Abstract
Background:
Hip arthroscopic surgery is a rapidly growing procedure, but it may be associated with a steep learning curve. Few studies have used patient-reported outcome (PRO) surveys to investigate the relationship between surgeon experience and patient outcomes after the arthroscopic treatment of femoroacetabular impingement (FAI).
Hypothesis:
Patients undergoing hip arthroscopic surgery for the treatment of FAI in the early stages of a surgeon’s career will have significantly worse outcomes and longer procedure times compared with patients treated after the surgeon has gained experience.
Study Design:
Cohort study; Level of evidence, 2.
Methods:
Patients undergoing hip arthroscopic surgery for FAI and labral injuries were prospectively enrolled during a sports medicine fellowship–trained surgeon’s first 15 months of practice. Patients were stratified into an early group, consisting of the first 30 consecutive cases performed by the surgeon, and a late group, consisting of the second 30 consecutive cases. Radiographic and physical examinations were performed preoperatively and postoperatively. PRO surveys, including the 12-item Short Form Health Survey (SF-12), the modified Harris Hip Score (mHHS), and the Hip disability and Osteoarthritis Outcome Score (HOOS), were administered preoperatively and at a minimum of 1 year postoperatively.
Results:
There was no difference between the early and late groups for patient age (37.2 ± 11.5 vs 35.3 ± 10.8 years, respectively; P = .489), body mass index (25.6 ± 4.0 vs 25.1 ± 4.5 kg/m2, respectively; P = .615), or sex (P = .465). There was a significantly increased procedure time (119.3 ± 21.0 vs 99.0 ± 28.6 minutes, respectively; P = .002) and traction time (72.7 ± 21.4 vs 59.0 ± 16.7 minutes, respectively; P = .007) in the early group compared with the late group. Mean postoperative PRO scores significantly improved in both groups compared with preoperative values for all surveys except for the SF-12 mental component summary. No differences were found in PRO score improvements or complication rates between the early and late groups.
Conclusion:
The total procedure time and traction time decrease after a surgeon’s first 30 hip arthroscopic surgery cases for FAI and labral tears, but patient outcomes can similarly improve regardless of surgeon experience in the early part of his or her career.
Keywords: hip arthroscopic surgery, FAI, surgeon experience, patient outcomes
Hip arthroscopic surgery is a growing surgical procedure that is used to treat a variety of debilitating hip conditions, including acetabular labral tears and femoroacetabular impingement (FAI).2 Multiple studies have shown the benefit of hip arthroscopic surgery to treat FAI based on improvements in postoperative patient-reported outcomes (PROs) using surveys that assess hip pain and functionality.2,10,12 The incidence of hip arthroscopic surgery performed from 2006 to 2010 has increased by over 600% based on an analysis of the American Board of Orthopaedic Surgery database.3 Additionally, a retrospective cross-sectional analysis revealed a 250% increase in hip arthroscopic surgery procedures from 2007 to 2011 in the United States in patients across all age groups.35 The rapidly increasing trend of hip arthroscopic surgery suggests an increased awareness of diagnoses in patients who may benefit from the procedure and also an increased emphasis in training new surgeons to be well versed in this technique.7
Hip arthroscopic surgery is a challenging procedure because of the spatial constraints of the joint and its surrounding capsule, demanding a high level of technical proficiency.24,25 Few studies have investigated the relationship between surgeon experience and patient outcomes for newly trained surgeons because data are rarely collected from their first surgery. Two studies of FAI demonstrated that complication rates in hip arthroscopic surgery decreased with experience31 and that lower complication rates occurred with a newly trained surgeon under supervision compared with a newly trained unsupervised surgeon, suggesting a need for supervision early in a surgeon’s career.9 However, a retrospective study of a single surgeon’s experience found that there was no significant change in the incidence of complications based on surgeon experience.36 Because overall complication rates of hip arthroscopic surgery are low,20 measuring PROs may provide a better understanding of a patient’s pain and functional status postoperatively.34 Konan et al19 assessed a single surgeon’s experience by analyzing Non-Arthritic Hip Score (NAHS), operation time, and complication rate and estimated that there was a learning curve of approximately 30 cases, as there was an increase in postoperative NAHS values between the early and late cases. An additional study by Lee et al22 investigated a surgeon’s experience using the modified Harris Hip Score (mHHS) and concluded that the surgeon required approximately 20 cases to achieve satisfactory mHHS value improvements.
Because of the small number of studies using PRO surveys to investigate surgeon experience and patient outcomes, it is unclear whether a newly trained surgeon’s early hip arthroscopic surgery cases will have different outcomes than the surgeon’s later cases. We aimed to conduct a prospective analysis of a sports medicine fellowship–trained surgeon’s first independently performed hip arthroscopic surgery cases in practice to evaluate the relationship between surgeon experience and patient outcomes for the arthroscopic treatment of FAI. The primary outcomes measured in this study were PRO scores, and secondary outcomes included operation times and complication rates. We hypothesized that the early group of patients would have significantly worse PRO scores and an increased number of complications as well as longer procedure and traction times compared with the later group of patients.
Methods
Patient Selection and Data Collection
Patients undergoing hip arthroscopic surgery for symptomatic FAI by a single sports medicine fellowship–trained orthopaedic surgeon (A.L.Z.) were prospectively enrolled. The surgeon completed fellowship training at the same institution before his appointment as faculty, but hip arthroscopic surgery training was not emphasized during his fellowship, as there was not a previous faculty member who specialized in sports injuries of the hip. All patients provided consent before enrollment, and the study protocol was reviewed and approved by the institutional review board. Inclusion criteria consisted of patients diagnosed with symptomatic pincer, cam, or mixed-type FAI with failure of conservative management and physical therapy. Although all except 1 patient also had labral abnormalities, this finding was not a specific inclusion criterion. Intra-articular injections were used for diagnostic and therapeutic purposes before arthroscopic surgery, but this was also not a strict inclusion criterion as some patients refused injections and elected for surgical treatment after failing physical therapy. Exclusion criteria included patients with hip dysplasia, osteoarthritis, hypermobility, and non-FAI surgery.
During the surgeon’s first 15 months of practice, 62 cases of arthroscopic FAI treatment were performed on patients who met the inclusion and exclusion criteria. All cases were performed without assistance or supervision by other faculty. Postoperatively, 2 patients were lost to follow-up (patients 43 and 46). The remaining 60 cases were divided into an “early” group, consisting of the first 30 consecutive cases performed by the surgeon, and a “late” group, consisting of the second 30 cases. Groups were stratified to 30 cases each based on previous studies of hip arthroscopic surgery that determined that a surgeon requires approximately 30 cases to demonstrate improved operating efficiency and lower complication rates.19,37 However, the true cutoff point for improvement has yet to be validated in the literature because of the limited number of studies that examine surgeon hip arthroscopic surgery experience with PROs as a primary measure.14 Therefore, we decided to explore 30 cases as the cutoff number in our study that includes PROs as a primary measure in FAI treatment.
There were 58 primary cases as well as 2 revision cases of primary hip arthroscopic surgery performed at outside institutions (1 in the early group and 1 in the late group). All postoperative data were analyzed at 1-year follow-up. A 1-year follow-up was utilized because of previous studies demonstrating that the minimal clinically important difference and substantial clinical benefit after the arthroscopic treatment of FAI were achieved within 1 year of surgery.28,29 Patient demographics such as age, sex, and body mass index were recorded. The radiographic evaluation for all patients included preoperative and postoperative radiographs of the pelvis in the supine anterior-posterior plane, Dunn lateral 45° views, and preoperative magnetic resonance imaging of the affected hip.32 The surgeon conducted a detailed physical examination on affected hips preoperatively and at the time of latest follow-up in the clinical setting.
Surgical Procedure
All hip arthroscopic surgery procedures were performed in the ambulatory surgery center of a tertiary referral academic center. The patient was placed supine on the operating table, and the indicated hip was placed in traction.6,17 The physician used 2 portals during the procedure (anterolateral and midanterior). Intraoperative data that were recorded included procedures performed, total procedure time (skin incision to skin closure), and traction time. Intraoperative grading of the acetabular cartilage condition, femoral cartilage condition, and labrum condition was performed based on the classification of Beck et al.1 Fluoroscopy was used to visualize portal placement and to confirm adequate cam and/or pincer resection. The surgeon utilizes limited capsulotomy and does not regularly perform capsular repair. Any intraoperative and postoperative complications were also recorded. Postoperatively, patients were restricted to touchdown weightbearing for 2 weeks without bracing. Patients attended postoperative physical therapy for 12 to 20 weeks.
Patient-Reported Outcomes
PRO scores were prospectively collected for each patient preoperatively and at 3 months, 6 months, and 1 year after surgery. Patients completed 3 PRO surveys: the 12-item Short Form Health Survey (SF-12), the mHHS, and the Hip disability and Osteoarthritis Outcome Score (HOOS). These PRO surveys have been validated in past studies of hip arthroscopic surgery outcomes to assess a patient’s pain, functional status, and quality of life.18,34 The SF-12 contains a physical component summary (PCS) and a mental component summary (MCS) to assess general health-related quality of life.11,15,16,38 The mHHS produces a single score assessing hip function.5,13 The HOOS has 5 subscales: symptoms, pain, activities of daily living (ADL), sport, and quality of life (QOL).26,27 In addition, patients rated their pain preoperatively and postoperatively on a visual analog scale (VAS) from 0 to 10, with 0 referring to no pain and 10 referring to the most pain. All data were collected in REDCap (version 7.0.19; Vanderbilt University).
Statistical Analysis
An a priori power analysis was performed based on results of a previous study that used similar PROs in hip arthroscopic surgery as their main outcome of interest.8 To adequately power the study to 1 – β = 0.80, it was found that 21 patients were needed for each group for the mHHS and 19 patients needed for each group for the HOOS.8 An unpaired Student t test was used to calculate statistical significance between preoperative and postoperative values, significance in the change in preoperative and postoperative scores between the early and late groups, and significance in demographic variables. A Pearson chi-square test was used to assess significance between categorical variables such as sex, affected hip side, and impingement type (cam, pincer, or mixed). A P value <.05 was considered statistically significant for all calculations. A post hoc power analysis conducted for the mHHS resulted in a power value of 93%. All statistical computations were conducted in StatPlus:mac (version v6; AnalystSoft Inc). SF-12 scores were calculated, with permission, using RAND VR-12 scoring programs in R software (version 3.4.0; R Foundation for Statistical Computing).
Results
Demographics
Demographic findings are provided in Table 1. A total of 60 hip arthroscopic surgery procedures in 58 patients were included for analysis. Thirty hips each were included in the early and late groups. All patients met a minimum 1-year follow-up, and postoperative data analysis was performed at the 1-year follow-up time point. There was no significant difference between the early and late groups in age (37.2 ± 11.5 vs 35.3 ± 10.8 years, respectively; P = .489), body mass index (25.6 ± 4.0 vs 25.1 ± 4.5 kg/m2, respectively; P = .615), sex (15 female and 15 male vs 13 female and 17 male, respectively; P = .465), involved hip side (P = .715), or isolated cam versus mixed type (there were no cases of isolated pincer type; P = .194).
TABLE 1.
Patient Demographicsa
| Early Group | Late Group | P Valueb | |
|---|---|---|---|
| Age, y | 37.2 ± 11.5 | 35.3 ± 10.8 | .489 |
| Body mass index, kg/m2 | 25.6 ± 4.0 | 25.1 ± 4.5 | .615 |
| Follow-up, mo | 15.5 ± 4.7 | 13.1 ± 2.7 | .017 |
| Sex, n | .465 | ||
| Female | 15 | 13 | |
| Male | 15 | 17 | |
| Side involved, n | .715 | ||
| Left | 15 | 14 | |
| Right | 15 | 16 | |
| Type of femoroacetabular impingement, n | .194 | ||
| Cam | 16 | 11 | |
| Mixed (cam + pincer) | 14 | 19 |
aValues are presented as mean ± SD unless otherwise specified.
bStudent unpaired-samples t test for means and chi-square test for categorical values.
Radiographic Findings
Radiographic findings are provided in Table 2. Preoperatively to postoperatively, there was a significant decrease in both the early and late groups for alpha angle (61.6° ± 7.0° to 46.6° ± 2.4° [P < .0001] vs 59.8° ± 3.8° to 46.5° ± 3.4° [P < .0001], respectively) and lateral center-edge angle (LCEA) (36.7° ± 6.4° to 30.3° ± 3.9° [P < .0001] vs 34.1° ± 7.2° to 28.2° ± 3.4° [P = .0003], respectively). There was no change between the preoperative and postoperative Tönnis grades in either group. In the early and late groups, 59 hips had a labral injury in addition to FAI. There was no significant difference in the change (difference between postoperative and preoperative values) in alpha angle and the change in LCEA between the early and late groups (Table 3).
TABLE 2.
Radiographic and Physical Examination Findingsa
| Preoperative | Postoperative | P Valueb | |
|---|---|---|---|
| Early group | |||
| Alpha angle, deg | 61.6 ± 7.0 | 46.6 ± 2.4 | <.0001 |
| LCEA, deg | 36.7 ± 6.4 | 30.3 ± 3.9 | <.0001 |
| Tönnis grade | 0.8 ± 0.6 | 0.7 ± 0.6 | .832 |
| Crossover sign (+), n | 4 | 1 | .160 |
| Flexion, deg | 115.9 ± 6.3 | 118.4 ± 4.8 | .085 |
| Extension, deg | 8.4 ± 3.6 | 9.3 ± 2.6 | .296 |
| Internal rotation, deg | 15.2 ± 8.2 | 27.1 ± 5.4 | <.0001 |
| External rotation, deg | 49.8 ± 7.1 | 46.6 ± 6.0 | .064 |
| FADIR (+), n | 29 | 4 | |
| Log roll (+), n | 1 | 0 | |
| FABER (+), n | 3 | 1 | |
| Ober (+), n | 0 | 0 | |
| Straight leg (+), n | 0 | 1 | |
| Stinchfield (+), n | 24 | 2 | |
| Neurovascular status (abnormal), n | 0 | 0 | |
| Gait (antalgic), n | 2 | 1 | |
| Tenderness (+), n | 1 | 0 | |
| Late group | |||
| Alpha angle, deg | 59.8 ± 3.8 | 46.5 ± 3.4 | <.0001 |
| LCEA, deg | 34.1 ± 7.2 | 28.2 ± 3.4 | .0003 |
| Tönnis grade | 0.5 ± 0.5 | 0.4 ± 0.5 | .445 |
| Crossover sign (+), n | 11 | 2 | .004 |
| Flexion, deg | 113.4 ± 11.2 | 118.0 ± 4.8 | .052 |
| Extension, deg | 9.6 ± 3.3 | 9.8 ± 0.9 | .786 |
| Internal rotation, deg | 19.5 ± 5.8 | 28.0 ± 3.7 | <.0001 |
| External rotation, deg | 45.0 ± 6.7 | 46.1 ± 2.5 | .431 |
| FADIR (+), n | 28 | 4 | |
| Log roll (+), n | 3 | 1 | |
| FABER (+), n | 4 | 2 | |
| Ober (+), n | 1 | 1 | |
| Straight leg (+), n | 1 | 1 | |
| Stinchfield (+), n | 20 | 3 | |
| Neurovascular status (abnormal), n | 0 | 0 | |
| Gait (antalgic), n | 4 | 0 | |
| Tenderness (+), n | 0 | 1 |
aValues are presented as mean ± SD unless otherwise specified. FABER, flexion, abduction, and external rotation; FADIR, flexion, adduction, and internal rotation; LCEA, lateral center-edge angle.
bStudent unpaired-samples t test for means and chi-square test for categorical values.
TABLE 3.
Change in Radiographic, Physical Examination, and Patient-Reported Outcome Findingsa
| Early Group | Late Group | P Valueb | |
|---|---|---|---|
| Radiographic findings | |||
| Change in alpha angle, deg | –15.0 ± 7.2 | –13.3 ± 4.4 | .268 |
| Change in LCEA, deg | –6.4 ± 6.0 | –5.9 ± 6.5 | .728 |
| Physical examination findings | |||
| Change in flexion, deg | 2.6 ± 7.4 | 4.6 ± 9.7 | .374 |
| Change in extension, deg | 0.9 ± 3.3 | 0.2 ± 3.5 | .449 |
| Change in internal rotation, deg | 11.9 ± 7.7 | 8.6 ± 5.8 | .070 |
| Change in external rotation, deg | –3.3 ± 7.7 | 1.1 ± 6.4 | .024 |
| Patient-reported outcome scores | |||
| Change in VAS pain | –2.1 ± 3.1 | –2.2 ± 2.4 | .921 |
| Change in SF-12 PCS | 12.1 ± 13.8 | 12.2 ± 13.8 | .970 |
| Change in SF-12 MCS | 7.5 ± 16.4 | 0.7 ± 10.5 | .077 |
| Change in mHHS | 20.2 ± 24.4 | 20.7 ± 24.7 | .940 |
| Change in HOOS- symptoms | 17.5 ± 25.4 | 19.8 ± 25.3 | .741 |
| Change in HOOS-pain | 18.7 ± 22.1 | 23.3 ± 26.9 | .487 |
| Change in HOOS-ADL | 21.0 ± 21.4 | 20.3 ± 25.0 | .917 |
| Change in HOOS-sport | 29.5 ± 32.1 | 29.9 ± 31.6 | .963 |
| Change in HOOS-QOL | 35.3 ± 30.9 | 36.6 ± 36.3 | .886 |
aValues are presented as mean ± SD. ADL, activities of daily living; HOOS, Hip disability and Osteoarthritis Outcome Score; LCEA, lateral center-edge angle; MCS, mental component summary; mHHS, modified Harris Hip Score; PCS, physical component summary; QOL, quality of life; SF-12, 12-item Short Form Health Survey; VAS, visual analog scale.
bStudent unpaired-samples t test.
Physical Examination Findings
Physical examination findings are provided in Table 2. The preoperative to postoperative passive range of motion was significantly improved only for internal rotation in both the early and late groups (15.2° ± 8.2° to 27.1° ± 5.4° [P < .0001] vs 19.5° ± 5.8° to 28.0° ± 3.7° [P < .0001], respectively). There was no significant improvement in preoperative to postoperative hip flexion, extension, and external rotation or strength in flexion, extension, abduction, or adduction for the early and late groups. There was no significant difference in the change in passive range of motion between the early and late groups for flexion, extension, and internal rotation; however, the change in external rotation in the early group was significantly worse compared with the late group (–3.3° ± 7.7° vs 1.1° ± 6.4°, respectively; P = .024) (Table 3).
Intraoperative Findings and Complications
Intraoperative findings are provided in Table 4. In the early group compared with the late group, there was a significant increase in procedure time (119.3 ± 21.0 vs 99.0 ± 28.6 minutes, respectively; P = .002) and traction time (72.7 ± 21.4 vs 59.0 ± 16.7 minutes, respectively; P = .007). Four postoperative complications in the form of transient neurapraxia were reported in the study (6.7%). The early group had 1 case of lateral femoral cutaneous nerve palsy and 1 case of pudendal nerve palsy. The late group suffered 2 cases of lateral femoral cutaneous nerve palsy. All neurapraxia complications resolved within 4 weeks. One patient in the early group required revision labral repair 1 year postoperatively after suffering a new traumatic injury (1.7%). No patients converted to total hip arthroplasty, and no deep vein thrombosis occurred in this cohort.
TABLE 4.
Intraoperative Findingsa
| Early Group | Late Group | P Valueb | |
|---|---|---|---|
| Procedure time, min | 119.3 ± 21.0 | 99.0 ± 28.6 | .002 |
| Traction time, min | 72.7 ± 21.4 | 59.0 ± 16.7 | .007 |
| Acetabular cartilage grade, median | 2 | 3 | |
| Femoral cartilage grade, median | 2 | 2 | |
| Labrum grade, median | 3 | 3 | |
| Wave sign (+), n | 16 | 19 | |
| Cam resection (femoroplasty), n | 30 | 30 | |
| Pincer resection (acetabuloplasty), n | 14 | 19 | |
| Labral repair, n | 27 | 28 | |
| Labral debridement, n | 2 | 2 | |
| Microfracture, n | 1 | 0 |
aValues are presented as mean ± SD unless otherwise specified.
bStudent unpaired-samples t test for means and chi-square test for categorical values.
Patient-Reported Outcomes
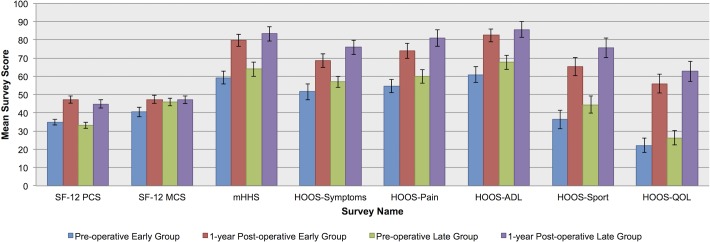
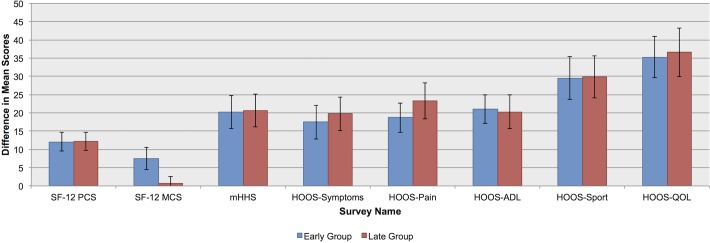
Preoperative and 1-year postoperative PRO findings are provided in Table 5 and Figure 1. There was a significant improvement from preoperative to postoperative scores in both the early and late groups for the VAS pain, SF-12 PCS, mHHS, HOOS-symptoms, HOOS-pain, HOOS-ADL, HOOS-sport, and HOOS-QOL (all P ≤ .005). There was no change in the SF-12 MCS. There was no significant difference in the change in PRO scores between the early and late groups for all PRO surveys (Table 3 and Figure 2). Two patients in the early group and 3 patients in the late group did not complete either a preoperative or postoperative PRO survey, and their data were excluded from the respective change in PRO score analysis.
TABLE 5.
Patient-Reported Outcome Scoresa
| Preoperative | Postoperative | P Valueb | |
|---|---|---|---|
| Early group | |||
| VAS pain | 4.6 ± 2.7 | 2.3 ± 2.0 | .0008 |
| SF-12 PCS | 35.0 ± 8.8 | 47.4 ± 11.3 | <.0001 |
| SF-12 MCS | 40.5 ± 14.1 | 47.4 ± 11.9 | .051 |
| mHHS | 59.3 ± 19.6 | 79.8 ± 19.0 | .0002 |
| HOOS-symptoms | 51.6 ± 24.0 | 68.7 ± 21.0 | .005 |
| HOOS-pain | 54.8 ± 20.1 | 74.0 ± 22.4 | .001 |
| HOOS-ADL | 60.9 ± 24.1 | 82.5 ± 20.0 | .0005 |
| HOOS-sport | 36.3 ± 27.2 | 65.2 ± 27.0 | .0002 |
| HOOS-QOL | 22.2 ± 21.2 | 56.0 ± 28.0 | <.0001 |
| Late group | |||
| VAS pain | 4.0 ± 2.5 | 1.8 ± 2.6 | .002 |
| SF-12 PCS | 33.1 ± 9.1 | 44.9 ± 13.2 | .0003 |
| SF-12 MCS | 46.0 ± 11.9 | 47.2 ± 11.7 | .720 |
| mHHS | 64.0 ± 21.7 | 83.3 ± 21.4 | .001 |
| HOOS-symptoms | 57.1 ± 17.0 | 75.9 ± 21.0 | .0005 |
| HOOS-pain | 59.9 ± 19.8 | 81.1 ± 25.1 | .0009 |
| HOOS-ADL | 67.7 ± 21.0 | 85.6 ± 23.8 | .004 |
| HOOS-sport | 44.5 ± 25.2 | 75.6 ± 28.9 | <.0001 |
| HOOS-QOL | 26.3 ± 21.5 | 62.7 ± 29.8 | <.0001 |
aValues are presented as mean ± SD. ADL, activities of daily living; HOOS, Hip disability and Osteoarthritis Outcome Score; MCS, mental component summary; mHHS, modified Harris Hip Score; PCS, physical component summary; QOL, quality of life; SF-12, 12-item Short Form Health Survey; VAS, visual analog scale.
bStudent unpaired-samples t test.
Figure 1.
Comparison of preoperative and postoperative patient-reported outcome (PRO) scores for the early and late groups after hip arthroscopic surgery. The error bars indicate SD. Mean postoperative PRO scores improved significantly from the preoperative scores in both groups for the 12-item Short Form Health Survey (SF-12) physical component summary (PCS), modified Harris Hip Score (mHHS), and all 5 subscales of the Hip disability and Osteoarthritis Outcome Score (HOOS) but did not significantly improve for the SF-12 mental component summary (MCS). ADL, activities of daily living; QOL, quality of life.
Figure 2.
Comparison of change (difference between postoperative and preoperative values) in patient-reported outcome scores for the early and late groups after hip arthroscopic surgery. The error bars indicate SD. The change in scores was not statistically significant for the 12-item Short Form Health Survey (SF-12) physical component summary (PCS) or mental component summary (MCS), modified Harris Hip Score (mHHS), or all 5 subscales of the Hip disability and Osteoarthritis Outcome Score (HOOS). ADL, activities of daily living; QOL, quality of life.
Discussion
Hip arthroscopic surgery is technically challenging but offers advantages compared with open surgery for FAI because of its minimally invasive nature.21,30 As previous studies have noted a steep learning curve for hip arthroscopic surgery,9,19,22,31 the purpose of this study was to prospectively evaluate the relationship between surgeon experience and patient outcomes for hip arthroscopic surgery in the setting of FAI. We found that although the total procedure time and traction time may decrease after a surgeon’s first 30 hip arthroscopic surgery cases for FAI and labral tears, PROs can improve regardless of surgeon experience.
The significantly decreased total procedure time and traction time in the late group compared with the early group indicated that accrued surgeon experience after 30 cases affected operating room efficiency. The decreased total procedure time is consistent with the learning curve study findings of Konan et al19 and Lee et al.22 Complication rates in our study were similar between the early and late groups (6.7%), which differed from previous studies that showed a higher complication rate in a newly trained surgeon’s first set of cases.9,19,31 One reason for this finding may be that although increased operative time has been associated with increased complications in hip arthroscopic surgery, it is traction time longer than 2 hours that has been most closely linked with postoperative complications.4,23 In our study, although traction time was longer in the early group by a mean of 14 minutes compared with the late group, it was still well below 2 hours (averaging 73 minutes). This may support the low complication rates in both the early and late groups despite longer procedure and traction times for this surgeon’s first 30 cases.
Further, to our knowledge, no previous studies of surgeon experience have evaluated the relationship of traction time and multiple PRO surveys on the arthroscopic treatment of FAI. Our results demonstrate that although operation and traction times decreased with surgeon experience, PRO scores improved in a similar manner after hip arthroscopic surgery in both the early and late groups. When examining PRO scores, Konan et al19 and Lee et al22 also demonstrated improved preoperative to postoperative scores in both early and late surgery groups. However, patients had higher postoperative NAHS values19 or had lower defined failure rates on the mHHS22 as the surgeon gained experience, which the studies attributed to the learning curve. In our study, the late group demonstrated a similar change in PRO scores compared with the early group. Therefore, we cannot conclude that the late group had superior PRO scores. Our study used the mean change in preoperative and postoperative scores to measure improvement, which differs from many studies that compared only postoperative PRO scores.10,12,19,22 Evaluating the mean change in values may be a better way of illustrating improvement because if the patient started at a lower preoperative score, this method captures his or her progress regardless of the final postoperative score. Additionally, our study benefited from the use of multiple PRO surveys instead of one and only evaluated patients treated for FAI and labral injuries.
The improvement from preoperative to postoperative PRO scores in our study was similar to other hip arthroscopic surgery studies for FAI treatment. For example, the mean change for the early and late groups in SF-12 PCS (12.1 and 12.2, respectively) and SF-12 MCS (7.5 and 0.7, respectively) scores were superior when compared with the change in SF-12 PCS (8.8) and SF-12 MCS (3.3) scores in a study for FAI treatment in female patients at 6-month follow-up.33 The late group’s slim change of 0.7 points in the SF-12 MCS score is reflective of the group’s high mean preoperative score of 46.0 (compared with the early group’s mean preoperative score of 40.5), which limited the amount of attainable postoperative improvement. The mean change in the mHHS score for the early and late groups (20.2 and 20.7, respectively) were comparable with the Nwachukwu et al29 study, in which the mean change in the mHHS score was 21.2 at 1-year follow-up. Additionally, the early and late groups’ mean changes in HOOS-symptoms (17.5 and 19.8, respectively), HOOS-pain (18.7 and 23.3, respectively), HOOS-ADL (21.0 and 20.3, respectively), HOOS-sport (29.5 and 29.9, respectively), and HOOS-QOL (35.3 and 36.6, respectively) scores were similar to the mean changes in HOOS-symptoms (23.6), HOOS-pain (20.1), HOOS-ADL (22.4), HOOS-sport (23.3), and HOOS-QOL (22.2) scores at a minimum 1-year follow-up in a study of FAI treatment8 in patients over the age of 25 years. Furthermore, the improvements in preoperative to postoperative PRO scores at 1-year follow-up in this study were comparable with 2-year follow-up studies of FAI treatment.2,12 For example, the early and late groups’ mean changes in the mHHS score (20.2 and 20.7, respectively) were similar to the mean changes in the mHHS score seen in the studies with 2-year follow-up (20.72 and 22.812).
Various factors in our study may explain why our PRO results differ from the other studies of surgeon experience in hip arthroscopic surgery.19,22 The surgeon in this study continued as an attending surgeon at the same institution where he completed his fellowship training. Transitioning to the start of his practice within a familiar environment may have been beneficial compared with surgeons who begin their career after fellowship training at a new institution. In addition, familiarity with operating room staff and equipment may have added to improved surgical conditions. Another factor may be the high volume of cases (N = 62) that the surgeon performed during his first 15 months of practice. The surgeon in the Konan et al19 study averaged around 17 surgeries a year for the first 100 cases, performed over 6 years, and in the Lee et al22 study, the surgeon performed 40 consecutive surgeries in 2 years. A systematic review of high- versus low-volume surgeons performing shoulder arthroplasty and arthroscopic rotator cuff repair supports the phenomenon that low-volume surgeons have worse outcomes compared with high-volume surgeons.39 Therefore, although our study demonstrates that surgeons may have successful outcomes performing hip arthroscopic surgery in the early phase of their career, performing these procedures on a regular basis may be an important factor for positive results. Further studies are needed to determine the relationship between hip arthroscopic surgery case volume and patient outcomes.
Limitations
The main limitation of this study was the use of a single surgeon’s experience. While this can standardize certain confounders such as surgical technique and equipment used, the results may be highly dependent on the training and skill level of the surgeon. Larger studies analyzing PRO data in multiple newly trained surgeons need to be conducted to determine if our results are unique to the surgeon in our study. Another limitation of our study was the small cohort of 30 cases in each group. However, this study had sufficient statistical power for preoperative to postoperative PRO scores in both groups, confirmed by a priori and post hoc power analyses. No study has determined the exact number of cases that a surgeon requires to become proficient in arthroscopic FAI treatment. This study used 30 cases as a cutoff point based on previous studies of surgeon experience and hip arthroscopic surgery.19,37 More studies are necessary to investigate the true cutoff number, and our results indicate that it may be less than 30 cases. Additionally, our study’s minimum 1-year follow-up prevented us from examining long-term outcomes after hip arthroscopic surgery. However, based on previous studies, patients undergoing hip arthroscopic surgery have been shown to achieve the minimal clinically important difference and substantial clinical benefit by 1 year postoperatively.28,29 Future longitudinal studies are needed to investigate the risk for revision surgery or conversion to total hip arthroplasty based on surgeon experience.
Conclusion
The total procedure time and traction time may decrease after a surgeon’s first 30 hip arthroscopic surgery cases for FAI and labral tears, but patient outcomes can improve in a similar manner regardless of surgeon experience in the early part of his or her career.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: S.E.F. was the recipient of the 2017 Heiman Fellowship Summer Grant. A.L.Z. was the recipient of the 2016 AOSSM Young Investigator Grant and is a consultant for Stryker.
Ethical approval for this study was obtained from the University of California, San Francisco Human Research Protection Program (approval No. 14-14742).
References
- 1. Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012–1018. [DOI] [PubMed] [Google Scholar]
- 2. Bedi A, Chen N, Robertson W, Kelly BT. The management of labral tears and femoroacetabular impingement of the hip in the young, active patient. Arthroscopy. 2008;24:1135–1145. [DOI] [PubMed] [Google Scholar]
- 3. Bozic KJ, Chan V, Valone FH, Feeley BT, Vail TP. Trends in hip arthroscopy utilization in the United States. J Arthroplasty. 2013;28:140–143. [DOI] [PubMed] [Google Scholar]
- 4. Brumback RJ, Ellison TS, Molligan H, Molligan DJ, Mahaffey S, Schdmidhauser C. Pudendal nerve palsy complicating intramedullary nailing of the femur. J Bone Joint Surg Am. 1992;74:1450–1455. [PubMed] [Google Scholar]
- 5. Byrd JWT. Hip arthroscopy: patient assessment and indications. Instr Course Lect. 2003;52:711–719. [PubMed] [Google Scholar]
- 6. Byrd JWT. Hip arthroscopy: the supine position. Clin Sports Med. 2001;20:703–731. [PubMed] [Google Scholar]
- 7. Colvin AC, Harrast J, Harner C. Trends in hip arthroscopy. J Bone Joint Surg Am. 2012;94:1–5. [DOI] [PubMed] [Google Scholar]
- 8. Cooper AP, Basheer SZ, Maheshwari R, Regan L, Madan SS. Outcomes of hip arthroscopy: a prospective analysis and comparison between patients under 25 and over 25 years of age. Br J Sports Med. 2013;47:234–238. [DOI] [PubMed] [Google Scholar]
- 9. Dietrich F, Ries C, Eiermann C, Miehlke W, Sobau C. Complications in hip arthroscopy: necessity of supervision during the learning curve. Knee Surg Sports Traumatol Arthrosc. 2014;22:953–958. [DOI] [PubMed] [Google Scholar]
- 10. Frank RM, Lee S, Bush-Joseph CA, Salata MJ, Mather RC, Nho SJ. Outcomes for hip arthroscopy according to sex and age: a comparative matched-group analysis. J Bone Joint Surg Am. 2016;98:797–804. [DOI] [PubMed] [Google Scholar]
- 11. Gill SC, Butterworth P, Rodgers B, Mackinnon A. Validity of the mental health component scale of the 12-item Short-Form Health Survey (MCS-12) as measure of common mental disorders in the general population. Psychiatry Res. 2007;152:63–71. [DOI] [PubMed] [Google Scholar]
- 12. Gupta A, Redmond JM, Stake CE, Dunne KF, Domb BG. Does primary hip arthroscopy result in improved clinical outcomes? 2-year clinical follow-up on a mixed group of 738 consecutive primary hip arthroscopies performed at a high-volume referral center. Am J Sports Med. 2016;44:74–82. [DOI] [PubMed] [Google Scholar]
- 13. Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 14. Hoppe DJ, de Sa D, Simunovic N, et al. The learning curve for hip arthroscopy: a systematic review. Arthroscopy. 2014;30:389–397. [DOI] [PubMed] [Google Scholar]
- 15. Jones D, Kazis L, Lee A, et al. Health status assessments using the Veterans SF-12 and SF-36: methods for evaluating outcomes in the Veterans Health Administration. J Ambul Care Manage. 2001;24:68–86. [DOI] [PubMed] [Google Scholar]
- 16. Kazis LE, Miller DR, Skinner KM, et al. Patient-reported measures of health: the Veterans Health Study. J Ambul Care Manage. 2004;27:70–83. [DOI] [PubMed] [Google Scholar]
- 17. Kelly BT, Weiland DE, Schenker ML, Philippon MJ. Arthroscopic labral repair in the hip: surgical technique and review of the literature. Arthroscopy. 2005;21:1496–1504. [DOI] [PubMed] [Google Scholar]
- 18. Kemp JL, Collins NJ, Roos EM, Crossley KM. Psychometric properties of patient-reported outcome measures for hip arthroscopic surgery. Am J Sports Med. 2013;41:2065–2073. [DOI] [PubMed] [Google Scholar]
- 19. Konan S, Rhee SJ, Haddad FS. Hip arthroscopy: analysis of a single surgeon’s learning experience. J Bone Joint Surg Am. 2011;93:52–56. [DOI] [PubMed] [Google Scholar]
- 20. Kowalczuk M, Bhandari M, Farrokhyar F, et al. Complications following hip arthroscopy: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2013;21:1669–1675. [DOI] [PubMed] [Google Scholar]
- 21. Kuhns BD, Frank RM, Pulido L. Open and arthroscopic surgical treatment of femoroacetabular impingement. Front Surg. 2015;2:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lee YK, Ha YC, Hwang DS, Koo KH. Learning curve of basic hip arthroscopy technique: CUSUM analysis. Knee Surg Sports Traumatol Arthrosc. 2013;21:1940–1944. [DOI] [PubMed] [Google Scholar]
- 23. Lo YP, Chan YS, Lien LC, Lee MS, Hsu KY, Shih CH. Complications of hip arthroscopy: analysis of seventy three cases. Chang Gung Med. 2006;29:86–92. [PubMed] [Google Scholar]
- 24. Logishetty K, Bedi A, Ranawat AS. The role of navigation and robotic surgery in hip arthroscopy. Oper Tech Orthop. 2010;20:255–263. [Google Scholar]
- 25. McCarthy JC, Lee JA. History of hip arthroscopy: challenges and opportunities. Clin Sports Med. 2011;30:217–224. [DOI] [PubMed] [Google Scholar]
- 26. Nilsdotter AK, Bremander A. Measures of hip function and symptoms: Harris Hip Score (HHS), Hip Disability and Osteoarthritis Outcome Score (HOOS), Oxford Hip Score (OHS), Lequesne Index of Severity for Osteoarthritis of the Hip (LISOH), and American Academy of Orthopedic Surgeons (AAOS) Hip and Knee Questionnaire. Arthritis Care Res. 2011;63 (suppl 11):S200–S207. [DOI] [PubMed] [Google Scholar]
- 27. Nilsdotter AK, Lohmander LS, Klässbo M, Roos EM. Hip Disability and Osteoarthritis Outcome Score (HOOS): validity and responsiveness in total hip replacement. BMC Musculoskelet Disord. 2003;4:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Nwachukwu BU, Chang B, Fields K, et al. Defining the ‘substantial clinical benefit’ after arthroscopic treatment of femoroacetabular impingement. Am J Sports Med. 2017;45:1297–1303. [DOI] [PubMed] [Google Scholar]
- 29. Nwachukwu BU, Fields K, Chang B, Nawabi DH, Kelly BT, Ranawat AS. Preoperative outcome scores are predictive of achieving the minimal clinically important difference after arthroscopic treatment of femoroacetabular impingement. Am J Sports Med. 2017;45:612–619. [DOI] [PubMed] [Google Scholar]
- 30. Nwachukwu BU, Rebolledo BJ, McCormick F, Rosas S, Harris JD, Kelly BT. Arthroscopic versus open treatment of femoroacetabular impingement: a systematic review of medium- to long-term outcomes. Am J Sports Med. 2016;44:1062–1068. [DOI] [PubMed] [Google Scholar]
- 31. Park MS, Yoon SJ, Kim YJ, Chung WC. Hip arthroscopy for femoroacetabular impingement: the changing nature and severity of associated complications over time. Arthroscopy. 2014;30:957–963. [DOI] [PubMed] [Google Scholar]
- 32. Pfirrmann CW, Mengiardi B, Dora C, Kalberer F, Zanetti M, Hodler J. Cam and pincer femoroacetabular impingement: characteristic MR arthrographic findings in 50 patients. Radiology. 2006;240:778–785. [DOI] [PubMed] [Google Scholar]
- 33. Pontiff M, Ithurburn MP, Ellis T, Cenkus K, Stasi SD. Pre- and post-operative self-reported function and quality of life in women with and without generalized joint laxity undergiong hip arthroscopy for femoroacetabular impingement. Int J Sports Phys Ther. 2016;11:378–387. [PMC free article] [PubMed] [Google Scholar]
- 34. Safran MR, Hariri S. Hip arthroscopy assessment tools and outcomes. Oper Tech Orthop. 2010;20:264–277. [Google Scholar]
- 35. Sing DC, Feeley BT, Tay B, Vail TP, Zhang AL. Age-related trends in hip arthroscopy: a large cross-sectional analysis. Arthroscopy. 2015;31:2307–2313. [DOI] [PubMed] [Google Scholar]
- 36. Souza BGS, Dani WS, Honda EK, et al. Do complications in hip arthroscopy change with experience? Arthroscopy. 2010;26:1053–1057. [DOI] [PubMed] [Google Scholar]
- 37. Vilchez F, Eriquicia J, Tey M. [Learning curve of arthroscopic hip surgery]. Acta Ortop Mex. 2010;24:177–181. [PubMed] [Google Scholar]
- 38. Ware J, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. [DOI] [PubMed] [Google Scholar]
- 39. Weinheimer KT, Smuin DM, Dhawan A. Patient outcomes as a function of shoulder surgeon volume: a systematic review. Arthroscopy. 2017;33:1273–1281. [DOI] [PubMed] [Google Scholar]