Abstract
Interest in nephrology careers continues to remain low in the USA. Educational innovations that enhance interest in nephrology among medical trainees are being actively studied. While internal medicine (IM) residency programs commonly offer the inpatient nephrology elective to the resident, outpatient nephrology experience is lacking. Understanding the provision of care in outpatient and home dialysis and management of patients with glomerular diseases, chronic kidney disease and kidney transplantation are vital components of an outpatient nephrology rotation. In this review article, we share our experiences in incorporating outpatient nephrology to the IM resident’s elective time. We also present the structure of the nephrology rotations at our programs and suggest several learning opportunities in outpatient nephrology that the training community can provide to medical residents. Strategies to effectively set up an outpatient nephrology rotation are also described. While more educational research on the impact of outpatient nephrology on resident learning and career choices are needed, we encourage a collaborative effort between faculty members in nephrology and the medicine residency programs to provide this unique learning opportunity to IM residents.
Keywords: educational research, elective, medicine resident, nephrology elective, rotation
Introduction
The number of applicants for nephrology fellowship training in the last several years has been dismally low when compared with the available positions [1]. Various educational research studies have recently attempted to identify reasons for the declining interest in nephrology among medical trainees [2–4]. A survey of US non-nephrology internal medicine (IM) subspecialty fellows in 2011 suggested that poor learning experiences and lack of mentorship were some key factors for not considering a career in nephrology [2]. Clinical educators thus have the opportunity and obligation to improve the educational experiences of medical trainees during their exposure to clinical nephrology.
Most nephrology subspecialty electives in IM residency in the USA are based in a teaching hospital. More than half of the 91 nephrology fellowship program directors surveyed in the USA in 2013 described their nephrology elective for IM residents to be a pure inpatient experience [5]. For programs that offered outpatient nephrology experiences only 11% offered several renal clinic experiences (on average one or two clinics per week) during their 4-week nephrology elective and even fewer (8.8%) did so during their 2-week elective [5]. There were no programs offering a 2- or 4-week inpatient rotation with an average of more than two clinics per week [5]. While most of the program directors (89%) agreed that an ideal nephrology elective should provide both inpatient and outpatient experiences, ‘inpatient service needs’, ‘too much work to coordinate outpatient experiences’, ‘lack of resources to rotate medical residents in outpatient hemodialysis unit’ and ‘lack of resources to rotate medical residents in outpatient renal clinics’ were the top four reasons cited for limited exposure to outpatient nephrology among IM residents.
In this review article, we share the various structures of outpatient nephrology rotations at our institutions and also discuss challenges that can be encountered in setting up an outpatient nephrology rotation. We also present strategies to help the educational community and leaders successfully introduce outpatient nephrology curriculum to their trainees and ways to measure outcome or feedback. While our discussions are focused on IM residents, the strategies described here can also be applied to medical student electives. We believe that our article can also offer ideas on educational research and is likely to aid faculty development, especially if faculty members take leadership roles in education of medical trainees and curriculum development.
Learning opportunities and benefits of the outpatient nephrology curriculum
There are several medical disorders (or topics) in nephrology that can be best taught in the outpatient clinic, including evaluation and management of chronic kidney disease (CKD), hypertension, glomerulonephritis, nephrotic syndrome, hematuria, proteinuria and nephrolithiasis. Reviewing the learning objectives as listed in the outpatient nephrology curriculum (Table 1) makes it clear that many of these disorders can be best taught to IM residents in the outpatient setting, and not in the hospital. Exposure to outpatient nephrology during residency also allows IM residents to better evaluate and manage common nephrological conditions that they themselves would encounter in the medicine clinics.
Table 1.
Learning objectives in an outpatient nephrology curriculum
| Competency domain | CKD | Hypertension | Glomerular diseases | Hematuria and proteinuria | Nephrolithiasis | Dialysis therapies and transplantation |
|---|---|---|---|---|---|---|
| Medical Knowledge | Discuss management of diabetic kidney disease, including hypertension control, glycemic control and use of ACE-I/ARB | State targets for blood pressure control based on risk for cardiovascular disease and CKD progression as recommended in the national guidelines | List the different causes of glomerulonephritis and nephrotic syndrome | State the various renal and extra renal causes of gross or microscopic hematuria | Identify risk factors for various stone diseases using data from 24-h urine studies or stone composition | Describe the following dialysis therapies, including how they work, and when they should be offered:
|
| Explain pathophysiology and management of anemia, hyperphosphatemia and secondary hyperparathyroidism in CKD | Compare and contrast the use of antihypertensive drugs including indications, mechanism of action and adverse effects in CKD | Describe the serological work-up and role of kidney biopsy in the diagnosis and prognosis of glomerular diseases | Outline the diagnostic workup of hematuria including imaging and referral to urologist | Discuss the medical options to reduce risk of future stone events | Describe the vascular access options for dialysis and demonstrate knowledge that central catheter is the least preferred access | |
| Summarize indications for use of ACE-I or ARB in hypertension and CKD, and management of adverse effects, i.e. hyperkalemia and AKI | Outline the use of proteinuria as a marker of glomerular injury and discuss clinical implications and therapies to reduce proteinuria | Summarize the important role of dietary and lifestyle changes in preventing stone disease | State common complications of dialysis especially infectious complications and management | |||
| List the contraindications for kidney transplantation by evaluating potential donor and recipient with a nephrologist | ||||||
| Patient care | Provide counseling on prevention of CKD progression, addressing:
|
Define resistant hypertension, list its causes and outline diagnostic workup of resistant hypertension | Review management of glomerulonephritis and nephrotic syndrome, including adverse effects of immunosuppression agents | Describe use of medications to reduce risk of kidney stones and indications for urological intervention | Describe the team approach to caring for a dialysis patient (nephrologist, nurse, dietitian and social worker) by participating in dialysis rounds or interdisciplinary meeting | |
| Understand the importance of patient involvement and social support by caregivers in home dialysis training | ||||||
| Systems-based practice | Discuss options for renal replacement such as dialysis, transplantation or conservative management in patients with CKD stages 4 and 5 | Understand the process of organ allocation in kidney transplantation | ||||
| Communication and interpersonal skills | Demonstrate competency to explain the basics about the diagnosis and stages of CKD (based on eGFR and albuminuria) | Counseling on lifestyle and dietary changes (sodium, potassium or phosphorus restriction as appropriate) |
ACE-I, angiotensin-converting enzyme inhibitors; ARB, angiotensin II receptor blockers; eGFR, estimated glomerular filtration rate; NSAID, nonsteroidal anti-inflammatory drugs.
Outpatient dialysis (in-center dialysis, home peritoneal dialysis and home hemodialysis) experiences are an essential component of the outpatient nephrology curriculum. Patients receiving their maintenance hemodialysis treatments in the outpatient or free-standing units are usually less sick and have better functional status than patients receiving acute or chronic dialysis in the hospital setting [6]. Thus, if IM residents were only exposed to sicker patients receiving dialytic therapies in the hospital setting, it is very likely that they would develop a skewed view of the many stable patients who chronically dialyze outside the hospital. Participation in outpatient hemodialysis rounds also allows IM residents to better understand the delivery of dialysis care by various members of the dialysis team (nephrologist, nurse, technicians, dietitian and social worker) who have different but intertwined roles in dialysis patient care. Furthermore, home dialysis options are being increasingly offered to patients with end-stage renal disease, thus allowing greater flexibility and choices than in-center hemodialysis [7]. A visit to the home dialysis program can also be an eye-opener, as it can expose the IM resident to the decision-making process, dialysis training and the quality of life enjoyed by the home dialysis patients [8]. Working with the transplant nephrologist in the transplant clinic would allow an understanding of the benefits and risks of kidney transplantation, immunosuppression protocols, transplant complications and the process of donor–recipient evaluations.
Medicine residents routinely take care of hospitalized patients with acute kidney injury (AKI) and electrolyte disorders such as hyponatremia and hyperkalemia, several of which may not require help of the inpatient nephrology team [9]. If the nephrology elective were to be purely inpatient-based, residents would be rounding on several patients with the same nephrology problems that they would otherwise encounter during their medicine ward and intensive care unit rotations. Moreover, they would lose the opportunities for learning many outpatient problems seen in nephrology, as mentioned earlier. Some may express concerns that transitioning from the inpatient to the outpatient setting in a subspecialty elective would cause IM residents to lose valuable learning time and patient interaction as there are no formal ‘bedside rounds’ in the clinic setting. We certainly do not wish to imply that performing inpatient consults is less useful than outpatient nephrology, as there is educational value to reviewing the evaluation and management of common inpatient nephrology issues with a specialist. However, we do not believe that repeating the discussions on workup of these inpatient conditions is an efficient use of the resident’s limited elective time. Outpatient nephrology learning complements and enhances learning in the inpatient setting. Furthermore, we believe that enhancing exposure to outpatient nephrology during the elective time provides a broader scope of what the field has to offer, especially if the resident wishes to consider a future career in nephrology.
Exposure to outpatient nephrology during IM residency would give a more realistic insight into the professional life of the practicing nephrologist as compared with that afforded by the pure inpatient elective. A significant percentage of the services provided by practicing nephrologists in the USA is based in the outpatient setting (dialysis unit and clinics). Exposure to outpatient nephrology would thus allow an understanding of the processes of care (such as clinic protocols for erythropoietin or intravenous iron administration), models of practice and clinical administrative responsibilities of the nephrologist. This is especially important for the IM resident potentially considering a career in nephrology.
Nephrologists cherish the continuity of care afforded when patients transition from CKD to dialysis to transplant [10]. This unique attribute of nephrology can best be evidenced in the outpatient setting, where the nephrologist plays a key role in guiding these transitions of patient care [11]. The importance of longitudinal care to resident learning is exemplified by the IM Residency Review Committee’s recommendation to increase outpatient learning [12]. As a result, many IM programs have a 4 + 1 structure (4 weeks of inpatient medicine followed by 1 week of outpatient clinic). Thus, there is a greater need than before for outpatient nephrology learning as residents are expected to spend more time in the outpatient setting.
Can outpatient nephrology experiences enhance interest in the field of nephrology?
While there is little evidence that exposure to outpatient nephrology increases the number of residents pursuing nephrology subspecialty training, surveys have shown great satisfaction among residents. At the North Shore University Hospital and Long Island Jewish Medical Center, half of the resident class was assigned to either the traditional inpatient nephrology or the redesigned inpatient–outpatient rotation. Eighty-six percent of IM residents who completed the 4-week redesigned nephrology elective reported that they would consider a career in nephrology, as opposed to 50% of the residents who underwent the pure inpatient elective [13]. Survey of the IM residents at the end of the study also revealed that those who experienced outpatient nephrology enjoyed the interaction with attendings and reported greater satisfaction than those who rotated only in the inpatient side.
It is hoped that with enhanced learning afforded by outpatient nephrology experiences, the common perceptions of IM residents toward nephrology (such as ‘dialysis patients being too sick’) is likely to change. Working with more attending faculty members as a result of the rotation design would allow different perspectives on nephrology careers to be shared and may also open up avenues for research collaboration such as quality improvement projects on CKD education or advanced care planning, thus overall benefiting the IM resident in their professional career. Also, an inpatient-based elective may well not expose the trainee to other career options that are available following nephrology fellowship training. However, a well-designed representative elective that includes both inpatient and extensive ambulatory (clinic, outpatient dialysis and transplantation) experiences would expose IM residents to additional nephrology career options that they may have never considered, such as transplant nephrology, medical directorship of a dialysis or transplant center, and interventional nephrology.
Incorporating outpatient nephrology experiences during medical residency
The University of Vermont Medical Center nephrology elective experience
The Division of Nephrology and Hypertension at the University of Vermont Medical Center (a 562-bed hospital in Burlington, VT) has nine clinical nephrologists and two transplant nephrologists providing inpatient and outpatient nephrology services (clinics and free-standing dialysis units). Prior to 2014, the 2-week nephrology elective for IM residents was purely inpatient. The resident would round with one hospital attending and be a part of the inpatient consult team that included fellows and medical students. Resident learning in the elective was limited to bedside teaching and nephrology case conferences.
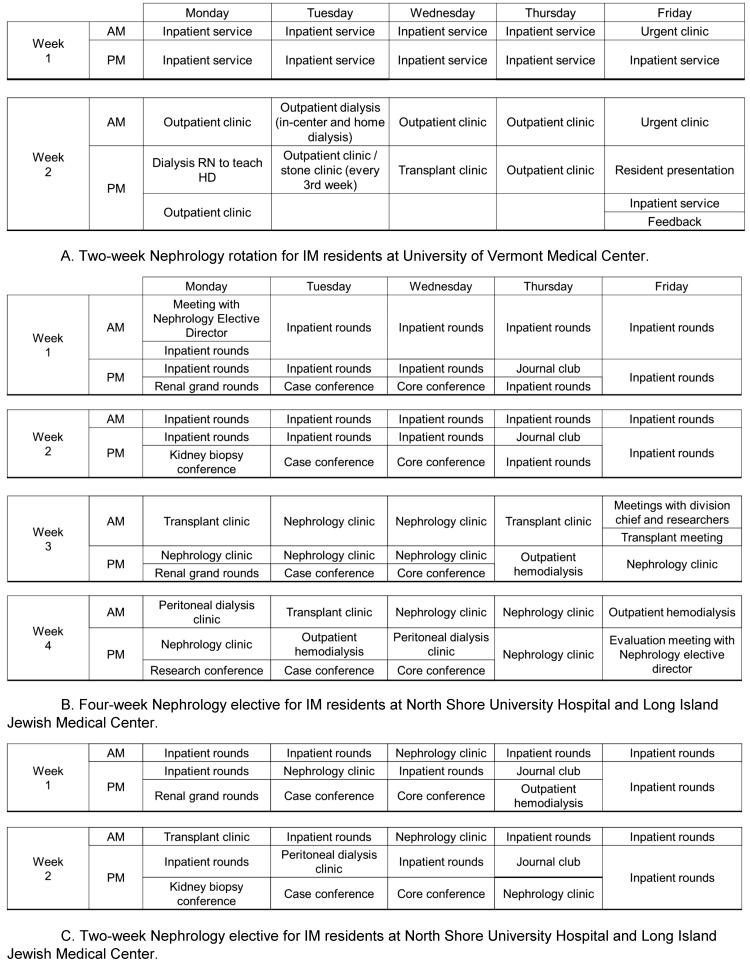
The initiative to incorporate outpatient nephrology curriculum into the resident’s education began in early 2014. Meetings with the nephrology division faculty, IM residency program director, chief medical residents and the education committee helped garner interest in this initiative. Various options of the rotation structure were considered including the nature of the rotation (elective versus mandatory), presence of half-day versus full-day clinics and a purely outpatient versus inpatient–outpatient design. Consensus was also obtained for making it mandatory for every IM resident to rotate in nephrology. We also chose not to have any half-day clinics during the inpatient rotation as this structure would have likely affected the learning and continuity of patient care, especially during the inpatient rounding. Hence, the 2-week rotation was equally divided into 1 week of full-day outpatient clinics and 1 week of inpatient rounding (Figure 1A). Residents would see new and established patients under supervision of the assigned attendings in the general nephrology clinic. We provided an electronic medical record template for data collection, presentation and to complete patient notes. Residents were also assigned to see patients in the stone clinic with either the urologist or the nephrologist. Outpatient hemodialysis rounds (that included a visit to the home program when possible) were included in the outpatient week. To enhance the overall learning experience, formal presentation of an assigned nephrology research paper was required. The IM milestones and the faculty evaluation form were revised to reflect competencies gained from outpatient nephrology. The newly designed rotation was initiated in March 2014 after receiving consensus and approval. At the beginning of each resident rotation, a schedule was created for each resident that listed the inpatient and outpatient assignments for the 2-week duration of the rotation. The resident schedules had to be individualized as attendings were occasionally unavailable because of other clinical or administrative responsibilities.
Fig. 1.
Structure of the nephrology rotation for medicine residents at University of Vermont Medical Center (A) and Northwell Health (B and C). (A) Residents are expected to participate in the medicine morning report, noon conference, medicine grand rounds and nephrology fellows case conference, and these are not represented in the figure. Residents are also asked to attend the monthly kidney biopsy pathology conference (every fourth Monday) and nephrology division journal club (every fourth Thursday). (B and C) Residents at Northwell Health may either choose the 4-week or the 2-week nephrology elective. RN, registered nurse; HD, hemodialysis.
To evaluate this novel elective experience, online surveys were sent to 5 residents in June 2014 and 17 residents in June 2015, of which 100% and 64.7%, respectively, responded [14]. On average, residents worked with four attendings. Free text comments by residents were mostly favorable (Table 2). Time to travel to the dialysis unit and clinic (10–15 min) was not considered burdensome by the residents. All residents found the topic for the assigned PowerPoint (nephrology research article) talk to be clinically relevant. Internal surveys by the IM residency program confirmed similar findings.
Table 2.
Responses from residents at University of Vermont Medical Center to the survey question ‘Any thoughts or comments on the Nephrology rotation?’
| ‘I think it was probably the most organized rotation I have gone through during my residency. I would have liked a bit more time. I would have also liked to actually do a home visit with the Home Dialysis program.’ |
| ‘I liked it—It exposed me to the outpatient side of nephro. It would have been cool to have seen more HTN, since that is so prevalent. Fellows and attendings were all cool to work with.’ |
| ‘It was great! I learned a lot and had a great time! The faculty loves to teach and everyone took time to do so! I wish I would have had the rotation earlier in my residency training.’ |
| ‘I enjoyed the nephrology rotation. I felt that the attendings were warm and welcoming. Even though it was a short rotation, I feel that it was a valuable experience.’ |
| ‘Really liked having both inpatient and outpatient experience particularly renal transplant clinic and Joy drive [outpatient dialysis unit].’ |
| ‘Much better than it used to be. I felt like I was part of the team. the support staff especially at clinic were wonderful.’ |
HTN, hypertension.
The Northwell Health nephrology elective experience
At the North Shore University Hospital and Long Island Jewish Medical Center (two large tertiary care teaching facilities of the Northwell Health, with 18 nephrology faculty), the 4-week nephrology elective for IM residents was initially restructured in 2010 (Figure 1B). The goal was to provide residents with a richer educational experience than a traditional pure inpatient-based elective. The restructured 4-week elective that was developed includes a pure 2-week inpatient consultative/dialysis experience and a dedicated 2-week extensive outpatient experience. During the outpatient elective time, IM residents experience various renal clinics, including CKD, hypertension, peritoneal dialysis and kidney transplant. In addition, they round with either a fellow or faculty member, or both, in the outpatient hemodialysis clinic several times during the elective. They also get to meet and discuss basic and clinical research studies with faculty members. Residents are also exposed to several faculty members with diverse interests and areas of expertise. Our experience with this elective in comparison with a traditional inpatient-based elective suggests that the combined elective format is perceived favorably by IM residents [13]. In addition to participation in divisional conferences (case conference, renal grand rounds, biopsy conference, journal club and core lecture) during the elective, residents are also assigned a topic in nephrology to read and prepare for presentation to both fellows and faculty. They are encouraged to present the assigned topic using non-traditional teaching tools [15, 16]. This presentation is given before the end of the rotation.
Besides the 4-week elective as described above, the 2-week pure inpatient nephrology elective that was also offered to IM residents prior to 2012 was restructured to incorporate several outpatient and educational nephrology experiences (Figure 1C). Presently, the IM residents have the option to experience either a pure 2-week outpatient nephrology elective or a combined 1-week pure inpatient and 1-week dedicated outpatient elective. The pure 2-week outpatient elective is more commonly chosen by IM residents who are interested in nephrology.
Implications and future considerations
With all the above-described benefits of exposing IM residents to outpatient nephrology, we recognize that there may be several difficulties related to incorporating this experience during elective time. Strategies to overcome some of these challenges are listed in Table 3. IM residency program directors may sometimes feel the need to have residents work preferentially in the hospital setting because of the increased demands of inpatient subspecialty services. In fact, this was the most common reason cited on a survey by US nephrology program directors for the inability to offer outpatient nephrology experience to the residents [5]. While this remains an important concern, it is incumbent upon the training community to provide a true insight into the professional life of practicing nephrologists during elective time. While all of nephrology and what it has to offer cannot be mastered in 2–4 weeks, we urge IM residency programs to work collaboratively with their clinician educators in nephrology and attempt to incorporate as much outpatient nephrology learning as possible.
Table 3.
Strategies to incorporate outpatient nephrology into the IM residency program
|
IM, internal medicine; ACGME, Accreditation Council for Graduate Medical Education.
Some clinical educators may argue that if career decisions are to be influenced, it is more important for medical students than residents to be exposed to outpatient nephrology. In a survey of 273 fourth-year medical students across five US medical schools, Rosner et al. reported that fewer than one-third of the students had any exposure to nephrology, thus lessening the probability of choosing a career in nephrology [18]. Interestingly, more than 40% of the surveyed students desired more outpatient exposure to nephrology [18]. Hence, incorporating outpatient nephrology experiences during medical student elective time is also important and should be strongly considered. Residents who are international medical graduates have their first exposure to nephrology practice in the USA during residency. As international medical graduates make up about 60% of the applicants who match into a nephrology fellowship, it is vital that appropriate exposure to outpatient nephrology occur in medicine residency [19].
Several IM residency programs may also have difficulty arranging outpatient nephrology experiences due to scattered practice locations such as outpatient clinics and dialysis units. Such programs should consider full-day clinics for their residents to minimize travel time. Use of online real-time streaming of live lectures such as resident noon conferences is likely to avoid residents missing out important educational content without wasting time on travel.
Finally, we would encourage the training community to make creative attempts to expose their IM residents to other educational and clinical activities in nephrology. Interventional nephrology is a field that is likely to appeal to residents interested in performing procedures and may be an attractive option to increase interest in nephrology [20]. A visit to the interventional nephrology suite, such as in an outpatient vascular access center, and allowing observation of procedures to establish or maintain vascular access may be considered based on the setup. Another opportunity would be to expose IM residents to the field of kidney transplantation during their residency. A well-planned 2- to 4-week elective in kidney transplantation would be an exciting option for interested IM residents, where they could learn about the organ allocation process, donor–recipient evaluation, follow-up of kidney transplant patients and an opportunity to interact with the surgeons on inpatient rounds or transplant committee meetings. Teaching bedside ultrasound to evaluate the kidneys, urinary bladder and methods to assess volume status is an exciting skill to teach residents as there is likely to be more demand for point-of-care ultrasound in the future [21, 22].
Training programs should consider providing an additional 2- to 4-week purely outpatient-based nephrology elective for IM residents, especially to those who have an interest in the field or if there is concern that the educational experience with the inpatient–outpatient rotation is superficial. Educational activities (such as creative writing, academic newsletter or crosswords) to keep the residents engaged during the rotation should also be considered. Further educational research studies are needed to understand the impact of outpatient nephrology rotation design on resident learning and career choices.
In conclusion, while there will be several challenges, we believe that incorporating outpatient nephrology experiences during IM residency can potentially enhance resident learning and interest in nephrology. The ambulatory care exposure during the nephrology rotation offers IM residents new learning opportunities in patient care, medical knowledge and systems-based practice in outpatient nephrology, and allows interaction with several more nephrology attendings than a purely inpatient-based rotation, thus increasing mentorship opportunities. Hence, IM residency programs and the training nephrology community should strongly consider incorporating outpatient nephrology curriculum based on the feasibility, resources and support available to them. While several factors play a vital role in an IM resident’s career choices, exposure to outpatient nephrology during medical residency will allow the resident to make a better-informed decision regarding whether nephrology is the right career choice for them.
Acknowledgements
We thank Mark Levine, M.D., F.A.C.P., Mark Pasanen, M.D., and Mary Ramundo, M.D. for their enthusiastic support in the outpatient nephrology curriculum at University of Vermont Medical Center. Findings in this article were presented at the National Kidney Foundation 2015 Spring Clinical Meetings, 25–29 March 2015, Dallas, TX, and the abstract was published in Am J Kidney Dis 2015; 65: A8.
Conflicts of interest statement
None declared.
References
- 1. Hsu C-Y, Parker MG, Ross MJ. et al. ; ASN Nephrology Match Task Force. Improving the nephrology match: the path forward. J Am Soc Nephrol 2015; 26: 2634–2639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Jhaveri KD, Sparks MA, Shah HH. et al. Why not nephrology? A survey of US internal Medicine Subspecialty Fellows. Am J Kidney Dis 2013; 61: 540–546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Shah HH, Jhaveri KD, Sparks MA. et al. Career choice selection and satisfaction among US adult nephrology fellows. Clin J Am Soc Nephrol 2012; 7: 1513–1520 [DOI] [PubMed] [Google Scholar]
- 4. Salsberg E, Quigley L, Mehfoud N. et al. The US Nephrology Workforce 2016: Developments and Trends. Washington, DC: American Society of Nephrology, 2016. https://www.asn-online.org/education/training/workforce/Nephrology_Workforce_Study_Report_2016.pdf. (1 December 2016, date last accessed) [Google Scholar]
- 5. Shah HH, Adams ND, Mattana J. et al. Nephrology elective experience during medical residency: a national survey of US nephrology fellowship training program directors. Ren Fail 2015; 37: 999–1006 [DOI] [PubMed] [Google Scholar]
- 6. Arora P, Kausz AT, Obrador GT. et al. Hospital utilization among chronic dialysis patients. J Am Soc Nephrol 2000; 11: 740–746 [DOI] [PubMed] [Google Scholar]
- 7. Rivara MB, Mehrotra R.. The changing landscape of home dialysis in the United States. Curr Opin Nephrol Hypertens 2014; 23: 586–591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Finkelstein FO, Schiller B, Daoui R. et al. At-home short daily hemodialysis improves the long-term health-related quality of life. Kidney Int 2012; 82: 561–569 [DOI] [PubMed] [Google Scholar]
- 9. Balasubramanian G, Al-Aly Z, Moiz A. et al. Early nephrologist involvement in hospital-acquired acute kidney injury: a pilot study. Am J Kidney Dis 2011; 57: 228–234 [DOI] [PubMed] [Google Scholar]
- 10. Adams ND. Choosing nephrology—or not. Am J Kidney Dis 2013; 61: 529–531 [DOI] [PubMed] [Google Scholar]
- 11. Adams ND. Longitudinal Nephrology Clinic [LNC] for residents. J Am Soc Nephrol 2008; 19: 811A [Google Scholar]
- 12. Meyers FJ, Weinberger SE, Fitzgibbons JP. et al. Redesigning residency training in internal medicine: the consensus report of the Alliance for Academic Internal Medicine Education Redesign Task Force. Acad Med 2007; 82: 1211–1219 [DOI] [PubMed] [Google Scholar]
- 13. Jhaveri KD, Shah HH, Mattana J.. Enhancing interest in nephrology careers during medical residency. Am J Kidney Dis 2012; 60: 350–353 [DOI] [PubMed] [Google Scholar]
- 14. Agrawal V. Enhancing interest in nephrology by introducing ambulatory clinic rotation for medicine residents. Am J Kidney Dis 2015; 65: A1625791961 [Google Scholar]
- 15. Jhaveri KD, Sparks MA, Shah HH.. Novel educational approaches to enhance learning and interest in nephrology. Adv Chronic Kidney Dis 2013; 20: 336–346 [DOI] [PubMed] [Google Scholar]
- 16. Calderon KR, Vij RS, Mattana J. et al. Innovative teaching tools in nephrology. Kidney Int 2011; 79: 797–799 [DOI] [PubMed] [Google Scholar]
- 17. McGee SR, Irby DM.. Teaching in the outpatient clinic. J Gen Intern Med 1997; 12: S34–S40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Rosner M, Parker M, Kohan D.. Nephrology as a career choice: a survey of medical students. J Am Soc Nephrol 2009; 20: 767A [Google Scholar]
- 19. Pivert K. NRMP SMS Nephrology Match for Appointment Year 2016–2017: ASN Brief Analysis https://www.asn-online.org/education/training/workforce/ASN_NRMP_SMS_2016_Analysis.pdf (24 July 2016, date last accessed)
- 20. Kalloo SD, Mathew RO, Asif A.. Is nephrology specialty at risk? Kidney Int 2016; 90: 31–33 [DOI] [PubMed] [Google Scholar]
- 21. Solomon SD, Fidencio S. Point-of-care ultrasound in medical education — stop listening and look. N Engl J Med 2014; 370: 1083–1085 [DOI] [PubMed] [Google Scholar]
- 22.Ross D, Barnett R, Shah HH. Lung ultrasonography: a novel tool to consider in nephrology. Kidney Int 2016; 89: 720–1 [DOI] [PubMed] [Google Scholar]