Abstract
Introduction:
We evaluated an intervention to teach physicians how to help their smoking patients quit compared to usual care in Argentina.
Methods:
Physicians were recruited from six clinical systems and randomized to intervention (didactic curriculum in two 3-hour sessions) or usual care. Smoking patients who saw participating physicians within 30 days of the intervention (index clinical visit) were randomly sampled and interviewed by telephone with follow-up surveys at months 6 and 12 after the index clinical visit. Outcomes were tobacco abstinence (main), quit attempt in the past month, use of medications to quit smoking, and cigarettes per day. Repeated measures on the same participants were accommodated via generalized linear mixed models.
Results:
Two hundred fifty-four physicians were randomized; average age 44.5 years, 53% women and 12% smoked. Of 1378 smoking patients surveyed, 81% were women and 45% had more than 12 years of education. At 1 month, most patients (77%) reported daily smoking, 20% smoked some days and 3% had quit. Mean cigarettes smoked per day was 12.9 ( SD = 8.8) and 49% were ready to quit within the year. Intention-to-treat analyses did not show significant group differences in quit rates at 12 months when assuming outcome response was missing at random (23% vs. 24.1%, P = .435). Using missing=smoking imputation rule, quit rates were not different at 12 months (15.6% vs. 16.4% P = .729). Motivated smokers were more likely to quit at 6 months (17.7% vs. 9.6%, P = .03).
Conclusions:
Training in tobacco cessation for physicians did not improve abstinence among their unselected smoking patients.
Introduction
The prevalence of cigarette smoking in Argentina in 2004 was 37.1% among persons between 16 and 65 years, 1 and tobacco consumption rates among physicians and medical students was similar to the general population. 2 Although half of physicians believed that smoking cessation counseling by clinicians is an effective tool to help patients quit, less than 30% of physicians and only 5% of medical students had received any training in counseling patients on tobacco cessation. 3
The role of healthcare professionals in smoking cessation has been the subject of considerable debate. 4 During the late 1980s there was evidence to suggest that advice from physicians to their smoking patients could be effective in facilitating smoking cessation even though the absolute increase in abstinence was small. 5 , 6 A 2013 Cochrane review analyzed pooled data from 17 trials conducted between 1972 and 1997 of brief advice versus no advice or usual care and detected a significant increase in the rate of quitting with a relative risk of 1.66 (95% confidence interval = 1.42% to 1.94%). 7 Although provision of advice and support to smokers results in only a 1% to 3% absolute increase in cessation rates, this would translate into a substantial public health benefit and be a component in a national tobacco control program.
Despite the clinical evidence in support of smoking cessation counseling, a low proportion of smoking patients report receiving advice on cessation from physicians in high-income countries. 8–11 Advice on smoking is often not offered systematically, 12 in part because 40% of primary care physicians felt that advising smokers about cessation is time-consuming and ineffective, 13 and because many physicians lack the skills for smoking cessation counseling. 14 In addition, most clinicians have difficulty in delivering the recommended “5-As” to most smokers in their care 15 , 16 and need alternative models to provide or refer to cessation services. 17 , 18
We did not identify studies about the provision of smoking cessation assistance by clinicians that were conducted in Latin America or in any low or middle-income country. This study aimed to test if an evidence-based intervention to teach physicians how to help their patients who smoke quit, would result in higher cessation rates compared to usual care in ambulatory clinical settings in Argentina.
Methods
Setting and Clinical Sites
The study was conducted from July 2009 to December 2011 in the City and Province of Buenos Aires, Argentina. General internists, family physicians, and gynecologists were recruited from six clinical systems in the cities of Buenos Aires, La Plata, and Olavarria. The “Hospital Italiano” is a staff model health maintenance organization serving patients with health coverage through their jobs in capitated care at 11 primary care sites. “Centro de Educación Médica e Investigación Clínica” is a health maintenance organization that cares for patients covered through their employment but with fee for service plans. Olavarria is a rural municipality with 31 clinics that provide health care for working class and poor populations. The public health system from the city of La Plata has 26 urban clinics serving mostly poor or uninsured patients. “Hospital Aleman” is a community hospital with a health plan using a fee for service model and “Medicus” is a fee-for-service health plan and both of these systems care for patients from upper middle class background who purchase this option through their employment or independently. Each of the participant institutions’ institutional review board and an NIH certified institutional review board based in Centro de Educación Médica e Investigación Clínica approved the protocol.
Sampling: Physicians
Invitations to participate were sent to physicians who saw more than 100 patients a month in the selected specialties within the 6 systems, 3 months before the study began. Those who agreed to participate signed informed consent and completed a baseline self-administered questionnaire. Physicians were randomized to intervention or usual care within each clinical system, stratified by specialty (general internal medicine/family medicine or gynecology). One year after the intervention, physicians completed a follow-up survey.
Clinician Intervention
The physician intervention consisted of two 3-hour sessions based on the course “Rx for Change: Clinician-Assisted Tobacco Cessation” 19 developed in the United States. The course content was translated to Spanish and adapted to Argentina. The course focused on brief tobacco cessation counseling interventions, including screening, brief counseling (≥3 minutes), and prescribing cessation medications. The theoretical basis of this course was the stages of change model using the 5-As counseling framework and addresses barriers and facilitators in the clinical setting. 20 The instructors taught participants how to use medications as adjuncts to counseling. In addition, physicians received information about how to use the project website www.cmtabaquismo.com.ar with information and materials for clinicians and patients. These included referring patients to the national telephone quit line, access to a self-help booklet, 21 , 22 and referring patients to a smoking cessation website www.dejardefumar.ucsf.edu . 23 Physicians also received monthly emails as reminders with useful tips to help patients stop smoking or manage withdrawal.
Patient Eligibility and Procedures
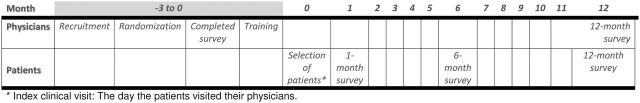
Lists of patients seen within 30 days after the study physicians were randomized (control) or had completed the smoking cessation course (intervention) were obtained. Patients were called to ascertain smoking status and confirmed smokers were randomly selected and invited to participate in the study by responding to the surveys. Smokers who had quit after the index clinical visit but before the 1-month survey were included in the study because we considered physicians potentially influenced their smoking cessation. Participants were anchored to this initial index clinical visit when asked what the physician discussed about smoking. This initial survey was the 1-month survey and follow-up surveys were completed 6 and 12 months after randomization of physicians. A smoker was defined as anyone who reported being a daily smoker or nondaily smoker and had smoked during the 30 days prior to the index clinical visit. Figure 1 shows a timeline of the project procedures.
Figure 1.
Timeline of the Argentina Physician Intervention Project, 2009–2011. The top part describes the recruitment of participants and below is the timing of this recruitment.
Measures
The 1-month telephone survey asked for age, years of education, self-rated health status, and the two-item depression screen (feeling sad and loss of interest in pleasant activities). Participants were asked about tobacco use history, number of cigarettes smoked per day, nicotine dependence measure defined by time to first cigarette, 24 smoking discussions during the index clinical visit, what steps the physician recommended, receipt of a self-help booklet including information about a website or a follow-up appointment about smoking. Follow-up surveys at 6 and 12 months ascertained smoking status, duration of time without smoking among self-reported quitters, cigarettes per day if still smoking, any use of the previously asked cessation methods, quit attempts in the previous month, and visits to their physician since the last survey.
Physicians responded to a baseline questionnaire about their training, type of practice, smoking history, and years since graduating from medical school. Clinicians were asked to report the quality of tobacco cessation training previously received with responses from very good, good, fair, poor, very poor, or no training received. Items about physicians practice in addressing smoking in the office included asking patients about tobacco use, recording their use in the medical record, counseling smokers to quit, smoking cessation counseling techniques used (reduce number of cigarettes per day, inform of risks of smoking and benefits of quitting, evaluating for motivation to quit), setting a quit date, and use of brochures, referral to a quit line or website, prescribe any indicated medications (nicotine replacement, bupropion, varenicline) and explain withdrawal symptoms. Physicians were also asked to estimate the average amount of time in minutes spent counseling.
Outcomes
The primary outcome measure was point-prevalence abstinence at 6 and 12 months. Secondary outcomes were quit attempts in the past month, use of medications to quit smoking, motivation to quit defined as the proportion of daily smokers who were ready to quit in the next month and those who were ready to quit during the next 12 months, and number of cigarettes smoked per day.
During each survey, patients were asked specific process variables about the index clinical visit at the 1-month survey, the visits over the previous 5 months at the 6-month survey and the visits that had occurred in the previous 6 months at the 12-month survey. Process variable outcomes included patient reports of whether their physician asked about their smoking status, advised them to quit smoking, advised them to reduce the number of cigarettes smoked, set a quit date, gave them a pamphlet about quitting, recommended a website, recommended a guide and whether they agreed to a follow-up appointment to discuss tobacco use in-person or by telephone.
Data Analysis
The longitudinal data had a two-level structure for physician outcomes (physicians, repeated measures within physicians) and a three-level structure for patient outcomes (physicians, patients within physicians, and repeated measures within patients). Intention to treat analyses included generalized linear mixed models with random intercepts that regressed longitudinally assessed binary or continuous outcomes onto X variables describing random group assignment, categorical time of assessment, and the group × time interaction. Primary analyses fit generalized linear mixed models to all available data from all participants and invoked the missing at random assumption. For the 7-day point prevalence outcome only, we additionally fit a generalized linear mixed model under the assumption that missing=smoking. As an adjunct to each model, custom contrasts tested group differences at each assessment. Reported levels of outcome response are model-predicted means or percentages, as appropriate.
Among physicians, we compared the baseline distribution of the demographic variables including age and gender, and years since graduation from medical school between intervention and control groups. We also compared smoking behavior, quality of training in tobacco cessation counseling, type of assistance in tobacco cessation they provide to their patients, and average time during patient visits devoted to tobacco counseling between intervention and control groups, at baseline and at 12 months.
Among patients, we compared demographic variables (gender, age, years of education), perceived health status, depressive symptoms and tobacco use, at the 1-month survey between intervention and control patients, adjusting for clustering of patients within physicians. We also compared main study outcomes (point prevalence abstinence, quit attempt in past month, use of medications to quit smoking, motivation to quit smoking in next month, and in next 12 months, and number of cigarettes per day) and process variable outcomes between intervention and control groups, at the 1-month, 6-month, and 12-month surveys.
Results
Of 620 physicians invited to participate, 254 (41%) agreed and were randomized. The average age was 44.5 years, 52% were women and 181 (71%) were general internists or family physicians. Physicians at the “Hospital Italiano” represented the largest group studied ( Table 1 ).
Table 1.
Demographic Characteristics of 254 Physicians at Baseline, Argentina, 2009–2011
| Control group N = 130, N (%) a | Intervention n = 124, N (%) a | Total N = 254, N (%) a | P | |
|---|---|---|---|---|
| Institution b | ||||
| Medicus | 14 (10.8) | 12 (9.7) | 26 (10.2) | .998 |
| Hospital Alemán | 12 (9.2) | 12 (9.7) | 24 (9.5) | |
| Olavarria Public Clinics | 15 (11.5) | 15 (12.1) | 30 (11.8) | |
| La Plata Public Clinics | 24 (18.5) | 24 (19.3) | 48 (18.9) | |
| Hospital Italiano HMO | 55 (42.3) | 53 (42.7) | 108 (42.5) | |
| CEMIC HMO | 10 (7.7) | 8 (6.5) | 18 (7.1) | |
| Specialty | ||||
| General internal medicine | 61 (46.9) | 63 (50.8) | 124 (48.8) | .822 |
| Family medicine | 30 (23.1) | 27 (21.8) | 57 (22.4) | |
| Gynecology | 39 (30.0) | 34 (27.4) | 73 (28.7) | |
| Gender | ||||
| Women | 66 (50.8) | 67 (54.0) | 133 (52.4) | .603 |
| Age (y) | ||||
| 18–34 | 19 (14.8) | 15 (12.2) | 34 (13.6) | .491 |
| 35–49 | 76 (59.4) | 78 (63.4) | 154 (61.3) | |
| 50–64 | 27 (21.1) | 28 (22.8) | 55 (21.9) | |
| ≥65 | 6 (4.7) | 2 (1.6) | 8 (3.2) | |
| Age | ||||
| Mean years ( SD ) | 44.7 (9.8) | 44.3 (9.2) | 44.5 (9.5) | .476 |
| Years since graduation from medical school | ||||
| Mean years ( SD ) | 18.9 (10.3) | 18.3 (9.5) | 18.6 (9.9) | .421 |
CEMIC = Centro de Educación Médica e Investigación Clínica; HMO = health maintenance organization.
a Percentages based on non-missing values.
b Institutions are listed in order of recruitment.
Physician Outcomes
Baseline
Only 12% of physicians were current smokers and 47% of these were nondaily smokers. A majority had never smoked cigarettes and 36% were former smokers. While 24% of physicians reported no previous training on tobacco cessation at baseline, 41% reported good or very good previous training. At baseline, most clinicians asked their patients about smoking, recorded this in the chart, gave advice about quitting, and informed their patients about the benefit of quitting and the risk of continuing to smoke. A majority associated smoking with patient’s current health problems, advised reducing the number of cigarettes per day as a strategy to quit and asked the patients to set a quit date ( Table 2 ). However, at most 10% of physicians used self-help materials or recommended a quit line or website to help their patients quit. About 36% of clinicians discussed withdrawal symptoms, 39% recommended NRT, 45% prescribed bupropion and 19% prescribed varenecline. The mean time reported spent devoted to tobacco counseling was 4.63 minutes ( SD = 3.67), but only 126 responded.
Table 2.
Smoking Cessation Counseling Practices by Physicians at Baseline and 12 Months by Intervention or Control Conditions, Argentina, 2009–2011
| Baseline ( N = 254) | 12 months | ||||||
|---|---|---|---|---|---|---|---|
| Control N = 130 (%) | Intervention N = 124 (%) | P | Control N (%) | Intervention N (%) | P | Group × time interaction* | |
| Tobacco use a | |||||||
| Never smoked | 65 (50.0) | 68 (54.8) | .601 | 42 (48.8) | 50 (54.4) | .401 b | |
| Former smoker | 51 (39.2) | 40 (32.3) | 37 (43.0) | 30 (32.6) | |||
| Some days | 7 (5.4) | 6 (4.8) | 4 (4.7) | 5 (5.4) | |||
| Every day | 7 (5.4) | 10 (8.1) | 3 (3.5) | 7 (7.6) | |||
| Tobacco training a | |||||||
| Very good | 15 (11.8) | 16 (13.1) | .797 | 15 (17.4) | 39 (42.4) | <.001 b | |
| Good | 39 (30.7) | 34 (27.9) | 29 (33.7) | 45 (48.9) | |||
| Fair | 26 (20.5) | 30 (24.6) | 17 (19.8) | 6 (6.5) | |||
| Poor | 12 (9.4) | 12 (9.8) | 5 (5.8) | 1 (1.1) | |||
| Very poor | 1 (0.8) | 3 (2.5) | 0 | 0 | |||
| None | 34 (26.8) | 27 (22.1) | 20 (23.3) | 1 (1.1) | |||
| Ask patients about tobacco use | |||||||
| Yes | 91.0 | 89.3 | .759 | 91.9 | 93.7 | .086 | 0.939 |
| Record patients’ tobacco use in medical chart | |||||||
| Yes | 88.1 | 85.5 | .577 | 93.9 | 89.7 | .730 | 0.735 |
| Give advice to patient about quitting | |||||||
| Yes | 89.2 | 89.5 | .928 | 97.7 | 98.1 | .742 | 0.879 |
| Suggest to patients reducing the number of cigarettes | |||||||
| Yes | 65.2 | 69.0 | .346 | 69.3 | 60.4 | .680 | 0.058 |
| Link current smoking with a health problem | |||||||
| Yes | 57.1 | 58.6 | .806 | 67.5 | 68.6 | .654 | 0.953 |
| Inform patients about risks of smoking | |||||||
| Yes | 84.5 | 88.6 | .276 | 92.0 | 92.1 | .895 | 0.580 |
| Inform patients of the benefits of quitting smoking | |||||||
| Yes | 79.2 | 82.9 | .376 | 86.5 | 93.0 | .160 | 0.399 |
| Evaluate patients’ motivation to quit | |||||||
| Yes | 61.1 | 53.0 | .269 | 58.7 | 67.0 | .194 | 0.026 |
| Ask to set a quit date for patients | |||||||
| Yes | 38.4 | 37.9 | .924 | 39.5 | 54.0 | .025 | 0.039 |
| Use self-help cessation brochures | |||||||
| Yes | 7.8 | 7.5 | .909 | 15.1 | 36.4 | <.001 | 0.010 |
| Recommend a smoking cessation website | |||||||
| Yes | 9.3 | 4.9 | .261 | 7.4 | 32.9 | <.001 | <0.001 |
| Recommend a telephone quit line | |||||||
| Yes | 6.2 | 3.2 | .378 | 5.6 | 19.6 | <.001 | 0.009 |
| Explain withdrawal symptoms | |||||||
| Yes | 42.1 | 31.2 | .188 | 36.0 | 44.9 | .061 | 0.004 |
| Prescribe medications to help quit smoking | |||||||
| Yes | 18.7 | 18.0 | .275 | 19.1 | 29.3 | .554 | 0.088 |
| Recommend/prescribe nicotine replacement therapy | |||||||
| Yes | 42.6 | 37.7 | .698 | 48.2 | 58.6 | .141 | 0.019 |
| Recommend/prescribe bupropion | |||||||
| Yes | 47.2 | 50.7 | .684 | 47.1 | 58.8 | .138 | 0.126 |
| Recommend/prescribe varenicline | |||||||
| Yes | 17.1 | 18.0 | .524 | 17.4 | 20.3 | .885 | 0.700 |
| Time in the visit devoted to tobacco cessation counseling | |||||||
| >3 min | 55.0 | 50.0 | .852 | 60.3 | 75.2 | .095 | 0.957 |
a Percentages based on non-missing values. All other percentages are model-predicted.
b P values from separate chi-square tests, stratified by time of assessment. All other P values were from corresponding generalized linear mixed models.
* P values for group × time interaction are from generalized linear latent and mixed models analysis (GLLAMM) accounting for clustering of observations by physician and repeated measures per patient.
12 Months
At the end of the study 178 of 254 (70.1%) physicians responded to the 12-month questionnaire, 86 from the control group and 92 from the intervention group; results are shown in Table 2 . There was a significant difference at 12 months between groups in the self-reported quality of training in tobacco cessation received, with 44 physicians (51%) in the control group and 84 (91%) in the intervention group reporting very good or good training ( P < .001). Most counseling strategies did not differ between intervention and control groups but intervention physicians were significantly more likely at 12 months to ask their patients to set a quit date, recommend use of self-help brochures, refer to a website or to a telephone quit line for cessation advice ( Table 2 ). There were no group differences in reported use of any cessation medications although there were nonsignificant trends for physicians in the intervention to explain withdrawal symptoms more frequently and to spend more time during the visit devoted to tobacco counseling compared to control physicians.
Patient Outcomes
At the 1-month interview a total of 1378 smoking patients were surveyed; 81% were women, 45% had more than 12 years of education, 81% rated their health status as good or excellent, all had visited their physician at least once, and 63% had access to the Internet ( Table 3 ). All patients reported smoking the month before the telephone call but 43 (3%) patients had quit smoking after the index clinical visit and before the survey was completed. Among respondents who were smoking at the time of the survey, most were daily smokers (1059 or 77%) but 276 (20%) were nondaily smokers only. Among all smokers, 8% stated their doctor did not know they smoked and an additional 9% were uncertain if their doctor knew. About 43% of patients endorsed one of the depression screener questions. At the 1-month interview, the mean number of cigarettes per day reported by daily smokers was 12.9 ( SD = 8.8), 41% lit their first cigarette in the first hour after awakening, 23% were ready to quit within the next month while 26% thought they would be ready to quit within the next 12 months ( Table 3 ).
Table 3.
Characteristics of 1378 Smoking Patients at the 1-Month Interview Seen by Study Physicians, Argentina, 2009–2011
| Control group n = 628, n (%) a | Intervention group n = 750, n (%) a | Total n = 1378, n (%) a | P b | |
|---|---|---|---|---|
| Institution | ||||
| Medicus | 71 (11.3) | 90 (12.0) | 161 (11.7) | .568 |
| Hospital Alemán | 85 (13.5) | 92 (12.3) | 177 (12.8) | |
| Olavarria | 76 (12.1) | 61 (8.1) | 137 (9.9) | |
| La Plata | 69 (11.0) | 170 (22.7) | 239 (17.3) | |
| Hospital Italiano | 243 (38.7) | 251 (33.4) | 494 (35.9) | |
| CEMIC | 84 (13.4) | 86 (11.5) | 170 (12.3) | |
| Gender | ||||
| Women | 504 (80.3) | 610 (81.3) | 1114 (80.9) | .737 |
| Age | ||||
| 18–34 | 154 (26.3) | 216 (30.2) | 370 (28.5) | .689 |
| 35–49 | 154 (26.3) | 182 (24.5) | 336 (25.8) | |
| 50–64 | 175 (29.8) | 195 (27.3) | 370 (28.5) | |
| ≥65 | 103 (17.6) | 121 (17.0) | 224 (17.2) | |
| Education | ||||
| Less than high school | 179 (28.9) | 228 (30.7) | 407 (29.8) | .348 |
| High school | 153 (24.7) | 196 (26.4) | 349 (25.6) | |
| Some college | 172 (27.7) | 212 (28.5) | 384 (28.2) | |
| College graduates | 116 (18.7) | 107 (14.4) | 223 (16.4) | |
| Health status | ||||
| Excellent/very good/good | 529 (84.2) | 592 (78.9) | 1121 (81.3) | .058 |
| Fair/bad | 99 (15.8) | 158 (21.1) | 257 (18.7) | |
| Access to internet | ||||
| Yes | 407 (65.2) | 457 (61.3) | 864 (63.1) | .471 |
| Depressive symptoms: sad feelings | ||||
| N/A | 8 (1.3) | 6 (0.8) | 14 (1.0) | .425 |
| Yes | 260 (41.4) | 336 (44.9) | 596 (43.3) | |
| No | 360 (57.3) | 407 (54.3) | 767 (55.7) | |
| Depressive symptoms: lack of interest | ||||
| N/A | 14 (2.2) | 11 (1.5) | 25 (1.8) | .251 |
| Yes | 204 (32.5) | 273 (36.5) | 477 (34.7) | |
| No | 410 (65.3) | 463 (62.0) | 873 (63.5) | |
| Does your doctor know you smoke? c | ||||
| Yes | 366 (80.3) | 471 (85.3) | 837 (83.0) | .182 |
| No | 42 (9.2) | 34 (6.2) | 76 (7.6) | |
| No answer/unknown | 48 (10.5) | 47 (8.5) | 95 (9.4) | |
| Tobacco use | ||||
| Smoke every day | 475 (75.6) | 584 (77.9) | 1059 (76.9) | .551 |
| Smoke some days | 134 (21.4) | 142 (18.9) | 276 (20.0) | |
| None (already quit) | 19 (3.0) | 24 (3.2) | 43 (3.1) | |
| Time to first cigarette (daily only) | n = 475, n (%) a | n = 584, n (%) a | N = 1059, n (%) a | |
| 5min or less | 57 (12.0) | 52 (8.9) | 109 (10.3) | .334 |
| Between 6–30 min | 68 (14.3) | 75 (12.8) | 143 (13.5) | |
| Between 31–60 min | 80 (16.8) | 99 (16.9) | 179 (16.9) | |
| More than 60 min | 270 (56.8) | 358 (61.3) | 628 (59.3) | |
| Motivation to quit smoking (daily only) | n = 475, n (%) a | n = 584, n (%) a | N = 1059, n (%) a | |
| Ready in next month | 109 (23.0) | 131 (22.4) | 240 (22.7) | .416 |
| In the next 12 months | 117 (24.6) | 163 (27.9) | 280 (26.4) | |
| Not motivated to quit | 249 (52.4) | 290 (49.7) | 539 (50.9) | |
| What did physician recommend? | n = 628, n (%) a | n = 750, n (%) a | N = 1378, n (%) a | |
| Asked about smoking | 413 (65.7) | 545 (72.7) | 958 (69.5) | .058 |
| Advised to quit | 397 (63.2) | 517 (68.9) | 914 (66.3) | .109 |
| Reduce cigarettes | 354 (56.4) | 469 (62.5) | 823 (59.7) | .108 |
| Set a quit date | 13 (2.1) | 20 (2.7) | 33 (2.4) | .486 |
| Give a pamphlet | 78 (12.4) | 150 (20.0) | 228 (16.6) | .003 |
| Recommend website | 32 (5.1) | 60 (8.0) | 92 (6.7) | .087 |
| Recommend a guide | 42 (6.7) | 75 (10.0) | 117 (8.5) | .066 |
| Follow-up appointment | 6 (1.2) | 7 (1.2) | 13 (1.2) | .951 |
| Telephone follow-up | 2 (0.4) | 4 (0.7) | 6 (0.6) | .567 |
| Quit after the visit | 19 (3.0) | 24 (3.2) | 43 (3.1) | .551 |
CEMIC = Centro de Educación Médica e Investigación Clínica.
a Percentages based on non-missing values.
b P values account for clustering of observations by physician.
c Among current smokers only; this question was added later so there are 370 missing answers.
At the 1-month interview, 70% of patients reported that their physicians asked about smoking during the index clinical visit, 66% were advised to quit and 60% were recommended to reduce the number of cigarettes they smoked. Only 17% of participants received a pamphlet (20% intervention and 12% control group), 7% a recommendation to use a web site, 9% a self-help guide and 2% reported setting a quit date ( Table 3 ).
At 6 months, 1107 patients (80%) responded to the follow up survey and at 12 months, 933 (68%). All patients reported at least one visit to their physician in the intervals between surveys at 1, 6, and 12 months. Primary generalized linear mixed models estimated cessation rates in the control group at 6 and 12 months equal to 15.1% and 23.0%, respectively, compared to 17.0% and 24.1% in the intervention group at 6 and 12 months respectively ( Table 4 ). In an analysis where missing data equals smoking, the corresponding cessation rates at 6 and 12 months were 11.9% and 15.6% ( P = .406), for the control condition, respectively, compared to 13.6% and 16.4% for the intervention group ( P = .729; not shown in table). Among the patients who reported smoking cessation at 12 months, the median days quit was 135 for control participants and 180 for intervention participants The proportions with a serious quit attempt at 6 and 12 months in the control group were 13.8% and 21.4% respectively, and 15.3% and 23.8% in the intervention group. Use of any recommended medications for tobacco cessation was 11% in the control group and 13% in the intervention group at 12 months. The proportion of patients who were motivated to quit smoking in the next month did not differ between intervention and control groups. Similarly, the mean the number of cigarettes smoked per day did not differ by intervention condition ( Table 4 ). None of the group × time interactions for these outcomes were statistically significant.
Table 4.
Outcomes in 1378 Patients by Intervention or Control Condition at 1-Month, 6-Month, and 12-Month Surveys, Argentina, 2009–2011 (628 Control and 750 Intervention)
| 1-month survey a | 6-month survey | 12-month survey | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Control % b | Intervention % b | P | Control % b | Intervention % b | P | Control % b | Intervention % b | P | Group × time interaction c | |
| Tobacco abstinence | 3.1 | 3.2 | .921 | 15.1 | 17.0 | .285 | 23.0 | 24.1 | .435 | 0.894 |
| Quit attempt in past month | 7.9 | 7.1 | .744 | 13.8 | 15.3 | .386 | 21.4 | 23.8 | .312 | 0.558 |
| Used medications to quit | 5.9 | 5.8 | .848 | 9.4 | 9.6 | .726 | 10.9 | 12.1 | .322 | 0.832 |
| Ready to quit in next month (daily smokers) | 23.2 | 22.9 | .833 | 15.8 | 17.5 | .658 | 18.1 | 18.1 | .915 | 0.758 |
| Motivated to quit within 12 months (daily smokers) d | 47.5 | 51.1 | .370 | 43.7 | 50.0 | .174 | 42.2 | 43.2 | .765 | 0.525 |
| Mean cigarettes/d | 13.3 | 12.7 | .212 | 12.9 | 12.2 | .530 | 12.3 | 11.9 | .964 | 0.916 |
| Dr asked about smoking | 67.3 | 72.7 | .004 | 74.0 | 76.6 | .155 | 74.9 | 81.3 | .037 | 0.385 |
| Dr advised to quit | 64.8 | 69.7 | .022 | 67.0 | 73.0 | .016 | 70.2 | 75.9 | .136 | 0.873 |
| Dr advised to reduce number of cigarettes | 58.3 | 63.4 | .018 | 63.8 | 68.9 | .028 | 63.3 | 69.3 | .084 | 0.933 |
| Set a quit date | 2.2 | 2.5 | .521 | 2.7 | 2.7 | .705 | 4.1 | 4.4 | .373 | 0.971 |
| Gave a pamphlet | 13.1 | 19.4 | <.001 | 18.7 | 23.8 | .021 | 25.2 | 29.2 | .138 | 0.332 |
| Recommended a website | 5.2 | 7.9 | .048 | 6.3 | 8.0 | .328 | 10.6 | 11.2 | .725 | 0.415 |
| Recommended a guide | 7.1 | 10.0 | .044 | 7.8 | 10.7 | .080 | 15.1 | 14.6 | .993 | 0.168 |
| Agreed to in-person follow-up appointment | 1.7 | 1.3 | .960 | 3.4 | 1.8 | .224 | 1.9 | 2.8 | .209 | 0.198 |
| Agreed to follow-up appointment by telephone | 0.6 | 0.9 | .657 | 2.4 | 2.0 | .634 | 0.4 | 1.3 | .258 | 0.377 |
a 1-month survey was completed within 30 days of index clinical visit after physician randomization and intervention.
b Tabled Percentages and means are model-predicted values from the corresponding generalized linear mixed model (GLMM).
c P values for group by time interaction are from GLMM analysis accounting for clustering of observations by physician and repeated measures per patient.
d Includes patients who answered they were planning to quit within next month, or within next 12 months.
At the 1-month interview intervention patients were more likely than control patients to report that their physician gave them a smoking cessation pamphlet (20% vs. 12%, P = .003), but this difference did not persist at 6 or 12 months ( Table 4 ). At 6 months, intervention patients were more likely than controls to report that their physician had asked them to set a quit date (72% vs. 66%, P = .046), but this difference did not persist at 12 months. The group × time interactions for these process variable outcomes that were statistically significant at the 6-month survey did not persist at the 12-month survey, indicating that any observed changes in outcomes over time were similar across intervention and control groups, and therefore, there were no lasting intervention effects.
We also analyzed the outcomes for primary care physicians only excluding gynecologists but there were no differences in abstinence rates at 6 months (13.5% vs. 16.6%, P = .23) or 12 months (21.9% vs. 21.6%, P = .92) (results not presented in tables). Finally we analyzed the outcomes for the 520 (49%) daily smokers motivated to quit within next 12 months. There was a significant intervention effect on point prevalence abstinence at 6 months (17.7% vs. 9.6% P = .027) that did not persist at 12 months (21.5% vs. 22.6%, P = .83), and a significant group × time interaction ( P = .034). A nonsignificantly higher proportion of the intervention group made a serious quit attempt in the previous month at 1-year follow-up compared to the control group (30.1% vs. 21.4%, P = .08). There were no significant differences by intervention assignment in cigarettes per day or having used medications to try to quit at either 6 or 12 months.
Discussion
This study showed that providing standardized training in tobacco cessation to primary care physicians practicing in Argentina did not improve the cessation rates among their patients at 6 or 12 months of follow-up. Despite the negative results of our main outcome, physicians participating in the study did perceive that the quality of their training in tobacco cessation improved significantly and they were more likely to report use of evidence-based counseling practices with their patients. Although 40% of respondents in our study reported having received poor quality or no training at all in tobacco cessation, lack of knowledge did not explain the low commitment of physicians with tobacco cessation interventions.
The 2013 Cochrane systematic review showed that overall patients who were counseled by their clinicians were more likely to quit, 7 but this research has not been conducted in middle-income countries. Studies infrequently described the motivation to quit of randomized participants. In a New York study, only 7% of 518 randomized patients were pre-contemplators, but intervention effects were not statistically significant (12% abstinence vs. 8%). 25 In our study there was a significant effect among motivated daily smokers at 6 months that did not persist. Earlier physician interventions were done at a time when there was little else available to promote smoking cessation and current policy changes facilitating cessation through indoor smoking restriction, increased cost of cigarettes through additional taxes, and alternative available interventions may limit the efficacy of a clinical intervention by strengthening a no-smoking societal norm.
Training clinicians to learn how to counsel patients on behavior change of smoking cessation is by evidence-based standards worthwhile to implement. Training improves general attitudes and approach to tobacco use as a medical problem and may promote staff engagement on this issue. Clinicians may not implement cessation counseling because of barriers and perceived low efficacy of intervention effect on quitting smoking. 26 Clinicians usually do not spend more than 5 minutes on a cessation intervention and one alternative strategy would focus on training to refer to higher efficacy interventions. Studies have shown that training physicians to refer to cessation-focused specialists or quit lines is effective and this can be complementary to direct smoking cessation counseling. 27
Nondaily smokers made up nearly 30% of the study participants, as they have become a larger proportion of current smokers. This may be one reason why we did not find significant differences, as interventions in nondaily smokers may need to differ and have not been developed. Contamination from increased counseling among control physicians may also have occurred given that that we randomized physicians to intervention or control within the same health system and may not have avoided their interaction. Intervention physicians did increase practice of four specific cessation techniques and a higher proportion dedicated 3 minutes or more to cessation counseling compared to control physicians. However, all participating physicians were highly motivated to learn smoking cessation expertise and this may have contributed to a null effect. 28
Another reason that may have led to a null result of the intervention is a possible ceiling effect due to the sample selection of physicians. Half of the participants had received training in tobacco cessation, 70% of them worked in clinical systems that were centers of excellence in health care with academic institutions and some prior experience with smoking cessation programs, and their smoking prevalence was lower than the previously reported rates for Argentine physicians. 2 , 29 The physicians in our study may have been more motivated and committed to smoking cessation with their patients and might be non-representative of the general population of Argentine physicians.
The intervention may have led to null results because it was based on the trans-theoretical model and there are concerns about the usefulness of this approach. 30 We used the model in large part because it has been the framework used to deliver clinician assisted interventions to promote smoking cessation and many organizations continue to use the framework to implement smoking cessation interventions in health care systems such as in Argentina’s National Guidelines for Tobacco Cessation. 31 Finally, we cannot exclude the possibility that the intervention lacked the elements, duration or intensity to produce the desired behavioral changes in physicians. Although participants were motivated to improve their skills in helping their patients quit and we delivered periodic reminders through email, perhaps a more intensive intervention could have had better results. Regardless, using the missing=smoking convention, about 16% of patients exposed to physicians over the year reported abstinence independent of intervention or control.
During the study period in Argentina many cities and provinces have passed laws that protect persons from passive smoking, limited advertising of tobacco products and prohibited the sale of cigarettes to minors. In 2011, the National Law against tobacco was passed but the public discussions took place while the study was being implemented. These social and political changes may have influenced physicians and could explain the increase in some performance indicators in the control group and therefore the lack of effect of the intervention. During the study period Argentina has experienced a dramatic decrease in cigarette smoking rates decreased from 37% in 2004 1 to 22% in 2012. 32
In conclusion, providing training to primary care physicians and gynecologists did not result in increased abstinence rate among randomly selected smokers at 6 and 12 months. However, about 23.5% of patients reported abstinence at 1 year that is surprisingly high for any type of educational or counseling intervention. The participating physicians also reported an increase in selected cessation methods. It is necessary to explore alternative strategies to change clinician behavior on this important health issue and to incorporate their role in the overall public health goal of promoting smoking cessation.
Funding
This research was funded by grant number TW05935 from the Tobacco Research Network Program, Fogarty International Center, National Cancer Institute, National Institute of Drug Abuse, National Institutes of Health, the National Cancer Institute for Redes en Acción (U01CA86117 and U54CA153511) and by grant number 001726-037 from Research on International Tobacco Control, International Development Research Center, Canada.
Declaration of Interests
None declared.
Acknowledgments
We thank the directors of the respective clinical institutions that facilitated access to the participating physicians; we also thank Cecilia Populus-Eudave for administrative and research support and Juliette Hong for statistical analyses at UCSF.
References
- 1. Secretaría de Programación para la Prevención de la Drogadicción y la Lucha contra el Narcotráfico . Segundo Estudio Nacional Sobre Consumo de Sustansias Psicoactivas Poblacion de 12 a 65 años . Buenos Aires, Argentina: : Ministerio de Salud; ; 2004. . [Google Scholar]
- 2. Zabert G . Smoking prevalence among Argentinean Physicians . Am Thorac Soc . 1998. ; 157 : A504 abstract. [Google Scholar]
- 3. Programa Nacional de Control del Tabaco . El tratamiento del tabaquismo en la formación médica. Buenos Aires, Argentina: Ministerio de Salud de la Nación . 2006. . www.msal.gov.ar/tabaco/images/stories/institucional/pdf/proy-curric-tabaco.pdf . Accessed July 27, 2015.
- 4. Chapman S . The role of doctors in promoting smoking cessation . BMJ . 1993. ; 307 ( 6903 ): 518 – 519 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cummings SR, Stein MJ, Hansen B, Richard RJ, Gerbert B, Coates TJ . Smoking counseling and preventive medicine. A survey of internists in private practices and a health maintenance organization . Arch Intern Med . 1989. ; 149 : 345 – 349 . [DOI] [PubMed] [Google Scholar]
- 6. Kottke TE, Brekke ML, Solberg LI, Hughes JR . A randomized trial to increase smoking intervention by physicians. Doctors Helping Smokers, Round I . JAMA . 1989. ; 261 ( 14 ): 2101 – 2106 . [PubMed] [Google Scholar]
- 7. Stead LF, Buitrago D, Preciado N, Sanchez G, Hartmann-Boyce J, Lancaster T . Physician advice for smoking cessation . Cochrane Database Syst Rev . 2013. ; 5 : CD000165 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Silagy C, Stead LF . Physician advice for smoking cessation . Cochrane Database Syst Rev . 2001. ; 2 : CD000165 . [DOI] [PubMed] [Google Scholar]
- 9. Wallace PG, Brennan PJ, Haines AP . Are general practitioners doing enough to promote healthy lifestyle? Findings of the Medical Research Council’s general practice research framework study on lifestyle and health . Br Med J (Clin Res Ed) . 1987. ; 294 (6577): 940 – 942 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Eckert T, Junker C . Motivation for smoking cessation: what role do doctors play? Swiss Med Wkly . 2001. ; 131 (35–36): 521 – 526 . [DOI] [PubMed] [Google Scholar]
- 11. Rogers LQ, Johnson KC, Young ZM, Graney M . Demographic bias in physician smoking cessation counseling . Am J Med Sci . 1997. ; 313 ( 3 ): 153 – 158 . [DOI] [PubMed] [Google Scholar]
- 12. Denny CH, Serdula MK, Holtzman D, Nelson DE . Physician advice about smoking and drinking: are U.S. adults being informed? Am J Prev Med . 2003. ; 24 ( 1 ): 71 – 74 . [DOI] [PubMed] [Google Scholar]
- 13. Vogt F, Hall S, Marteau TM . General practitioners’ and family physicians’ negative beliefs and attitudes towards discussing smoking cessation with patients: a systematic review . Addiction . 2005. ; 100 ( 10 ): 1423 – 1431 . [DOI] [PubMed] [Google Scholar]
- 14. Humair JP, Cornuz J . A new curriculum using active learning methods and standardized patients to train residents in smoking cessation . J Gen Intern Med . 2003. ; 18 ( 12 ): 1023 – 1027 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jaén CR, McIlvain H, Pol L, Phillips RL, Jr, Flocke S, Crabtree BF . Tailoring tobacco counseling to the competing demands in the clinical encounter . J Fam Pract . 2001. ; 50 (10): 859 – 863 . [PubMed] [Google Scholar]
- 16. Hu S, McAlister AL, Meshack AF, Margolis JA . Physicians’ views and practice of smoking cessation . Tex Med . 2003. ; 99 ( 11 ): 57 – 63 . [PubMed] [Google Scholar]
- 17. Schroeder SA . What to do with a patient who smokes . JAMA . 2005. ; 294 ( 4 ): 482 – 487 . [DOI] [PubMed] [Google Scholar]
- 18. Woolf SH, Glasgow RE, Krist A, et al. Putting it together: finding success in behavior change through integration of services . Ann Fam Med . 2005. ; 3 ( suppl 2 ): S20 – 27 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. University of California San Francisco . Rx for Change . 2004. . http://rxforchange.ucsf.edu/ . Accessed July 5, 2013 .
- 20. Prochaska JO, Velicer WF . The transtheoretical model of health behavior change . Am J Health Promot . 1997. ; 12 (1): 38 – 48 . [DOI] [PubMed] [Google Scholar]
- 21. Pérez-Stable EJ, Sabogal F, Marín G, Marín BV, Otero-Sabogal R . Evaluation of “Guia para Dejar de Fumar,” a self-help guide in Spanish to quit smoking . Public Health Rep . 1991. ; 106 : 564 – 570 . [PMC free article] [PubMed] [Google Scholar]
- 22. National Cancer Institute , ed. Guia para dejar de fumar [Guide for quitting smoking] . Washington, DC: : Department of Health and Human Services; ; 2002. . [Google Scholar]
- 23. Munoz RF, Lenert LL, Delucchi K, et al. Toward evidence-based Internet interventions: a Spanish/English Web site for international smoking cessation trials . Nicotine Tob Res . 2006. ; 8 ( 1 ): 77 – 87 . [DOI] [PubMed] [Google Scholar]
- 24. Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO . The Fagerström Test for Nicotine Dependence: a revision of the Fagerström Tolerance Questionnaire . Br J Addict . 1991. ; 86 (9): 1119 – 1127 . [DOI] [PubMed] [Google Scholar]
- 25. Unrod M, Smith M, Spring B, DePue J, Redd W, Winkel G . Randomized controlled trial of a computer-based, tailored intervention to increase smoking cessation counseling by primary care physicians . J Gen Intern Med . 2007. ; 22 ( 4 ): 478 – 484 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Coleman T, Murphy E, Cheater F . Factors influencing discussion of smoking between general practitioners and patients who smoke: a qualitative study . Br J Gen Pract . 2000. ; 50 (452): 207 – 210 . [PMC free article] [PubMed] [Google Scholar]
- 27. McRobbie H, Hajek P, Feder G, Eldridge S . A cluster-randomised controlled trial of a brief training session to facilitate general practitioner referral to smoking cessation treatment . Tob Control . 2008. ; 17 ( 3 ): 173 – 176 . [DOI] [PubMed] [Google Scholar]
- 28. Schoj V, Mejia R, Alderete M, et al. . Use of smoking cessation interventions by physicians in Argentina [published online ahead of print November 21, 2014] . J Smok Cessat . 2014. . doi: 10.1017/jsc.2014.24 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Minervini MC, Zabert G, Rondelli M, et al. Tobacco use among Argentine physicians: personal behaviour and attitudes . Revista Argentina de Medicina Respiratoria . 2006. ; 3 : 100 – 105 . [Google Scholar]
- 30. West R . Time for a change: putting the Transtheoretical (Stages of Change) Model to rest . Addiction . 2005. ; 100 (8): 1036 – 1039 . [DOI] [PubMed] [Google Scholar]
- 31. Ministerio de Salud . Guia de Practica Clinica Nacional de Tratamiento de la Adiccion al Tabaco . Buenos Aires, Argentina: : Ministerio de Salud de la Nacion; ; 2014. . www.msal.gov.ar/images/stories/bes/graficos/0000000536cnt-2014-09_guia-tratamiento-adiccion-tabaco-2014.pdf . Accessed July 27, 2015. [Google Scholar]
- 32. Ministerio de Salud . GATS. Encuesta Mundial de Tabaquismo en Adultos . Buenos Aires, Argentina: : Ministerio de Salud de la Nacion; ; 2013. . www.msal.gov.ar/tabaco/images/stories/info-para-ciudadanos/pdf/2013-07_GATS_FactSheetARG_FINAL_spanish.pdf . Accessed July 27, 2015. [Google Scholar]