insights in the affective pathway to psychosis. Schizophr Bull. 2014;40:278–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Reininghaus U, Kempton MJ, Valmaggia L, et al. Stress sensitivity, aberrant salience, and threat anticipation in early psychosis: an experience sampling study. Schizophr Bull. 2016;42:712–722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cramer AO, Borsboom D, Aggen SH, Kendler KS. The pathoplasticity of dysphoric episodes: differential impact of stressful life events on the pattern of depressive symptom inter-correlations. Psychol Med. 2012;42:957–965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Isvoranu AM, Borsboom D, van Os J, Guloksuz S. A network approach to environmental impact in psychotic disorder: brief theoretical framework. Schizophr Bull. 2016;42:870–873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wigman JTW, van Os J, Thiery E, et al. Psychiatric diagnosis revisited: towards a system of staging and profiling combining nomothetic and idiographic parameters of momentary mental states. PLoS ONE. 2013;8:e59559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kendler KS, Zachar P, Craver C. What kinds of things are psychiatric disorders?Psychol Med. 2011;41:1143–1150. [DOI] [PubMed] [Google Scholar]
- 19. Cramer AO, Borsboom D, Aggen SH, Kendler KS. The pathoplasticity of dysphoric episodes: differential impact of stressful life events on the pattern of depressive symptom inter-correlations. Psychol Med. 2012;42:957–965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wichers M, Wigman JTW, Myin-Germeys I. Micro-level affect dynamics in psychopathology viewed from complex dynamical system theory. Emotion Review. 2015;7:362–367. [Google Scholar]
- 21. Bringmann LF, Vissers N, Wichers M, et al. A network approach to psychopathology: new insights into clinical longitudinal data. PLoS One. 2013;8:e60188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Pe ML, Kircanski K, Thompson RJ, et al. Emotion-network density in major depressive disorder. Clin Psychol Sci. 2015;3:292–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wigman JTW, van Os J, Borsboom D, et al. Exploring the underlying structure of mental disorders: cross-diagnostic differences and similarities from a network perspective using both a top-down and a bottom-up approach. Psychol Med. 2015;45:2375–2387. [DOI] [PubMed] [Google Scholar]
- 24. Wichers M. The dynamic nature of depression: a new micro-level perspective of mental disorder that meets current challenges. Psychol Med. 2014;44:1349–1360. [DOI] [PubMed] [Google Scholar]
- 25. Collip D, Nicolson NA, Lardinois M, Lataster T, van Os J, Myin-Germeys I; G.R.O.U.P Daily cortisol, stress reactivity and psychotic experiences in individuals at above average genetic risk for psychosis. Psychol Med. 2011;41:2305–2315. [DOI] [PubMed] [Google Scholar]
- 26. Lataster J, Myin-Germeys I, Wichers M, Delespaul PA, van Os J, Bak M. Psychotic exacerbation and emotional dampening in the daily life of patients with schizophrenia switched to aripiprazole therapy: a collection of standardized case reports. Ther Adv Psychopharmacol. 2011;1:145–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lataster T, Valmaggia L, Lardinois M, van Os J, Myin-Germeys I. Increased stress reactivity: a mechanism specifically associated with the positive symptoms of psychotic disorder. Psychol Med. 2013;43:1389–1400. [DOI] [PubMed] [Google Scholar]
- 28. Van der Steen Y, Gimpel-Drees J, Lataster T, et al. Clinical high risk for psychosis: the association between momentary stress, affective and psychotic symptoms. Acta Psychiatr Scand. 2017. doi:10.1111/acps.12714. [DOI] [PubMed] [Google Scholar]
- 29. Delespaul PA. Assessing Schizophrenia in Daily Life: The Experience Sampling Method [Dissertation]. Maastricht, the Netherlands: Maastricht University; 1995. [Google Scholar]
- 30. Oorschot M, Lataster T, Thewissen V, Wichers M, Myin-Germeys I. Mobile assessment in schizophrenia: a data-driven momentary approach. Schizophr Bull. 2012;38:405–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Palmier-Claus JE, Dunn G, Lewis SW. Emotional and symptomatic reactivity to stress in individuals at ultra-high risk of developing psychosis. Psychol Med. 2012;42:1003–1012. [DOI] [PubMed] [Google Scholar]
- 32. Myin-Germeys I, Delespaul P, van Os J. Behavioural sensitization to daily life stress in psychosis. Psychol Med. 2005;35:733–741. [DOI] [PubMed] [Google Scholar]
- 33. Lataster T, Wichers M, Jacobs N, et al. Does reactivity to stress cosegregate with subclinical psychosis? A general population twin study. Acta Psychiatr Scand. 2009;119:45–53. [DOI] [PubMed] [Google Scholar]
- 34. Jacobs N, Myin-Germeys I, Derom C, Delespaul P, van Os J, Nicolson NA. A momentary assessment study of the relationship between affective and adrenocortical stress responses in daily life. Biol Psychol. 2007;74:60–66. [DOI] [PubMed] [Google Scholar]
- 35. nlme: Linear and Nonlinear Mixed Effects Models [computer program]. Version 3 2015;1–120.
- 36. Bates D, Maechler M, Bolker B, Walker S. Fitting Linear Mixed-Effects Models using lme4. J Stat Softw. 2015;67:1–48. [Google Scholar]
- 37. Epskamp S, Cramer A, Waldorp L, Schmittmann V, Borsboom D. qgraph: network visualizations of relationships in psychometric data. J Stat Softw. 2012;48:1–18. [Google Scholar]
- 38. Good P. Permutation, Parametric and Bootstrap Tests of Hypotheses. 3rd ed. New York, NY: Springer; 2005. [Google Scholar]
- 39. Wigman JT, van Os J, Borsboom D, et al. ; MERGE. Exploring the underlying structure of mental disorders: cross-diagnostic differences and similarities from a network perspective using both a top-down and a bottom-up approach. Psychol Med. 2015;45:2375–2387. [DOI] [PubMed] [Google Scholar]
- 40. Klippel A, Myin-Germeys I, Chavez-Baldini U, et al. Modeling the interplay between psychological processes and adverse, stressful contexts and experiences in pathways to psychosis: an experience sampling study. Schizophr Bull. 2017;43:302–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Scheffer M, Carpenter SR, Lenton TM, et al. Anticipating critical transitions. Science. 2012;338:344–348. [DOI] [PubMed] [Google Scholar]
- 42. Cramer AOJ. The Glue of (ab) Normal Mental Life: Networks of Interacting Thoughts, Feelings and Behaviors [Dissertation]. Amsterdam, The Netherlands: University of Amsterdam; 2013. [Google Scholar]
- 43. Wigman JT, de Vos S, Wichers M, van Os J, Bartels-Velthuis AA. A transdiagnostic network approach to psychosis. Schizophr Bull. 2017;43:122–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.