Abstract
The primary goals of this longitudinal study were to examine the relationship between family functioning and adolescent alcohol use and to examine whether depressed mood mediates this relationship. An additional goal was to explore whether these relations were moderated by gender. The sample included 1,031 high school students from the Mid-Atlantic United States. Participants completed surveys in school during the spring of 2007, 2008, and 2009. Path analysis results indicated that family functioning predicted alcohol use for girls. Moreover, depressed mood mediated this relationship. None of the direct paths between family functioning and adolescent alcohol use were significant for boys. However, similar to girls, depressed mood negatively predicted alcohol use for boys. Taken together, the findings highlight the need for prevention programs targeting adolescent substance use to consider gender-specific trajectories.
Keywords: adolescence, family, depression, substance use, alcohol
As children progress through adolescence and become young adults, they often engage in exploration and experimentation as they establish a sense of self. However, risk behavior during this time can mark the beginning of dysfunctional patterns of behavior; for instance, adult substance use disorders often have their early roots in adolescence (Degenhardt et al., 2013; Marshall, 2014; McCambridge, McAlaney, & Rowe, 2011; Zucker, Donovan, Masten, Mattson, & Moss, 2008). In addition to increasing the risk for alcohol use disorders, the effects of alcohol use during adolescence may be acute. Especially concerning for adolescent well-being is engagement in heavy episodic drinking behavior, also called binge drinking (Courtney & Polich, 2009). Research indicates that the prevalence rates for binge drinking increase across the adolescent years, climbing from approximately 10% for 8th grade students to over 20% for 12th grade students (Johnston, O'Malley, Bachman, & Schulenberg, 2010; Johnston, O’Malley, Miech, Bachman, & Schulenberg, 2015). Also concerning is that binge drinking behavior may continue to escalate across the late adolescent years into emerging adulthood (Brown et al., 2008).
Binge drinking may be potentially problematic for a number of reasons, including the likelihood of later alcohol dependence (McCambridge et al., 2011). Especially relevant for adolescents and emerging adults, binge drinking is associated with cognitive impairment which may lead to acute and enduring risks. Importantly, it is the acute effects of alcohol use that carry the most severe consequences for adolescents, as impaired cognition and poor judgment resulting from alcohol use are associated with accidents, homicide, and suicide – the three leading causes of morbidity and mortality among adolescents (CDC, 2015; Hingson & Kenkel, 2004; Miniño 2010; USDHHS, 2007; Windle & Windle, 2005).
The Family and Adolescent Substance use
According to developmental systems models of human development (Fitzgerald, Zucker, & Yang, 1995; Overton & Lerner, 2014), contextual factors play a key role in the organization, disorganization, and reorganization of developmental pathways (Fitzgerald et al., 1995; Overton & Lerner, 2014). In keeping with a developmental systems perspective, prior research suggests that the family may play an important role (e.g., via family conflict, parental monitoring) in the development of alcohol use disorders (Chassin, Curran, Hussong, & Colder, 1997; Keller, Cummings, Davies, & Mitchell, 2008; Nargiso, Friend, & Florin, 2013; Ohannessian, 2013).
Through the lens of family systems theory, problematic drinking behavior can be understood as an indicator of struggles within the larger family as a social unit (Bowen, 1974). Family systems theory emphasizes the role of emotional connectedness in understanding individual behavior, and research has found that family relationship quality during adolescence predicts social and emotional wellbeing (Broderick, 1993; Pesola et al., 2015; Van Ryzin, Fosco, & Dishion, 2012). Of note, prior research has established predictive associations between family variables, such as communication, as well as relationship cohesion and satisfaction, and subsequent adolescent problem drinking (Chan, Kelly, & Toumbourou, 2013; Ohannessian, 2013). Accordingly, adolescent problem drinking can be interpreted as a maladaptive psychosocial outcome influenced by family discord and negative or impaired family communication.
There is evidence that family conflict predicts adolescent drinking across cultures and ethnic groups. For instance, in a large longitudinal sample of 6,522 White, Mexican American, and African American intermediate school students Bray, Adams, Getz, and Baer (2001) found that family conflict predicted alcohol use across all ethnic and racial groups. Similar results have been reported more recently from large school-based samples from Australia, Iceland, and the United States (Kelly et al. 2011; Kristjansson, Sigfusdottir, Allegrante, & Helgason, 2009; Skeer et al., 2011). Likewise, Chan et al. (2013) found a predictive relationship between family conflict and adolescent problem drinking in a sample of 886 Australian adolescents aged 12–14 years, but only for adolescent girls.
Although family conflict has been found to consistently predict adolescent substance use, the relationship between family communication and adolescent drinking is more complex. Research examining family communication has indicated that open communication may act as a buffer against maladaptive psychosocial outcomes, including depression and substance use (Ohannessian, 2013; Yu et al., 2006). Conversely, problem communication has been found to predict a variety of negative behaviors, including substance use and delinquency (Wang et al., 2013). Moreover, there is evidence of a differential gender effect, indicating that adolescent girls experience increased sensitivity to the effects of family communication compared to their male counterparts (Ohannessian, 2013).
Similar to open communication, family cohesion (perceived sense of unity or togetherness) may act as a buffer against adverse psychosocial outcomes. Research has shown that family cohesion is inversely related to drinking behaviors (Soloski, Kale Monk, & Durtschi, 2015), and that elements of family cohesion or bonding may buffer against the ill effects of parental problem drinking (Farrell, Barnes, & Banerjee, 1995; Kuendig & Kuntsche, 2006). Family satisfaction, adolescents’ perceived happiness with the amount of personal freedom, support, and emotional intimacy within the family, also appears to be negatively related to drinking behavior during adolescence. In a study of Italian adolescents, researchers found that heavy drinkers reported the lowest levels of family satisfaction (Laghi, Baiocco, Lonigro, Capacchione, & Baumgartner, 2012). Collectively, these indices of family life have important implications for adolescent drinking behavior, as well as other psychosocial outcomes, including depression.
Depression and Substance Use
While it is important to note that reciprocal relationships likely exist between depressed mood and substance use (Buckner, Keough, & Schmidt, 2007), research examining adolescent and young adult populations consistently indicates that depressed mood predicts substance use, alcohol use in particular (King, Iacono, & McGue, 2004; Sihvola et al., 2008). Of note, there is evidence that gender differences emerge in late adolescence as rates of substance use disorders (SUDs) are greater for young men than for young women at age 18; however, these differences do not exist earlier in adolescence (Schulte, Ramo, & Brown, 2009; Young et al., 2002). The differential increase in diagnosis rates has led to a research emphasis on articulating pathways to problem drinking for young men, without comparable investigation into gender-specific problem drinking pathways for young women (Schulte et al., 2009). Importantly, research suggests depressive symptomology may uniquely account for problem drinking behavior among adolescent and emerging adult females, pointing to a potentially important gender-specific pathway for young women (Chan et al., 2013; Dakof, 2000; Harrell & Karim, 2008; Kelly et al., 2011). More specifically, the link between depressed mood and problem drinking appears stronger for girls than for boys during adolescence (Saraceno, Heron, Munafò, Craddock, & van den Bree, 2012). However, the reason for this propensity remains unclear. One possibility is that depression onset may be earlier and swifter for girls rather than for boys, as research suggests that early adolescence and puberty may represent a time of particular vulnerability to depression for girls (Saraceno et al., 2012). Depression may spur some adolescent girls to engage in drinking behavior as a form of self-medication, potentially setting the stage for the development of problem drinking during adolescence (Marmorstein, 2010). Indeed, some research has indicated that during late adolescence, girls are more likely to engage in drinking as a response to emotional distress than are boys (Shippee & Owens, 2011).
Another related explanation is that family conflict may negatively influence adolescent girls more than adolescent boys. Some research indicates that an increased emphasis on communion for girls, that is, a tendency towards connection with others, may heighten vulnerability to depression as a result of family conflict (Davies & Lindsay, 2004). During puberty in particular, evidence suggests that increasing pressure to conform to gendered social expectations drives boys to become more independent and autonomous and girls to become more communal and concerned with others (Davies & Lindsay, 2001). This increased concern with interpersonal relationships may give rise to adolescent girls being differentially susceptible to the negative effects of family woes, such that they experience more emotional distress by dint of greater empathy. Indeed, emotional distress accounts for drinking behavior for girls more so than for boys during adolescence and emerging adulthood (Shippee & Owens, 2011).
The Present Study
Clearly, research suggests that the paths between family functioning and alcohol use during adolescence may be gender specific. A recent study conducted by Chan and colleagues (Chan et al., 2013) found depressed mood to mediate family conflict and alcohol use during early adolescence (their sample included 12–14 year-old Australian adolescents), especially for girls. The present study sought to replicate the depressed mood mediational model during late adolescence (our sample included 15–18 year-old adolescents), when problem drinking is more common. There is compelling evidence that family conflict during this time predicts depressive symptoms for girls (Herrenkohl, Kosterman, Hawkins, & Mason, 2009), and that there is a link between depression and problem drinking behavior (Buckner et al., 2007). Given that a sharp increase in problem drinking behavior for girls may occur during late adolescence (Brown et al., 2008; Grucza, Norberg, & Bierut, 2009), the focus of this study was to examine gender specific pathways to problem drinking during mid to late adolescence. In sum, the following research questions were addressed in a large, diverse sample of older adolescents from the United States: (a) Is family functioning (family satisfaction, and adolescent-parent communication) associated with adolescent alcohol use? (b) Is family functioning associated with adolescent depressed mood? (c) Does adolescent depressed mood mediate the relationship between family functioning and adolescent alcohol use? and (d) Do these relations differ by the gender of the adolescent?
Method
Participants
All of the adolescents participated in a larger research project (XXX). Participating youth (N=1,036, 52% girls) resided in the Mid-Atlantic region of the United States. During the spring of 2007 (Time 1), the spring of 2008 (Time 2), and the spring of 2009 (Time 3), participants were administered surveys in school. At Time 1, the adolescents were in 10th or 11th grade. The mean age of the adolescents at Time 1 was 16.15 (SD = .75). Most of the adolescents (58%) were White; 23% were African-American, 12% were Hispanic, and 2% were Asian (the remainder responded “other”). These percentages reflect the area from which the sample was drawn at that time (71% White, 23% African American, 7% Hispanic, 4% Asian; U.S. Census Bureau, 2008).
The majority of the adolescents (77%) lived with two or more caregivers. Of note, most of the parents (96% of mothers and 95% of fathers) were high school graduates. Some of the parents (26% of mothers and 24% of fathers) had graduated from a four-year college. A minority of the parents (10% of mothers and 7% of fathers) had attended graduate school.
Procedures
The study protocol was approved by the University of Delaware’s Institutional Review Board. Seven public high schools (from Delaware, Maryland, and Pennsylvania) within approximately 60 miles of the study site participated. During the spring of 2007, 10th and 11th grade students from these high schools were invited to participate in the study. Seventy one percent of the students participated. Most of the non-participating students were absent on the day of data collection. Only three percent of the adolescents who were present during data collection did not participate. Adolescents who had parental consent and provided assent were administered a self-report survey in school by trained research staff (all of whom were certified with human subjects training). The participants were informed that participation was voluntary, they could withdraw from the study at any time, and all data collected were confidential. In addition, they were told that an active Certificate of Confidentiality from the U.S. government was in place to further protect their privacy. The survey took approximately 40 minutes to complete. Participants were given a movie pass immediately after turning in their completed survey.
All of the participants were invited to participate in the study again during the spring of 2008 (Time 2) and the spring of 2009 (Time 3). The same protocol was followed at each wave. Twenty percent of the youth participating at Time 1 did not participate at subsequent waves. Adolescents who participated at all three times of measurement were compared to those who participated only at one time of measurement to examine whether they differed in regard to the study variables. The only difference between the longitudinal and non-longitudinal subsamples was that the longitudinal sample reported greater family satisfaction at the first time point [t(969) = −2.84, p < .05].
Measures
All of the adolescents completed a demographic questionnaire. This questionnaire included questions on age, race, family structure (living with one or more than one parent), and parents’ highest education level completed (1 = elementary school to 6 = graduate or medical school). The specific measures administered for this study are discussed in detail below.
Adolescent-parent communication
The Parent-Adolescent Communication Scale (Barnes & Olson, 2003) was administered to the adolescents to measure communication between adolescents and their parents. A sample item is “I find it easy to discuss problems with my mother/father.” The response scale ranges from 1 = strongly disagree to 5 = strongly agree. The 20-item total communication score was used in this study. Total communication scores (range = 20–100) were obtained separately for adolescents and their mothers and adolescents and their fathers. Prior research has supported the construct validity of this measure (Barnes & Olson, 2003). In our sample, the Cronbach alpha coefficients were .90–.94 for adolescent-mother communication and .90–.92 for adolescent-father communication, across the three times of measurement.
Family satisfaction
The Family Satisfaction Scale (FSS; Olson & Wilson, 1989) was used to measure the adolescents’ family satisfaction. A FSS sample item is “How satisfied are you with how close you feel to the rest of your family?” The response scale ranges from 1 = dissatisfied to 5 = extremely satisfied. Previous studies have supported the validity of the FSS (Olson, 2011). In our sample, Cronbach alpha coefficients were .90–.92 across the three waves of measurement.
Depressed mood
Adolescent depression was assessed with the Center for Epidemiological Studies Depression Scale for Children (CES-DC; Weissman, Orvaschell, & Padian, 1980). The CES-DC is completed in relation to how the respondent felt or acted during the past week. A representative CES-DC item is “I felt sad.” The CES-DC response scale ranges from 1 = not at all to 4 = a lot. In this study, the 20 items from the CES-DC were summed to reflect a total depressive symptomatology score (range = 20–80). Previous research has demonstrated that the CES-DC is a reliable and valid measure of depressive symptomatology (Garrison, Addy, Jackson, McKeown, & Waller, 1991; Ohannessian, 2012; Ohannessian, Lerner, Lerner, & von Eye, 1999). The Cronbach alpha coefficients for the CES-DC in our sample were .90–.92, across the three times of measurement.
Alcohol use
In order to measure alcohol quantity, the adolescents were asked to report how much, “on the average day,” they usually drank in the last six months (separate questions were used for beer, wine, and liquor). The response scale ranged from 0 = none to 9 = more than 8 drinks. A drink was defined as a can/bottle of beer, a glass of wine, or a drink containing liquor (1 shot = 1 ounce). To measure alcohol frequency, the adolescents were asked to report how often they usually had a drink (beer, wine, and liquor) in the last six months. The response scale for this question was 0 = never, 1 = a few times, 2 = about once a month, 3 = 2–3 days a month, 4 = about once a week, 5 = 2–3 days a week, 6 = 4–5 days a week, and 7 = every day. Sums were calculated across the beverage types for quantity and frequency. The quantity and frequency scores then were multiplied to reflect an estimated total volume consumed (QF) (refer to Sobell & Sobell, 1995, for additional information). To assess binge drinking, the adolescents were asked how many times they drank six or more drinks (cans/bottles of beer, glasses of wine, or drinks of liquor) on one occasion during the last six months. The alcohol use and binge drinking variables were positively skewed. Therefore, the logarithmic transformation was used for these variables. Of note, during the six months prior to data collection, 53% of the adolescents reported drinking alcohol and 21% reported binge drinking.
Analysis Plan
First, bivariate relations between the variables of interest were examined. Independent samples t-tests were used to test for mean level gender differences in the study variables. Path analyses were conducted to examine the direct paths between the family functioning variables (family satisfaction and adolescent-parent communication) at Time 1 and the alcohol use variables (alcohol use and binge drinking) at Time 3. Indirect paths also were examined to explore whether family functioning at Time 1 predicted depressed mood at Time 2, and whether depressed mood, in turn, predicted alcohol use and binge drinking at Time 3. Baseline levels of the dependent variables, age, race/ethnicity, parent education, and family structure were included as covariates in the models. Full Information Maximum Likelihood (FIML) estimation was used to handle missing data. Because FIML utilizes all available data to produce statistics based on maximum likelihood, it has been found to produce unbiased parameter estimates (Wothke, 2000).
Based on both theoretical and empirical evidence that suggests that the relations among the variables differ for girls and boys (Brown et al., 2008; Chan et al., 2013; Dakof, 2000; Grucza et al., 2009; Harrell & Karim, 2008; Kelly et al., 2011; Saraceno et al., 2012), a multiple group comparison was run. This approach allows for a more rigorous test of gender differences than simply controlling for gender by including it as a covariate or by running separate models by gender. The latter methods do not formally examine whether gender differences are statistically significant. In contrast, a multiple group analysis allows for the testing of invariance of path coefficients, variances, and covariances across gender. Following the recommendations of Vandenberg and Lance (2000), an unconstrained model with freely estimated parameters for both groups (boys and girls) was compared to a series of models that constrained path coefficients, variances, and covariances to be equal across groups.
Results
Descriptive Statistics and Bivariate Analyses
Descriptive statistics and Pearson product-moment correlations for all variables of interest at baseline (Time 1) are presented in Table 1. As shown, adolescent reports of family satisfaction, adolescent-mother communication, and adolescent-father communication all were positively and significantly correlated with one another for both girls and boys. These family variables also were significantly associated with depressed mood such that higher levels of reported family satisfaction, and adolescent-parent communication were related to less depressive symptoms. For boys, none of the family variables were significantly related to alcohol use or binge drinking. However, for girls, higher levels of adolescent-mother communication and family satisfaction were significantly related to less binge drinking and alcohol use, respectively.
Table 1.
Correlations, Means, and Standard Deviations Among Study Variables at Time 1
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | Mean | SD |
|---|---|---|---|---|---|---|---|---|
| 1. Adolescent Mother Communication | -- | .34*** | .52*** | −.28*** | .01 | .05 | 66.78 | 14.05 |
| 2. Adolescent Father Communication | .21*** | -- | .49*** | −.31*** | −.07 | −.02 | 64.39 | 15.50 |
| 3. Family Satisfaction | .61*** | .41*** | -- | −.33*** | −.03 | −.01 | 48.36 | 10.77 |
| 4. Depressed Mood | −.42*** | −.26*** | −.41*** | -- | .01 | −.03 | 33.75*** | 9.97 |
| 5. Alcohol Use | −.16 | .03 | −.18*** | .10 | -- | .72*** | 5.58 | 13.86 |
| 6. Binge Drinking | −.24*** | .04 | −.15 | .13* | .72*** | -- | 1.77 | 6.03 |
| Mean | 67.32 | 63.62 | 48.53 | 37.52*** | 4.25 | 1.67 | -- | -- |
| SD | 16.33 | 16.74 | 10.95 | 11.67 | 11.86 | 6.11 | -- | -- |
Note. Means and correlations for boys and girls are presented above and below the diagonal, respectively. The means for both boys and girls are marked with * to indicate significant gender differences.
p<.05;
p<.01;
p<.001.
Independent samples t-tests were run to compare mean-level gender differences in the study variables at Time 1. As shown in Table 1, significant gender differences were not found for adolescent reports of adolescent-mother communication, adolescent-father communication, family satisfaction, alcohol use, or binge drinking. However, there was a significant gender difference for depressed mood, indicating that girls reported higher levels of depressed mood in comparison to boys (see Table 1).
Longitudinal Analyses
As a first step for the longitudinal analyses, a multiple group comparison analysis was conducted. When comparing the unconstrained model to the other models, the chi-square difference test statistic was found to be significant for the structural intercepts, structural means, structural covariances, and structural residuals (ΔX2(24) = 41.58, p < .05; ΔX2(33) = 57.21, p < .05; ΔX2(51) = 99.95, p < .001; ΔX2(55) = 103.22, p < .001 respectively), indicating that these parameters differed significantly by gender. Therefore, parameter estimates and fit statistics of the unconstrained model are reported. Indices of model fit suggested that the specified model fit the data well (X2(70) = 144.67, p < .001; CMIN/DF = 2.07; CFI = .95; RMSEA = .03).
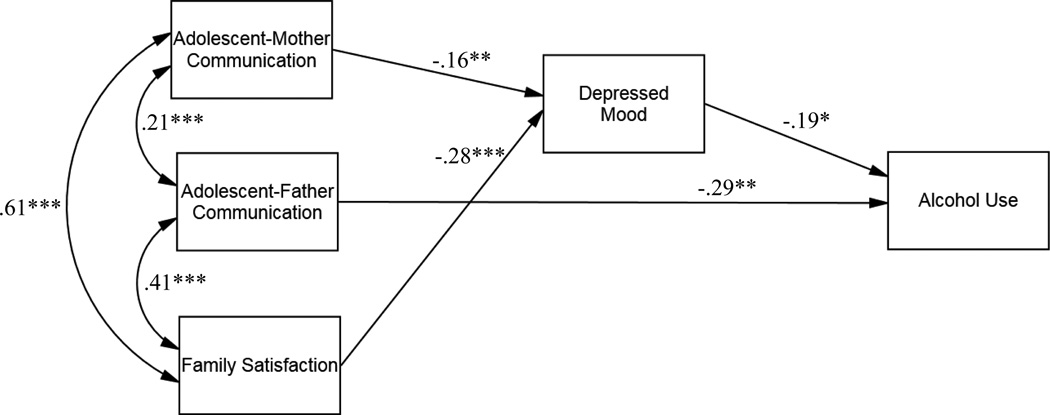
Results for girls
As shown in Figure 1, adolescent-mother communication and adolescent family satisfaction negatively predicted depressed mood (β = −.16, p < .01; β = −.28, p < .001 respectively). Depressed mood, in turn, negatively predicted alcohol use (β = −.19, p < .05). Sobel tests were conducted to examine whether depressed mood mediated the paths between adolescent-mother communication and alcohol use and between family satisfaction and adolescent alcohol use. Results indicated that depressed mood did not significantly mediate adolescent-mother communication and adolescent alcohol use (c.r. =1.75, p = .09). In contrast, depressed mood significantly mediated the path between adolescent family satisfaction and adolescent alcohol use (c.r. =2.05, p = .04).
Figure 1.
Final model for girls. Standardized regression coefficients are presented. For ease of interpretation, only significant paths are included. The control variables also are not shown. *p < .05; **p < .01; ***p < .001.
A direct path also was observed between adolescent-father communication and adolescent alcohol use (β = −.29, p < .001), suggesting that poorer communication predicted more alcohol use for girls. Neither of the family functioning variables nor depressed mood significantly predicted binge drinking for girls.
Results for boys
In contrast to the results for girls, none of the paths between the family functioning variables and depressed mood and between the family functioning variables and the alcohol use variables were significant for boys. The only significant path that emerged suggested that, similar to the finding for girls, greater depressed mood at Time 2 significantly predicted less alcohol use at Time 3 (β = −.22, p < .05).
Discussion
The primary goal of this study was to examine the relationship between family functioning and adolescent alcohol use and to examine whether depressed mood mediates this relationship. Results from this study echo the novel findings from Chan et al. (2013), suggesting that indicators of family functioning and depressed mood are significant predictors of adolescent alcohol use. Of note, there are several parallels between the methods used in our study and the Chan et al. (2013) study: Both studies used 3 waves of annual longitudinal data collected with similar measures in schools from large community samples (N=1,036, and N=886, respectively). The primary difference between the two studies relates to the samples. The Chan et al. sample included adolescents from Australia, whereas our study examined adolescents from the U.S. In addition, the adolescents in the Chan et al. study were 12–14 years of age, whereas the adolescents in our study were 15–18 years of age. Therefore, the present study builds on Chan and colleagues’ work, contributing to the literature by demonstrating that gender-based longitudinal variations in the links between family dynamics, depressed mood, and alcohol use extend beyond middle adolescence through late adolescence, when heavy alcohol use is more common. As these two studies represent different cultural groups, our results suggest that the underpinnings of gender differences in risk behavior in Australia and the United States may have commonalities - perhaps in the emphasis girls place on closeness, and subsequent increased communication, within the family (Davies & Lindsay, 2004; Shippee & Owens, 2011).
In our study, adolescent-mother communication and adolescent reported family satisfaction negatively predicted levels of depressed mood for girls. These findings are consistent with the literature (Davies & Lindsay, 2004) and with Chan et al.’s findings showing that family conflict predicted depressed mood, especially for girls. It is noteworthy that in both the Chan et al. study and our study, the family appeared to play a more salient role for girls than for boys. In the Chan et al. study, the relationship between family conflict and depressed mood was stronger for girls than for boys and in our study, none of the direct paths or indirect paths between the family functioning variables and alcohol use was significant for boys. These findings are consistent with research indicating that girls are more enmeshed in the family and more likely to experience family stress than are boys (Gore, Aseltine, & Colten, 1993; Kort-Butler, 2009). Given that girls are more sensitive to disruptions and conflict in their family environments in comparison to boys during adolescence (Chan et al., 2013; Davies & Lindsay, 2004; Unger, Brown, Tressel, & McLeod, 2000), problems in the family and family relationships should be more likely to negatively affect girls than boys. Support for differential gender effects may also be drawn from a family systems theory perspective, as subsystems with a family may have different relationship dynamics. For example, patterns of conflict within the mother-child subsystem may not be the same as those that characterize father-child relationships. Hence gender-specific pathways to adolescent outcomes may be influenced by subsystem-specific relationship dynamics, including levels of availability and conflict in parent-child communication.
In both the Chan et al. study and our study, depressed mood was found to significantly mediate family functioning and adolescent alcohol use for girls. In our study, depressed mood specifically mediated the path between adolescent reported family satisfaction and girls’ alcohol use. While depressed mood did not act as a mediator between family functioning and alcohol use for the boys in our sample, there was a significant predictive relationship between depressed mood and alcohol use. In contrast to Chan et al.’s findings, in our study, depressed mood played a role in both girls’ and boys’ alcohol use. Also of note, while depressed mood significantly predicted adolescent alcohol use in both studies, the direction of this path differed across studies. In Chan et al.’s study of early adolescents, depressed mood positively predicted later alcohol use, whereas in our study of older adolescents, depressed mood negatively predicted later alcohol use. Results from our study indicated that adolescents who were more depressed reported less alcohol use. Although this finding may seem counterintuitive, it is important to consider that during late adolescence, social drinking is commonplace (O’Hara, Armeli, & Tennen, 2015). Given that a hallmark of depression is withdrawal and that depression is associated with impairments in social functioning (Jaycox et al., 2009), decreased peer support (Hankin, 2006), and uneasiness in group situations (Weissman et al., 1980), it is not surprising that adolescents reporting more depressed mood reported less alcohol use. An important next step would be for future research to examine whether social behavior mediates the link between depressed mood and alcohol use observed for the adolescents in our study. Taken together, the findings from Chan et al.’s (2013) study and our study highlight the need to take the developmental stage of the adolescent into account. Although a significant relationship between depressed mood and alcohol use was observed in both studies, the direction of the relationship appeared to depend on the age of the adolescent.
This study extended the current literature by examining whether depressed mood mediates the relationship between family functioning and adolescent alcohol use in a sample of older adolescents. Nonetheless, caveats should be noted. The adolescents in this study resided in the Mid-Atlantic region of the United States. In addition, the adolescents who remained in the study over time had higher levels of family satisfaction in comparison to adolescents who dropped out of the study. Therefore, the adolescent participants might not be truly representative of the broader population and caution should be taken in generalizing the results to other adolescents. It also should be noted that the study relied on self-report data. However, research has indicated that adolescents are accurate reporters of their own behaviors, including their substance use (Deković et al., 2006). Nevertheless, it would be informative for future studies to replicate the study findings with research using other types of methodology (e.g., parent reports). In this study, depressed mood was examined as the mediator. Given that depression is more common for girls than for boys during adolescence (Negriff & Susman, 2011; Ohannessian et al., 1999), it would be informative for future research to examine problems that are relatively more common for adolescent boys (e.g., externalizing behaviors; Grant et al., 2006) as potential mediators. It also should be noted that only family satisfaction and adolescent-parent communication were assessed as indicators of family functioning. Future consideration of other family dynamic indicators not measured in the present study is warranted, as the lack of significant family pathways found here should not be misconstrued as an absence of family influence on adolescent boys’ alcohol use more broadly. Finally, although the data were longitudinal, causality cannot be assumed.
Despite these limitations, results from this study underscore the importance of exploring the underlying mechanisms involved in the relationship between family functioning and adolescent alcohol use. Moreover, the findings highlight the need to consider gender differences in the mediation process. Of note, the large, diverse sample was drawn from the community and followed over time. It also is noteworthy that structural equation modeling was used to estimate all paths simultaneously (rather than separate regression models), which yields a more comprehensive test of the associations at play. These strengths further validate the results.
Importantly, findings from this study also have implications for prevention. The role of family communication in predicting alcohol use underscores the importance of parent and family-based prevention efforts, which while effective, are not widely employed at present (Smit, Verdurmen, Monshouwer & Smit, 2008; Spoth, Redmond & Shin, 2001). Specifically, our findings speak to the need to enhance the quality of communication between adolescents and parents, particularly for girls, during the transition years of middle to late adolescence, when alcohol use tends to increase (Brown et al., 2008).
Acknowledgments
We are grateful to the schools and students who participated in the study. Special thanks go to members of the AAP staff, especially Jessica Schulz, Kelly Cheeseman, Lisa Fong, Alyson Cavanaugh, Sara Bergamo, Ashley Malooly, Ashley Ings, and Magdalena Owczarska. This research was supported by NIH grant number K01-AA015059.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Barnes H, Olson DH. Parent-Adolescent Communication Scale. Minneapolis: Life Innovations, Inc.; 2003. [Google Scholar]
- Bowen M. Alcoholism as viewed through family systems theory and family psychotherapy. Annals of the New York Academy of Sciences. 1974;233(1):115–122. doi: 10.1111/j.1749-6632.1974.tb40288.x. [DOI] [PubMed] [Google Scholar]
- Bray JH, Adams GJ, Getz JG, Baer PE. Developmental, family, and ethnic in influences on adolescent alcohol usage: A growth curve approach. Journal of Family Psychology. 2001;15(2):301. doi: 10.1037//0893-3200.15.2.301. [DOI] [PubMed] [Google Scholar]
- Brown SA, McGue M, Maggs J, Schulenberg J, Hingson R, Swartzwelder S, Martin C, Chung T, Tapert SF, Sher K, Winters KC, Lowman C, Murphy S. A developmental perspective on alcohol and youths 16 to 20 years of age. Pediatrics. 2008;121(Supplement 4):S290–S310. doi: 10.1542/peds.2007-2243D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broderick CB. Understanding family process: Basics of family systems theory. Newbury Park, CA: Sage; 1993. [Google Scholar]
- Buckner JD, Keough ME, Schmidt NB. Problematic alcohol and cannabis use among young adults: The roles of depression and discomfort and distress tolerance. Addictive Behaviors. 2007;32(9):1957–1963. doi: 10.1016/j.addbeh.2006.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Disease Control and Prevention and the National Center for Health Statistics. Adolescent Health. 2015 Retrieved from: http://www.cdc.gov/nchs/fastats/adolescent-health.htm.
- Chan GC, Kelly AB, Toumbourou JW. Accounting for the association of family conflict and heavy alcohol use among adolescent girls: The role of depressed mood. Journal of Studies on Alcohol and Drugs. 2013;74(3):396. doi: 10.15288/jsad.2013.74.396. [DOI] [PubMed] [Google Scholar]
- Chassin L, Curran PJ, Hussong AM, Colder CR. The relation of parent alcoholism to adolescent substance use: A longitudinal follow-up study. In: Marlatt GA, VandenBos GR, editors. Addictive Behaviors: Readings in Etiology, Prevention, and Treatment. Washington, DC: American Psychological Association; 1997. pp. 509–533. [Google Scholar]
- Courtney KE, Polich J. Binge drinking in young adults: Data, definitions, and determinants. Psychological Bulletin. 2009;135(1):142. doi: 10.1037/a0014414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dakof GA. Understanding gender differences in adolescent drug abuse: Issues of comorbidity and family functioning. Journal of Psychoactive Drugs. 2000;32(1):25–32. doi: 10.1080/02791072.2000.10400209. [DOI] [PubMed] [Google Scholar]
- Davies PT, Lindsay L. Does gender moderate the effects of conflict on children? In: Grych J, Fincham, editors. Child Development and Interparental Conflict. New York: Cambridge University Press; 2001. pp. 64–97. [Google Scholar]
- Davies PT, Lindsay LL. Interparental conflict and adolescent adjustment: Why does gender moderate early adolescent vulnerability? Journal of Family Psychology. 2004;18(1):160. doi: 10.1037/0893-3200.18.1.160. [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Coffey C, Romaniuk H, Swift W, Carlin JB, Hall WD, Patton GC. The persistence of the association between adolescent cannabis use and common mental disorders into young adulthood. Addiction. 2013;108(1):124–133. doi: 10.1111/j.1360-0443.2012.04015.x. [DOI] [PubMed] [Google Scholar]
- Deković M, ten Have M, Vollebergh WA, Pels T, Oosterwegel A, Wissink IB, Ormel J. The cross-cultural equivalence of parental rearing measure: EMBU-C. European Journal of Psychological Assessment. 2006;22(2):85–91. [Google Scholar]
- Farrell MP, Barnes GM, Banerjee S. Family cohesion as a buffer against the effects of problem-drinking fathers on psychological distress, deviant behavior, and heavy drinking in adolescents. Journal of Health and Social Behavior. 1995:377–385. [PubMed] [Google Scholar]
- Fitzgerald HE, Zucker RA, Yang H. Developmental systems theory and alcoholism: Analyzing patterns of variation in high-risk families. Psychology of Addictive Behaviors. 1995;9(1):8–22. [Google Scholar]
- Garrison CZ, Addy C, Jackson KL, McKeown R, Waller JL. The CES-D as a screen for depression and other psychiatric disorders in adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 1991;30:636–641. doi: 10.1097/00004583-199107000-00017. [DOI] [PubMed] [Google Scholar]
- Gore S, Aseltine RH, Colten ME. Gender, socialrelational involvement, and depression. Journal of Research on Adolescence. 1993;3:101–125. [Google Scholar]
- Grant KE, Compas BE, Thurm AE, McMahon SD, Gipson PY, Campbell AJ, Krochock K, Westerholm RI. Stressors and child and adolescent psychopathology: Evidence of moderating and mediating effects. Clinical Psychology Review. 2006;26:257–283. doi: 10.1016/j.cpr.2005.06.011. [DOI] [PubMed] [Google Scholar]
- Grucza RA, Norberg KE, Bierut LJ. Binge drinking among youths and young adults in the United States: 1979–2006. Journal of the American Academy of Child & Adolescent Psychiatry. 2009;48(7):692–702. doi: 10.1097/CHI.0b013e3181a2b32f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL. Adolescent depression: Description, causes, and interventions. Epilepsy & Behavior. 2006;8(1):102–114. doi: 10.1016/j.yebeh.2005.10.012. [DOI] [PubMed] [Google Scholar]
- Harrell ZA, Karim NM. Is gender relevant only for problem alcohol behaviors? An examination of correlates of alcohol use among college students. Addictive Behaviors. 2008;33(2):359–365. doi: 10.1016/j.addbeh.2007.09.014. [DOI] [PubMed] [Google Scholar]
- Herrenkohl TI, Kosterman R, Hawkins JD, Mason WA. Effects of growth in family conflict in adolescence on adult depressive symptoms: Mediating and moderating effects of stress and school bonding. Journal of Adolescent Health. 2009;44(2):146–152. doi: 10.1016/j.jadohealth.2008.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hingson R, Kenkel D. Social health and economic consequences of underage drinking. In: Bonnie RJ, O’Connell ME, editors. Reducing Underage Drinking: A Collective Responsibility. Washington, DC: National Academies Press; 2004. pp. 351–382. [PubMed] [Google Scholar]
- Jaycox LH, Stein BD, Paddock S, Miles JV, Chandra A, Meredith LS, Burnam MA. Impact of teen depression on academic, social, and physical functioning. Pediatrics. 2009;124(4):596–605. doi: 10.1542/peds.2008-3348. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future: National Survey Results on Drug Use, 1975–2009. Volume I: Secondary School Students. Bethesda, MD: National Institute on Drug Abuse; 2010. (NIH Publication No. 10-7584) [Google Scholar]
- Johnston LD, O'Malley PM, Miech RA, Bachman JG, Schulenberg JE. Monitoring the Future national results on adolescent drug use: Overview of key findings, 2014. Ann Arbor, Mich: Institute for Social Research, the University of Michigan; 2015. [Google Scholar]
- Keller PS, Cummings EM, Davies PT, Mitchell PM. Longitudinal relations between parental drinking problems, family functioning, and child adjustment. Development and Psychopathology. 2008;20(1):195–212. doi: 10.1017/S0954579408000096. [DOI] [PubMed] [Google Scholar]
- Kelly AB, O'Flaherty M, Toumbourou JW, Connor JP, Hemphill SA, Catalano RF. Gender differences in the impact of families on alcohol use: A lagged longitudinal study of early adolescents. Addiction. 2011;106(8):1427–1436. doi: 10.1111/j.1360-0443.2011.03435.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King SM, Iacono WG, McGue M. Childhood externalizing and internalizing psychopathology in the prediction of early substance use. Addiction. 2004;99(12):1548–1559. doi: 10.1111/j.1360-0443.2004.00893.x. [DOI] [PubMed] [Google Scholar]
- Kort-Butler LA. Coping styles and sex differences in depressive symptoms and delinquent behavior. Journal of Youth and Adolescence. 2009;38:122–136. doi: 10.1007/s10964-008-9291-x. [DOI] [PubMed] [Google Scholar]
- Kristjansson AL, Sigfusdottir ID, Allegrante JP, Helgason AR. Parental divorce and adolescent cigarette smoking and alcohol use: Assessing the importance of family conflict. Acta Paediatrica. 2009;98(3):537–542. doi: 10.1111/j.1651-2227.2008.01133.x. [DOI] [PubMed] [Google Scholar]
- Kuendig H, Kuntsche E. Family bonding and adolescent alcohol use: Moderating effect of living with excessive drinking parents. Alcohol and Alcoholism. 2006;41(4):464–471. doi: 10.1093/alcalc/agl018. [DOI] [PubMed] [Google Scholar]
- Laghi F, Baiocco R, Lonigro A, Capacchione G, Baumgartner E. Family functioning and binge drinking among Italian adolescents. Journal of Health Psychology. 2012;17(8):1132–1141. doi: 10.1177/1359105311430005. [DOI] [PubMed] [Google Scholar]
- Marmorstein NR. Longitudinal associations between depressive symptoms and alcohol problems: The influence of comorbid delinquent behavior. Addictive Behaviors. 2010;35(6):564–571. doi: 10.1016/j.addbeh.2010.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall EJ. Adolescent alcohol use: Risks and consequences. Alcohol and Alcoholism. 2014;49(2):160–164. doi: 10.1093/alcalc/agt180. [DOI] [PubMed] [Google Scholar]
- McCambridge J, McAlaney J, Rowe R. Adult consequences of late adolescent alcohol consumption: A systematic review of cohort studies. PLoS Medicine. 2011;8(2):1–13. doi: 10.1371/journal.pmed.1000413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miniño AM. Mortality among teenagers aged 12–19 years: United States, 1999–2006. Hyattsville, MD: National Center for Health Statistics; 2010. NCHS data brief, no 37. [Google Scholar]
- Nargiso JE, Friend K, Florin P. An examination of peer, family, and community context risk factors for alcohol use and alcohol use intentions in early adolescents. The Journal of Early Adolescence. 2013;33(7):973–993. [Google Scholar]
- Negriff S, Susman EJ. Pubertal timing, depression, and externalizing problems: A framework, review, and examination of gender differences. Journal of Research on Adolescence. 2011;21:717–746. [Google Scholar]
- Ohannessian CM. Does technology use moderate the relationship between parental alcoholism and adolescent alcohol and cigarette use? Addictive behaviors. 2009;34(6):606–609. doi: 10.1016/j.addbeh.2009.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohannessian CM. Parental problem drinking and adolescent psychosocial adjustment: The mediating role of adolescent–parent communication. Journal of Research on Adolescence. 2012;22(3):498–511. [Google Scholar]
- Ohannessian CM. Parental problem drinking and adolescent psychological problems: The moderating effect of adolescent-parent communication. Youth & Society. 2013;45(1):3–26. [Google Scholar]
- Ohannessian CM, Lerner RM, Lerner JV, von Eye A. Does self-competence predict gender differences in adolescent depression and anxiety? Journal of Adolescence. 1999;22:397–411. doi: 10.1006/jado.1999.0231. [DOI] [PubMed] [Google Scholar]
- O’Hara RE, Armeli S, Tennen H. College students’ drinking motives and social-contextual factors: Comparing associations across levels of analysis. Psychology of Addictive Behaviors. 2015;29(2):420–429. doi: 10.1037/adb0000046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olson D. FACES IV and the circumplex model: Validation study. Journal of Marital and Family Therapy. 2011;37:64–80. doi: 10.1111/j.1752-0606.2009.00175.x. [DOI] [PubMed] [Google Scholar]
- Olson DH, Wilson M. Family satisfaction. In: Olson DH, McCubbin HI, editors. Family inventories. St Paul, MN: Family Social Science, University of Minnesota; 1989. [Google Scholar]
- Overton WF, Lerner RM. Fundamental concepts and methods in developmental science: A relational perspective. Research in Human Development. 2014;11(1):63–73. [Google Scholar]
- Pesola F, Shelton KH, Heron J, Munafò M, Hickman M, van den Bree MB. The developmental relationship between depressive symptoms in adolescence and harmful drinking in emerging adulthood: The role of peers and parents. Journal of Youth and Adolescence. 2015:1–15. doi: 10.1007/s10964-015-0295-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saraceno L, Heron J, Munafò M, Craddock N, van den Bree M. The relationship between childhood depressive symptoms and problem alcohol use in early adolescence: Findings from a large longitudinal population-based study. Addiction. 2012;107(3):567–577. doi: 10.1111/j.1360-0443.2011.03662.x. [DOI] [PubMed] [Google Scholar]
- Schulte MT, Ramo D, Brown SA. Gender differences in factors influencing alcohol use and drinking progression among adolescents. Clinical Psychology Review. 2009;29(6):535–547. doi: 10.1016/j.cpr.2009.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shippee ND, Owens TJ. GPA, depression, and drinking: A longitudinal comparison of high school boys and girls. Sociological Perspectives. 2011;54(3):351–376. [Google Scholar]
- Sihvola E, Rose RJ, Dick DM, Pulkkinen L, Marttunen M, Kaprio J. Early-onset depressive disorders predict the use of addictive substances in adolescence: A prospective study of adolescent Finnish twins. Addiction. 2008;103(12):2045–2053. doi: 10.1111/j.1360-0443.2008.02363.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skeer MR, McCormick MC, Normand SLT, Mimiaga MJ, Buka SL, Gilman SE. Gender differences in the association between family conflict and adolescent substance use disorders. Journal of Adolescent Health. 2011;49(2):187–192. doi: 10.1016/j.jadohealth.2010.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smit E, Verdurmen J, Monshouwer K, Smit F. Family interventions and their effect on adolescent alcohol use in general populations; a meta-analysis of randomized controlled trials. Drug and Alcohol Dependence. 2008;97(3):195–206. doi: 10.1016/j.drugalcdep.2008.03.032. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Alcohol consumption measures. In: Allen JP, Columbus M, editors. Assessing alcohol problems: A guide for clinicians and researchers. NIAAA Treatment Handbook Series 4. Washington, D.C.: U.S. Department of Health and Human Services; 1995. [Google Scholar]
- Soloski KL, Kale Monk J, Durtschi JA. Trajectories of early binge drinking: A function of family cohesion and peer use. Journal of Marital and Family Therapy. 2015 doi: 10.1111/jmft.12111. Advance online publication. [DOI] [PubMed] [Google Scholar]
- Spoth RL, Redmond C, Shin C. Randomized trial of brief family interventions for general populations: Adolescent substance use outcomes 4 years following baseline. Journal of Consulting and Clinical Psychology. 2001;69(4):627. doi: 10.1037//0022-006x.69.4.627. [DOI] [PubMed] [Google Scholar]
- Unger DG, Brown MB, Tressel PA, McLeod LE. Interparental conflict and adolescent depressed mood: The role of family functioning. Child Psychiatry and Human Development. 2000;31:23–41. doi: 10.1023/a:1001922004459. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. U.S. Census Bureau: State and county QuickFacts. 2008 Retrieved from http://quickfacts.census.gov/qfd/states/10/10003.html.
- United States Department of Health and Human Services. The surgeon general’s call to action to prevent and reduce underage drinking. Washington, DC: USDHHS, Office of the Surgeon General; 2007. [PubMed] [Google Scholar]
- Vandenberg RJ, Lance CE. A review and synthesis of the measurement invariance literature: Suggestions, practices, and recommendations for organizational research. Organizational Research Methods. 2000;3(1):4–70. [Google Scholar]
- Van Ryzin MJ, Fosco GM, Dishion TJ. Family and peer predictors of substance use from early adolescence to early adulthood: An 11-year prospective analysis. Addictive Behaviors. 2012;37(12):1314–1324. doi: 10.1016/j.addbeh.2012.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang B, Stanton B, Li X, Cottrell L, Deveaux L, Kaljee L. The influence of parental monitoring and parent–adolescent communication on Bahamian adolescent risk involvement: A three-year longitudinal examination. Social Science & Medicine. 2013;97:161–169. doi: 10.1016/j.socscimed.2013.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman M, Orvaschell H, Padian N. Children’s symptom and social functioning: Self-report scales. Journal of Nervous and Mental Disorders. 1980;168:736–740. doi: 10.1097/00005053-198012000-00005. [DOI] [PubMed] [Google Scholar]
- Windle M, Windle RC. Alcohol consumption and its consequences among adolescents and young adults. In: Galanter M, editor. Recent developments in alcoholism: Volume 17. Alcohol problems in adolescent and young adults. Epidemiology neurobiology prevention treatment. New York: Kluwer Academic/Plenum Publishers; 2005. pp. 67–83. [DOI] [PubMed] [Google Scholar]
- Wothke W. Longitudinal modeling with missing data. In: Little TD, Schnabel KU, Baumert J, editors. Modeling longitudinal and multilevel data: Practical issues, applied approaches, and specific examples. Mahwah, NJ: Lawrence Erlbaum Associates; 2000. pp. 219–240. [Google Scholar]
- Young SE, Corley RP, Stallings MC, Rhee SH, Crowley TJ, Hewitt JK. Substance use, abuse and dependence in adolescence: prevalence, symptom profiles and correlates. Drug and Alcohol Dependence. 2002;68(3):309–322. doi: 10.1016/s0376-8716(02)00225-9. [DOI] [PubMed] [Google Scholar]
- Yu S, Clemens R, Yang H, Li X, Stanton B, Deveaux L, Harris C. Youth and parental perceptions of parental monitoring and parent-adolescent communication, youth depression, and youth risk behaviors. Social Behavior and Personality. 2006;34(10):1297–1310. [Google Scholar]
- Zucker RA, Donovan JE, Masten AS, Mattson ME, Moss HB. Early developmental processes and the continuity of risk for underage drinking and problem drinking. Pediatrics. 2008;121(Supplement 4):S252–S272. doi: 10.1542/peds.2007-2243B. [DOI] [PMC free article] [PubMed] [Google Scholar]