Abstract
Objective:
To evaluate the effectiveness of nudge activities at school on the students’ body mass index (BMI).
Design:
School-based factorial randomized community trial.
Setting:
Eighteen public schools in the municipality of Duque de Caxias, metropolitan area of Rio de Janeiro, Brazil.
Participants and intervention:
The 18 schools will be randomized into 4 group arms: group 1—control (without any activity); group 2—will receive educational activities in the classroom; group 3—will receive changes in the school environment (nudge strategies); group 4—will receive educational activities and changes in the school environment. Activities will occur during the 2018 school-year.
Main outcome measure(s):
The primary (BMI) and secondary (body fat percentage) outcomes will be assessed at baseline and after the study using a portable electronic scale with a segmental body composition monitor. The height will be measured by a portable stadiometer.
Analysis:
Statistical analyses for each outcome will be conducted through linear mixed models that took into account the missing data and cluster effect of the schools.
Keywords: adolescent, choice behavior, food consumption, obesity, prevention
1. Introduction
In Brazil, 1 in 5 adolescents are overweight or obese.[1] Environmental factors have great influence on the genesis of the obesity epidemic, due mainly to the consumption of energy-dense foods, low levels of physical activity, and sedentary lifestyle. Thus, these 2 components—diet and energy expenditure—are the cornerstones of prevention and treatment programs of obesity.[2,3]
Interventions in schools to prevent obesity have been established as an important strategy to address the problem, but previous research has shown that interventions towards healthy behaviors have had humble results.[4] Observed effects imply high levels of knowledge, awareness, and positive attitude towards healthy eating,[5] yet underscoring the problem that information and positive attitudes are not enough to produce actual change.
In this context, some interventions have used nudge strategy to alter people's behavior in a predictable way to make healthy behavior more likely.[6,7] Nudging is an aspect of the choice architecture (the way of presentation and framing of choices) that alters the individuals’ choice in a predictable and desirable way, without forbidding any options or significantly changing their economic incentives,[8,9] assuming that individual behavior is strongly influenced by the environment in which decisions are taken.[10]
Some studies conducted in developed countries have reported success in nudge interventions. Williamson et al[11] observed positive results in food consumption after several changes in the school cafeteria environment. Wansink et al[12] found a positive effect in making vegetables more attractive, by giving them nicknames, increasing their consumption in American school cafeterias. However, some studies did not find significant association between the use of nudge and healthier eating by the adolescents investigated. Bucher et al[13] observed that point-of-purchase messages had no effect on vegetable basket sales in a college foodservice setting. Coyle et al[14] showed that the presence of a salad bar was not associated with greater fruit and vegetable consumption in elementary schools.
Systematic reviews showed that the choice architecture seems effective to promote healthier food choices,[13,15] and the most effective strategy was to increase food availability.[16] However, the authors concluded that there is an important literature gap,[7] and few high-quality studies evaluated nudge strategy in real-life scenarios[13,15] and quantified the impact of these strategies on health outcomes, mainly obesity.[13,17,18]
Adolescents are highly susceptible to environmental influences, suggesting that nudging is an interesting tool in the prevention of obesity and school a strategy place to promote nudging.[7]
This project is a factorial trial which continues previous research called PAAPPAS study (Portuguese abbreviation of “parents, students, community health agents and teachers for healthy eating”).[19] The present project will be conducted in schoolchildren, keeping the already consolidated components of primary prevention and including actions that aim to improve the adherence response to the interventions and providing a broad spectrum of actions to reach adolescence-based obesity prevention, including changes in School environment. More specifically, the present research aims to estimate the effect of “nudge” strategies on the students’ body mass index (BMI), from changes at the school environment, with the aim of creating school cafeterias that guide smarter food choices.
2. Methods
2.1. Study design and setting
PAAPPAS Nudge is a randomized community-based, school-based trial designed to promote healthful choices in a low-income scenario, which will be held in 2018 school-year in 18 municipal public schools in the municipality of Duque de Caxias, metropolitan area of Rio de Janeiro, Brazil (http://duquedecaxias.rj.gov.br/portal/). All students from the fifth and sixth grade from the 18 selected schools will be invited to participate to the study.
The study design will be of the factorial type, with 4 group arms:
-
1)
Group 1: control (without any activity)
-
2)
Group 2: will receive educational activities in the classroom
-
3)
Group 3: will receive changes in the school environment (nudge strategies)
-
4)
Group 4: will receive educational activities and changes in the school environment
In the factorial study, it is possible to verify both the main effect of each factor and an interaction of factors in the outcome variable.[20]
Schools will be sequentially numbered and randomized using opaque envelopes in the presence of investigators not involved in the current study. The statistical analysis will be conducted by investigators blinded to intervention allocation.
Participants in the Nudge control will receive individual encouragement.
The Municipality of Duque de Caxias is a poor area with a prevalence of overweight/obesity among adolescents of 24%.[21]
The study adhere to the Consolidated Standards of Reporting Trials (CONSORT) guidelines for cluster-randomized trials.[22] Ethics approval for this study was obtained from Ethics Committee, and all the participants’ parents provided informed written consent.
2.2. Sample size calculation
Sample size of PAAPPAS Nudge was calculated based on a minimum effect of 0.15 in BMI variation and considering intra and intergroup comparisons. A sample size of 640 adolescents was required based on 95% power and a correlation between repeated measures of 0.5. Considering the intracluster correlation and refusal rate, the total sample size required was increased, leading 1300 adolescents, which can be achieved achieved with 10 schools with 4 to 5 classes of 30 students each one.
In addition, a subsample of 96 adolescents (48 boys and 48 girls) was calculated to detect a mean difference in daily energy expenditure of 110 kcal and a coefficient of variation equal to 1 (standard deviation [SD] of 110 kcal),[23] with an α of 0.05 (2-sided) and β of 0.10.[24] The adolescents were sampled from 1 intervention (n = 48) and 1 control school (n = 48).
2.3. Intervention
The activities will occur during the 2018 school-year and will combine different intervention strategies: educational interventions (in the classroom) and modifications in the environment (school canteens and sports court).
Group 2 will receive classroom-based educational activities based on an earlier study, which was developed in the same city and constituted a school-based intervention with the objective of reducing the consumption of sweetened beverages and biscuits, and increase the consumption of fruits, vegetables, and beans.[25]
In group 3, changes in the environment will be included that will facilitate both physical activity and healthy food choices. Interventions will be based on a nudge strategy, a tool of the architectural field of choice, which is defined as a way of influencing choices without limiting personal decisions or having to implement actions or interventions of greater cost and operational difficulty.[26] The concept of nudging is based on the theory of the double process originated in the field of psychology, which involves the division of human cognition into 2 systems: the reflective and the automatic. The first is rational and involves conscious decisions, whereas the latter is more controlled by instinct.[27,28] These 2 systems are taken into account for a number of cognitive biases, which explains, for example, why people, though conscious, have difficulty in translating intentions into actions. Using the understanding of these 2 biases is possible to changing behavior developing new ways of how food choices are presented in an environment, and individuals are unconsciously “motivated” to adopt healthy choices.
The approaches can be divided into passive and active. The passive approach, also called choice architecture, seeks to induce healthy choices through small changes in the environment. The active approach includes placing reminders in the environment. In the school context, the intention is to change the environment in which schoolchildren are inserted with the perspective of associating convenience with healthier practices and making less healthy practices less convenient, aiming to increase the consumption of healthier foods and stimulate the practice of physical activity. The convenience of healthy practices both preserves the power of choice (students are not required to consume healthy food or engage in physical activity) and encourages healthy behavior.[17]
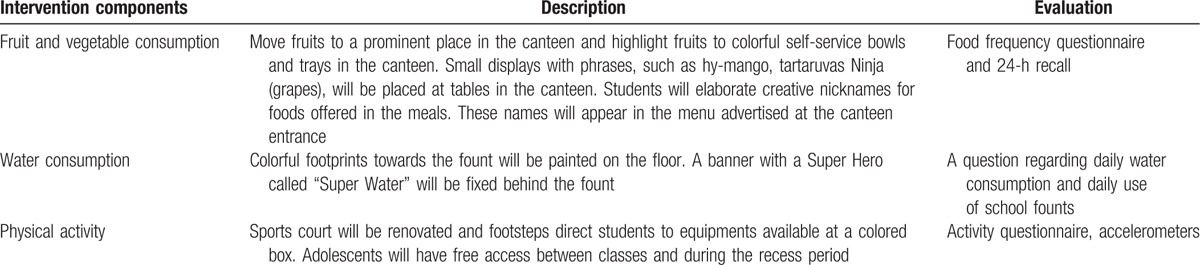
Table 1 describes the intervention components and evaluation tools conducted in PAAPPAS Nudge.
Table 1.
Intervention components, description, and evaluation.
Interventions regarding food consumption were based on those strategies of the Smarter Lunchrooms Movement (SLM)—an intervention study conducted in US school lunchrooms to led students to eat more fruits and vegetables, with positive results.[29] In the present study, school lunchrooms will be the central place of modifications regarding food consumption, where the strategies that were effective in SLM will be reproduced:
-
1)
Arrange the fruits served in the school lunch in a prominent position, in containers of bright and contrasting colors, to serve them. In this approach the student himself is served, which will probably result in his ingestion.
-
2)
Creative names for food served at meals will be created by the students used on displays at canteen tables, posters on the way of the cafeteria, and at a menu outside the cafeteria. Increasing students’ expectancy increases their likelihood of choosing and eating new dishes. Students will be encouraged to participate actively in this stage. They will receive a list of the most commonly served vegetables at the lunch and will be asked to create fun-filled names for each of them, such as “carrots x-ray vision” and “super strength spinach.”
Moreover, to encourage water consumption, footprints that lead them to water fountains will be painted on the floor. To stimulate physical activity, several sports equipment (basketball hoops, volleyball nets, balls, ropes, shuttlecock, and a lot of toys) will be available for use in the school sports court. The courts will be renovated and footsteps will be painted to nudging students to the sports equipment.
Group 4 received both interventions.
The measurable intervention outcomes are fruits, vegetables, and water consumption (quantities in g or mL) obtained from the 24-hour recall, and estimated physical activity and daily energy expenditure.
2.4. Data collection
2.4.1. Physical activity
Physical activity levels will be measured through a validated questionnaire including 6 questions about frequency and time of different physical activities domains (commuting to school, physical education classes, and other physical activities/sports) performed during the previous 7 days. Adolescents will be classified as active (≥300 minutes), insufficiently active (150–299 and 1–149 minutes), and inactive (no physical activity) according to their accumulated physical activity level.[30] In addition, total energy expenditure will be measured using triaxial accelerometers (Actigraph, GT3X)[31] in a subsample of 96 adolescents (48 boys and 48 girls). The accelerometers will be placed on the right hip (anterior iliac crest) during a 6-day period, except while bathing or during water activities.
2.4.2. Food consumption
Food intake will be assessed by a food frequency questionnaire validated for teenagers in Rio de Janeiro[32] and one 24-hour recall (Rec24-h). Netbooks containing a computer program developed for school use[27,33] based on a technique called “Multiple Pass Method”[34] will be used.
2.5. Expected outcomes
2.5.1. Primary and secondary outcomes
The primary outcome of the study will be the variation of BMI and secondary outcome will be the variation of body fat percentage.
The body weight and body fat percentage will be measured by a portable electronic scale with a segmental body composition monitor (Tanita BC-558). The height will be measured by a portable stadiometer (brand: “AlturaExata”). The waist circumference will be measured with an inextensible measure tape, with amplitude of 150 cm and variation of 0.1 mm. All the measures will be taken according the protocol designed by Gordon et al.[35] Each adolescent will be evaluated 3 times: baseline—at the begging of the school-year, the second—at the middle of the school-year; and the third—at the end of the school-year. To avoid follow-up losses, schools will be visited three times in each measurement time.
2.6. Statistical analysis
Statistical analyses for each outcome are conducted through linear mixed models that took into account the missing data and cluster effect of the schools. The models will be used to assess the impact of treatment (nudge or control school), time (treated as continuous, in months), and the treatment-by-time interaction. In this analysis, the distribution of probabilities more suitable for the variable of interest will be verified, and also the correlation structure between repeated measurements. Data analysis will be performed using the Statistical Analysis System, version 9.4 (SAS Institute Inc, Cary, NC).
2.7. Ethics and dissemination
The protocol was approved by the Ethics Committee of the Institute of Social Medicine (Comitê de ética do Instituto de Medicina Social—CAAE: 10471313.2.0000.5260). Written informed consent will be sent to all participants’ parents, by their children. All the researchers had access to the final trial dataset. The final dataset of the trial will be available for the researchers without names or any identification of the participants. The results of the study will be published in scientific journal and will be also sent to participants’ schools.
3. Discussion
Nudge strategies have been tested in developed countries with successful results in changing obesity-related behaviors.[11,12,36] We are testing a combination of these strategies to improve adolescents’ eating and activity behaviors in schools of a low-income scenario.
In Brazil, the National School Food Program stipulates that all public schools should offer no cost daily meals for students, including fruits and vegetables on menus.[37] However, data from a previous research carried out in the same locality of the present study[25] indicate that a percentage of more than 30% of students do not consume the food offered at school.
Proving these low-cost nudge strategies as an effective step in changing obesity-related behaviors is an important and feasible tool to improve the consumption of school meals, in public schools in Brazil. Moreover, the inclusion of these strategies on a well-established school-based randomized trial will fill the gap in the literature to evaluate the nudge strategy in high-quality studies using real scenarios. The main study is now in progress, and the primary interventions started in July.
To the best of our knowledge, there are no studies on school nudge in Brazil. Moreover, nudge strategies to increase physical activity among children and adolescents have not been studied. The randomized controlled trial of the PAAPPAS Nudge intervention described in this protocol paper will provide data on the effects of choice architecture intervention approaches for increasing fruit and vegetable, and water consumption at the school environment among students in low-income countries, and also it is innovative in investigating the behavioral effects of environmental changes to encourage physical activity in a school setting.
4. Conclusions
The results of this study, if shown to be effective, will confirm the importance of incorporating environmental changes into traditional nutrition education interventions to facilitate healthier choices. Thus, the research will provide new tools to contribute to reduction of growing prevalence of obesity and poor nutrition in adolescents.
Footnotes
Abbreviations: BMI = body mass index, CONSORT = Consolidated Standards of Reporting Trials, PAAPPAS = Portuguese abbreviation of parents, students, community health agents and teachers for healthy eating, Rec24-h = 24-hour recall, SLM = Smarter Lunchrooms Movement.
Funding: This work was supported by Foundation of Support of Research of the State of Rio de Janeiro (FAPERJ), E-26/010.001656/2016.
The authors report no conflicts of interest.
References
- [1].IBGE. National Household Budget Survey 2008–2009: Anthropometry and Nutritional Status of Children, Teenagers and Adults in Brazil. Rio de Janeiro; 2011. [Google Scholar]
- [2].Monasta L, Batty GD, Cattaneo A, et al. Early-life determinants of overweight and obesity: a review of systematic reviews. Obes Rev 2010;11:695–708. [DOI] [PubMed] [Google Scholar]
- [3].Mikkelsen BE, Ohri-Vachaspati P. Hunger, overconsumption and youth: future directions for research in school-based public health nutrition strategies. Public Health Nutr 2013;16:953–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Khambalia AZ, Dickinson S, Hardy LL, et al. A synthesis of existing systematic reviews and meta-analyses of school-based behavioural interventions for controlling and preventing obesity. Obes Rev 2012;13:214–33. [DOI] [PubMed] [Google Scholar]
- [5].Pérez-Cueto FJ, Aschemann-Witzel J, Shankar B, et al. Assessment of evaluations made to healthy eating policies in Europe: a review within the EATWELL Project. Public Health Nutr 2012;15:1489–96. [DOI] [PubMed] [Google Scholar]
- [6].Kremers SPJ, Eves FF, Andersen RE. Environmental changes to promote physical activity and healthy dietary behavior. J Environ Public Health 2012;2012:1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Nornberg TR, Houlby L, Skov LR, et al. Choice architecture interventions for increased vegetable intake and behaviour change in a school setting: a systematic review. Perspect Public Health 2016;136:132–42. [DOI] [PubMed] [Google Scholar]
- [8].Thaler RH, Sunstein CR. Nudge: Improving Decisions about Health Wealth, and Happiness. New York: Penguin Books; 2008. [Google Scholar]
- [9].Marteau TM, Ogilvie D, Roland M, et al. Judging nudging: can nudging improve population health? BMJ 2011;342:d228. [DOI] [PubMed] [Google Scholar]
- [10].de Wijk RA, Maaskant AJ, Polet IA, et al. An in-store experiment on the effect of accessibility on sales of wholegrain and white bread in supermarkets. PLoS One 2016;11:e0151915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Williamson DA, Han H, Johnson WD, et al. Modification of the school cafeteria environment can impact childhood nutrition. Results from the Wise Mind and LA Health studies. Appetite 2013;61:77–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Wansink B, Just DR, Payne CR, et al. Attractive names sustain increased vegetable intake in schools. Prev Med 2012;55:330–2. [DOI] [PubMed] [Google Scholar]
- [13].Bucher T, Collins C, Rollo ME, et al. Nudging consumers towards healthier choices: a systematic review of positional influences on food choice. Br J Nutr 2016;115:2252–63. [DOI] [PubMed] [Google Scholar]
- [14].Coyle KK, Potter S, Schneider D, et al. Distributing free fresh fruit and vegetables at school: results of a pilot outcome evaluation. Public Health Rep 2009;124:660–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Skov LR, Lourenço S, Hansen GL, et al. Choice architecture as a means to change eating behaviour in self-service settings: a systematic review. Obes Rev 2013;14:187–96. [DOI] [PubMed] [Google Scholar]
- [16].Hu, Q. (2014). Application of nudge theory for changing diet and physical activity : a systematic review. (Thesis). University of Hong Kong, Pokfulam, Hong Kong SAR. Retrieved from http://dx.doi.org/10.5353/th_b5320341. [Google Scholar]
- [17].Oliver A. Is nudge an effective public health strategy to tackle obesity? Yes. BMJ 2011;13:d2168. [DOI] [PubMed] [Google Scholar]
- [18].Oliver A, Ubel P. Nudging the obese: a UK-US consideration. Heal Econ Policy Law 2014;9:329–42. [DOI] [PubMed] [Google Scholar]
- [19].Sgambato MR, Cunha DB, Henriques VT, et al. PAAPPAS community trial protocol: a randomized study of obesity prevention for adolescents combining school with household intervention. BMC Public Health 2016;16:809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Montgomery DG. Design and Analysis of Experiments. New York: Wiley & Sons; 1996. [Google Scholar]
- [21].Lopes T, Rosely S, Salles-Costa R, et al. Family food insecurity and nutritional risk in adolescents from a low-income area of Rio de Janeiro, Brasil. J Biosoc Sci 2013;45:661–74. [DOI] [PubMed] [Google Scholar]
- [22].Campbell MK, Piaggio G, Elbourne DR, et al. Consort 2010 statement: extension to cluster randomised trials. BMJ 2012;345:e5661. [DOI] [PubMed] [Google Scholar]
- [23].Belle G van. Statistical Rules of Thumb. 2nd edNew York: Wiley-Interscience; 2008. [Google Scholar]
- [24].Julious SA. Sample Sizes for Clinical Trials. New York: Chapman and Hall/CRC; 2010. [Google Scholar]
- [25].Cunha DB, Souza B da SN de, Pereira RA, et al. Effectiveness of a randomized school-based intervention involving families and teachers to prevent excessive weight gain among adolescents in Brazil. PLoS One 2013;8:e57498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Hausman DM, Welch B. Debate: to nudge or not to nudge. J Polit Philos 2010;18:123–36. [Google Scholar]
- [27].Kahneman D. Thinking, Fast and Slow. New York: Farrar Straus Giroux; 2011. [Google Scholar]
- [28].Stanovich KE, West RF. Individual differences in reasoning: implications for the rationality debate? Behav Brain Sci 2000;23: 645-65-726. [DOI] [PubMed] [Google Scholar]
- [29].Hanks AS, Just DR, Smith LE, et al. Healthy convenience: nudging students toward healthier choices in the lunchroom. J Public Health (Oxf) 2012;34:370–6. [DOI] [PubMed] [Google Scholar]
- [30].Tavares LF, Castro IRR de, Cardoso LO, et al. Validade de indicadores de atividade física e comportamento sedentário da Pesquisa Nacional de Saúde do Escolar entre adolescentes do Rio de Janeiro, Brasil. Cad Saude Publica 2014;30:1861–74. [DOI] [PubMed] [Google Scholar]
- [31].Pedisic Z, Bauman A. Accelerometer-based measures in physical activity surveillance: current practices and issues. Br J Sports Med 2015;49:219–23. [DOI] [PubMed] [Google Scholar]
- [32].Araujo MC, Yokoo EM, Pereira RA. Validation and calibration of a semiquantitative food frequency questionnaire designed for adolescents. J Am Diet Assoc 2010;110:1170–7. [DOI] [PubMed] [Google Scholar]
- [33].Barufaldi LA, Abreu G de A, Veiga GV da, et al. Programa para registro de recordatório alimentar de 24 horas: aplicação no Estudo de Riscos Cardiovasculares em Adolescentes. Rev Bras Epidemiol 2016;19:464–8. [DOI] [PubMed] [Google Scholar]
- [34].Moshfegh AJ, Rhodes DG, Baer DJ, et al. The US Department of Agriculture automated multiple-pass method reduces bias in the collection of energy intakes. Am J Clin Nutr 2008;88:324–32. [DOI] [PubMed] [Google Scholar]
- [35].Gordon CC, Chumlea WC, Roche AF. Lohman TG, Roche AF, Martorell R. Stature, recumbent length, and weight. Human Kinetics Books, Antropometric Standardization Reference Manual. Illinois:1988. [Google Scholar]
- [36].Wansink B, Just DR, Hanks AS, et al. Pre-sliced fruit in school cafeterias. Am J Prev Med 2013;44:477–80. [DOI] [PubMed] [Google Scholar]
- [37].Nogueira RM, Barone B, Barros TT de, et al. Sixty years of the National Food Program in Brazil. Rev Nutr 2016;29:253–67. [Google Scholar]


