Abstract
Objective
The objective of this study was to compare the analgesic effect and tolerance profile of acupuncture versus intravenous (IV) titrated morphine in patients presenting to the emergency department (ED) with renal colic.
Materials and methods
A total of 115 patients were randomized into two groups. Patients in the IV titrated-morphine group (n=61) received 0.1 mg/kg morphine every 5 minutes until pain score dropped by at least 50% of its baseline value. Patients in the acupuncture group (n=54) received an acupuncture session of 30 minutes following a prespecified protocol. The visual analog scale (VAS) was used to assess pain intensity at baseline and at 10, 20, 30, 45, and 60 minutes following the start of the treatment protocol. Possible treatment side effects were also recorded.
Results
No significant differences were found between the two groups concerning age, sex, or baseline VAS score. From the 10th minute until the end of the intervention, acupuncture was associated with a deeper analgesic effect than titrated morphine (P<0.05 from the 10th minute and over). Analgesia was also faster in the acupuncture group, with time to obtain 50% reduction of baseline VAS of 14 minutes in the acupuncture group versus 28 minutes in the IV titrated-morphine group (P<0.001). Only three patients in the acupuncture group experienced minor side effects versus 42 in the morphine group (P<0.001). No major side effects were observed in this study.
Conclusion
In ED patients with renal colic, acupuncture was associated with a much faster and deeper analgesic effect and a better tolerance profile in comparison with titrated IV morphine.
Keywords: acupuncture, morphine, renal colic
Introduction
Renal colic (RC) is one of the commonest complaints in the emergency department (ED).1,2 It accounts for ~1% of all ED visits and hospitalizations,3 and is more frequent in men.3–5 The prevalence of urinary stones in RC is 10%–15%.6 Pain experienced in the acute phase of RC is often described as “the worst pain ever”,7 making effective pain control a priority in RC management. Currently, analgesics represent the mainstay treatment for this condition, and for many years, opioids have been used as first-line treatment.8,9 However, concerns have been raised about the correlation between opioid dose and side effects, including respiratory depression, gastrointestinal disorders, and hypotension.10 Acupuncture, a branch of traditional Chinese medicine, has been proven to be effective in the management of pain and other acute/chronic conditions, including RC.11,12 However, its application in the ED setting is insufficient and needs further exploration.13 The aim of this study was to compare the analgesic effects and tolerance of acupuncture compared to intravenous (IV) morphine in patients presenting to the ED with RC.
Materials and methods
Study design
This randomized controlled trial was carried out in the ED of Fattouma Bourguiba University Hospital from July 2014 to June 2015. It was registered at ClinicalTrials.gov (NCT02781415). The protocol was approved by the ethics committee of Fattouma Bourguiba University Hospital.
Inclusion criteria
We included all consecutive patients aged >18 years and presenting to the ED with the clinical suspicion of uncomplicated RC and a pain score >70 (ranging from 0 for no pain to 100 for maximum imaginable pain) using the visual analog scale (VAS). RC was considered if the patient description of pain included sudden onset of symptoms; unilateral flank or lower abdomen pain; irradiation to the back, side, or groin region; urination problems, including urinating difficultly and/or an abnormally dark or red urine; and the absence of other obvious conditions explaining patient symptoms.
Exclusion criteria
We excluded patients with complicated RC, defined by the presence of bilateral pain, fever, and/or decreased urine output (<500 mL per day). Patients presenting with post-traumatic pain, those taking anticoagulant medications or with coagulation problems, those with skin afflictions (infections, hematoma, dermatosis) that would impair the use of certain acupuncture points, those unable to assess the degree of pain using the VAS, those who had received analgesics in the 6 hours prior to enrollment, those refusing or unable to give written consent, and pregnant women were also excluded from this study. All participants read and signed the informed consent form of the study, which was approved by the ethics committee of Fattouma Bourguiba University Hospital.
Interventions
Patients were randomly assigned to one of the two study groups using a randomly generated number protocol and sealed envelopes. Patients allocated to the titrated-morphine group received a bolus of 0.1 mg/kg actual body weight of morphine chloral hydrate solution by direct IV route. This solution had been prepared by a study nurse by diluting a 10 mg/1 mL of morphine chloral hydrate in 9 mL solution of serum saline to obtain a 10 mL preparation. A titration dose of 0.1 mg/kg body weight was repeated every 5 minutes until reaching the therapeutic goal.
In the acupuncture group, patients underwent a 30-minute acupuncture session with a licensed physician. Skin was disinfected with chlorhexidine at the needle insertion site. Sterile acupuncture needles were used (0.25×0.5 mm). Patients were installed in a seated position and needles inserted perpendicularly through the skin to a depth of 1–2 cm until deqi, a feeling of numbness and tingling within the range of the acupuncture point, was achieved.14 Insertion sites correspond to the urinary bladder meridian points to the side of the pain (UB21–24, UB26, UB45–49). All details regarding our protocol intervention, assessed by the standards for reporting interventions in controlled trials of acupuncture, are reported in Table S1.
Method of measurement
A 100-mm linear VAS was used to measure pain intensity in all participants. Patients rated their pain just before the intervention and at 10, 20, 30, 45 and 60 minutes after it. Patients were followed during the whole protocol period and until discharge for the occurrence of side effects, including drowsiness, dizziness, nausea and vomiting, respiratory distress, and hypotension in the morphine group and local rash/bleeding, itching, needle blockage, and fainting in the acupuncture group. For all subjects, we collected demographic and clinical data, VAS scores, and potentially treatment-related side effects.
Efficacy outcome
The efficacy of each treatment strategy was judged based on two conditions: success rate in achieving durable analgesia, defined by a drop in VAS score of at least 50% from baseline (T0) at 30 minutes following the start of the protocol and lasting till the end of the intervention (T60), and rapidity in obtaining an analgesic effect, defined by the interval between the start of the protocol (T0) and the decrease in VAS score of at least 50% from baseline.
Safety outcome
Possible adverse events related to the care delivered were investigated via a checklist during the 1-hour protocol treatment and until the patient had been discharged from the ED.
Statistical analysis
Variables are expressed as means ± SD, medians with 25%–75% interquartile range (IQR), or values with 95% CIs as appropriate. The normality of the parameters was tested with the Kolmogorov–Smirnov test. Comparison of data between the groups was performed using a two-sample Student’s t-test or Mann–Whitney U test, as appropriate. All tests were two-tailed, and P<0.05 was considered statistically significant. Calculations were performed with SPSS version 19.
Results
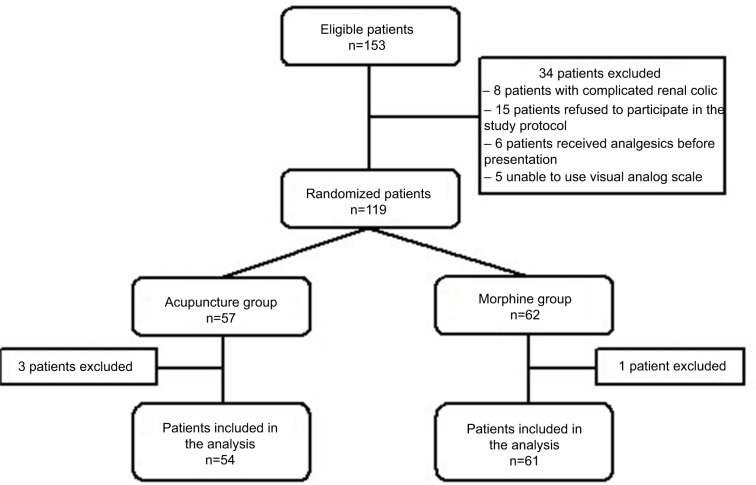
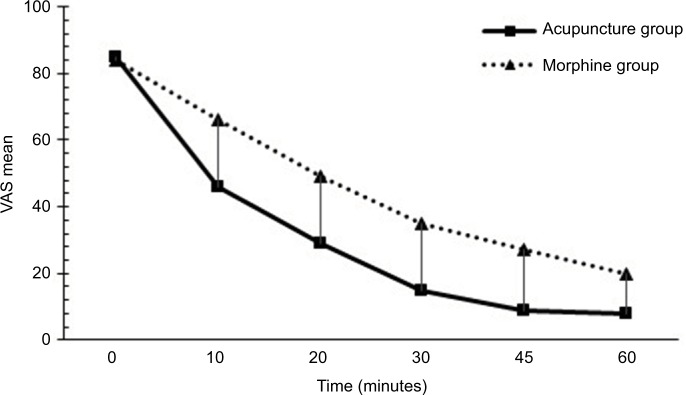
A total of 153 consecutive patients who presented to our ED with signs and symptoms suggestive of RC were screened during the study period. Of these, 19 did not meet the inclusion criteria, and 15 declined to participate in the study. The remaining 119 patients were randomly allocated to two groups: 57 patients in the acupuncture group and 62 in the morphine group. Of these, four patients were lost to follow-up during the study period. Overall, 115 patients completed the present study, and data from all these patients were analyzed (per-protocol analysis), as shown in Figure 1. Baseline characteristics were similar between the two study groups, and there were no differences in age, sex, medical history, or baseline VAS scores between the groups (Table 1). As shown in Table 2, there was a statistically significant decrease in VAS scores in both groups (difference between baseline and after 60 minutes 77 in the acupuncture group and 64 in the morphine group, P<0.001). Success rates were similar between the groups, with 87% of participants achieving the main goal in the acupuncture group and 83% in the morphine group (P=0.6). Mean pain scores were significantly lower in the acupuncture group than in the morphine group from the 10th minute of the protocol start until the 60th minute (P<0.005 at all-time points). Acupuncture was associated with a faster analgesic effect, with time to achieve 50% reduction in baseline pain score being almost half that obtained with morphine in reduction time. In fact, with acupuncture, a 50% reduction in baseline pain score was achieved in half the time taken by morphine (14 versus 28 minutes, P<0.001) (Figure 2). At the end of the 60-minute study period, 24 patients in the morphine group and 35 in the acupuncture group were pain-free (VAS score 0). In this trial, the mean dose of opioids used per participant in the morphine group was 16.7±6 mg of morphine chloral hydrate (10–27 mg). Side effects were observed more frequently in the morphine group than in the acupuncture group (42 versus three, P<0.001). There were no major side effects recorded in this study (Table 3).
Figure 1.
Patient flowchart.
Table 1.
Baseline characteristics of patients
| Characteristics | Acupuncture, n=54 | Morphine, n=61 | P |
|---|---|---|---|
| Age, years | 42±14.8 | 41.8±13.21 | 0.82 |
| Sex, female/male | 28/26 | 26/35 | 0.32 |
| Medical history, n (%) | |||
| Diabetes | 7 (12.9) | 7 (11.4) | 0.8 |
| Hypertension | 8 (14.8) | 7 (11.4) | 0.59 |
| Gastrointestinal ulcer | 2 (3.7) | 4 (6.5) | 0.49 |
| Previous renal colic | 13 (24) | 11 (18) | 0.42 |
| History of urolithiasis | 5 (9.2) | 8 (13.1) | 0.51 |
| Physical examination findings | |||
| Heart rate, bpm | 83±12 | 81±14 | 0.51 |
| Systolic blood pressure, mmHg | 136±27 | 133±20 | 0.42 |
| Diastolic blood pressure, mmHg | 80±21 | 78±12 | 0.62 |
| Oxygen saturation, % | 98±1 | 98±1 | 0.94 |
| Temperature, °C | 36.9±0.3 | 36.9±0.3 | 0.24 |
Table 2.
Main outcomes in the two study groups
| Outcome criteria | Acupuncture, n=54 | Morphine, n=61 | P |
|---|---|---|---|
| VAS at admission, median (IQR) | 83 (77–92) | 85 (75–96) | 0.5 |
| VAS at 60 minutes, median (IQR) | 10 (6–15) | 22 (14–26) | 0.002 |
| Success rate* at 60 minutes, n (%) | 47 (87) | 51 (83) | 0.6 |
| Resolution time** (minutes), mean ± SD | 14.5±7.8 | 28.2±12.4 | <0.001 |
Notes:
Decrease in admission VAS of at least 50%;
time to obtain decrease in VAS of at least 50%.
Abbreviation: IQR, interquartile range; VAS, visual analog scale.
Figure 2.
Visual analog scale (VAS) score over time in patients with renal colic.
Notes: Repeated VAS score analysis showed a significant and greater reduction of pain intensity in the acupuncture group compared to the morphine group from the 10-minute to the 60-minute time points.
Table 3.
Adverse effects
| Outcome criteria | Acupuncture, N=54 | Morphine, N=61 | P |
|---|---|---|---|
| Minor, n | |||
| Drowsiness | 0 | 1 | 0.356 |
| Dizziness | 0 | 26 | <0.001 |
| Nausea and vomiting | 0 | 13 | <0.001 |
| Rash | 0 | 1 | 0.356 |
| Hypotension | 0 | 1 | 0.356 |
| Needle blockage | 1 | 0 | 0.376 |
| Itching/rash/bleeding at insertion point | 2 | 0 | 0.179 |
| Major, n | 0 | 0 | – |
| Total, n | 3 | 42 | <0.001 |
Discussion
Although success rates were similar in both groups, the analgesic effect of acupuncture was significantly faster than that of morphine. Both titrated morphine and acupuncture succeeded in achieving a 50% reduction in baseline VAS scores in most patients with RC; nevertheless, acupuncture was much better tolerated. Through their everyday work, emergency physicians are confronted with a variety of painful conditions, including severe pain syndromes. Alleviating pain represents a health-care priority worldwide.15 RC is often described by patients as “the worst pain ever”. In patients with acute severe pain, opioids tend to be prescribed by ED physicians as first-line treatment.16 Nevertheless, systemic administration of opioids carries a high risk of side effects that correlates with dose given.17 Many other analgesic modalities have been investigated, including such nonpharmacologic pain relief techniques as acupuncture. Acupuncture is growing in popularity worldwide. The World Health Organization stated more than 40 diseases could benefit from acupuncture treatment,18 and recently, many comprehensive review articles have been published regarding this matter,13,19–22 with a particular emphasis on the analgesic effect of acupuncture.23 The effect of this technique on pain is related to the release of endogenous opioids,24 modulation of the adrenergic system,25 the 5-hydroxy tryptamine-signaling system,26 and the N-methyl-d-aspartate-signaling system.27 In addition, acupuncture seems to have an anti-inflammatory effect and to activate the diffuse noxious inhibitory control system.28 Although very few studies have been carried out on the use of acupuncture in the management of severe acute pain, some results are encouraging. In a randomized controlled trial29 of 607 healthy women in labor, Borup et al demonstrated that acupuncture was efficient in relieving pain during delivery and reduced the need for pain medication. In a study comprising 120 patients with acute dental pain30 with a mean baseline VAS score of 65±1.8, Grillo et al showed that acupuncture was a good method to control pain. Goertz et al included 100 patients with acute pain in a protocol comparing auricular acupuncture with standard ED care versus standard ED care alone.31 The mean baseline pain score was 69 in the acupuncture group and 77 in the standard care group. Participants in the acupuncture group experienced a 23% reduction in pain before leaving the ED, while average pain levels in the standard medical care group remained unchanged. In a systematic review article of acupuncture in acute low-back pain patients of 11 randomized controlled trials,21 Lee et al concluded that acupuncture may be more effective than pharmacologic interventions for pain relief. Recently, Kaynar et al included 121 patients with urolithiasis-driven RC in a randomized trial of IV acetaminophen versus acupuncture versus intramuscular diclofenac.32 The authors demonstrated that acupuncture was associated with the most rapid analgesia, and no side effects were observed in this group. They concluded that acupuncture should be considered an alternative treatment modality in specific groups of RC patients with contraindication to nonsteroidal anti-inflammatory drugs and acetaminophen.
Our study had some limitations, which should be stressed. First, it was monocentric with limited sample size. Second, we assessed pain intensity using the VAS, which could be unsuitable for some patients’ conditions. Third, the duration of the protocol was limited to 60 minutes, whereas the beneficial effects of treatments may last longer. Finally, other aspects of pain management were not studied, such as the feasibility of acupuncture in ED settings and its economic impact on both patients and health systems. Of note, results from a recent observational study indicated that acupuncture was acceptable and effective for pain management in ED patients.33 We must also specify that acupuncture needs to be performed by trained practitioners in the particular setting of the ED.
Conclusion
In this study, we demonstrated that the analgesic effect of acupuncture was significantly higher and quicker than titrated morphine in ED patients with RC. This represents an alternative to currently available analgesic drugs, especially in patients with high risk of adverse events. Its place in the ED analgesic armamentarium deserves to be further investigated.
Supplementary material
Table S1.
Quality report of acupuncture intervention
| Style of acupuncture | Local and distal points |
|---|---|
| Technique | Bilateral and unilateral |
| Number of needles | Left to the discretion of the physician, perhaps 2–16 |
| Needling depth | As we felt the deqi, we stopped, as described in traditional texts |
| Deqi | Mentioned |
| Type of stimulation | Manual only |
| Needle retention time | 20 minutes |
| Needle gauge and length | 0.25×50 mm |
| Rationale of acupuncture | TCM diagnosis-based |
| Practitioner’s background | GP registered with Tunisian medical acupuncture society, with >3 years’ acupuncture treatment experience |
| Treatment regimen | For kidney colic only, one session |
| Control intervention | Conventional treatment (morphine) |
| Cointervention | None |
Note: Assessed by the standards for reporting interventions in controlled trials of acupuncture.
Abbreviations: GP, general practitioner; TCM, traditional Chinese medicine.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Scales CD, Smith AC, Hanley JM, Saigal CS. Prevalence of kidney stones in the United States. Eur Urol. 2012;62:160–165. doi: 10.1016/j.eururo.2012.03.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Romero V, Akpinar H, Assimos DG. Kidney stones: a global picture of prevalence, incidence, and associated risk factors. Rev Urol. 2010;12:e86–e96. [PMC free article] [PubMed] [Google Scholar]
- 3.Afshar K, Jafari S, Marks AJ, Eftekhari A, MacNeily AE. Nonsteroidal anti-inflammatory drugs (NSAIDs) and non-opioids for acute renal colic. Cochrane Database Syst Rev. 2015:CD006027. doi: 10.1002/14651858.CD006027.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fisang C, Anding R, Müller SC, Latz S, Laube N. Urolithiasis: an interdisciplinary diagnostic, therapeutic and secondary preventive challenge. Dtsch Arztebl Int. 2015;112:83–91. doi: 10.3238/arztebl.2015.0083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cervellin G, Mora R, Ticinesi A, et al. Epidemiology and outcomes of acute abdominal pain in a large urban emergency department: retrospective analysis of 5,340 cases. Ann Transl Med. 2016;4:362. doi: 10.21037/atm.2016.09.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Claros OR, Silva CH, Consolmagno H, Sakai AT, Freddy R, Fugita OE. Current practices in the management of patients with ureteral calculi in the emergency room of a university hospital. Clinics (Sao Paulo) 2012;5:415–418. doi: 10.6061/clinics/2012(05)02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Holdgate A, Pollock T. Systematic review of the relative efficacy of non-steroidal anti-inflammatory drugs and opioids in the treatment of acute renal colic. BMJ. 2004;7453:1401. doi: 10.1136/bmj.38119.581991.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Holdgate A, Pollock T. Nonsteroidal anti-inflammatory drugs (NSAIDs) versus opioids for acute renal colic. Cochrane Database Syst Rev. 2004:CD004137. doi: 10.1002/14651858.CD004137.pub2. [DOI] [PubMed] [Google Scholar]
- 9.Afshar K, Jafari S, Marks AJ, Eftekhari A, MacNeily AE. Nonsteroidal anti-inflammatory drugs (NSAIDs) and non-opioids for acute renal colic. Cochrane Database Syst Rev. 2015:CD006027. doi: 10.1002/14651858.CD006027.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Engeler DS, Schmid S, Schmid HP. The ideal analgesic treatment for acute renal colic: theory and practice. Scand J Urol Nephrol. 2008;2:137–142. doi: 10.1080/00365590701673716. [DOI] [PubMed] [Google Scholar]
- 11.Kaymar M, Koyuncu F, Buldu I, et al. Comparison of the efficacy of diclofenac, acupuncture, and acetaminophen in the treatment of renal colic. Am J Emerg Med. 2015;33:749–753. doi: 10.1016/j.ajem.2015.02.033. [DOI] [PubMed] [Google Scholar]
- 12.Lee YH, Lee WC, Chen MT, Huang JK, Chung C, Chang LS. Acupuncture in the treatment of renal colic. J Urol. 1992;147:16–18. doi: 10.1016/s0022-5347(17)37121-5. [DOI] [PubMed] [Google Scholar]
- 13.Kim KH, Lee BR, Ryu JH, Choi TY, Yang GY. The role of acupuncture in emergency department settings: a systematic review. Complement Ther Med. 2013;21:65–72. doi: 10.1016/j.ctim.2012.12.004. [DOI] [PubMed] [Google Scholar]
- 14.Zhou W, Benharash P. Significance of “deqi” response in acupuncture treatment: myth or reality. J Acupunct Meridian Stud. 2014;7:186–189. doi: 10.1016/j.jams.2014.02.008. [DOI] [PubMed] [Google Scholar]
- 15.Goldberg DS, McGee SJ. Pain as a global public health priority. BMC Public Health. 2011;11:770. doi: 10.1186/1471-2458-11-770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Golzari SE, Soleimanpour H, Rahmani F, et al. Therapeutic approaches for renal colic in the emergency department: a review article. Anesth Pain Med. 2014;4:e16222. doi: 10.5812/aapm.16222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Knoedler JJ, Lieske JC. Non-steroidal anti-inflammatory drugs for renal colic. Lancet. 2016;387:1971–1972. doi: 10.1016/S0140-6736(16)00745-5. [DOI] [PubMed] [Google Scholar]
- 18.Han JS. Acupuncture analgesia: areas of consensus and controversy. Pain. 2011;152:S41–S48. doi: 10.1016/j.pain.2010.10.012. [DOI] [PubMed] [Google Scholar]
- 19.Derry C, Derry S, McQuay H, Moore RA. Systematic review of systematic reviews of acupuncture published 1996-2005. Clin Med (Lond) 2006;6:381–386. doi: 10.7861/clinmedicine.6-4-381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ernst E, Lee MS, Choi TY. Acupuncture: does it alleviate pain and are there serious risks? A review of reviews. Pain. 2011;152:755–764. doi: 10.1016/j.pain.2010.11.004. [DOI] [PubMed] [Google Scholar]
- 21.Lee JH, Choi TY, Lee MS, Lee HJ, Shin BC, Lee HS. Acupuncture for acute low back pain: a systematic review. Clin J Pain. 2013;29:172–185. doi: 10.1097/AJP.0b013e31824909f9. [DOI] [PubMed] [Google Scholar]
- 22.Manheimer E, White A, Berman B, Forys K, Ernst E. Meta-analysis: acupuncture for low back pain. Ann Intern Med. 2005;142:651–663. doi: 10.7326/0003-4819-142-8-200504190-00014. [DOI] [PubMed] [Google Scholar]
- 23.Zhao ZQ. Neural mechanism underlying acupuncture analgesia. Prog Neurobiol. 2008;85:355–375. doi: 10.1016/j.pneurobio.2008.05.004. [DOI] [PubMed] [Google Scholar]
- 24.Cao X. Scientific bases of acupuncture analgesia. Acupunct Electrother Res. 2002;27:1–14. doi: 10.3727/036012902816026103. [DOI] [PubMed] [Google Scholar]
- 25.Kim SK, Park JH, Bae SJ, et al. Effects of electroacupuncture on cold allodynia in a rat model of neuropathic pain: mediation by spinal adrenergic and serotonergic receptors. Exp Neurol. 2005;195:430–436. doi: 10.1016/j.expneurol.2005.06.018. [DOI] [PubMed] [Google Scholar]
- 26.Chang FC, Tsai HY, Yu MC, Yi PL, Lin JG. The central serotonergic system mediates the analgesic effect of electroacupuncture on zusanli (ST36) acupoints. J Biomed Sci. 2004;11:179–185. doi: 10.1007/BF02256561. [DOI] [PubMed] [Google Scholar]
- 27.Sun RQ, Wang HC, Wan Y, et al. Suppression of neuropathic pain by peripheral electrical stimulation in rats: µ-opioid receptor and NMDA receptor implicated. Exp Neurol. 2004;187:23–29. doi: 10.1016/j.expneurol.2003.12.011. [DOI] [PubMed] [Google Scholar]
- 28.Le Bars D, Villanueva L, Bouhassira D, Willer JC. Diffuse noxious inhibitory controls (DNIC) in animals and in man. Patol Fiziol Eksp Ter. 1992:55–65. [PubMed] [Google Scholar]
- 29.Borup L, Wurlitzer W, Hedegaard M, Kesmodel US, Hvidman L. Acupuncture as pain relief during delivery: a randomized controlled trial. Birth. 2009;36:5–12. doi: 10.1111/j.1523-536X.2008.00290.x. [DOI] [PubMed] [Google Scholar]
- 30.Grillo CM, Wada RS, de Sousa ML. Acupuncture in the management of acute dental pain. J Acupunct Meridian Stud. 2014;7:65–70. doi: 10.1016/j.jams.2013.03.005. [DOI] [PubMed] [Google Scholar]
- 31.Goertz CM, Niemtzow R, Burns SM, Fritts MJ, Crawford CC, Jonas WB. Auricular acupuncture in the treatment of acute pain syndromes: a pilot study. Mil Med. 2006;171:1010–1014. doi: 10.7205/milmed.171.10.1010. [DOI] [PubMed] [Google Scholar]
- 32.Kaynar M, Koyuncu F, Buldu I, et al. Comparison of the efficacy of diclofenac, acupuncture, and acetaminophen in the treatment of renal colic. Am J Emerg Med. 2015;33:749–753. doi: 10.1016/j.ajem.2015.02.033. [DOI] [PubMed] [Google Scholar]
- 33.Reinstein AS, Erickson LO, Griffin KH, et al. Acceptability, adaptation, and clinical outcomes of acupuncture provided in the emergency department: a retrospective pilot study. Pain Med (Malden Mass) 2017;18:169–178. doi: 10.1093/pm/pnv114. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1.
Quality report of acupuncture intervention
| Style of acupuncture | Local and distal points |
|---|---|
| Technique | Bilateral and unilateral |
| Number of needles | Left to the discretion of the physician, perhaps 2–16 |
| Needling depth | As we felt the deqi, we stopped, as described in traditional texts |
| Deqi | Mentioned |
| Type of stimulation | Manual only |
| Needle retention time | 20 minutes |
| Needle gauge and length | 0.25×50 mm |
| Rationale of acupuncture | TCM diagnosis-based |
| Practitioner’s background | GP registered with Tunisian medical acupuncture society, with >3 years’ acupuncture treatment experience |
| Treatment regimen | For kidney colic only, one session |
| Control intervention | Conventional treatment (morphine) |
| Cointervention | None |
Note: Assessed by the standards for reporting interventions in controlled trials of acupuncture.
Abbreviations: GP, general practitioner; TCM, traditional Chinese medicine.