Recently, reports of syphilis have increased rapidly in Japan, with most cases being men who have sex with women and young women who have sex with men.
Abstract
Background
In Japan, syphilis reports have recently increased rapidly. However, unlike other developed countries where men who have sex with men (MSM) were associated with the rise, the increase in Japan has been attributed more to men who have sex with women (MSW) and women who have sex with men (WSM). We report on this increase based on surveillance data.
Methods
Syphilis is a notifiable disease requiring all laboratory-confirmed cases to be reported; stage and sex of the sex partner(s) suspected as the infection source are also reported. Focusing on primary and secondary (P&S) cases, we describe the temporal, demographic, and geographic distributions of reported cases in 2012 through 2016.
Results
A total of 7040 (64.0%) of 10,997 cases were P&S; the annual rate of increase was greatest for P&S and the proportion of P&S increased over time. Among P&S cases (1609 MSM, 2768 MSW, and 1323 WSM), MSW and WSM each surpassed MSM cases in 2016. Men were older with a wider age distribution (median, 37 years; interquartile range, 28–46 years) relative to women (median, 26 years; interquartile range, 21–34 years). Among women, 20- to 24-year-olds consistently had the highest reporting rate, reaching 9.0 per 100,000 in 2016. Congenital syphilis reports increased from 0.4 in 2012 to 1.4 per 100,000 live births in 2016. Although Tokyo prefecture had the highest reporting rate (3.98 per 100,000 person-years), the proportionate contribution from Tokyo decreased in 2016.
Conclusions
Reports on P&S syphilis increased yearly among MSW and WSM. Young women seem to be at particular risk, and with increased reports of congenital syphilis, syphilis prevention and control is currently a public health priority in Japan.
Syphilis has recently returned to the global scene as a reemerging public health concern, and Japan has been no exception, with reports of syphilis rapidly increasing in the last few years. Similar to many other countries, this old sexually transmitted infection (STI) caused by Treponema pallidum has a long history in Japan and has been a nationally notifiable disease since 1948 under the Venereal Diseases Prevention Law. Although its resurgence has been reported from many other countries, some of the epidemiologic features observed in the current increase in Japan have been distinct from those reported elsewhere.
Similar to other developed settings,1–6 the initial increase in syphilis reports was associated mostly with men who have sex with men (MSM),7–9 but the more recent—and dramatic—rise has been linked to men who have sex with women (MSW) and women who have sex with men (WSM).10,11 Although there have been reports of increase in cases among women elsewhere such as in the United States,1,12 the magnitude of the increase in WSM and MSW in Japan has been remarkable. Here, focusing on primary and secondary (P&S) syphilis, we describe the temporal, demographic, and geographic trends and distributions of syphilis cases based on reported surveillance data, and highlight potential risk groups and ongoing public health responses.
MATERIALS AND METHODS
In Japan, in accordance with the Infectious Diseases Control Law established in 1999 and updated in 2007, syphilis has been a nationally notifiable disease, with data managed in its current standardized format under the National Epidemiological Surveillance of Infectious Diseases (NESID) system since May 2006. The reportable case definition of syphilis requires a positive result by both a specific treponemal test (e.g., T. pallidum hemagglutination assay and T. pallidum latex agglutination) and a nonspecific treponemal test (e.g., rapid plasma reagin and latex agglutination), or laboratory identification of T. pallidum (detection by India ink or Giemsa staining method and/or polymerase chain reaction detection of the bacterial genome from skin lesions).7 Physicians are required to report all such cases to the local public health center, who in turn report the data to the prefectural and national level through NESID; although confirmations may be made at a commercial or public health laboratory, reporting must be done by a physician. As a notifiable disease, any physician, regardless of sector (e.g., public or private), is legally required to report all such cases (the health system in Japan is composed of a mixture of public and private hospitals and clinics, and laboratory tests for syphilis are covered by the national health insurance).
For the purposes of national infectious disease surveillance, syphilis is reported based on stages, defined as follows7: primary syphilis, characterized by early induration or hard chancre in the infected site and/or painless enlargement of the inguinal lymph node, appearing approximately 3 to 6 weeks after infection; secondary syphilis, characterized by syphilitic roseola, papular syphilid, or condyloma latum on the skin or mucous membrane approximately 3 months after infection; late (symptomatic) syphilis, characterized by gumma, cardiovascular, neurologic, and/or ocular signs/symptoms that may appear about 3 years or later after infection. If a physician examines a patient with such clinical manifestations and confirms syphilis based on the laboratory methods described earlier, the physician must notify the case within 7 days. In addition, asymptomatic individuals who test positive for a specific treponemal test are also reportable when the following nonspecific treponemal test criteria are met: sera with titer of at least 16 based on the rapid plasma regain card test, the agglutination test or the slide precipitation test, or, sera with titer of at least 16.0 RU, 16.0 U, or 16.0 SU/mL based on automated tests, all using cardiolipin as the antigen.
For congenital syphilis, at least one of the following must be met7: (1) considerably higher antibody level in the infant relative to that of the mother; (2) persisting antibody titer level in the infant, considerably higher than that expected from the maternal antibody; (3) positive IgM antibody against T. pallidum derived from the infant; (4) signs or symptoms of early (e.g., secondary symptomatic syphilitic roseola and osteochondritis) or late (e.g., Hutchinson triad) congenital syphilis.
For the first time in this millennium, annual syphilis reports surpassed a thousand cases in 2013. Thus, we focused on the 5 years from 2012 to 2016 and describe the temporal, demographic, and geographic features of reported syphilis cases, based on NESID (data extracted on March 10, 2017). Data included were method of testing, diagnosis and reporting date, sex, age at diagnosis, self-reported transmission route (i.e., sex of the sex partner(s) suspected as the source of infection), place of report, stage of syphilis (i.e., primary, secondary, asymptomatic, late [symptomatic], or congenital), and the voluntary free text comments. We restricted the main analyses to P&S syphilis because the focus was on recent infections contributing to the current outbreak. Reporting rates were calculated using national population statistics from the Portal Site of Official Statistics of Japan.13 Data were descriptively summarized using STATA (version 10.0). Ethical approval or informed consent was not required because this study was conducted for public health purposes using legally notifiable surveillance data, and identifiable information is not reported.
RESULTS
A total of 10,997 syphilis cases were reported from 2012 to 2016. Most (n = 10,978; 99.8%) were reported based on the combined positive results of the specific treponemal and nonspecific treponemal tests. By stage, 2993 (27.2%) were primary, 4047 (36.8%) were secondary, 3510 (31.9%) were asymptomatic, 402 (3.7%) were late (symptomatic), and 45 (0.4%) were congenital (Table 1). Information on sex was recorded for all cases, and 8070 (73.4%) were men. Information on self-reported sexual transmission route (i.e., sex of the sex partner(s) suspected as the source of infection) was recorded for 9479 (86.2%) cases. Among 7116 men, 3489 (49.0%) were MSW, 2589 (36.3%) were MSM, 72 were recorded as both MSM and MSW (1.0%), and 966 (13.6%) were recorded as “unknown.” Among 2363 women, 2120 (89.7%) were WSM, 17 (0.7%) were women who have sex with women (WSW), 3 (0.1%) were recorded as both WSM and WSW, and 223 (9.4%) were recorded as unknown.
TABLE 1.
Number of Reported Syphilis Cases by Report Year and Stage, Japan, 2012–2016: Total (A), MSM (B), MSW (C), and WSM (D)*
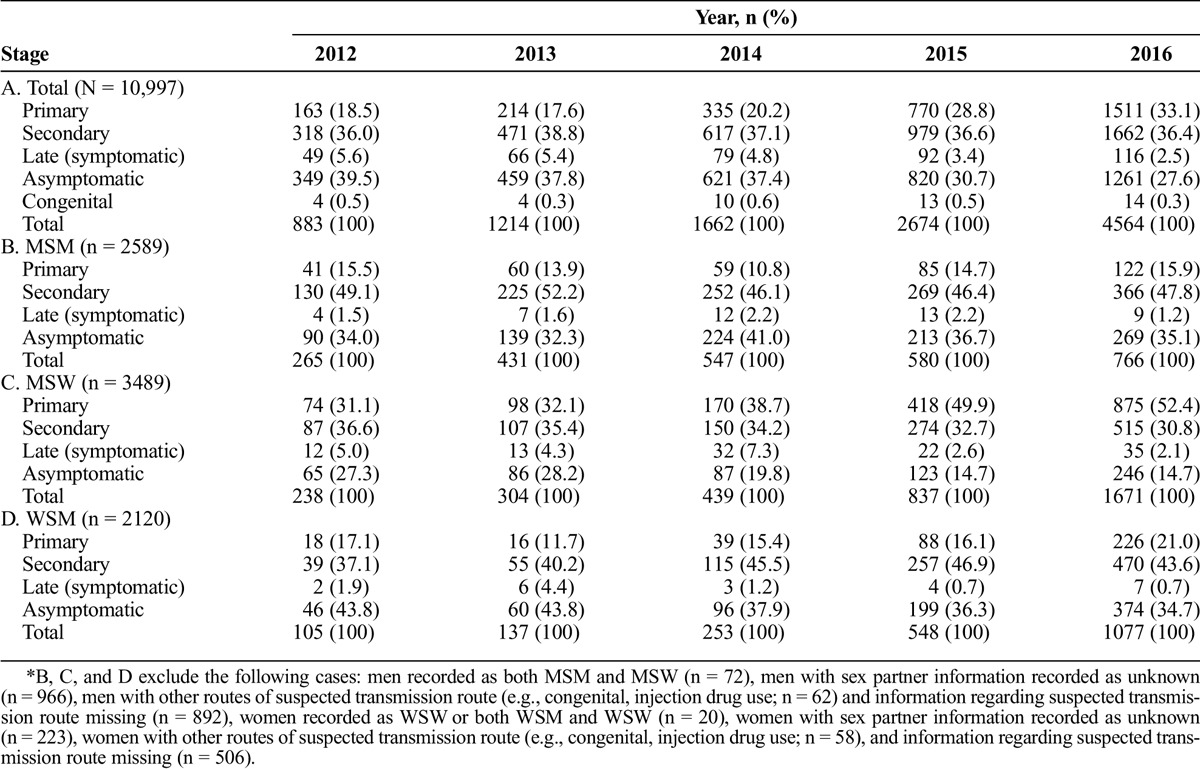
Over time, the distribution of stages changed, with the proportion of cases that were P&S increasing, reaching nearly 70% in 2016 (Table 1). Reports increased every year, with a greater than 5-fold increase from 2012 (0.7 per 100,000) to 2016 (3.6 per 100,000), and this increase was greater for P&S cases (9.3- and 5.2-fold, respectively, or combined P&S of 6.7-fold increase from 0.4 in 2012 to 2.5 per 100,000 in 2016) relative to asymptomatic (3.6-fold) or late (2.4-fold) cases (Table 1). The rate of increase in annual reports compared with the previous year also increased, from 1.4-fold in 2013 to 1.7-fold in 2016; this increase was also greatest for P&S cases, increasing from 1.4-fold in 2013 to 1.8-fold in 2016.
Among the P&S cases (n = 7040), the median age was 35 years (interquartile range [IQR], 26–44 years), and the majority were men (n = 5459 [77.5%]). Information on self-reported sexual transmission route was recorded for 6554 (93.1%) cases; although the distribution was similar to that of all stages, the proportion of MSW was greater and the proportion of MSM was smaller. Among 5098 men, 2768 (54.3%) were MSW, 1609 (31.6%) were MSM, 44 were recorded as both MSM and MSW (0.9%), and 677 (13.3%) were recorded as unknown. Among 1456 women, 1323 (90.9%) were WSM, 11 (0.8%) were WSW, 3 (0.2%) were recorded as both WSM and WSW, and 119 (8.2%) were recorded as unknown.
Assessing sexual transmission routes of P&S cases over time, we observed notable changes. Although most cases were consistently men, the proportion of cases that were men peaked in 2013 at 86.7% and declined to 74.0% in 2016. This distribution was driven by the differential trends among MSM, MSW, and WSM; the largest annual increase in reports in MSM occurred in 2013 (1.7-fold from 2012), whereas MSW and WSM experienced a concomitant and greater rate of increase in the latter years (Table 1 and Fig. 1). Although reports increased every year among all 3 groups, MSW (n = 1390) and WSM (n = 696) cases both surpassed those of MSM (n = 488) in 2016 (Fig. 1B).
Figure 1.
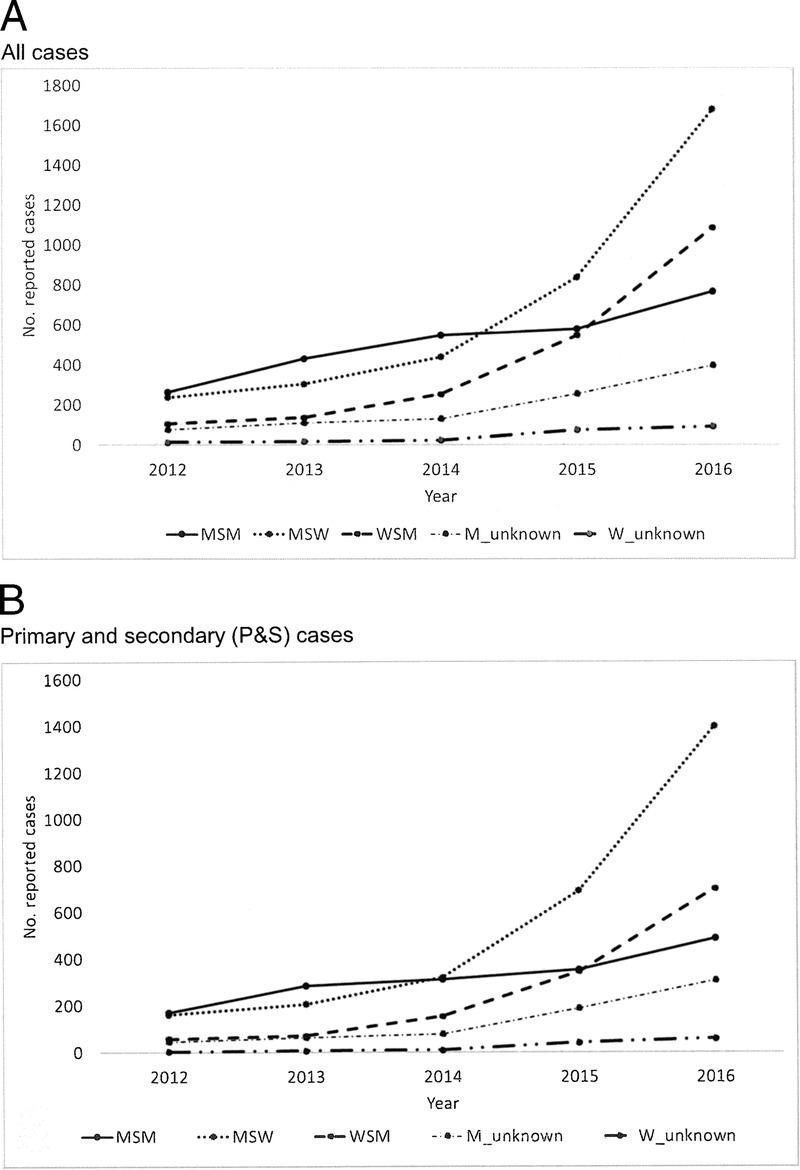
Number of reported syphilis cases by year and sexual transmission route*, Japan, 2012 to 2016. A, All cases. B, P&S cases. *Sexual transmission route based on self-report: M_unknown, men with sex partner information recorded as unknown; W_unknown, women with sex partner information recorded as unknown. Excludes men recorded as both MSM and MSW (total: n = 72; P&S: n = 44) and women recorded as WSW or both WSM and WSW (total: n = 20; P&S: n = 14).
In addition, the age distribution differed considerably when disaggregated by sex, and men (median, 37 years; IQR, 28–46 years) were considerably older than women (median, 26 years; IQR, 21–34 years; Fig. 2). The age distribution among men showed a widespread, with those in their late 20s to early 40s making up 59.6% of the P&S cases (MSM [median, 36 years; IQR, 28–43 years] and MSW [median, 38 years; IQR, 28–46 years]). In contrast, women showed a distribution more highly skewed to the young, with those in their 20s making up 53.6% of P&S cases. Among those younger than 25 years, the reporting rate per 100,000 was higher in women than in men (Fig. 2). Among women, although those aged 20 to 24 years were the most frequently reported age group in all 5 years, the absolute number and the proportion among this age group increased from 2012 (n = 20; 27.8%) to 2016 (n = 268; 32.5%), with the reporting rate increasing from 0.7 to 9.0 per 100,000. Comparing such age distributions over time, differences were also observed between men and women. Among women, although the median age was 26 years for both 2012 and 2016, the distribution became narrower and younger from 2012 (IQR, 23–38 years) to 2016 (22–34 years). In contrast, among men, the age distribution became slightly older; for MSM, the median age (IQR) was 35 years (29–41 years) in 2012 and 36 years (28–44 years) in 2016, and for MSW, it was 37 years (26–46 years) in 2012 and 39 years (29–47 years) in 2016.
Figure 2.
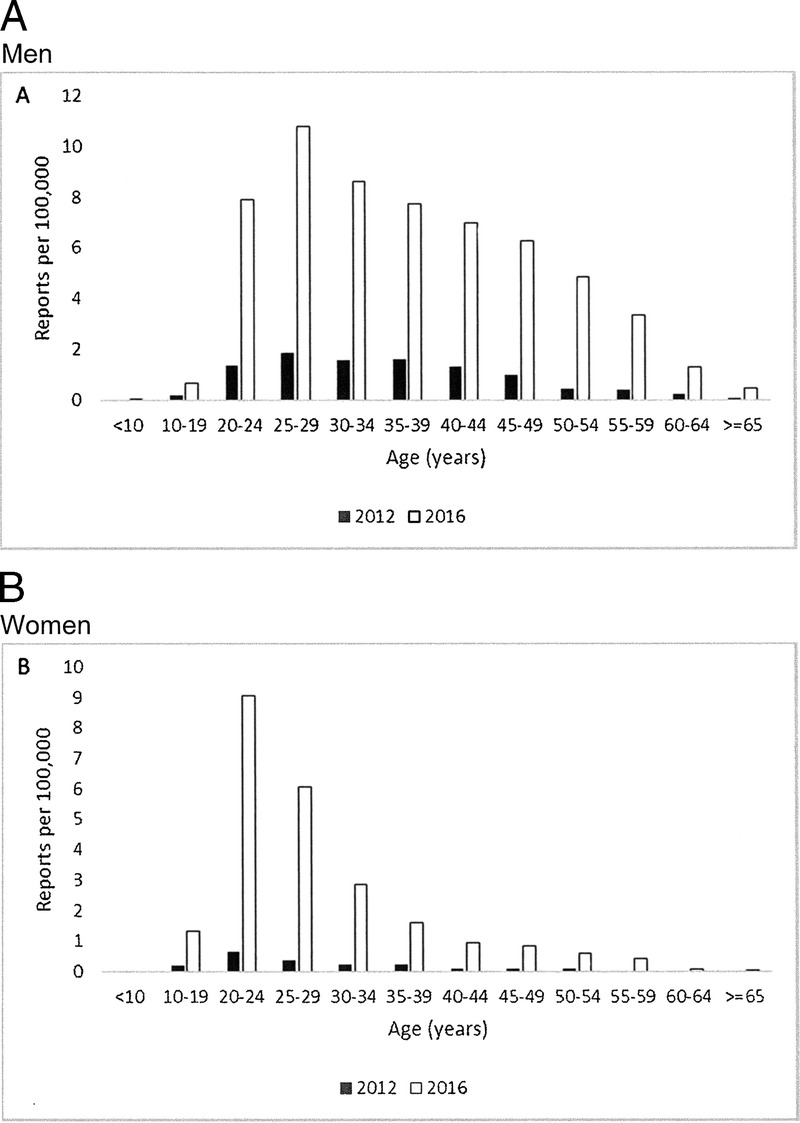
Reporting rate of P&S syphilis cases per 100,000 population, by sex and age, Japan, 2012 and 2016. White bars indicate 2016 and black bars indicate 2012. A, Men. B, Women.
Among P&S cases, Tokyo (n = 2667 [37.9%]) and Osaka (n = 924 [13.1%]), 2 major metropolitan prefectures, reported more than half of all cases and reporting rates were disproportionately higher in these 2 areas (based on the 2014 census data, reporting rate per 100,000 person-years was 3.98 cases in Tokyo and 2.09 cases in Osaka, relative to the national rate of 1.11). Assessing the geographic distribution over time, reports from Tokyo consistently made up approximately a third of the cases, ranging from 31.0% (2014) to 43.1% (2015). In 2016, when the number of reports was highest and the annual rate of increase relative to the previous year was greatest, the proportion of cases reported from Tokyo decreased to 37.6%. Among the 5 other prefectures (Aichi, Hyogo, Kanagawa, Osaka, and Saitama) that also reported more than 100 P&S cases in 2016, the increase in reporting rate per 100,000 population from 2015 to 2016 (ranging from 2.0- to 2.5-fold) was higher than that in Tokyo (1.6-fold increase).
Although reports were few, congenital syphilis cases (n = 45) increased over the study period. Excluding one noninfant case reported in 2014, reports per 100,000 live births increased from 4 cases each in 2012 and 2013 (0.4 per 100,000 live births for both years), 9 in 2014 (0.9 per 100,000 live births), 13 in 2015 (1.3 per 100,000 live births), and 14 in 2016 (1.4 per 100,000 live births). In the free-text comment section, the number of cases among women with either “pregnant” or “found through pregnancy screening” increased over time, from 3 cases in 2012, 6 in 2013, 13 in 2014, 16 in 2015, and 33 in 2016.
DISCUSSION
The current syphilis resurgence observed in Japan is substantial, surpassing 4000 cases in 2016, the first time to reach this mark since the early 1970s. In addition, the epidemiology of the current outbreak—over time, person, and place—seems to be rapidly evolving, with increase in reports every year, particularly for MSW and WSM, and an expansion in geographic area. Importantly, we are not aware of reports from other developed settings where syphilis reports attributed to MSW and WSM transmission have each respectively overtaken those of MSM. In addition, although the age distribution among men was widespread, much of the burden among women was focused among those in their early 20s; in fact, although most reported cases were men, among the young, women actually had higher reporting rates than did men.
The increase in cases among young women is especially concerning. Although there was a broad age group affected throughout the period among men, women aged 20 to 24 years were disproportionately affected and increasingly so over time. In fact, although this age group also had the highest reporting rate in women in the United States in 2015 (5.1 per 100,000),1 and comparisons require caution, the P&S reporting rate in Japan for 2016 (9.0 per 100,000) was far higher. The high frequency of reports in this age group is consistent with that observed from the national STI sentinel surveillance data (a national surveillance system based on approximately 1000 sentinel sites distributed throughout the country, composed mostly of urology and obstetrics/gynecology clinics with monthly aggregate reporting of number of cases of Chlamydia trachomatis, condyloma acuminatum, genital herpes, and Neisseria gonorrhoeae, by sex-disaggregated 5-year age groups), where those aged 20 to 24 years consistently have the highest reporting rates among women for N. gonorrhoeae, condyloma acuminatum, and C. trachomatis since 2000.14 Thus, women in this age group may be at high risk for STIs regardless of birth cohort, and there is particular concern for mother-to-child transmission of syphilis. In fact, although rare, congenital syphilis reports—both in absolute number and in reporting rate per 100,000 live births—also increased in parallel with the increase observed in young women. Although reports are fortunately still few (potentially due to the universal screening policy for syphilis for all pregnant women in the first trimester, covered by the national health insurance scheme), such trends highlight the need for targeted STI prevention strategies for young women.
A key limitation in our assessment is related to the nature of the surveillance data, which are affected by changes in awareness levels and behaviors surrounding health seeking, testing, and/or reporting.6,15 However, we believe that the recent increase in MSW and WSM is unlikely to be entirely attributable to such surveillance bias. First, with the increase in reports, there has been a decline in the proportion of asymptomatic cases and late (symptomatic)-stage cases among both MSW and WSM (Table 1), indicating that the recent increase cannot be simply explained by increased reporting of cases that are asymptomatic or prevalent but not recently infected patients. In fact, the magnitude of the increase in reports was even greater when restricted to P&S cases—the proportionate increase from 2012 to 2016 is higher for primary (11.8-fold for MSW and 12.6-fold for WSM) and secondary cases (5.9-fold for MSW and 12.1-fold for WSM), relative to asymptomatic (3.8-fold for MSW and 8.1-fold for WSM) or late-stage cases (2.9-fold for MSW and 3.5-fold for WSM; Table 1). In terms of temporality, although information dissemination and risk communication began in 2013 and 2014, the messaging was toward MSM, and communication targeted at women and MSW began in late 2015, only after the alarming increase in reports from these groups was observed. Similarly, although some local jurisdictions have increased the accessibility to syphilis testing at local public health centers, these activities began reactively only after increase in reports was recognized, and most cases continued to be reported from obstetrics/gynecology/urology/sexually transmitted disease clinics rather than public health centers. In addition, the increase among MSW, WSM, and congenital syphilis cases is temporally correlated; if men were increasingly misreporting MSM status as MSW, it would be difficult to explain the concurrent rise in women and congenital syphilis cases. Furthermore, there have also been numerous anecdotal reports by clinicians reporting unprecedented increase in the number of female patients presenting with syphilis in recent years (T. Hamada, personal communication, Shinjuku Ladies Clinic, March 2017). Lastly, it is notable that, despite the decreasing birth rate in Japan, the number of cases among women with a written record of either “pregnant” or “found through pregnancy screening” increased, from 3 cases in 2012 to 33 cases in 2016. Although the voluntary nature of recording such information on the free-text section on the surveillance reporting form may have been biased over time with increased awareness of syphilis, given the universal screening policy for all pregnant women, such increase, at least, cannot be explained by increased testing among pregnant women. In fact, in a sample of 257 obstetrics/gynecology clinics surveyed in Japan in 2015, there were 53 pregnant women testing positive for syphilis, considerably higher than the annual ranges of 25 to 31 reported in 2011 through 2014 (based on a different case definition used in surveillance).16 In a national setting of universal syphilis screening for all pregnant women and declining birth rate, the increased reports among pregnant women seem to point toward an increase in syphilis prevalence in WSM.
Thus, taken together, although the reason(s) for the increase in syphilis remains unknown (e.g., spillover from MSM,17 changes related to sexual behavior/practices or commercial sex work, increase in imported cases from abroad), the increase in MSW and WSM seems to be real, and active awareness-raising and risk communication activities are ongoing. In-depth investigations are also underway. In spring 2016, we began an in-depth qualitative study among mothers of patients with congenital syphilis to describe their sociodemographic characteristics and health access/utilization practices to better understand the nature of congenital syphilis occurrence. As for MSW and WSM cases, given the case-only nature and the limited amount and type of data from surveillance, we cannot assess specific factors that may be associated with syphilis acquisition, such as condom use, commercial sex work (as an occupation and/or as a contact), reinfection status, HIV status, or use of mobile phone applications to seek partners. Thus, after the MSM experience,9 we have initiated a case-control study to assess potential risk factors for syphilis infection among MSW and WSM. The study, currently actively under way, will help shed light on the epidemiology of syphilis acquisition, which will be important in identifying core risk groups and behaviors to better target prevention and control measures against syphilis.
Footnotes
Acknowledgment: The authors thank notifying physicians and all the staff at local public health centers and prefectural and municipal public health institutes who contribute to surveillance activities. They also greatly appreciate Dr Takashi Hamada, Shinjuku Ladies Clinic, for the discussions and the valuable insights from the field.
This work was supported by a grant from the Ministry of Health, Labor and Welfare of Japan (H29-Shinkou-Ippan-008).
Conflicts of Interest and Source of Funding: All authors report no conflict of interest relevant to this article.
REFERENCES
- 1.Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2015. Atlanta: U.S. Department of Health and Human Services, 2016. Available at: https://www.cdc.gov/std/stats15/default.htm Accessed July 30, 2017. [Google Scholar]
- 2.Public Health England. Syphilis Epidemiology in London. London; August 17, 2016. Available at: https://www.gov.uk/government/publications/syphilis-epidemiology-in-london Accessed July 30, 2017.
- 3.Pinto-Sander N, Youssef E, Tweed M, et al. A significant increase in cases of infectious syphilis in men who have sex with men since November 2013. Int J STD AIDS 2016; 27:697–698. [DOI] [PubMed] [Google Scholar]
- 4.Jansen K, Schmidt AJ, Drewes J, et al. Increased incidence of syphilis in men who have sex with men and risk management strategies, Germany, 2015. Euro Surveill 2016; 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Champenois K, Cousien A, Ndiaye B, et al. Risk factors for syphilis infection in men who have sex with men: Results of a case-control study in Lille, France. Sex Transm Infect 2013; 89:128–132. [DOI] [PubMed] [Google Scholar]
- 6.Chow EPF, Callander D, Fairley CK, et al. Increased syphilis testing of men who have sex with men: Greater detection of asymptomatic early syphilis and relative reduction in secondary syphilis. Clin Infect Dis 2017; 13. [DOI] [PubMed] [Google Scholar]
- 7.National Institute of Infectious Diseases. Syphilis 2008–2014. Infectious Agents Surveillance Report 36: 17–19, February 2015 No2(No420). Available at: https://wwwniidgojp/niid/en/index-e/865-iasr/5413-tpc420html Accessed July 30, 2017.
- 8.Sugishita Y, Yamagishi T, Arima Y, et al. Increase in primary and secondary syphilis notifications in men in Tokyo, 2007–2013. Jpn J Infect Dis 2016; 69:154–157. [DOI] [PubMed] [Google Scholar]
- 9.Ishikane M, Arima Y, Itoda I, et al. Responding to the syphilis outbreak in Japan: Piloting a questionnaire to evaluate potential risk factors for incident syphilis infection among men who have sex with men in Tokyo, Japan, 2015. Western Pac Surveill Response J 2016; 7:36–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Institute of Infectious Diseases. Increase in syphilis notifications and characteristics of reported cases, as of October 2015. Infectious Diseases Weekly Report. November 13, 2015. Available at: https://wwwniidgojp/niid/en/survei/2292-idwr/idwr-article-en/6203-idwrc-1544-enhtml Accessed July 30, 2017.
- 11.Sunagawa T. Syphilis—Japan: Increased incidence, comment. ProMED-mail. Archive Number: 20160201.3982647. 2016-02-01 07:09:33. Available at: http://www.promedmail.org/post/3982647 Accessed July 30, 2017.
- 12.Bowen V, Su J, Torrone E, et al. Increase in incidence of congenital syphilis—United States, 2012–2014. MMWR Morb Mortal Wkly Rep 2015; 64:1241–1245. [DOI] [PubMed] [Google Scholar]
- 13.Statistics Bureau, Ministry of Internal Affairs and Communications. Portal Site of Official Statistics of Japan. Available at: https://www.e-stat.go.jp/SG1/estat/eStatTopPortal.do Accessed July 30, 2017. [In Japanese].
- 14.Ministry of Health, Labour and Welfare. March 2017. Available at: http://www.mhlw.go.jp/topics/2005/04/tp0411-1.html Accessed July 30, 2017.
- 15.Cretikos M, Mayne D, Reynolds R, et al. Testing-adjusted chlamydia notification trends in New South Wales, Australia, 2000 to 2010. Western Pac Surveill Response J 2014; 5:7–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ministry of Health, Labour and Welfare. Arakawa study group report. Available at: http://mhlw-grants.niph.go.jp/niph/search/NIDD02.do?resrchNum=201617003A Accessed September 12, 2017. [In Japanese].
- 17.Mao H, Ma W, Lu H, et al. High incidence of HIV and syphilis among migrant men who have sex with men in Beijing, China: A prospective cohort study. BMJ Open 2014; 4:e005351 Available at: http://bmjopen.bmj.com/content/4/9/e005351 Accessed July 30, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]


