Abstract
Aim
The objective of this study was to evaluate the prognostic value of ARID1A, p53, p21, p16 and ß-Catenin in endometrioid and clear cell ovarian and endometrial carcinomas.
Materials and methods
97 tumors were available for analysis of ARID1A, p53, p21, p16 and ß-Catenin with the techniques of tissue microarray and immunohistochemistry. 32 were ovarian carcinomas and 65 were endometrial carcinomas.
Results
Endometrioid ovarian carcinomas showed negative staining for ARID1A (a) and p21 (b), aberrant expression of p53 (c) and p16 (d) and ß-Catenin positive nuclear expression (e) respectively in 19% (a), 100% (b), 28.6% (c), 52.4% (d) and 4.8% (e) of all cases. In the group of clear cell ovarian carcinomas it was 63.6% (a), 100% (b), 81.8% (c), 54.5% (d) and 0% (e). For endometrioid uterine carcinomas it was 75.7% (a), 94.9% (b), 30.5% (c), 52.1% (d) and 6.8% (e) and for clear cell uterine carcinomas it was 8.6% (a), 100% (b), 50% (c), 100% (d) and 0% (e). Survival analysis showed that negative expression of ARID1A, p53 aberrant expression and ß-Catenin nuclear positive staining are independent negative prognosticators in both, clear cell and endometrioid carcinoma, regardless of ovarian or uterine origin. Cox-Regression analysis showed them again as negative prognostic factors. Furthermore, we found a significant correlation between ARID1A and ß-Catenin expression in endometrioid uterine tumors.
Conclusion
The analyzed gynaecological carcinoma showed a distinct expression scheme of proteins that are associated with tumor suppression. We may conclude that ARID1A, p53 and ß-Catenin are the strongest prognostic factors by analyzing a subgroup of tumor suppressor genes in clear cell and endometrioid subtypes of ovarian and endometrial cancer and may be used along with traditional morphological and clinical characteristics for prognosis.
Introduction
The traditional histopathological classification of endometrial epithelial cancer, which was first proposed by Bokhman, includes type I tumors that are usually estrogen-dependent low-grade endometrioid cancers and type II tumors which are usually estrogen-independent high-grade serous or clear cell carcinomas [1]. While the first pathogenetic type has a frequency of 80–90% and is associated with highly or moderately differentiated tumors with a favorable prognosis, the second type has a frequency of only 10–20% and includes poorly differentiated tumors with a doubtful prognosis [1].
For ovarian epithelial cancer pathogenesis a less accepted paradigm exists suggesting to differ between type I and type II molecular profiles [2]. Type I tumors contain endometrioid, clear cell and low-grade serous carcinoma and mostly arise from atypical endometriosis or from borderline serous tumors [2,3]. Type II carcinomas include high-grade serous, which show typically a p53 mutation and, at least for patients with a BRCA mutation frequently arise from the fimbriated end of the fallopian tube via serous tubar intraepithelial carcinoma (STIC) [4,5].
Many studies have aimed to understand the cell origin and pathogenesis of these cancer subtypes in order to better diagnose and treat patients. Recently several studies suggested that the origin of clear cell and endometrioid carcinomas might derive from atypical endometriosis, which is believed to originate from the endometrium by retrograde menstruation [6–8]. The three-staged tumor grading system of endometrioid ovarian carcinoma is equivalent to the grading of endometrioid endometrial cancer and considers growth patterns and nuclear aplasia while there is no validated grading system for clear cell ovarian cancer, which are still classified as high-grade carcinoma [9].
Considerable interest has not only been generated in understanding the pathogenesis but also in the identification of factors that influence the prognosis of these tumors. Early diagnosis of epithelial ovarian and uterine cancer is critical for patient survival. Ovarian cancer has the highest mortality rate of the three main malignant tumors of the female reproductive system, with an overall 5-year survival rate of 45% [10]. Known prognostic factors of ovarian and endometrial carcinoma are histological subtype, tumor grading, International Federation of Gynecology and Obstetrics (FIGO) staging as well as estrogen receptor positivity for endometrial carcinoma and age, general condition and residual tumor for ovarian cancer [9,11]. Previous studies have explored molecular alterations in clear cell and endometrioid ovarian and endometrial tumors as additional prognostic factors, including changes in expression of ARID1A, p53, p21, p16 and ß-Catenin carcinoma.
ARID1A is a recently identified tumor suppressor participating in forming SWI/SNF chromatin complexes [12]. Somatic inactivating mutations of ARID1A and loss of ARID1A expression appear to be an early event in the development of most ovarian clear cell and endometrioid carcinomas as well as atypical endometriosis [13,14]. ARID1A is also frequently mutated and plays an important role in tumor progression in uterine endometrioid carcinoma [15,16].
p53 is a well-studied tumor suppressor gene that plays a key role in regulating the cell cycle. It is a principal mediator of growth arrest, senescence and apoptosis in response to a broad array of cellular damage [17]. The p53 wild-type protein directly induces the expression of the p21 protein which binds to a variety of cyclin-dependent kinases and inhibits their activity as well as regulates the repair of DNA and blocks its replication by inhibiting cell-cycle progression [18,19].
The p16 protein is also a tumor suppressor gene that, in response to various stresses, inhibits cyclin-dependent kinases and causes the arrest of the cell-cycle in G1 phase [20].
ß-Catenin however is the effector of the Wnt signaling pathway [21]. It accumulates in cell-cell junctions in cells not receiving the Wnt signal bound by a complex referred to as the destruction complex. When cells receive the Wnt signal it is stabilized, enters the nucleus and activates Wnt target genes [21]. Inappropriate activation of the Wnt pathway underlies many cancers including ovarian and uterine carcinoma, mostly endometrioid [22].
In this study the expression of ARID1A, p53, p21, p16 and ß-Catenin was determined in 97 tumors by performing immunohistochemistry to evaluate their prognostic value. Human tissue samples of the ovary and the uterus, obtained after surgical resection, were used to investigate the correlation between their expression and clinical parameters, including overall survival.
Materials and methods
Tumors and patients
This study assessed 97 patients who all underwent primary surgery between January 1, 1990 and December 31, 2001 in the Department of Gynaecology, Ludwig-Maximilians-University, Munich, Germany. A total of 59 cases were endometrioid uterine carcinoma, 6 clear cell uterine carcinoma, 21 endometrioid ovarian carcinoma and 11 clear cell ovarian carcinoma. The analyzed tissue samples were taken from the hospital archive of the Department of Pathology, Ludwig-Maximilians-University, Munich, Germany. In cooperation with the tumor register of Munich necessary data about the patients’ survival was available. The patients were staged and the tumors graded according to 1988 International Federation of Gynaecology and Obstetrics (FIGO) criteria [23]. Patients’ characteristics, e.g. age, FIGO stage, histological subtype and FIGO grade are shown in Table 1. Survival was taken from the date of confirmed histological diagnosis after primary surgery to the date of recurrence or last visit.
Table 1. Patients characteristics (N = 97).
| Age (median) | 61.0 (range 35–82) |
| Histopathology | |
| Clear cell uterine carcinoma | 6 (6.2) |
| Endometrioid uterine carcinoma | 59 (60.8) |
| Clear cell ovarian carcinoma | 11 (11.3) |
| Endometrioid ovarian carcinoma | 21 (21.6) |
| Tumor grading | |
| Grade 1 | 27 (27.8) |
| Grade 2 | 29 (29.9) |
| Grade 3 | 41 (42.3) |
| FIGO-staging | |
| I | 24 (24.7) |
| II | 20 (20.6) |
| III | 24 (24.7) |
| IV | 29 (29.9) |
Ethical approval
All patients´ data were fully anonymized, and the study was performed according to the standards set in the Declaration of Helsinki 1975. All tumor tissue used was leftover material that had initially been collected for histopathological diagnostics. All diagnostic procedures had already been fully completed when samples were retrieved for the study. The current study was approved in writing by the Ethics Committee of the Ludwig Maximilians University, Munich, Germany (approval number 449–14). Authors were blinded for clinical information during experimental analysis.
Sampling and tissue microarray construction of ovarian and uterine cancer tissue
New samples from the original slides of tumors were taken and representative areas of tumor tissues were selected. Three core biopsies from each specimen were removed and attached on tissue microarrays. The presence of tumor tissue on the arrayed samples was verified by a pathologist.
Immunohistochemistry and interpretation
Serial sections of the recipient tissue microarray paraffin blocks were cut at 2–3 μm, deparaffinized with xylene, and rehydrated through a series of graded alcohols. The immunostaining procedure was performed using an automated stainer (Benchmark® XT, Ventana). The following monoclonal primary antibodies were used: ARID1A/BAF250a Rabbit mAb (New England Biolabs GmbH) directed against ARID1A protein, p53 Ab-5 (Thermo Scientific) directed against 53, p16-Arc (p16INK4a, CINtec® Histology) directed against p16, p21 Cip (CDKN1A) directed against p21 and ß-Catenin Mouse IgG-1 (Roche, Ventana, ready to use) directed against ß-Catenin. All staining’s were performed at the Department of Pathology, Ludwig-Maximilians-University, Munich.
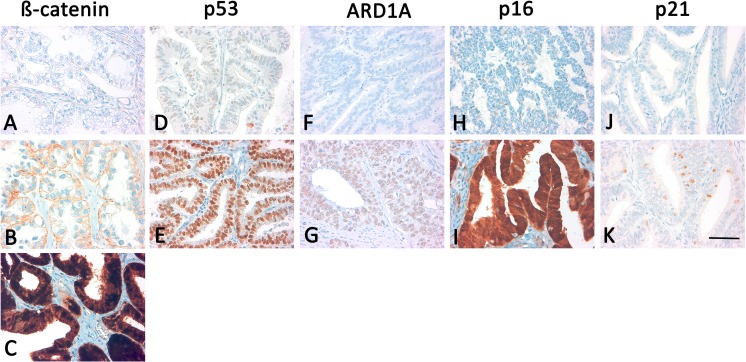
The IHC stains were evaluated by the authors (MH and DM) in a double-blind process using the immunoreactive Remmele score (IRS) [24]. The quantity of cells stained was scored as: 0 = no staining, 1 = 1–10%, 2 = 11–50%, 3 = 51–80% and 4 = >81% staining. The IRS was rendered as a product of the scores obtained for staining intensity (0 = no expression, 1 = weak expression, 2 = moderate expression, 3 = strong expression) and quantity. A total score of 0–2 was considered negative, 3–5: weak, 6–8: moderate and 9–12: strong immunoreactivity. ARID1A and p21 were dichotomized into negative (0–2 points in IRS) and positive cases (3–12 points in IRS) and p53 and p16 were dichotomized into no expression/overexpression (= aberrant) and normal expression (= regulated). Weak to moderate immunoreactivity (3–8 points in IRS) was considered p53/p16 normal expression. Strong and diffuse nuclear p53/p16 immunoexpression (9–12 points in IRS) or complete absence of p53/p16 staining (0–2 points in IRS) was interpreted as likely indicating a p53/p16 gene mutation. The presence of rare weakly positive nuclear staining is a pattern that is commonly associated with wild type p53 and can be found in normal ovarian and uterine tissues [25]. ß-Catenin was classified in 3 groups of ß-Catenin nuclear negative (0–2 points in IRS) and membrane positive (n-m+) staining (3–12 points in IRS), nuclear negative (0–2 points in IRS) and membrane weak (3–6 points in IRS) or negative staining (n-m-) (0–2 points in IRS) and ß-Catenin nuclear and membrane/cytoplasm positive (n+m+) staining (3–12 points in IRS) (Fig 1).
Fig 1.
Immunohistochemical stainings for ß-Catenin, p53, ARID1A, p16 and p21 in clear-cell (A and B) and endometrioid (C—K) carcinomas. Focal, very weak membranous (n-m-) (A), membranous (n-m+) (B) and nuclear (n+m+) (C) expression of β-catenin. Regulated (D) and aberrant (E) expression of p53. Preserved expression of ARID1A (F) and loss (G) of ARID1A expression. Negative staining (H) and positive (I) staining for p16. Negative (J) and positive staining (K) of p21. 400 × magnification was used for all pictures; scale bar (K) refers to 60 μm for all images.
Statistical analysis
For statistical analysis the SPSS Statistics Version 23 (SPSS Inc., Chicago, IL, USA) was used. For testing proportional differences in univariate analysis the Pearson’s Chi-square test or Fisher’s exact test for qualitative variables and unpaired t-test for quantitative normally distributed variables was applied. For normally distributed variables in several groups the single-factor variance analysis was used. The survival curves were generated by using the Kaplan Meier technique and differences between these curves were tested by the log-rank test. All tests were two-sided and the level of statistical significance was accepted at p ≤ 0.05. For multivariate analyses the Cox regression model was used with tumor-related death as the endpoint.
Results
Results from immunohistochemistry
ARID1A
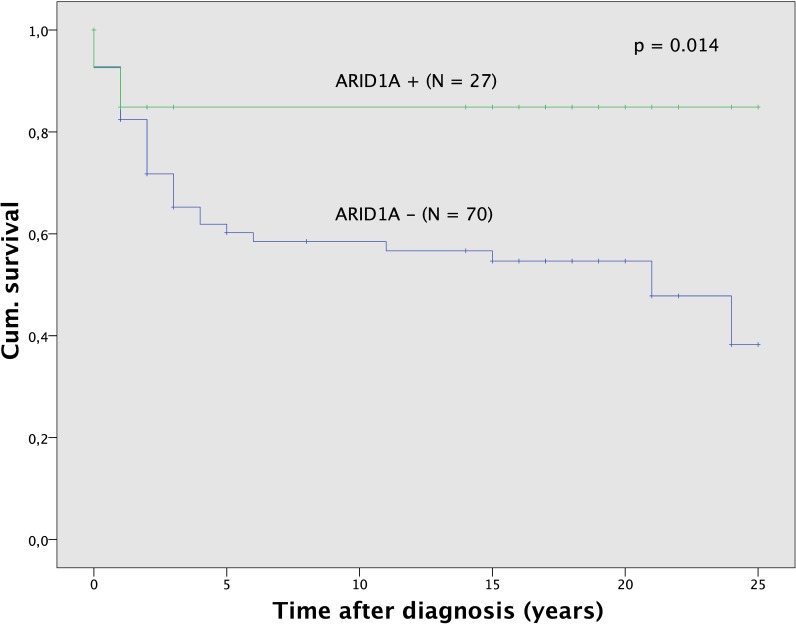
ARID1A nuclear positive staining was observed in 27 (27.8) out of 97 tumors. The ARID1A status was significantly (p < 0.001) related to histological subtype (Table 2). Positive nuclear staining seen more frequently in endometrioid tumors and it was infrequent in clear cell carcinoma. The ARID1A status alone was not associated with tumor grade (p = 0.581) or age (p = 0.369), but it was related statistically significantly to FIGO stage (p < 0.001). Positive nuclear staining for ARID1A was seen more frequently in FIGO I tumors while FIGO III and IV tumors were mostly ARID1A negative (S1 Fig). Survival analysis (Fig 2) demonstrated significant (p = 0.014) differences for patients according to the ARID1A status. Patients with ARID1A negative tumors had a 5-year survival of 60.2% compared with 84.9% survival for those with ARID1A positive tumors. Significantly better survival in the subgroup of ARID1A positive tumors could also be observed for sole analysis of all endometrioid (p = 0.039) and all ovarian carcinoma (p = 0.008) as well as tumors of grading G3 (p = 0.028).
Table 2. Status of ARID1A, p53, p21, p16 and ß-Catenin according to histological subtypes (N = 97).
| Expression N (%) | ARID1A – | ARID1A + | P53 -/+++ | P53 + | P16 -/+++ | P16 + | P21 – | P21 + | ß-Catenin n-m+ | ß-Catenin n-m- | ß-Catenin n+m+ |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 70 (72.2) | 27 (27.8) | 36 (37.1) | 61 (62.9) | 48 (49.5) | 49 (50.5) | 94 (96.9) | 3 (3.1) | 64 (66.0) | 28 (28.9) | 5 (5.2) | |
| Histology | |||||||||||
| Clear cell uterine | 6 (8.6) | 0 (0) | 3 (8.3) | 3 (4.9) | 6 (12.5) | 0 (0) | 6 (6.4) | 0 (0) | 1 (1.6) | 5 (17.9) | 0 (0) |
| Endometrioid uterine | 53 (75.7) | 6 (22.2) | 18 (50) | 41 (67.2) | 25 (52.1) | 34 (69.4) | 56 (58.3) | 3 (3.1) | 42 (65.6) | 13 (46.4) | 4 (80) |
| Clear cell ovarian | 7 (10.0) | 4 (14.8) | 9 (25) | 2 (3.3) | 6 (12.5) | 5 (10.2) | 11 (11.5) | 0 (0) | 6 (9.4) | 5 (17.9) | 0 (0) |
| Endometrioid ovarian | 4 (5.7) | 17 (63.0) | 6 (16.7) | 15 (24.6) | 11 (22.9) | 10 (20.4) | 21 (21.9) | 0 (0) | 15 (23.4) | 5 (17.9) | 1 (20) |
| P-value | < 0.001 | < 0.001 | 0.008 | 0.008 | 0.049 | 0.049 | 0.756 | 0.756 | 0.07 | 0.07 | 0.07 |
Fig 2. Survival analysis for ARID1A.
Survival was better for the subgroup of patients with ARID1A positive tumors (N = 27) compared to the subgroup with ARID1A negative tumors (N = 70).
p53
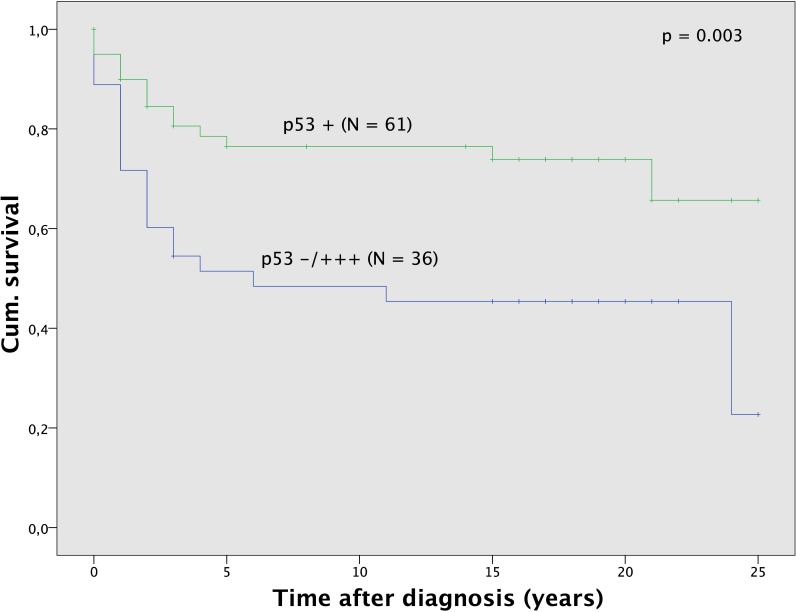
p53 overexpression or complete absence was seen in 36 (37.1) out of 97 carcinoma. The status of p53 was significantly (p = 0.008) associated with histological subtype (Table 2). p53 overexpression or complete absence was seen mostly in clear cell tumors, but infrequent in endometrioid carcinoma. The p53 status was not related to age (p = 0.487) or FIGO stage (p = 0.081), but it was associated significantly (p < 0.001) with tumor grade. Overexpression or no expression of p53 was most frequently seen in poorly differentiated (G3) clear cell and endometrioid tumors and infrequent in G1 and G2 endometrioid tumors (S1 Table). Survival analysis (Fig 3) showed significant (p = 0.003) differences for patients according to p53 status. Patients with overexpression or complete absence of p53 in their tumors had a 5-year survival rate of 51.5% compared to 76.5% survival for those with positive p53 expression. Significantly better survival in the subgroup of p53 regulated tumors could also be observed for sole analysis of all clear cell (p = 0.020) and all uterine carcinoma (p = 0.012) as well as tumors of grading G1 and G2 (p = 0.036) and G3 (p = 0.011) and tumors with FIGO staging 0, I and II (p = 0.012).
Fig 3. Survival analysis for p53.
Survival was better for the subgroup of patients with p53 positive tumors (N = 61) compared to the subgroup with p53 negative/overexpression tumors (N = 36).
p16
p16 overexpression or complete absence was seen in 48 (49.5) out of 97 tumors. The p16 status was significantly (p = 0.049) related to histological subtype (Table 2). p16 overexpression or no expression was seen more frequently in clear cell tumors and it was infrequent in endometrioid carcinoma. The p16 status alone was not associated with tumor grade (p = 0.749), age (p = 0.359), FIGO stage (p = 0.645) or survival (p = 0.436).
p21
p21 nuclear positive staining was confined to the nucleus and observed in 3 (5.1%) out of 97 carcinoma, which were all endometrioid uterine tumors. The p21 status was not related to histological subtype (p = 0.756), grading (p = 0.114), age (p = 0.673), FIGO stage (p = 0.433) or survival (p = 0.153).
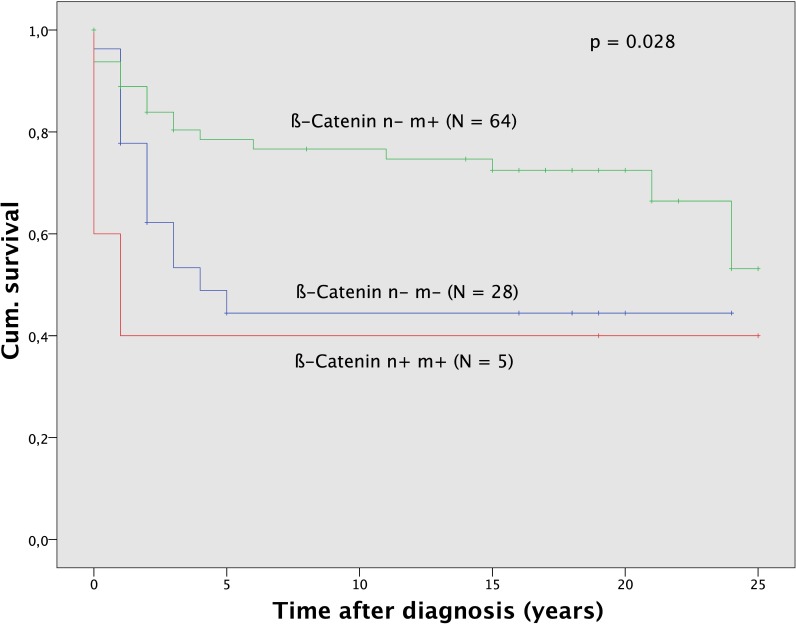
ß-Catenin
ß-Catenin nuclear negative and positive membrane staining (n-m+) was observed in 64 (66.0), ß-Catenin nuclear and membrane negative (n-m-) staining in 28 (28.8) and ß-Catenin positive nuclear and membrane/cytoplasm staining (n+m+) in 5 (5.2) out of 97 tumors. The ß-Catenin status was significantly (p = 0.07) related to histological subtype (Table 2). ß-Catenin n-m+ staining was more frequently seen in endometrioid tumors and it was infrequent in clear cell carcinoma. ß-Catenin n+m+ staining was only observed in endometrioid tumors, mostly in endometrial cancer. The ß-Catenin status was not related to age (p = 0.483) or FIGO stage (p = 0.750). It was significantly (p = 0.046) associated with tumor grade. Thus ß-Catenin n+m+ staining and n-m- staining was mostly seen in G2 and G3 tumors whereas positive membrane staining alone was almost evenly spread among all grading. Survival analysis (Fig 4) demonstrated significant (p = 0.028) differences for patients according to ß-Catenin status.
Fig 4. Survival analysis for ß-Catenin.
Survival analysis for ß-Catenin. Survival was better for the subgroup of patients with ß-Catenin n-m+ tumors (N = 64) compared to the subgroup ß-Catenin n-m- (N = 28) and ß-Catenin n+m+ tumors (N = 5).
Patients with n-m- staining for ß-Catenin in their tumors had a 5-year survival rate of 44.4% and patients with n+m+ staining had a 5-year survival rate of 40,0% compared to 78.5% survival for those with n-m+ expression. Significantly better survival in the subgroup of ß-Catenin n-m+ stained tumors could also be observed for sole analysis of all endometrioid tumors (p = 0.031) and uterine carcinoma (p = 0.014) as well as tumors of grading G3 (p = 0.036) and tumors with FIGO staging III and IV (p = 0.021).
Relationship between ARID1A/ß-Catenin status, and ß-Catenin/p16 status and their association to clinico-pathological data
Correlation between the expressions of the five different proteins was tested by using Pearsons chi-square test (Table 3). A low significant correlation was found between ARID1A and ß-Catenin with a corrected coefficient of contingency of Ccor = 0.282 (p = 0.045) and ß-Catenin and p16 with a corrected coefficient of contingency of Ccor = 0.282 (p = 0.045). Further the differences between the expressions of ARID1A/ß-Catenin and ß-Catenin/p16 were investigated based on different clinical parameters, including age, histological subtype, grading and FIGO staging. While the ARID1A/ß-Catenin status was not significantly related to age (p = 0.697), a significant correlation to histological subtype (p < 0.001), grading (p = 0.018) and FIGO staging (p = 0.014) was observed (Table 4). ARID1A negative staining and simultaneous ß-Catenin n+m+ staining was only seen in endometrioid uterine tumors. ARID1A negative staining and simultaneous ß-Catenin n-m- staining was also observed mostly in endometrioid endometrial cancer. This staining combination was found to be mostly in tumors with grading G3 and FIGO staging IV. ARID1A positive staining and simultaneous ß-Catenin n-m+ staining were mostly seen in endometrioid ovarian carcinoma and the tumors belonged mostly to FIGO staging I.
Table 3. Correlation among ARID1A/ß-Catenin and ß-Catenin/p16 in endometrioid and clear cell ovarian and uterine tissues.
| ß-Catenin n-m-/n+m+ | ß-Catenin n-m+ | ||
|---|---|---|---|
| N (%) | 33 (34.0) | 64 (66.0) | N (%) |
| ARID1A - | 28 | 42 | 70 (72.2) |
| ARID1A + | 5 | 22 | 27 (27.8) |
| Ccorr = 0.282, p-value: 0.045 | 97 | ||
| P16 –o +++ | 21 | 27 | 48 (49.5) |
| P16 + | 12 | 37 | 49 (50.5) |
| Ccorr = 0.282, p-value: 0.045 | 97 |
Ccorr, corrected coefficient of contingency
Table 4. Status of ARID1A/ß-Catenin according to histological subtype, grading and FIGO staging.
| Expression N (%) | ARID1A +/ ß-Catenin n-m+ |
ARID1A +/ ß-Catenin n+m+ |
ARID1A -/ ß-Catenin n-m- |
ARID1A -/ ß-Catenin n-m+ |
ARID1A -/ ß-Catenin n+m+ |
|---|---|---|---|---|---|
| 25 (25.8) | 2 (2.1) | 25 (25.8) | 42 (43.3) | 3 (3.1) | |
| Histological subtype | |||||
| Clear cell uterine | 0 (0) | 0 (0) | 5 (20) | 1 (2.4) | 0 (0) |
| Endometrioid uterine | 5 (20) | 1 (50) | 13 (52) | 37 (88.1) | 3 (100) |
| Clear cell ovarian | 4 (16) | 0 (0) | 5 (20) | 2 (4.8) | 0 (0) |
| Endometrioid ovarian | 16 (64) | 1 (50) | 2 (8) | 2 (4.8) | 0 (0) |
| P-value < 0.001 | |||||
| Grading | |||||
| G1 | 7 (28) | 1 (50) | 3 (12) | 16 (38.1) | 0 (0) |
| G2 | 5 (20) | 1 (50) | 6 (24) | 16 (38.1) | 1 (33.3) |
| G3 | 13 (52) | 0 (0) | 16 (64) | 10 (23.8) | 2 (67.7) |
| P-value = 0.018 | |||||
| FIGO staging | |||||
| FIGO I | 13 (52) | 1 (50) | 4 (16) | 6 (14.3) | 0 (0) |
| FIGO II | 6 (24) | 1 (50) | 4 (16) | 9 (21.4) | 0 (0) |
| FIGO III | 4 (16) | 0 (0) | 7 (28) | 12 (28.6) | 1 (33.3) |
| FIGO IV | 2 (8) | 0 (0) | 10 (40) | 15 (35.7) | 2 (67.7) |
| P-value = 0.014 |
The ß-Catenin/p16-status showed no significant correlation to the parameters mentioned above (age (p = 0.750), histological subtype (p = 0.189), grading (p = 0.379) and FIGO staging (p = 0.613)).
Multivariate analysis
In a multivariate Cox regression analysis with tumor-related death as the end point significant and independent prognostic factors were ARID1A status with hazard ratio (HR) of 3.359, p53 status with HR of 3.408, ß-Catenin status with HR of 2.251 and ARID1A/ß-Catenin status with HR of 2.209 (Tables 5–8). An HR of 2.209 for concomitant ARID1A negativity and ß-Catenin n-m-/n+m+ staining of tumors versus other combinations of ARID1A/ß-Catenin meant a 2.209 fold increased risk for tumor-related death for patients who belonged to the first subgroup. Similarly, an HR of 3.359 for ARID1A negative tumors versus ARID1A positive tumors, an HR of 3.408 for p53 aberrant expression versus p53 regulated expression and an HR of 2.251 for ß-Catenin weak/negative membranous and positive nuclear expression versus ß-Catenin positive membranous expression meant a 3.359, 3.408 respectively 2.251 fold increased risk for tumor-related death for patients who belonged to the first subgroups.
Table 5. Multivariate Cox regression analysis with tumor related death as endpoint for ARID1A.
| Variable | Hazard Ratio | 95% Confidence Interval | P-Value | n |
|---|---|---|---|---|
| Age (years) | 0.990 | 0.959–1.021 | 0.514 | 97 |
| Histological subtype (endometrioid vs. clear cell carcinoma) | 2.110 | 0.942–4.728 | 0.070 | 97 |
| Grading (G1+G2 vs. G3 tumors) |
1.064 | 0.524–2.162 | 0.864 | 97 |
| FIGO stage (I+II vs. III + IV tumors) |
1.079 | 0.533–2.186 | 0.833 | 97 |
| ARID1A (+ vs. -) | 3.359 | 1.152–9.792 | 0.026 | 97 |
Table 8. Multivariate Cox regression analysis with tumor related death as endpoint for ARID1A/ß-Catenin status.
| Variable | Hazard Ratio | 95% Confidence Interval | P-Value | n |
|---|---|---|---|---|
| Age (years) | 0.992 | 0.960–1.024 | 0.614 | 97 |
| Histological subtype (endometrioid vs. clear cell carcinoma) | 1.678 | 0.736–3.822 | 0.218 | 97 |
| Grading (G1+G2 vs. G3 tumors) |
1.459 | 0.696–3.058 | 0.317 | 97 |
| FIGO stage (I+II vs. III + IV tumors) |
1.198 | 0.593–2.421 | 0.614 | 97 |
| Others vs. ARID1A-/ß-Catenin n-m-/ß-Catenin n+m+ | 2.209 | 1.031–4.734 | 0.041 | 97 |
Table 6. Multivariate Cox regression analysis with tumor related death as endpoint for p53.
| Variable | Hazard Ratio | 95% Confidence Interval | P-Value | n |
|---|---|---|---|---|
| Age (years) | 0.987 | 0.956–1.019 | 0.426 | 97 |
| Histological subtype (endometrioid vs. clear cell carcinoma) | 1.605 | 0.716–3.599 | 0.251 | 97 |
| Grading (G1+G2 vs. G3 tumors) |
1.957 | 0.903–4.239 | 0.194 | 97 |
| FIGO stage (I+II vs. III + IV tumors) |
1.589 | 0.790–3.196 | 0.194 | 97 |
| p53 (+ vs.—o+++) | 3.408 | 1.567–7.415 | 0.002 | 97 |
Table 7. Multivariate Cox regression analysis with tumor related death as endpoint for ß-Catenin.
| Variable | Hazard Ratio | 95% Confidence Interval | P-Value | n |
|---|---|---|---|---|
| Age (years) | 0.993 | 0.961–1.026 | 0.674 | 97 |
| Histological subtype (endometrioid vs. clear cell carcinoma) | 1.743 | 0.774–3.928 | 0.180 | 97 |
| Grading (G1+G2 vs. G3 tumors) |
1.430 | 0.691–2.957 | 0.335 | 97 |
| FIGO stage (I+II vs. III + IV tumors) |
1.249 | 0.633–2.511 | 0.532 | 97 |
| ß-Catenin (n-m+ vs. n-m-/n+m+) |
2.251 | 1.096–4.625 | 0.027 | 97 |
Discussion
Endometrial cancer can be subdivided into two histological subtypes, the estrogen-associated type I which includes endometrioid carcinomas and the estrogen-independent type II which comprises mostly high-grade serous and clear cell carcinoma [1]. The type II carcinoma is known to metastasize more often and to have a worse survival. A less accepted paradigm for ovarian cancer also differs between type I tumors which include endometrioid, clear cell and low-grade serous carcinoma and type II tumors containing p53-mutated high-grade serous carcinoma [2].
Many biomarkers, including different tumor suppressors such as ARID1A, p53, p21, p16 and ß-Catenin, were discovered to be changed in expression in endometrioid and clear cell subtypes in recent years [26–29]. The aim of this study was to evaluate their prognostic value, particularly in the synopsis of all the above mentioned factors, by using immunhistochemical methods.
Ovarian clear cell carcinoma usually showed p53 overexpression or no expression (81.8%), while ovarian endometrioid carcinoma mostly was observed to have positive p53 expression (71.4%). Both subtypes consisted in equal parts of p16 overexpression/no expression or positive expression and all stained negatively for p21. These findings confirm the results of various studies [30–32], which indicate that most of the ovarian clear cell tumors show p53 mutations, while most of endometrioid tumors do not. There are several studies showing that p16 is overexpressed in high-grade serous ovarian carcinoma compared with other morphologic types of ovarian cancer [33], whereas inactivation of the gene was observed in 3 out of 9 endometrioid and 1 out of 4 clear cell ovarian carcinomas [34]. Another study explored the expression of p21 in endometrioid and clear cell ovarian carcinoma and found p21 negativity in 59.5% (endometrioid) and 31.2% (clear cell) [35].
For endometrial carcinoma we can report that clear cell subtypes consisted in equal parts of p53 overexpression/no expression or positive expression and all showed p16 overexpression/no expression while endometrioid subtypes mostly were found to have positive p53 (69.5%) and p16 (69.4%) staining. Both subtypes were stained mostly p21 negative. In several studies, the p53 mutation prevalence among clear cell uterine carcinoma ranges from 28.5% to 76.9% [36,37].
For endometrioid uterine carcinoma however, most of the tumors appear to have no p53 mutation [38], which is in agreement with our results. In endometrioid uterine carcinoma the expression pattern of p16 is typically described as weakly positive unlike the strong expression generally seen in endocervial adenocarcinomas of the usual type [39]. However, another study found up to 33% overexpression and 65% no expression in clear cell endometrial carcinoma and different p16 expression in endometrioid endometrial carcinoma according to FIGO grade [40]. In FIGO grade 1 and 2 endometrioid subtypes were found to be mostly stained p16 negative while in FIGO grade 3 about 25% turned out to be p16 positive. For p21 expression in endometrial cancer some studies showed about 54% p21 negativity, increasing with older age and current smoking [41]. In contrast to these results other studies figured out that p21 seems to be mostly positively expressed in endometrial cancer [26]. The contradictory findings related to p16 and p21 may be due to different staining protocols, cut-off values for p16 and p21 expression, and characteristics of the study populations examined.
In this analysis the ß-Catenin expression of ovarian and uterine tumors was determined. ß-Catenin mutations are particularly common in endometrioid ovarian and uterine cancer [22]. However, their prevalence ranges widely from 16–54% across the several studies [42]. It could be confirmed that ß-Catenin n+m+ staining was only seen in endometrioid tumors, mostly uterine.
ARID1A has been recently classified as a novel tumor suppressor, which regulates p53-controlled genes [43]. Reduced ARID1A expression is mostly induced by nonsense mutations as well as insertions and deletions in the gene-coding region, which lead to mRNA decay or sequence truncation [44]. It has been published that promoter hypermethylation may also be responsible for the loss of ARID1A expression [45]. ARID1A mutations are frequently in various tumors including gastric cancer, colorectal cancer, breast cancer, lung cancer and gynaecological cancer [46]. High rates of ARID1A mutations were observed in 46–57% of ovarian clear cell carcinomas, 30% of ovarian endometrioid carcinomas and 40% of uterine endometrioid carcinomas [15,47,48]. In this study, we also demonstrated that negative expression of ARID1A was common in clear cell (63.6%) and endometrioid (19%) ovarian tumors as well as clear cell (100%) and endometrioid (89.8%) uterine cancer. Moreover, we determined a significant relationship between ARID1A loss and higher FIGO stages which is similar to previous studies [49,50].
No study could be found that examined the combined ARD1A/ß-Catenin status of ovarian and uterine tumors yet. However, few studies indicate that there is an association between the two tumor suppressor genes. ARID1A silencing seems to be inducing a subcellular redistribution of β-catenin from the plasma membrane to the cytoplasm and nucleus in gastric cancer, which was found to be significantly associated with worse clinical prognosis [51]. Another study demonstrated that the chromatin-remodeling factor ARID1B, forming the BAF complex together with ARID1A, represses the Wnt/ß-Catenin signaling pathway indicating this might contribute to cancer through deregulation of developmental and oncogenic pathways [52]. It also suggests ARID1A might operate in a similar fashion as ARID1B in Wnt/β-Catenin pathway. In this study a significant correlation between ARID1A and ß-Catenin could be shown. Concomitantly ARID1A negative staining and ß-Catenin n+m+ staining respectively ß-Catenin n-m- staining was usually seen in endometrioid uterine cancer with poor grading (G2 and G3) and poor FIGO staging (FIGO III and FIGO IV). In a multivariate Cox Regression analysis this staining combination of ARID1A and ß-Catenin meant a 2.209 fold increased risk for tumor-related death. This indicates that the ARID1A/ß-Catenin pathway connection might play a role in tumor progression in endometrioid endometrial carcinoma. It could already be demonstrated that ARID1A loss and ß-Catenin mutation, each seen individually, are important in progression of different types of human cancer [16,53,54]. Additional studies will have to be conducted to evaluate the association between ß-Catenin and the chromatin remodelling gene ARID1A in uterine endometrioid carcinoma further.
In the present study it was possible to identify three prognostic factors that showed differences in independent survival analysis. For the tumor suppressor gene p53 we were able to show that patients with overexpression or no expression of p53 had a worse overall survival compared to those with normal p53 expression. This is consistent with a number of studies determining the prognostic value of p53 in ovarian and uterine carcinoma [27,35] and in contrast to other studies [54,55].
It could be observed that nuclear and membrane/cytoplasm positive staining as well as nuclear and membrane negative staining of ß-Catenin were markers for worse overall survival which agrees with some studies [56,57] that show reduced ß-Catenin cell surface expression was a predictor for poor survival but not with other studies [58,59] that associate strong membranous β-Catenin expression with shorter progression free survival. Discordance between these results could be due to different patterns of ß-Catenin and p53 expression in ovarian and uterine carcinoma, especially in different staging and grading, and differences in the methods of immunohistochemical interpretation.
Similar to previous studies it could be determined that ARID1A loss in ovarian and uterine tumors is a predictor for poor survival [49,60–62]. ARID1A expression was also reported to be a prognostic marker for several other cancers such as gastric cancer, clear cell renal cell carcinoma and cervical cancer [63–65].
At this point some limitations of this study may be noted which can be addressed in future studies. They include mostly the limited numbers of cases within histological subgroups, especially clear cell carcinoma with a total number of only 17 cases. To prevent the effect, that ovarian and uterine carcinoma can be very heterogeneous in immunohistochemical interpretation the tissue microarray construction was done by using three core biopsies from each specimen. Nevertheless some cases might not have been adequately represented due to loss of cancer tissue material.
In summary, a significant association between AIRD1A and ß-Catenin expression was discovered in endometrioid uterine tumors. This suggests that concomitantly ARID1A negative staining and ß-Catenin nuclear and membrane/cytoplasm positive (n+m+) staining respectively ß-Catenin nuclear and membrane negative staining (n-m-) might play a role in tumor progression in type I endometrial cancer. Furthermore ARID1A, p53 and ß-Catenin turned out to be three promising prognostic factors showing significant differences in independent survival analysis, indicating that ARID1A, p53 and ß-Catenin could be used along traditional clinical and morphologic factors to predict the prognosis of patients with clear cell and endometrioid ovarian and uterine cancer.
Supporting information
(DOCX)
(XLSX)
(TIF)
Data Availability
All relevant data (i.e., the DNA and RNA data underlying our findings) are within the paper and its Supporting Information files.
Funding Statement
These studies were supported by a grant from Heuer Stiftung für medizinische Forschung (https://www.heuer-stiftung.de/), no grant number was received. Dr. Linda Hertlein received the funding. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Kurman RJ, Caracangiu ML, Herrington CS, Young RH (2014) International Agency for Research on Cancer, World Health Organization WHO classification of tumours of female reproductive organs France: Lyon: International Agency for Research on Cancer, 2014. [Google Scholar]
- 2.Shih IeM, Kurman RJ (2004) Ovarian tumorigenesis: a proposed model based on morphological and molecular genetic analysis. Am J Pathol 164: 1511–1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cho KR, Shih IeM (2009) Ovarian cancer. Annu Rev Pathol 4: 287–313. doi: 10.1146/annurev.pathol.4.110807.092246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Crum CP, Drapkin R, Miron A, Ince TA, Muto M, Kindelberger DW et al. (2007) The distal fallopian tube: a new model for pelvic serous carcinogenesis. Curr Opin Obstet Gynecol 19: 3–9. doi: 10.1097/GCO.0b013e328011a21f [DOI] [PubMed] [Google Scholar]
- 5.Piek JM, Verheijen RH, Kenemans P, Massuger LF, Bulten H, van Diest PJ (2003) BRCA1/2-related ovarian cancers are of tubal origin: a hypothesis. Gynecol Oncol 90: 491. [DOI] [PubMed] [Google Scholar]
- 6.Halme J, Hammond MG, Hulka JF, Raj SG, Talbert LM (1984) Retrograde menstruation in healthy women and in patients with endometriosis. Obstet Gynecol 64: 151–154. [PubMed] [Google Scholar]
- 7.King CM, Barbara C, Prentice A, Brenton JD, Charnock-Jones DS (2016) Models of endometriosis and their utility in studying progression to ovarian clear cell carcinoma. J Pathol 238: 185–196. doi: 10.1002/path.4657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pearce CL, Templeman C, Rossing MA, Lee A, Near AM, Webb PM et al. (2012) Association between endometriosis and risk of histological subtypes of ovarian cancer: a pooled analysis of case-control studies. Lancet Oncol 13: 385–394. doi: 10.1016/S1470-2045(11)70404-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Deutsche Krebsgesellschaft DK, AWMF (2016) S3-Leitlinie Diagnostik, Therapie und Nachsorge maligner Ovarialtumoren, Langversion 2.0.
- 10.Siegel RL, Miller KD, Jemal A (2015) Cancer statistics, 2015. CA Cancer J Clin 65: 5–29. doi: 10.3322/caac.21254 [DOI] [PubMed] [Google Scholar]
- 11.Saso S, Chatterjee J, Georgiou E, Ditri AM, Smith JR, Ghaem-Maghami S (2011) Endometrial cancer. BMJ 343: d3954 doi: 10.1136/bmj.d3954 [DOI] [PubMed] [Google Scholar]
- 12.Wang X, Nagl NG, Wilsker D, Van Scoy M, Pacchione S, Yaciuk P, et al. (2004) Two related ARID family proteins are alternative subunits of human SWI/SNF complexes. Biochem J 383: 319–325. doi: 10.1042/BJ20040524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ayhan A, Mao TL, Seckin T, Wu CH, Guan B, Ogawa H, et al. (2012) Loss of ARID1A expression is an early molecular event in tumor progression from ovarian endometriotic cyst to clear cell and endometrioid carcinoma. Int J Gynecol Cancer 22: 1310–1315. doi: 10.1097/IGC.0b013e31826b5dcc [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lowery WJ, Schildkraut JM, Akushevich L, Bentley R, Marks JR, Huntsman D, et al. (2012) Loss of ARID1A-associated protein expression is a frequent event in clear cell and endometrioid ovarian cancers. Int J Gynecol Cancer 22: 9–14. doi: 10.1097/IGC.0b013e318231f140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guan B, Mao TL, Panuganti PK, Kuhn E, Kurman RJ, Maeda D, et al. (2011) Mutation and loss of expression of ARID1A in uterine low-grade endometrioid carcinoma. Am J Surg Pathol 35: 625–632. doi: 10.1097/PAS.0b013e318212782a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mao TL, Ardighieri L, Ayhan A, Kuo KT, Wu CH, Wang TL, et al. (2013) Loss of ARID1A expression correlates with stages of tumor progression in uterine endometrioid carcinoma. Am J Surg Pathol 37: 1342–1348. doi: 10.1097/PAS.0b013e3182889dc3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Levine AJ (1997) p53, the cellular gatekeeper for growth and division. Cell 88: 323–331. [DOI] [PubMed] [Google Scholar]
- 18.El-Deiry W, Tokino T, Velculescu V, Levy D, Parsons R, Trent JM, et al. (1993) WAF1, a Potential Mediator of p53 Tumor Suppression. Cell 75: 817–825. [DOI] [PubMed] [Google Scholar]
- 19.Michieli P, Chedid M, Lin D, Pierce JH, Mercer WE, Givol D (1994) Induction of WAF1/CIP1 by a p53-independent pathway. Cancer Res 54: 3391–3395. [PubMed] [Google Scholar]
- 20.Serrano M, Hannon GJ, Beach D (1993) A new regulatory motif in cell-cycle control causing specific inhibition of cyclin D/CDK4. Nature 366: 704–707. [DOI] [PubMed] [Google Scholar]
- 21.Cadigan KM, Peifer M (2009) Wnt signaling from development to disease: insights from model systems. Cold Spring Harb Perspect Biol 1: a002881 doi: 10.1101/cshperspect.a002881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Polakis P (2007) The many ways of Wnt in cancer. Curr Opin Genet Dev 17: 45–51. doi: 10.1016/j.gde.2006.12.007 [DOI] [PubMed] [Google Scholar]
- 23.Shepherd JH (1989) Revised FIGO staging for gynaecological cancer. Br J Obstet Gynaecol 96: 889–892. [DOI] [PubMed] [Google Scholar]
- 24.Remmele W, Stegner HE (1987) Recommendation for uniform definition of an immunoreactive score (IRS) for immunohistochemical estrogen receptor detection (ER-ICA) in breast cancer tissue. Pathologe 8: 138–140. [PubMed] [Google Scholar]
- 25.Yemelyanova A, Vang R, Kshirsagar M, Lu D, Marks MA, Shih IeM, et al. (2011) Immunohistochemical staining patterns of p53 can serve as a surrogate marker for TP53 mutations in ovarian carcinoma: an immunohistochemical and nucleotide sequencing analysis. Mod Pathol 24: 1248–1253. doi: 10.1038/modpathol.2011.85 [DOI] [PubMed] [Google Scholar]
- 26.Buchynska LG, Nesina IP (2006) Expression of the cell cycle regulators p53, p21(WAF1/CIP1) and p16(INK4a) in human endometrial adenocarcinoma. Exp Oncol 28: 152–155. [PubMed] [Google Scholar]
- 27.Lee YH, Heo JH, Kim TH, Kang H, Kim G, Kim J, et al. (2011) Significance of cell cycle regulatory proteins as malignant and prognostic biomarkers in ovarian epithelial tumors. Int J Gynecol Pathol 30: 205–217. doi: 10.1097/PGP.0b013e3182063e71 [DOI] [PubMed] [Google Scholar]
- 28.Saegusa M, Machida BD, Okayasu I (2001) Possible associations among expression of p14(ARF), p16(INK4a), p21(WAF1/CIP1), p27(KIP1), and p53 accumulation and the balance of apoptosis and cell proliferation in ovarian carcinomas. Cancer 92: 1177–1189. [DOI] [PubMed] [Google Scholar]
- 29.Steinbakk A, Skaland I, Gudlaugsson E, Janssen EA, Kjellevold KH, Klos J, et al. (2009) The prognostic value of molecular biomarkers in tissue removed by curettage from FIGO stage 1 and 2 endometrioid type endometrial cancer. Am J Obstet Gynecol 200: 78 e71–78. [DOI] [PubMed] [Google Scholar]
- 30.Köbel M, Kalloger SE, Boyd N, McKinney S, Mehl E, Palmer C, et al. (2008) Ovarian carcinoma subtypes are different diseases: implications for biomarker studies. PLoS Med 5: e232 doi: 10.1371/journal.pmed.0050232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lai CR, Hsu CY, Chen YJ, Yen MS, Chao KC, Li AF (2013) Ovarian cancers arising from endometriosis: a microenvironmental biomarker study including ER, HNF1ss, p53, PTEN, BAF250a, and COX-2. J Chin Med Assoc 76: 629–634. doi: 10.1016/j.jcma.2013.07.008 [DOI] [PubMed] [Google Scholar]
- 32.Rechsteiner M, Zimmermann AK, Wild PJ, Caduff R, von Teichman A, Fink D, et al. (2013) TP53 mutations are common in all subtypes of epithelial ovarian cancer and occur concomitantly with KRAS mutations in the mucinous type. Exp Mol Pathol 95: 235–241. doi: 10.1016/j.yexmp.2013.08.004 [DOI] [PubMed] [Google Scholar]
- 33.Phillips V, Kelly P, McCluggage WG (2009) Increased p16 expression in high-grade serous and undifferentiated carcinoma compared with other morphologic types of ovarian carcinoma. Int J Gynecol Pathol 28: 179–186. doi: 10.1097/PGP.0b013e318182c2d2 [DOI] [PubMed] [Google Scholar]
- 34.Ichikawa Y, Yoshida S, Koyama Y, Hirai M, Ishikawa T, Nishida M, et al. (1996) Inactivation of p16/CDKN2 and p15/MTS2 genes in different histological types and clinical stages of primary ovarian tumors. Int J Cancer 69: 466–470. [DOI] [PubMed] [Google Scholar]
- 35.Skirnisdottir I, Seidal T (2013) Association of p21, p21 p27 and p21 p53 status to histological subtypes and prognosis in low-stage epithelial ovarian cancer. Cancer Genomics Proteomics 10: 27–34. [PubMed] [Google Scholar]
- 36.Hoang LN, McConechy MK, Meng B, McIntyre JB, Ewanowich C, Gilks CB, et al. (2015) Targeted mutation analysis of endometrial clear cell carcinoma. Histopathology 66: 664–674. doi: 10.1111/his.12581 [DOI] [PubMed] [Google Scholar]
- 37.Arai T, Watanabe J, Kawaguchi M, Kamata Y, Nishimura Y, Jobo T, et al. (2006) Clear cell adenocarcinoma of the endometrium is a biologically distinct entity from endometrioid adenocarcinoma. Int J Gynecol Cancer 16: 391–395. [DOI] [PubMed] [Google Scholar]
- 38.Alvarez T, Miller E, Duska L, Oliva E (2012) Molecular profile of grade 3 endometrioid endometrial carcinoma: is it a type I or type II endometrial carcinoma? Am J Surg Pathol 36: 753–761. doi: 10.1097/PAS.0b013e318247b7bb [DOI] [PubMed] [Google Scholar]
- 39.McCluggage WG, Jenkins D (2003) p16 immunoreactivity may assist in the distinction between endometrial and endocervical adenocarcinoma. Int J Gynecol Pathol 22: 231–235. doi: 10.1097/01.PGP.0000055172.04957.2F [DOI] [PubMed] [Google Scholar]
- 40.Reid-Nicholson M, Iyengar P, Hummer AJ, Linkov I, Asher M, Soslow RA (2006) Immunophenotypic diversity of endometrial adenocarcinomas: implications for differential diagnosis. Mod Pathol 19: 1091–1100. doi: 10.1038/modpathol.3800620 [DOI] [PubMed] [Google Scholar]
- 41.Felix AS, Sherman ME, Hewitt SM, Gunja MZ, Yang HP, Cora RL, et al. (2015) Cell-cycle protein expression in a population-based study of ovarian and endometrial cancers. Front Oncol 5: 25 doi: 10.3389/fonc.2015.00025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bell DA (2005) Origins and molecular pathology of ovarian cancer. Mod Pathol 18 Suppl 2: S19–32. [DOI] [PubMed] [Google Scholar]
- 43.Guan B, Wang TL, Shih IeM (2011) ARID1A, a factor that promotes formation of SWI/SNF-mediated chromatin remodeling, is a tumor suppressor in gynecologic cancers. Cancer Res 71: 6718–6727. doi: 10.1158/0008-5472.CAN-11-1562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wu JN, Roberts CW (2013) ARID1A mutations in cancer: another epigenetic tumor suppressor? Cancer Discov 3: 35–43. doi: 10.1158/2159-8290.CD-12-0361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhang X, Sun Q, Shan M, Niu M, Liu T, Xia B, et al. (2013) Promoter hypermethylation of ARID1A gene is responsible for its low mRNA expression in many invasive breast cancers. PLoS One 8: e53931 doi: 10.1371/journal.pone.0053931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jones S, Li M, Parsons DW, Zhang X, Wesseling J, Kristel P, et al. (2012) Somatic mutations in the chromatin remodeling gene ARID1A occur in several tumor types. Hum Mutat 33: 100–103. doi: 10.1002/humu.21633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jones S, Wang TL, Shih IeM, Mao TL, Nakayama K, Roden R, et al. (2010) Frequent mutations of chromatin remodeling gene ARID1A in ovarian clear cell carcinoma. Science 330: 228–231. doi: 10.1126/science.1196333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wiegand KC, Shah SP, Al-Agha OM, Zhao Y, Tse K, Zeng T, et al. (2010) ARID1A mutations in endometriosis-associated ovarian carcinomas. N Engl J Med 363: 1532–1543. doi: 10.1056/NEJMoa1008433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fadare O, Renshaw IL, Liang SX (2012) Does the Loss of ARID1A (BAF-250a) Expression in Endometrial Clear Cell Carcinomas Have Any Clinicopathologic Significance? A Pilot Assessment. J Cancer 3: 129–136. doi: 10.7150/jca.4140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Werner HM, Berg A, Wik E, Birkeland E, Krakstad C, Kusonmano K, et al. (2013) ARID1A loss is prevalent in endometrial hyperplasia with atypia and low-grade endometrioid carcinomas. Mod Pathol 26: 428–434. doi: 10.1038/modpathol.2012.174 [DOI] [PubMed] [Google Scholar]
- 51.Yan HB, Wang XF, Zhang Q, Tang ZQ, Jiang YH, Fan HZ, et al. (2014) Reduced expression of the chromatin remodeling gene ARID1A enhances gastric cancer cell migration and invasion via downregulation of E-cadherin transcription. Carcinogenesis 35: 867–876. doi: 10.1093/carcin/bgt398 [DOI] [PubMed] [Google Scholar]
- 52.Vasileiou G, Ekici AB, Uebe S, Zweier C, Hoyer J, Engels H, et al. (2015) Chromatin-Remodeling-Factor ARID1B Represses Wnt/beta-Catenin Signaling. Am J Hum Genet 97: 445–456. doi: 10.1016/j.ajhg.2015.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Voeller HJ, Truica CI, Gelmann EP (1998) Beta-catenin mutations in human prostate cancer. Cancer Res 58: 2520–2523. [PubMed] [Google Scholar]
- 54.Yokoyama Y, Mori S, Hamada Y, Hieda M, Kawaguchi N, Shaker M, et al. (2011) Platelet-derived growth factor regulates breast cancer progression via beta-catenin expression. Pathobiology 78: 253–260. doi: 10.1159/000328061 [DOI] [PubMed] [Google Scholar]
- 55.Skirnisdottir IA, Sorbe B, Lindborg K, Seidal T (2011) Prognostic impact of p53, p27, and C-MYC on clinicopathological features and outcome in early-stage (FIGO I-II) epithelial ovarian cancer. Int J Gynecol Cancer 21: 236–244. doi: 10.1097/IGC.0b013e31820986e5 [DOI] [PubMed] [Google Scholar]
- 56.Faleiro-Rodrigues C, Macedo-Pinto I, Pereira D, Lopes CS (2004) Loss of beta-catenin is associated with poor survival in ovarian carcinomas. Int J Gynecol Pathol 23: 337–346. [DOI] [PubMed] [Google Scholar]
- 57.Voutilainen KA, Anttila MA, Sillanpaa SM, Ropponen KM, Saarikoski SV, Juhola MT, et al. (2006) Prognostic significance of E-cadherin-catenin complex in epithelial ovarian cancer. J Clin Pathol 59: 460–467. doi: 10.1136/jcp.2005.029876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bodnar L, Stanczak A, Cierniak S, Smoter M, Cichowicz M, Kozlowski W, et al. (2014) Wnt/beta-catenin pathway as a potential prognostic and predictive marker in patients with advanced ovarian cancer. J Ovarian Res 7: 16 doi: 10.1186/1757-2215-7-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wang H, Wang H, Makki MS, Wen J, Dai Y, Shi Q, et al. (2014) Overexpression of beta-catenin and cyclinD1 predicts a poor prognosis in ovarian serous carcinomas. Int J Clin Exp Pathol 7: 264–271. [PMC free article] [PubMed] [Google Scholar]
- 60.Itamochi H, Oumi N, Oishi T, Shoji T, Fujiwara H, Sugiyama T, et al. (2015) Loss of ARID1A expression is associated with poor prognosis in patients with stage I/II clear cell carcinoma of the ovary. Int J Clin Oncol 20: 967–973. doi: 10.1007/s10147-015-0811-x [DOI] [PubMed] [Google Scholar]
- 61.Katagiri A, Nakayama K, Rahman MT, Rahman M, Katagiri H, Nakayama N, et al. (2012) Loss of ARID1A expression is related to shorter progression-free survival and chemoresistance in ovarian clear cell carcinoma. Mod Pathol 25: 282–288. doi: 10.1038/modpathol.2011.161 [DOI] [PubMed] [Google Scholar]
- 62.Yokoyama Y, Matsushita Y, Shigeto T, Futagami M, Mizunuma H (2014) Decreased ARID1A expression is correlated with chemoresistance in epithelial ovarian cancer. J Gynecol Oncol 25: 58–63. doi: 10.3802/jgo.2014.25.1.58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Cho H, Kim JS, Chung H, Perry C, Lee H, Kim JH (2013) Loss of ARID1A/BAF250a expression is linked to tumor progression and adverse prognosis in cervical cancer. Hum Pathol 44: 1365–1374. doi: 10.1016/j.humpath.2012.11.007 [DOI] [PubMed] [Google Scholar]
- 64.Lichner Z, Scorilas A, White NM, Girgis AH, Rotstein L, Wiegand KC, et al. (2013) The chromatin remodeling gene ARID1A is a new prognostic marker in clear cell renal cell carcinoma. Am J Pathol 182: 1163–1170. doi: 10.1016/j.ajpath.2013.01.007 [DOI] [PubMed] [Google Scholar]
- 65.Wang DD, Chen YB, Pan K, Wang W, Chen SP, Chen JG, et al. (2012) Decreased expression of the ARID1A gene is associated with poor prognosis in primary gastric cancer. PLoS One 7: e40364 doi: 10.1371/journal.pone.0040364 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(XLSX)
(TIF)
Data Availability Statement
All relevant data (i.e., the DNA and RNA data underlying our findings) are within the paper and its Supporting Information files.