Abstract
Background:
Ankylosing spondylitis (AS) is an inflammatory rheumatic disease and strongly associated with an increased risk of fractures. A great proportion of patients with AS are suffering from sustaining fractures and the aim of this study is to evaluate and quantify the association between the site of the fracture and AS by performing a meta-analysis.
Methods:
A systematic literature search was performed on Medline database from 1966 to August 15, 2016 and Embase database from 1980 to August 15, 2016. Studies were evaluated by 2 independent reviewers and quantitative estimates regarding the association between ankylosing spondylitis and the risk of any, hip, or vertebral fracture were presented. After the heterogeneity of selected studies was assessed by using Cochran I2 statistics, the random effect model was used to combine effect size. Publication bias was measured by Egger and Begg's regression tests.
Results:
A total of 6 articles were involved in our study. The results of meta-analysis revealed that AS was strongly associated with the risk of vertebral fracture (odds ratio [OR] = 4.25, 95% confidence interval [CI] = 1.07–7.42) and was not significantly associated with the risk of any fracture (OR=2.00, 95%CI = 0.94–3.06) or hip fracture (OR=1.28, 95%CI =0.16–2.40).
Conclusion:
In the present study, a general knowledge of the association between AS and the risk of 3 kinds of fractures were presented, which could improve the ways of prevention of fracture in the patients with AS.
Keywords: ankylosing spondylitis, fracture, meta-analysis, vertebrae
1. Introduction
AS is a chronic inflammatory rheumatic disease associated with an increased risk of osteoporosis and fractures, and it mainly affects axial skeleton, involvement of peripheral joints or extra-articular structures.[1] The prevalence of AS is 0.1 to 1.4% worldwide, and it is more common in Europe and Asia.[2] AS appears more commonly in male subjects, with a male/female ratio of 2:1.[3] The signs and symptoms of AS often appear gradually, with the peak age of onset between 20 and 30 years.[4] As the disease progresses, AS can also invade other body systems accompanied by several other lesion such as heart disease,[5] uveitis,[6] and chronic otitis media.[7] AS is one of the seronegative spondyloarthropathies and the heritability of AS is estimated at around 90%.[8] It is believed that the major gene association with AS is human leukocyte antigen (HLA)-B27 with approximately 95% of patients positive for the gene.[9,10]
Increased risk of fracture is strongly related to AS and it is reported that patients with AS have a fourfold fracture risk compared with general population.[11,12] Chronic inflammatory process is the main cause of loss of bone mass and bone erosions in AS. According to the recent data, even patients with early spondyloarthropathies have a low bone mineral density (BMD) and a high prevalence of vertebral fractures.[13,14] Through a chronic inflammatory process, AS can change the biomechanical properties of the vertebrae, resulting in a structural damage of bone and leading to an increased risk of vertebral fractures, even from minor injury.[11,12,15]
Fractures of the vertebral body are accepted features in patients with AS. According to the previous studies, the reported prevalence rate of vertebral fractures is ranging from 10 to 43%,[14,16–18] and the risk of vertebral fractures in the patients with AS is 2- to 8-fold increased compared with the non-AS subjects.[19–21] AS is also accepted as a great risk of hip fracture and the incidence of hip fracture in AS patients is 30 to 50%.[22–24]
Meta-analysis could provide a powerful means of summarizing the results from different studies. The present study aimed to conduct a systematic meta-analysis to evaluate the association between the site of fracture and AS by reviewing the literature. In this way, we can get a general knowledge of the overall fracture condition of AS patients and improve the ways of prevention of fracture in the patients with AS.
2. Materials and methods
This meta-analysis was conducted in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.[25] Our study did not involve any patient's intervention or information and ethical approval was not necessary.
2.1. Literature search strategy and study selection
Medline database was searched from 1966 to August 15, 2016 and Embase database was searched from 1980 to August 15, 2016 for case–control studies. All of the relevant studies were performed using medical subject headings (MeSH) or free text words. Fracture and ankylosing spondylitis were combined as search terms. Studies were included in the meta-analysis if they met the following criteria: (1) case–control design; (2) adult population; (3) the independent variables of ankylosing spondylitis; (4) the outcome of interest was any, hip, or vertebral fracture; (5) the risk estimates, such as odds ratios with 95% CIs, were reported. Those studies that did not meet the inclusion criteria were excluded during the initial review. Additionally, reference lists of relevant studies were hand searched and all of the studies that our search identified as relevant publications were reviewed. Studies were evaluated by 2 independent reviewers and quantitative estimates regarding the association between ankylosing spondylitis and the risk of any, hip, or vertebral fracture were presented. When there was uncertainty regarding any points, a third reviewer was consulted and discrepancies between their decisions regarding study inclusion and data interpretation were resolved by arbitration, and consensus was reached after discussion.
2.2. Data extraction
A standardized data collection form was used for extracting all data. The discrepancies in judgment were resolved by discussion and consulting the original articles. Data extracted from studies that met the inclusion criteria were included: the first author's last name, publication year, country, recruitment time, size of study population, participant sex and age, the number of cases, ankylosing spondylitis/fracture ascertainment, the adjustment variables, and the risk estimates with corresponding CIs for categories of consumption variables. We extracted the ORs and 95% CIs that reflected the greatest degree of control for potential confounders and used these values in our main analyses. A third reviewer served to resolve disagreement regarding the abstracted data.
2.3. Statistical analysis
ORs were used as the means of measuring association across studies. For the meta-analysis, random-effects models were used. The heterogeneity of selected studies were assessed by using Cochran I2 statistics.[26] As suggested by Higgins et al,[27]I2 values of 25% were considered as low, 50% as moderate, and 75% as high. Publication bias was measured by Egger and Begg's regression tests. Stata 11 (StataCorp, College Station, TX) was used to perform all of the analyses, and P < .05 was considered as statistically significant.
3. Results
3.1. Study characteristics
A flow diagram of the study selection was shown in Figure 1. After the initial identification of 231 articles, 205 were excluded according to the title and abstract, and the full texts of 26 were assessed for eligibility. Subsequently, 20 articles were excluded, and the reasons for which were shown in Figure 1. Finally, a total of 6 studies[19,20,28–31] were selected for the meta-analysis. Table 1 showed the information of authors, publication year, national sources, mean age, sex, study size, fracture site, disease ascertainment, and adjustments of the 6 studies.
Figure 1.
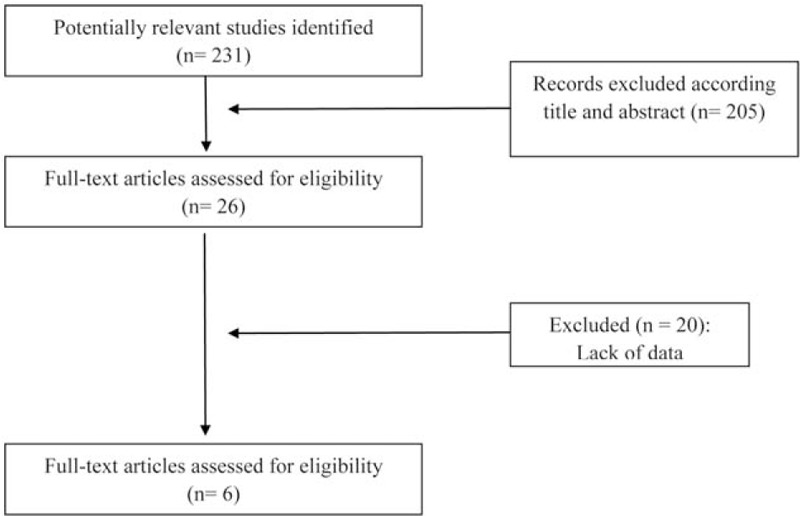
Flow diagram for studies retrieved through the searching and selecting processes.
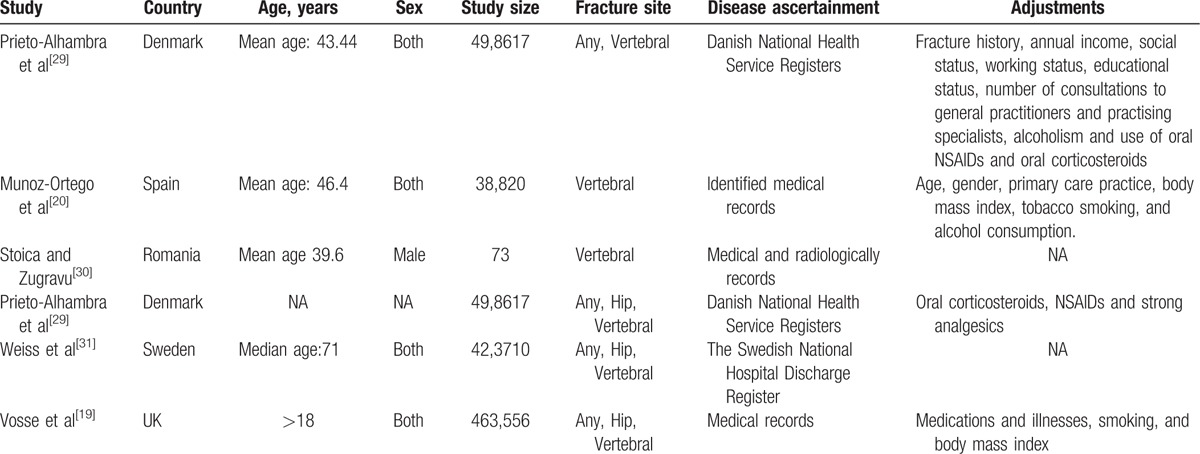
Table 1.
Characteristics of the prospective studies included in the meta-analysis.
3.2. Meta-analysis of the association between the risk of any fracture and AS
As shown in Figure 2, the 3 studies[19,29,31] were high heterogeneous (I-squared=97.8%, P=.000) and the random effects model was utilized to combine effect size. Overall, the meta-analysis identified a significant association between the risk of any fracture and AS from these 3 articles (OR=2.00, 95%, CI = 0.94–3.06). The Egger test (P < .1) and Begg's test (P < .1) exhibited publication bias in the study during the meta-analyses for the association between the risk of any fracture and AS.
Figure 2.
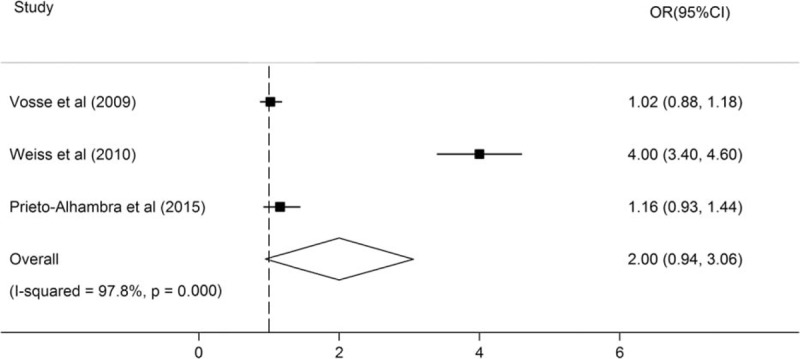
Forest plots of the risk of any fracture in patients with AS. AS = ankylosing spondylitis
3.3. Meta-analysis of the association between the risk of hip fracture and AS
As shown in Figure 3, the 3 studies[19,28,31] were high heterogeneous (I-squared=92.2%, p = .000). The meta-analysis identified a significant association between the risk of hip fracture and AS from these 3 articles (OR = 1.28, 95%, CI = 0.16–2.40). Publication bias was assessed by Egger's test (P > .1) and Begg's test (P > .1) and no publication bias was found.
Figure 3.
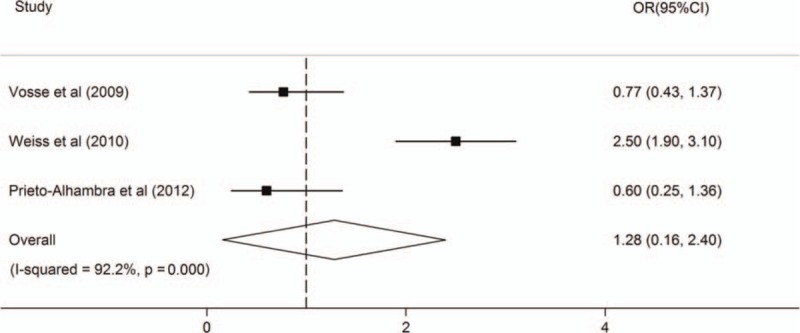
Forest plots of the risk of hip fracture in patients with AS. AS = ankylosing spondylitis.
3.4. Meta-analysis of the association between the risk of vertebral fracture and AS
As shown in Figure 4, the 5 studies[19,20,29–31] were high heterogeneous (I-squared=92.8%, P = .000) and the random effects model was utilized to combine effect size. Overall, the meta-analysis identified a significant association between the risk of vertebral fracture and AS from these 5 articles (OR = 4.25, 95%CI = 1.07–7.42). Publication bias was assessed by Egger's test (p > 0.1) and Begg's test (P > 0.1) and no publication bias was found.
Figure 4.
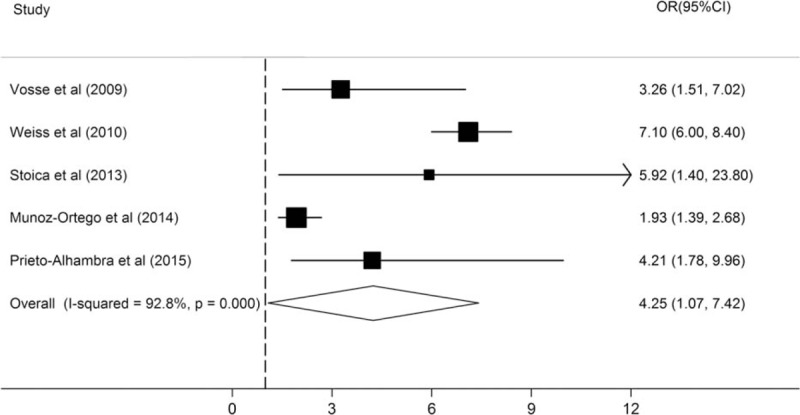
Forest plots of the risk of vertebral fracture in patients with AS. AS = ankylosing spondylitis.
4. Discussion
This meta-analysis aimed to systematically evaluate and quantify the association between AS and the risk of any, hip, or vertebral fracture. Our study reported that AS significantly increased the probability of vertebral fracture and the association between AS and the risk of any fracture or any fracture was not significant.
A great proportion of patients with AS are suffering from sustained fractures especially vertebral fractures which may cause acute pain, disability, and even mortality.[32] In a case–control study of 53,108 patients with fractures using the Swedish National Hospital Discharge Register, Weiss et al[31] concluded that the risk of fractures was much higher in AS (OR = 7.1) than in rheumatoid arthritis (RA) (OR = 2.7), with the largest increase for vertebral fracture. Although the high risk of vertebral fracture in patients with AS has been recognized, the prevalence of vertebral fractures is quite variable in different studies, up to 30%. In addition, nonvertebral fractures also occur frequently in patients with AS.[20,29] In a large-scale study based on Danish health registries, a 35% increased risk of non-vertebral fractures was found in patients with AS.[29] In a nested case–control study, Vosse et al[19] found that the adjusted risk of any clinical fracture was increased in patients with AS with a history of inflammatory bowel disease (IBD) (OR 2.79; 95% CI 1.10 to 7.08), but was decreased in patients with AS taking nonsteroidal anti-inflammatory drugs (NSAIDs) (OR 0.65; 95% CI 0.50 to 0.84), and the risk for any fracture was not associated with back pain, psoriasis, joint replacement therapy or use of sulfasalazine, indicating that the risk of any fracture in patients with AS is worth attention.
In patients with long-term AS, loss of bone mass in both hips and vertebrae owing to inflammation are well recognized[33]; in parallel, the changes of biomechanical properties, such as spinal rigidity, may reduce shock absorption and increase the fragility of bone.[29] Both of the factors increase the risk of fractures, which may have devastating consequences for patients with severe AS.[34,35] Minor trauma is the main cause of sustained clinical fractures, especially vertebral fractures,[36] for this reason, patients should be assessed for fracture risk early after AS diagnosis and education of the patients and their caregivers about how to avoid spinal trauma is important.[37,38]
Imaging of the spine plays a crucial role in the management of AS patients, allowing an early detection of vertebral fractures, which can reduce the high rate of mortality and morbidity in such patients.[15] However, the diagnosis of vertebral fractures is still challenged.[39] Vertebral fractures are often clinically overlooked or misdiagnosed as the acute back pain from their usual inflammatory pain even with the help of radiographs.[4,38,40] Delayed diagnosis may worsen prognosis, as vertebral fractures are often unstable and require proper treatment in order to avoid primary and secondary neurological injury.[15,41] It was reported that more than 50% of vertebral fractures might be clinically silent,[42] and in another study, Delmas et al[43] compared the results of local reports of radiographs with a reference center of 2000 patients and they found that vertebral fractures were misdiagnosed in 29 to 46% of them.
Meta-analysis is a systematic and quantitative analysis, which combines the data collected from several independent studies on the same problem and pools outcomes to gain an unbiased and scientific conclusion. We have tried our best to avoid bias; however, the present study still has some limitations that should be mentioned. Firstly, of the 6 available studies, the same research sample was used in 2 studies,[28,29] although the data of the risk of hip fracture was only included in the study[28] published in 2012. Secondly, OR (95% CI) of vertebral fractures in S. Stoica's study was not adjusted, unlike the other studies in which OR (95% CI) was adjusted according to several factors such as tobacco smoking and body mass index.
Thirdly, publication bias may cause a disproportionate number of positive studies and distort the meta-analysis, however, the result of Egger test and Begg's test (P < .1 in both tests) suggested the possibility of publication bias in the study during the meta-analysis for the association between AS and the risk of any fracture.
In conclusion, this meta-analysis of published data revealed that AS was associated with the risk of any, hip, or vertebral fractures and AS was most closely related to vertebral fractures.
Footnotes
Abbreviations: AS = ankylosing spondylitis, BMD = bone mineral density, CI = confidence interval, HLA = human leukocyte antigen, IBD = inflammatory bowel disease, NSAIDs = nonsteroidal anti-inflammatory drugs, OR = odds ratio, RA = rheumatoid arthritis.
This work was partly supported by the National Natural Science Foundation of China (Nos. 81202349, 81373186 and 81671601), Anhui Provincial Natural Science Foundation of Institution of Higher Education (No. KJ2012Z154) and the School Research Fund of Anhui Medical University (No. 2011xkj066).
The authors have no conflicts of interest to disclose.
References
- [1].Davey-Ranasinghe N, Deodhar A. Osteoporosis and vertebral fractures in ankylosing spondylitis. Curr Opin Rheumatol 2013;25:509–16. [DOI] [PubMed] [Google Scholar]
- [2].Stolwijk C, Essers I, van Tubergen A, et al. The epidemiology of extra-articular manifestations in ankylosing spondylitis: a population-based matched cohort study. Ann Rheum Dis 2015;74:1373–8. [DOI] [PubMed] [Google Scholar]
- [3].Fan D, Liu L, Ding N, et al. Male sexual dysfunction and ankylosing spondylitis: a systematic review and metaanalysis. J Rheumatol 2015;42:252–7. [DOI] [PubMed] [Google Scholar]
- [4].Sambrook PN, Geusens P. The epidemiology of osteoporosis and fractures in ankylosing spondylitis. Ther Adv Musculoskelet Dis 2012;4:287–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Essers I, Stolwijk C, Boonen A, et al. Ankylosing spondylitis and risk of ischaemic heart disease: a population-based cohort study. Ann Rheum Dis 2016;75:203–9. [DOI] [PubMed] [Google Scholar]
- [6].Sun L, Wu R, Xue Q, et al. Risk factors of uveitis in ankylosing spondylitis: an observational study. Medicine 2016;95:e4233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Camilleri AE, Swan IR, Murphy E, et al. Chronic otitis media: a new extra-articular manifestation in ankylosing spondylitis? Ann Rheum Dis 1992;51:655–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Brown MA, Kennedy LG, MacGregor AJ, et al. Susceptibility to ankylosing spondylitis in twins: the role of genes, HLA, and the environment. Arthritis Rheum 1997;40:1823–8. [DOI] [PubMed] [Google Scholar]
- [9].Brophy S, Hickey S, Menon A, et al. Concordance of disease severity among family members with ankylosing spondylitis? J Rheumatol 2004;31:1775–8. [PubMed] [Google Scholar]
- [10].Hamersma J, Cardon LR, Bradbury L, et al. Is disease severity in ankylosing spondylitis genetically determined? Arthritis Rheum 2001;44:1396–400. [DOI] [PubMed] [Google Scholar]
- [11].Westerveld LA, Verlaan JJ, Oner FC. Spinal fractures in patients with ankylosing spinal disorders: a systematic review of the literature on treatment, neurological status and complications. Eur Spine J 2009;18:145–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Finkelstein JA, Chapman JR, Mirza S. Occult vertebral fractures in ankylosing spondylitis. Spinal Cord 1999;37:444–7. [DOI] [PubMed] [Google Scholar]
- [13].van der Weijden MA, Claushuis TA, Nazari T, et al. High prevalence of low bone mineral density in patients within 10 years of onset of ankylosing spondylitis: a systematic review. Clin Rheumatol 2012;31:1529–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].van der Weijden MA, van der Horst-Bruinsma IE, van Denderen JC, et al. High frequency of vertebral fractures in early spondylarthropathies. Osteoporos Int 2012;23:1683–90. [DOI] [PubMed] [Google Scholar]
- [15].Jacobs WB, Fehlings MG. Ankylosing spondylitis and spinal cord injury: origin, incidence, management, and avoidance. Neurosurg Focus 2008;24:E12. [DOI] [PubMed] [Google Scholar]
- [16].Jun JB, Joo KB, Her MY, et al. Femoral bone mineral density is associated with vertebral fractures in patients with ankylosing spondylitis: a cross-sectional study. J Rheumatol 2006;33:1637–41. [PubMed] [Google Scholar]
- [17].Vosse D, van der Heijde D, Landewe R, et al. Determinants of hyperkyphosis in patients with ankylosing spondylitis. Ann Rheum Dis 2006;65:770–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Ghozlani I, Ghazi M, Nouijai A, et al. Prevalence and risk factors of osteoporosis and vertebral fractures in patients with ankylosing spondylitis. Bone 2009;44:772–6. [DOI] [PubMed] [Google Scholar]
- [19].Vosse D, Landewe R, van der Heijde D, et al. Ankylosing spondylitis and the risk of fracture: results from a large primary care-based nested case-control study. Ann Rheum Dis 2009;68:1839–42. [DOI] [PubMed] [Google Scholar]
- [20].Munoz-Ortego J, Vestergaard P, Rubio JB, et al. Ankylosing spondylitis is associated with an increased risk of vertebral and nonvertebral clinical fractures: a population-based cohort study. J Bone Miner Res 2014;29:1770–6. [DOI] [PubMed] [Google Scholar]
- [21].Cooper C, Carbone L, Michet CJ, et al. Fracture risk in patients with ankylosing spondylitis: a population based study. J Rheumatol 1994;21:1877–82. [PubMed] [Google Scholar]
- [22].Guan M, Wang J, Zhao L, et al. Management of hip involvement in ankylosing spondylitis. Clin Rheumatol 2013;32:1115–20. [DOI] [PubMed] [Google Scholar]
- [23].Ulucay C, Ozler T, Guven M, et al. Etiology of coxarthrosis in patients with total hip replacement. Acta Orthop Traumatol Turc 2013;47:330–3. [DOI] [PubMed] [Google Scholar]
- [24].Cooksey R, Brophy S, Husain MJ, et al. The information needs of people living with ankylosing spondylitis: a questionnaire survey. BMC Musculoskelet Disord 2012;13:243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 2009;6:e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002;21:1539–58. [DOI] [PubMed] [Google Scholar]
- [27].Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003;327:557–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Prietoalhambra D, Munozortego J, Cooper C, et al. Ankylosing spondylitis is strongly related to clinical spine fractures independently of drugs use: a register-based case-control study. Arthritis Rheum-US 2012;10:S936. [Google Scholar]
- [29].Prieto-Alhambra D, Munoz-Ortego J, De Vries F, et al. Ankylosing spondylitis confers substantially increased risk of clinical spine fractures: a nationwide case-control study. Osteoporos Int 2015;26:85–91. [DOI] [PubMed] [Google Scholar]
- [30].Stoica S, Zugravu G. AB0907 The prevalence of vertebral fractures and their relationship with bone mineral density in mild ankylosing spondylitis men pacients. Ann Rheum Dis 2014;71(suppl 3):690–1690. [Google Scholar]
- [31].Weiss RJ, Wick MC, Ackermann PW, et al. Increased fracture risk in patients with rheumatic disorders and other inflammatory diseases—a case-control study with 53,108 patients with fracture. J Rheumatol 2010;37:2247–50. [DOI] [PubMed] [Google Scholar]
- [32].Leone A, Marino M, Dell’Atti C, et al. Spinal fractures in patients with ankylosing spondylitis. Rheumatol Int 2016;36:1335–46. [DOI] [PubMed] [Google Scholar]
- [33].Will R, Palmer R, Bhalla AK, et al. Osteoporosis in early ankylosing spondylitis: a primary pathological event? Lancet 1989;2:1483–5. [DOI] [PubMed] [Google Scholar]
- [34].Graham B, Van Peteghem PK. Fractures of the spine in ankylosing spondylitis. Diagnosis, treatment, and complications. Spine 1989;14:803–7. [DOI] [PubMed] [Google Scholar]
- [35].Fox MW, Onofrio BM, Kilgore JE. Neurological complications of ankylosing spondylitis. J Neurosurg 1993;78:871–8. [DOI] [PubMed] [Google Scholar]
- [36].Vosse D, Feldtkeller E, Erlendsson J, et al. Clinical vertebral fractures in patients with ankylosing spondylitis. J Rheumatol 2004;31:1981–5. [PubMed] [Google Scholar]
- [37].Masiero S, Bonaldo L, Pigatto M, et al. Rehabilitation treatment in patients with ankylosing spondylitis stabilized with tumor necrosis factor inhibitor therapy: a randomized controlled trial. J Rheumatol 2011;38:1335–42. [DOI] [PubMed] [Google Scholar]
- [38].Waldman SK, Brown C, Lopez de Heredia L, et al. Diagnosing and managing spinal injury in patients with ankylosing spondylitis. J Emerg Med 2013;44:e315–9. [DOI] [PubMed] [Google Scholar]
- [39].Lems WF. Clinical relevance of vertebral fractures. Ann Rheum Dis 2007;66:2–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Geusens P, Vosse D, van der Linden S. Osteoporosis and vertebral fractures in ankylosing spondylitis. Curr Opin Rheumatol 2007;19:335–9. [DOI] [PubMed] [Google Scholar]
- [41].Westerveld LA, van Bemmel JC, Dhert WJ, et al. Clinical outcome after traumatic spinal fractures in patients with ankylosing spinal disorders compared with control patients. Spine J 2014;14:729–40. [DOI] [PubMed] [Google Scholar]
- [42].Pongchaiyakul C, Nguyen ND, Jones G, et al. Asymptomatic vertebral deformity as a major risk factor for subsequent fractures and mortality: a long-term prospective study. J Bone Miner Res 2005;20:1349–55. [DOI] [PubMed] [Google Scholar]
- [43].Delmas PD, van de Langerijt L, Watts NB, et al. Underdiagnosis of vertebral fractures is a worldwide problem: the IMPACT study. J Bone Miner Res 2005;20:557–63. [DOI] [PubMed] [Google Scholar]


