Abstract
Antihypertensive treatment has beneficial effects in the elderly. Surveying the situation of blood pressure in the elderly is quite important for planning strategies to manage elderly hypertensives. The aim of the present study was to investigate changes in blood pressure in the elderly over the past 15 years.
As part of a physical check-up program between 2001 and 2015, 29,363 elderly participants (≥65 years of age) attended and were enrolled in the present study. The characteristics of the participants in each year were analyzed cross-sectionally and the results were compared over the 15 years. Changes in blood pressure, hypertension prevalence, and treatment rates, and the rate of reaching target blood pressure in the elderly were investigated.
The prevalence of hypertension during the study period increased with increasing participant age. However, both the treatment rate and the rate of reaching target blood pressure in treated subjects improved. The blood pressure of treated hypertensive elderly subjects decreased from 146.1/83.0 to 130.6/75.4 mm Hg, and the reduction was most evident after revision of Japanese Society of Hypertension guidelines regarding target blood pressure in elderly hypertensives. Blood pressure in the entire cohort of elderly subjects decreased from 133.8/78.4 mm Hg in 2001 to 127.9/74.6 mm Hg in 2015.
Blood pressure in elderly subjects had decreased over the 15-year study period primarily due to reductions in blood pressure in elderly hypertensive patients on medication. Guidelines for the treatment of hypertension have had a beneficial effect on the management of hypertension in the elderly.
Keywords: alternation, blood pressure, elderly, hypertension, prevalence
1. Introduction
A chronic increase in blood pressure is one of the most important risk factors for cardiovascular disease, which is the leading cause of morbidity and mortality in developed countries.[1–3] Accumulating evidence strongly suggests that reducing blood pressure in individuals with hypertension reduces cardiovascular morbidity and mortality.[4–6] However, only a limited number of large-scale clinical trials have investigated the effects of antihypertensive treatment in elderly hypertensive patients, despite the increase in the elderly population worldwide. A few trials targeting hypertensive individuals aged ≥60 years have demonstrated that antihypertensive treatment in elderly subjects with mean systolic blood pressure (SBP) of 168 to 197 mm Hg resulted in a 17% to 60% reduction in cardiovascular events with a reduction in SBP of 9 to 21 mm Hg.[7–15] The mean age of the subjects included in those trials was around 70 years, and only the HYpertension in the Very Elderly Trial (HYVET)[15] demonstrated beneficial effects of antihypertensive medication in patients aged ≥80 years. Although available evidence is limited, the beneficial effects of antihypertensive treatment in the elderly are generally accepted.[16–19] In line with this background, most guidelines for the management of hypertension recommended antihypertensive treatment in elderly hypertensives aged ≥65 years, with particular attention to multiple diseases, atypical presentations, and marked individual differences in the elderly, although blood pressure levels to be treated and target blood pressure levels differ among guidelines.[3,18,20,21] These guidelines may have an effect on the physicians providing primary care and may have improved the knowledge of hypertension in the general population,[22] leading to improvements in the elderly population from the viewpoint of blood pressure.
The prevalence of hypertension in the elderly is quite high because of the gradual increase in blood pressure with age,[23,24] and the appropriate management of these patients should be emphasized to prevent cardiovascular diseases and to extend healthy life expectancy.[3,17–21] Thus, the aim of the present study was to investigate changes in blood pressure levels, hypertension prevalence, and treatment rates, and the rate at which target blood pressure is reached in elderly subjects over the past 15 years. This survey may provide important information for further improvements in blood pressure status in the elderly.
2. Methods
2.1. Study design
The present study was a survey of participants who visited Enshu hospital for their yearly physical check-up between 2001 and 2015. A cross-sectional analysis was performed in each year during the study period and the results were compared to assess changes in blood pressure levels, hypertension prevalence, and treatment rates, and the rate at which target blood pressure was reached. The study was performed in accordance with the principles of the Declaration of Helsinki, and the study protocol was approved by the Ethics Committee of Enshu Hospital. All patients provided written informed consent to participate before the start of the study and at each study visit.
2.2. Study subjects and procedures
Participants aged ≥20 years were eligible for inclusion in the present study. Between 2001 and 2015, 109,134 subjects [mean (± standard deviation) age 56.5 ± 11.7 years; 71,007 (65.1%) men] visited Enshu hospital for a physical check-up. The present study is not a follow-up study of a cohort, and the data in each year represent the results obtained for the participants attending for the physical examination in that year. Of the 109,134 subjects, 29,363 were elderly [≥65 years of age; 20,070 (68.4%) men] in any visit across all 15 years. The elderly subjects were divided into 2 groups: young-old (65–74 years of age; n = 23,825) and old-old (≥75 years of age; n = 5538).
The physical check-up program included a routine physical examination, chest X-ray, electrocardiogram, and laboratory assessment of cardiovascular risk factors. Participants were instructed to take antihypertensive drugs in the morning of their physical check-up. Blood pressure was measured using a mercury sphygmomanometer 3 times at 2-minute intervals after a 5-minute rest in a chair with the subject's back supported. The mean of the second and third measurements was recorded as the blood pressure. Hypertension was defined as SBP ≥140 mm Hg or diastolic blood pressure (DBP) ≥90 mm Hg, or if the subject was using any antihypertensive medications.[3] The use of antihypertensive agents was investigated by a questionnaire. Diabetes mellitus was defined as fasting plasma glucose ≥126 mg/dL or the use of antidiabetic medications, and dyslipidemia was defined as low-density lipoprotein cholesterol ≥140 mg/dL, high-density lipoprotein cholesterol < 40 mg/dL, triglycerides ≥150 mg/dL, or the use of antidyslipidemic medications.[25] Estimated glomerular filtration rate (eGFR) was calculated using the Chronic Kidney Disease Epidemiology Collaboration equation[26] and eGFR <60 mL/min per 1.73 m2 was defined as chronic kidney disease (CKD).
2.3. Statistical analysis
Statistical analyses were performed using SPSS version 24 (IBM, Chicago, IL). Data in the text and the tables are presented as the mean ± standard deviation. The characteristics of the participants in each year were analyzed cross-sectionally and compared during the study period. The Chi-squared test was used for comparisons of the prevalence and treatment rates of hypertension, as well as the rate at which target blood pressure was reached during the study period. Changes in blood pressure over the 15 years were evaluated using 1-way analysis of variance (ANOVA). The significance of differences between 2 mean values was determined using Student t test, whereas comparisons of categorical data were made using the Chi-squared test. Two-sided P < .05 was considered significant.
3. Results
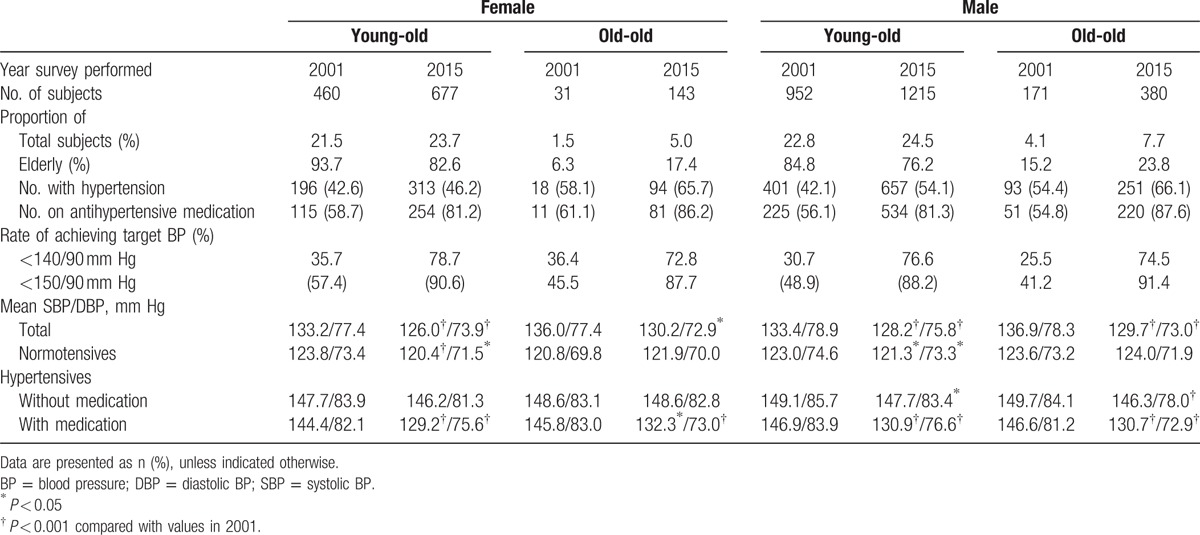
Table 1 lists the characteristics of the study participants taking part in the physical check-up program in 2001 and 2015. In 2001, approximately 25.5% of participants were elderly and, of these, 44% had hypertension. In 2001, blood pressure and the prevalence of hypertension were higher and eGFR was lower in elderly subjects (mean age 69.7 years) than in all subjects (mean age 56.3 years), although the lipid profile did not change with age. These observations did not change during the study period (Table 1). Yearly changes in the number of participants in the physical check-up program and their age distribution are shown in Fig. 1. The proportion of elderly subjects increased gradually over the 15 years (from 25.5% in 2001 to 31% in 2015) and slight aging was observed in the entire study cohort (from a mean age of 56.3 years in 2001 to 57.0 years in 2015; Table 1). The number of old-old people in 2015 was approximately 2.6-fold greater than in 2001 for both males (2.2-fold greater) and females (4.6-fold greater), and the proportion of old-old people of the total elderly in 2015 was approximately 1.7-fold greater than in 2001 (1.6- and 2.8-fold greater for males and females, respectively; Table 2). Despite the increase in the number of hypertensive elderly during the study period, the ratio of hypertensive elderly to all elderly showed only a modest increase (Fig. 2). However, the number of elderly hypertensives on medication and the rate of treatment of hypertension in elderly hypertensives were markedly increased in both young-old and old-old people (Fig. 3; Table 2). Of note, the rate at which target blood pressure, defined as SBP <140 mm Hg and DBP <90 mm Hg, was reached in elderly hypertensives on antihypertensive medication increased markedly, especially during the last 9 years of the study period, after 2006 (Fig. 4; Table 2). Similar results were obtained in analyses where the target blood pressure was defined as <150/90 mm Hg (data not shown).
Table 1.
Subject characteristics in 2001 and 2015.
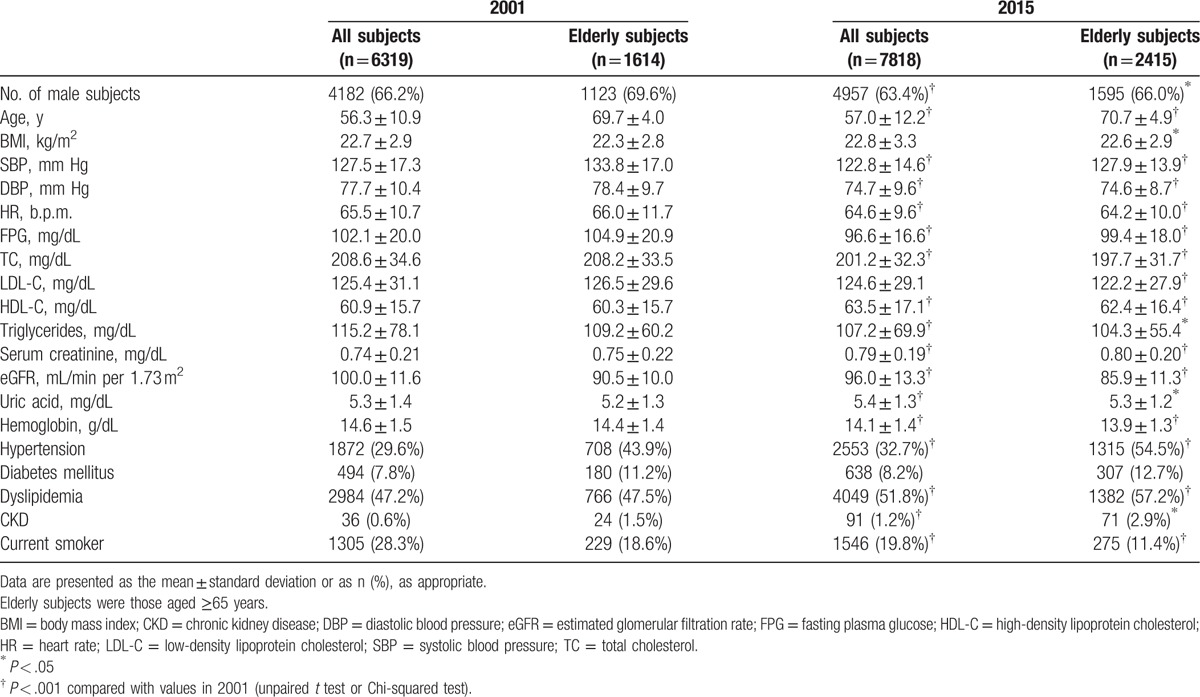
Figure 1.
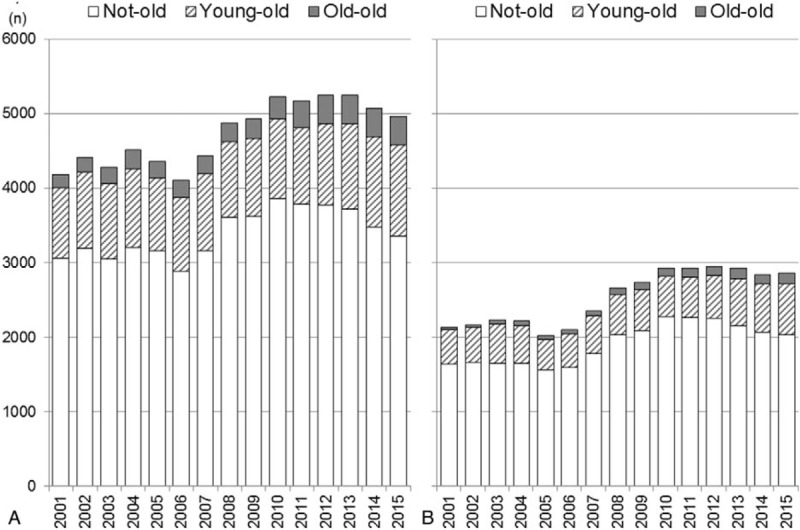
Changes in the number of (A) male and (B) female participants from 2001 to 2015. Not-old, subjects <65 years of age; young-old, subjects aged between 65 and <70 years; old-old, subjects aged ≥75 years. The ratio of elderly subjects to all participants increased for both male and female subjects over the 15 years of the study (P < .001, Chi-squared test).
Table 2.
Comparison of indices relevant to blood pressure in the young-old (65–74 years of age) and old-old (≥75 years of age) between 2001 and 2015.
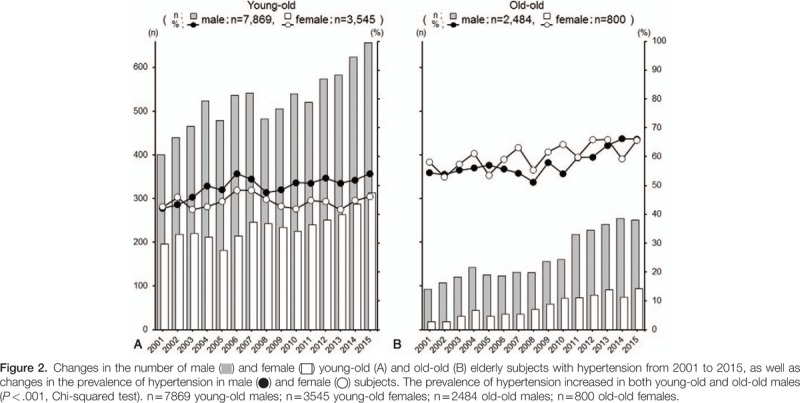
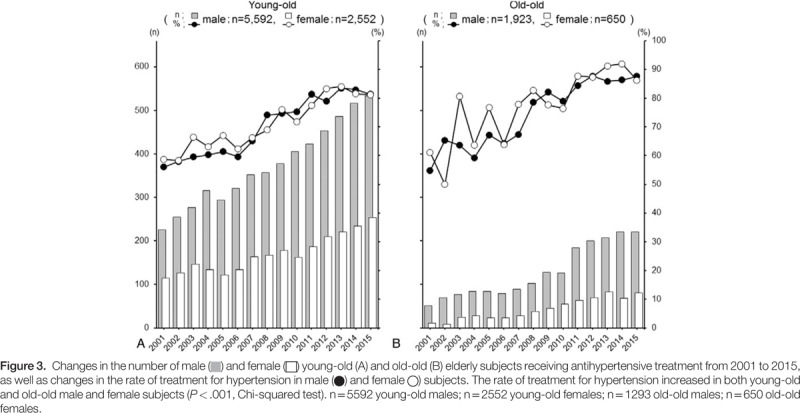
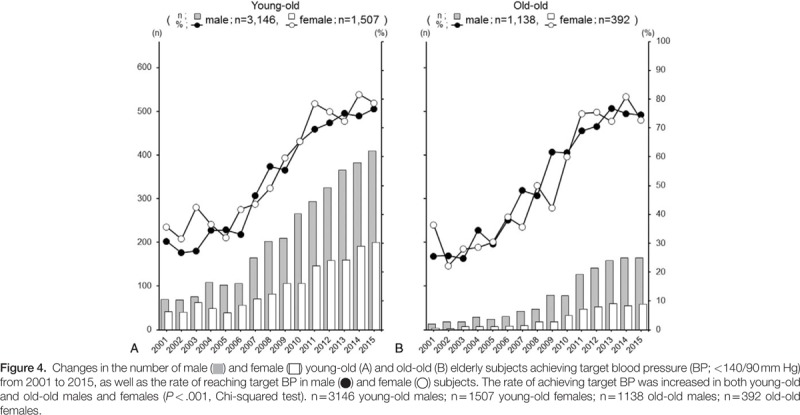
Mean blood pressure in the elderly decreased gradually and significantly in both males (from 134.0 ± 17.2/78.8 ± 9.7 mm Hg in 2001 to 128.5 ± 14.0/75.1 ± 8.7 mm Hg in 2015) and females (from 133.4 ± 16.4/77.4 ± 9.4 mm Hg in 2001 to 126.7 ± 13.8/73.8 ± 8.6 mm Hg in 2015; Fig. 5 ; Table 2), with a prominent decrease in mean blood pressure from 2006 to 2011. The decrease in blood pressure levels in the elderly was consistent in young-old and old-old people. The reduction in blood pressure levels over the 15 years was more prominent in hypertensive elderly subjects on antihypertensive medication than in other groups, and this had a considerable effect on the blood pressure reduction that was evident across all elderly subjects (Fig. 5 ).
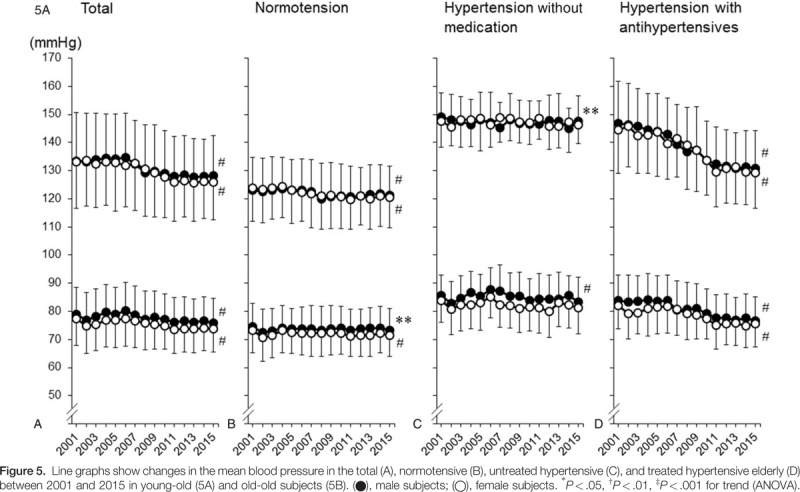
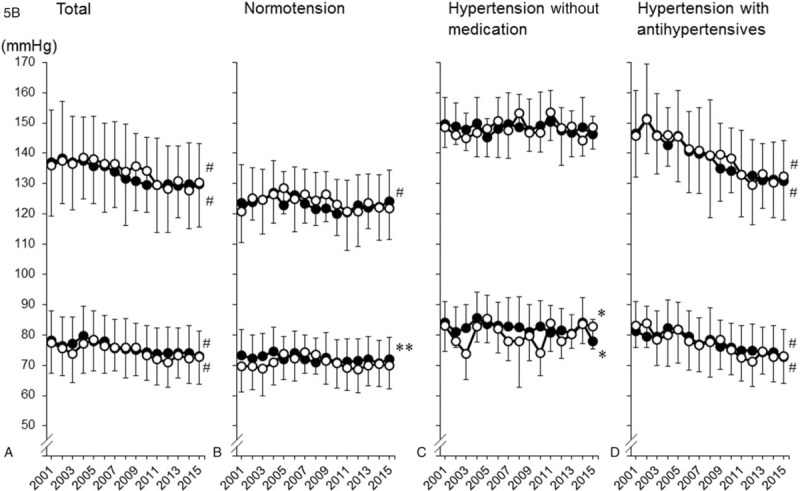
The Japanese Society of Hypertension (JSH) has published 4 guidelines for the management of hypertension (JSH2000,[27] JSH2004,[28] JSH2009,[29] and JSH2014[3]). In the present study, the mean changes in SBP in elderly hypertensives on medical treatment were –0.7 mm Hg/year (2001–2004), –1.4 mm Hg/year (2004–2009), –1.2 mm Hg/year (2009–2014), and –0.1 mm Hg/year (2014–2015).
4. Discussion
The present study has demonstrated that there was a marked reduction in the blood pressure of hypertensive elderly subjects on medication, which contributed to the gradual reduction in the mean blood pressure of elderly subjects over the past 15 years. The guidelines published by the JSH for the treatment of hypertension in 2004 and thereafter may have influenced the yearly changes in blood pressure in the elderly.
As noted for most areas in the world, over the 15 years of the present study, there was a gradual aging of subjects attending for their annual physical check-up. Aging of elderly participants, as well as all participants attending for the annual physical check-up, was evident, because the ratio of old-old to all elderly people was markedly increased, despite a reduction in the ratio of young-old to all elderly people. Aging naturally increases blood pressure,[23,24] which was confirmed in the present study by the observation that the prevalence of hypertension increased during the study period. Paradoxically, blood pressure levels in the elderly decreased gradually over the 15 years. This was due primarily to the marked reduction in blood pressure in both young-old and old-old hypertensive elderly subjects on antihypertensive medication, because there were no changes in blood pressure levels over the same time frame in normotensive elderly and hypertensive elderly subjects not on antihypertensive medication. The reduction in blood pressure in the hypertensive elderly on medication may be attributable to the marked increase in the rate at which target blood pressure, defined as less than 140/90 mm Hg, was reached. The JSH guidelines published in 2004[28] recommended lower target blood pressure in elderly hypertensives (<140/90 mm Hg) than the guidelines published in 2000[27] (<140–170/90 mm Hg depending on age), and this may have affected the results. Furthermore, an increase in the treatment rate may have contributed to the gradual reduction in blood pressure levels in the elderly. This may reflect changes in the guideline recommendations for blood pressure levels requiring treatment from JSH2000 to JSH2004. JSH2000 recommended treatment of elderly subjects in their 60s with blood pressure ≥140–160/90 mm Hg, those in their 70s with blood pressure ≥160–170/90 mm Hg, and those aged ≥80 years with blood pressure ≥160–180/90 mm Hg.[27] However, JSH2004 and the guidelines published thereafter (JSH2009[29] and JSH 2014[3]) recommended that elderly subjects with blood pressure ≥140/90 mm Hg receive antihypertensive treatment. Indeed, changes in the treatment rate of hypertension seemed to have an inflection point at 2006, though this was not supported by statistical analysis, when the intention of JSH2004 was widely disseminated among general physicians and the general population. These results and the interpretation of the results described above suggest that guidelines for the treatment of hypertension had, at least in part, an effect on blood pressure levels in the general population.[22] However, numerous factors other than the updating JSH guidelines may also have been associated with observed changes in blood pressure levels.
As noted above, the target blood pressure recommendations in JSH2000[27] for specific age groups was revised in 2004 to a single level of <140/90 mm Hg in elderly individuals aged ≥65 years.[28] Although there was a consistent reduction in blood pressure levels during the study period in hypertensive elderly subjects on antihypertensive medication, the yearly reduction was somewhat more prominent after 2006 in both young-old and old-old elderly. The guidelines may have affected the management of hypertension by general physicians. However, the present study did not investigate the causal relationship between the progressive improvement in the control of blood pressure and the updating of the JSH guidelines. Although the guidelines may have influenced the control of blood pressure, the evolution of pharmacological antihypertensive therapy, the improvement of adherence to antihypertensive therapy, and lifestyle modification may also have contributed to the improvement in the control of blood pressure during the last 15 years. Notably, the mean blood pressure in elderly hypertensives reached a level of <140/90 mm Hg in 2011 without obvious differences between young-old and old-old, and remained lower than 140/90 mm Hg thereafter. Because the mean blood pressure, but not BP in all individuals, was reduced to <140/90 mm Hg in the elderly, physicians may have managed their hypertensive elderly patients with special regard for marked individual differences in the elderly.
In contrast with the excellent blood pressure control coinciding with the guideline recommendations, there were a few hypertensive elderly subjects, especially young-old subjects, who were not on antihypertensive medication, indicating that the education of the general population regarding hypertension may not yet be sufficient. This concept agrees, at least in part, with the observation that the prevalence of hypertension increased slightly and gradually over the 15 years of the study. Primary prevention of hypertension was not successful and lifestyle modification did not appear to reduce the incidence of hypertension. New strategies to improve lifestyle and for the primary prevention of hypertension, as well as to further educate the population with regard to hypertension, are needed for further improvements of the blood pressure status of the elderly.
Interpretation of the data is limited because of the following study imitations. The present study was a survey of participants attending a physical check-up program. Although the prevalence of hypertension in each generation was similar to that reported previously in the general population,[22] there was an important selection bias that may have affected the deduction in results. In addition, because blood pressure was measured once a year at the annual physical check-up, the value may not accurately represent usual blood pressure in individuals, and information about antihypertensive drugs was obtained by questionnaire, without checking prescriptions. Finally, the present cross-sectional study did not investigate causal relationships between the improvement of the control of blood pressure and the updating of the JSH guidelines. Despite these limitations, the information obtained from more than 29,000 elderly subjects over 15 years is valuable.
In conclusion, the blood pressure level in elderly subjects decreased gradually between 2001 and 2015, primarily due to reductions in blood pressure in hypertensive elderly subjects receiving antihypertensive treatment, although the prevalence of hypertension increased slightly during the same period. This suggests that the intention of the JSH guidelines for the treatment of hypertension and their revisions has been widely disseminated among the elderly, as well as general physicians, resulting in improved management of hypertension in the elderly. However, the prevention of hypertension has not been achieved as yet.
Footnotes
Abbreviations: ANOVA = analysis of variance, CKD = chronic kidney disease, DBP = diastolic blood pressure, eGFR = estimated glomerular filtration rate, FPG = fasting plasma glucose, JSH = Japanese Society of Hypertension, SBP = systolic blood pressure.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Kannel WB. Hypertension as a risk factor for cardiac events: epidemiologic results of long-term studies. J Cardiovasc Pharmacol 1993;21(Suppl 2):S27–37. [DOI] [PubMed] [Google Scholar]
- [2].Ikeda A, Iso H, Yamagishi K, et al. Blood pressure and the risk of stroke, cardiovascular disease, and all cause mortality among Japanese: the JPHC Study. Am J Hypertens 2009;22:273–80. [DOI] [PubMed] [Google Scholar]
- [3].Shimamoto K, Ando K, Fujita T, et al. Japanese Society of Hypertension Committee for Guidelines for the Management of Hypertension. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2014). Hypertens Res 2014;37:253–387. [DOI] [PubMed] [Google Scholar]
- [4].Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ 2009;338:b1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Ettehad D, Emdin CA, Kiran A, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet 2016;387:957–67. [DOI] [PubMed] [Google Scholar]
- [6].Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering treatment in hypertension: 8. Outcome reductions vs. discontinuations because of adverse drug events: meta-analyses of randomized trials. J Hypertens 2016;34:1451–63. [DOI] [PubMed] [Google Scholar]
- [7].Amery A, Birkenhäger W, Brixko P, et al. Mortality and morbidity results from the European working party on high blood pressure in the elderly trial. Lancet 1985;325:1349–54. [DOI] [PubMed] [Google Scholar]
- [8].Coope J, Warrender T. Randomised trial of treatment of hypertension in elderly patients in primary care. Br Med J (Clin Res Ed) 1986;293:1145–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Dahlöf B, Lindholm LH, Hansson L, et al. Morbidity and mortality in the Swedish Trial in Old Patients with Hypertension (STOP-Hypertension). Lancet 1991;338:1281–5. [DOI] [PubMed] [Google Scholar]
- [10].SHEP. Cooperative Research, Group, Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). JAMA 1991;265:3255–64. [PubMed] [Google Scholar]
- [11].MRC Working Party. Medical Research Council trial of treatment of hypertension in older adults: principal results. BMJ 1992;304:405–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Gong L, Zhang W, Zhu Y, et al. Shanghai trial of nifedipine in the elderly (STONE). J Hypertens 1996;14:1237–45. [DOI] [PubMed] [Google Scholar]
- [13].Staessen JA, Fagard R, Thijs L, et al. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. The Systolic Hypertension in Europe (Syst-Eur) Trial Investigators. Lancet 1997;350:757–64. [DOI] [PubMed] [Google Scholar]
- [14].Liu L, Wang JG, Gong L, et al. Systolic Hypertension in China (Syst-China) Collaborative Group. Comparison of active treatment and placebo in older Chinese patients with isolated systolic hypertension. J Hypertens 1998;16:1823–9. [DOI] [PubMed] [Google Scholar]
- [15].Beckett NS, Peters R, Fletcher AE, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med 2008;358:1887–98. [DOI] [PubMed] [Google Scholar]
- [16].Pimenta E, Oparil S. Management of hypertension in the elderly. Nat Rev Cardiol 2012;9:286–96. [DOI] [PubMed] [Google Scholar]
- [17].Oliva RV, Bakris GL. Management of hypertension in the elderly population. J Gerontol A Biol Sci Med Sci 2012;67:1343–51. [DOI] [PubMed] [Google Scholar]
- [18].Alhawassi TM, Krass I, Pont LG. Hypertension in older persons: a systematic review of national and international treatment guidelines. J Clin Hypertens 2015;17:486–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Williamson JD, Supiano MA, Applegate WB, et al. SPRINT Research Group. Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged ≥75 years: a randomized clinical trial. JAMA 2016;315:2673–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 2013;34:2159–219. [DOI] [PubMed] [Google Scholar]
- [21].James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014;311:507–20. [DOI] [PubMed] [Google Scholar]
- [22].Mogi M, Hasebe N, Horiuchi M, et al. The results of a survey of physicians about the Japanese Society of Hypertension Guidelines for the Management of Hypertension 2014 and its clinical use. Hypertens Res 2016;39:660–3. [DOI] [PubMed] [Google Scholar]
- [23].Fagard RH. Epidemiology of hypertension in the elderly. Am J Geriatr Cardiol 2002;11:23–8. [DOI] [PubMed] [Google Scholar]
- [24].Robles NR, Macias JF. Hypertension in the elderly. Cardiovasc Hematol Agents Med Chem 2015;12:136–45. [DOI] [PubMed] [Google Scholar]
- [25].Teramoto T, Sasaki J, Ueshima H, et al. Japan Atherosclerosis Society (JAS) Committee for Epidemiology and Clinical Management of Atherosclerosis. Diagnostic criteria for dyslipidemia. Executive summary of Japan Atherosclerosis Society (JAS) guideline for diagnosis and prevention of atherosclerotic cardiovascular diseases for Japanese. J Atheroscler Thromb 2007;14:155–8. [DOI] [PubMed] [Google Scholar]
- [26].Levey AS, Stevens LA, Schmid CH, et al. CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration). A new equation to estimate glomerular filtration rate. Ann Intern Med 2009;150:604–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Japanese Society of Hypertension Guidelines Subcommittee for the Management of, Hypertension. Guidelines for the management of hypertension for general practitioners. Hypertens Res 2001;24:613–34. [DOI] [PubMed] [Google Scholar]
- [28].Japanese Society of Hypertension. Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2004). Hypertens Res 2006;29(Suppl):S1–05. [DOI] [PubMed] [Google Scholar]
- [29].Ogihara T, Kikuchi K, Matsuoka H, et al. Japanese Society of Hypertension Committee. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2009). Hypertens Res 2009;32:3–107. [PubMed] [Google Scholar]


