Abstract
Escalating costs and concerns about quality of cancer care have increased calls for quality measurement and performance accountability for providers and health plans. The purpose of the present cross-sectional study was to assess variability in the quality of cancer care by health insurance type in California.
Persons with breast, ovary, endometrium, cervix, colon, lung, or gastric cancer during the period 2004 to 2014 were identified in the California Cancer Registry. Individuals were stratified into 5 health insurance categories: private insurance, Medicare, Medicaid, dual Medicare and Medicaid eligible, and uninsured. Quality of care was evaluated using Commission on Cancer quality measures. Logistic regression models were generated to assess the independent effect of health insurance type on stage at diagnosis, quality of care and survival after adjusting for age, sex, race/ethnicity, and socioeconomic status (SES).
A total of 763,884 cancer cases were evaluated. Individuals with Medicaid or Medicare-Medicaid dual-eligible coverage and the uninsured had significantly lower odds of receiving recommended radiation and/or chemotherapy after diagnosis or surgery for breast, endometrial, and colon cancer, relative to those with private insurance. Dual eligible patients with gastric cancer had 21% lower odds of having the recommended number of lymph nodes removed and examined compared to privately insured patients.
After adjusting for known demographic confounders, substantial and consistent disparities in quality of cancer care exist according to type of health insurance in California. Further study is needed to identify particular factors and mechanisms underlying the identified treatment disparities across sources of health insurance.
Keywords: cancer, disparities, health insurance, public health, quality improvement, quality of care
1. Introduction
Approximately 173,000 new cancer cases are diagnosed in California each year, and 1.4 million Californians alive today are living with cancer or have a history of the disease.[1,2] Rapidly rising costs of cancer care and deficiencies in the quality of cancer care are of growing concern.[3] Direct spending on cancer care in the United States doubled between 1990 and 2010, from approximately 63 billion dollars in 1990 to 125 billion in 2010. Spending is estimated to rise to $158 to 207 billion by 2020.[4] The escalating cost of cancer care and the observed quality of care shortcomings have increased calls for quality measurement and performance accountability for providers of cancer care.
Previous studies have indicated that advances in cancer treatment have not benefitted cancer patients equally; disparities exist in quality of cancer treatment according to demographic factors such as race/ethnicity, socioeconomic status (SES), and source of health insurance.[5–9] Several studies have found African-Americans and Hispanic cancer patients receive lower quality of care relative to their non-Hispanic white counterparts.[10–12] The associations between health insurance type and quality of cancer care are not well defined, but some studies have reported lower quality of care for some specific cancers among individuals who were uninsured or on Medicaid insurance at the time of their cancer diagnosis.[11,13–15]
The present study builds on a prior descriptive report which identified disparities in the quality and outcomes of cancer care by source of health insurance among cancer patients in California.[16] While the univariate findings presented in the previous report suggested some disparities in quality of care, these results were not adjusted for demographic factors such as race, SES, and age. The purpose of this more granular analysis was to determine if the quality of care disparities across type of health insurance exist after accounting for possibly confounding demographic characteristics.
2. Methods
2.1. Study population
Individuals diagnosed with cancers of the breast, ovary, endometrium, cervix, colon, lung, or stomach during the period 2004–2014, were identified in the California Cancer Registry (CCR). The CCR is the largest, population-based cancer surveillance system for a geographically contiguous area in the world, collecting incidence reports on over 160,000 new cases of cancer diagnosed annually in California. The CCR has collected data on tumor characteristics, diagnosis, treatment, follow-up, and patient's demographic information for incident cancers diagnosed since 1988. The CCR has consistently met the highest national standards for data quality and completeness. Data are collected through a network of regional registries, which are also affiliated with the National Cancer Institute's Surveillance, Epidemiology and End Results (SEER) program. Site-specific cancer cases were identified using site and histology codes as defined in the International Classification of Diseases for Oncology, Third Edition (ICD-O-3).[17] The rationale for only including cases diagnosed from 2004 forward is that information on stage of disease classified according to the American Joint Commission on Cancer (AJCC) staging scheme is only available starting in 2004. This study was approved by the institutional review board at the University of California, Davis.
2.2. Description of variables
The outcome of interest in this study was receipt of high quality cancer care, as specified by established Commission on Cancer (COC) quality measures for which reliable information was available in the CCR.[18] Each measure includes detailed specifications along with case eligibility criteria, which were used to select cases. Quality of care was measured using 10 performance measures across the 7 cancer sites included in the analysis.
CCR collects information on both primary and secondary payer at the time of diagnosis. Information from these 2 variables was aggregated to create 5 categories of health insurance: Medicare, Medicaid, dual eligible (both Medicare and Medicaid insurance), privately insured, and uninsured. In addition to those with health maintenance organization (HMO), preferred provider organization (PPO) or fee for service insurance, private insurance included individuals on Medicare with private supplement. Persons with Medicaid in either the primary or secondary payer categories were classified as either dual eligible (cases with both Medicare and Medicaid insurance) or Medicaid (Medicaid + other source of insurance). Persons having Medicare-Medicaid dual eligibility (i.e., persons with Medicare primary coverage and Medicaid supplemental insurance) are of particular interest from a cancer care perspective because disproportionate numbers of these “dual eligible” persons are at higher risk for cancer (compared to the general population) due to advanced age and adverse socioeconomic circumstances, among other factors.
Patients with payer source designated as county health insurance or Indian Health Service were not included in the analysis due to the heterogeneity of program administration and delivery of care for these persons. There is great variation across California's 58 counties in the way locally financed (i.e., county-financed) health care is delivered. Some counties operate large healthcare systems, while others purchase medical services from private providers.[19] The delivery of care among individuals with Indian Health Service (IHS) insurance also varies throughout the state because the vast majority of Native Americans in California reside in urban areas, rather than on reservations where residents are more likely to receive care via IHS facilities.[20] Individuals with any type of military service-related insurance (Department of Veterans Affairs or Department of Defense), were also excluded from the analysis since the CCR is only authorized to use these data for public health surveillance.
Stage of disease was classified according to the AJCC staging scheme.[21] Type of surgery was classified based on codes from the American College of Surgeons’ Commission on Cancer Facility Oncology Registry Data Standards (FORDS).[22] Race/ethnicity was coded according to the North American Association of Central Cancer Registries’ Hispanic and Asian/Pacific Islander Identification Algorithm.[23] Age at diagnosis was grouped into four categories: under 40 years, 40 to 64, 65 to 74, and over 75 years of age. As one of the breast cancer quality measures specified an upper age limit of 70, age at diagnosis for this analysis was grouped into 3 categories: under age 50, 50 to 59, and 60 to 69. SES was measured using an established aggregate measure of neighborhood SES, based on patients’ block group of residence at the time of diagnosis.[24]
2.3. Statistical analysis
Descriptive statistics were generated to summarize the demographic characteristics of the study population by cancer type. Multivariate logistic regression models were run to assess the associations between receipt of appropriate surgery/recommended treatment (measured by adherence to individual COC quality measures—yes/no), and source of health insurance at the time of diagnosis. Private insurance was the referent category. All models were adjusted for sex, age, race/ethnicity, SES, and stage (for those measures that did not have stage as a defining criterion). Cases with unknown values for any of the modelled variables (summarized in Table 1) were excluded from the multivariate analysis.
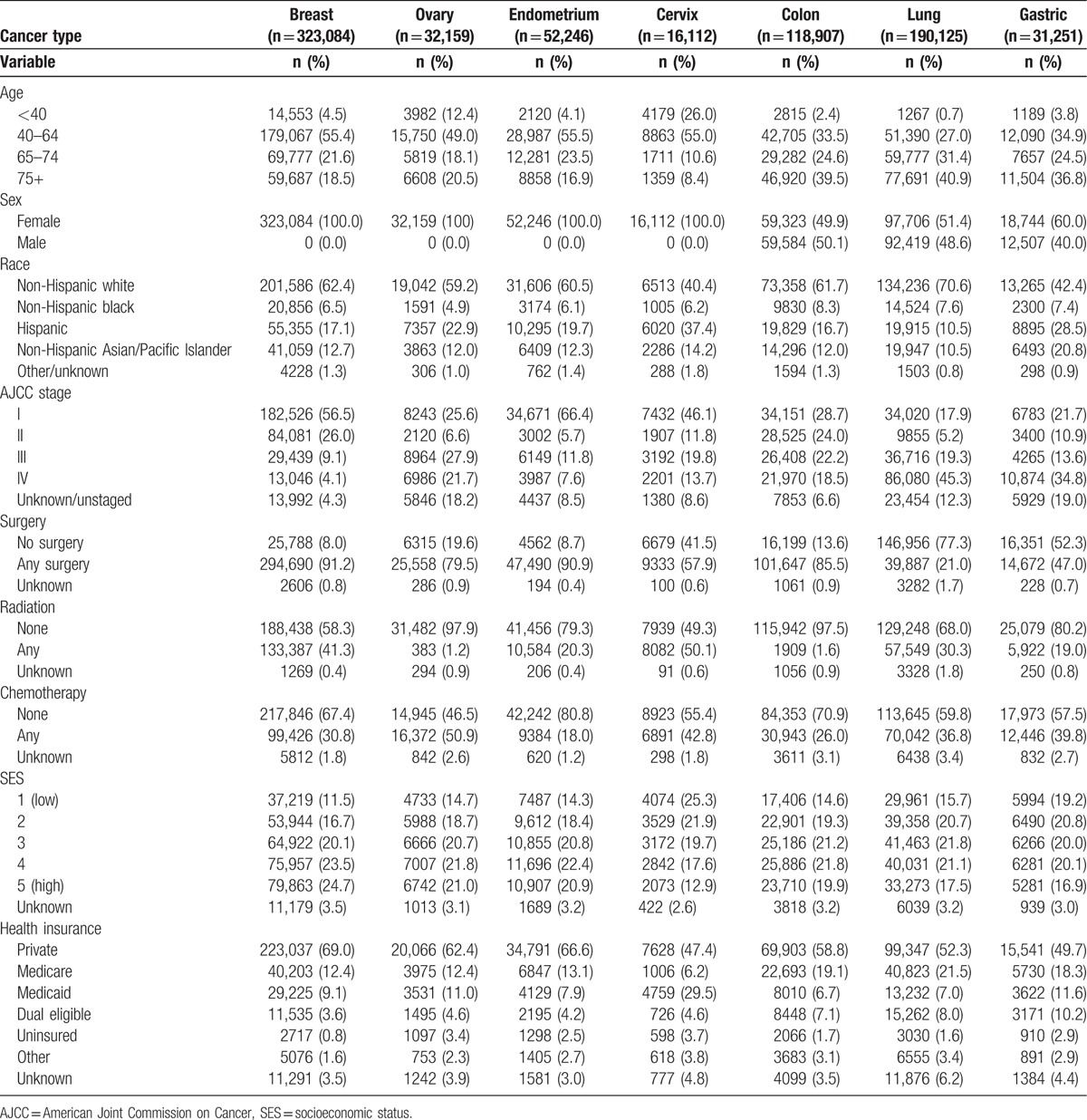
Table 1.
Demographic characteristics of California cancer patients by cancer site, 2004–2014 (n = 763,884).
3. Results
3.1. Characteristics of the study population
Demographic and clinical characteristics of the study population are summarized in Table 1. A total of 763,884 cases were available for analysis across the 7 cancer sites examined, with cancer specific sample sizes ranging from 16,112 cervical cancer cases to 323,084 breast cancers. As expected, the largest proportions were diagnosed between 40 and 64 years of age for all cases. Consistent with known incidence patterns, considerably larger proportions of individuals with cervical cancer were under age 40, compared to those diagnosed with other cancer types. Larger proportions of colon and lung cancer cases were 75 years or older at the time of diagnosis compared to the proportions diagnosed in this age group with other cancer types.
The single largest insurance grouping was private insurance for all cancer types. Slightly lower proportions of cervix and gastric cancer patients were privately insured relative to those with other cancer types. The proportions of cancer patients with Medicare insurance at the time of diagnosis ranged from 6% (cervix) to 22% (lung). The cervical cancer group had the highest proportions of individuals with Medicaid (30%) and those who were uninsured (3.7%) at the time of diagnosis compared with patients diagnosed with other cancers.
3.2. Breast cancer
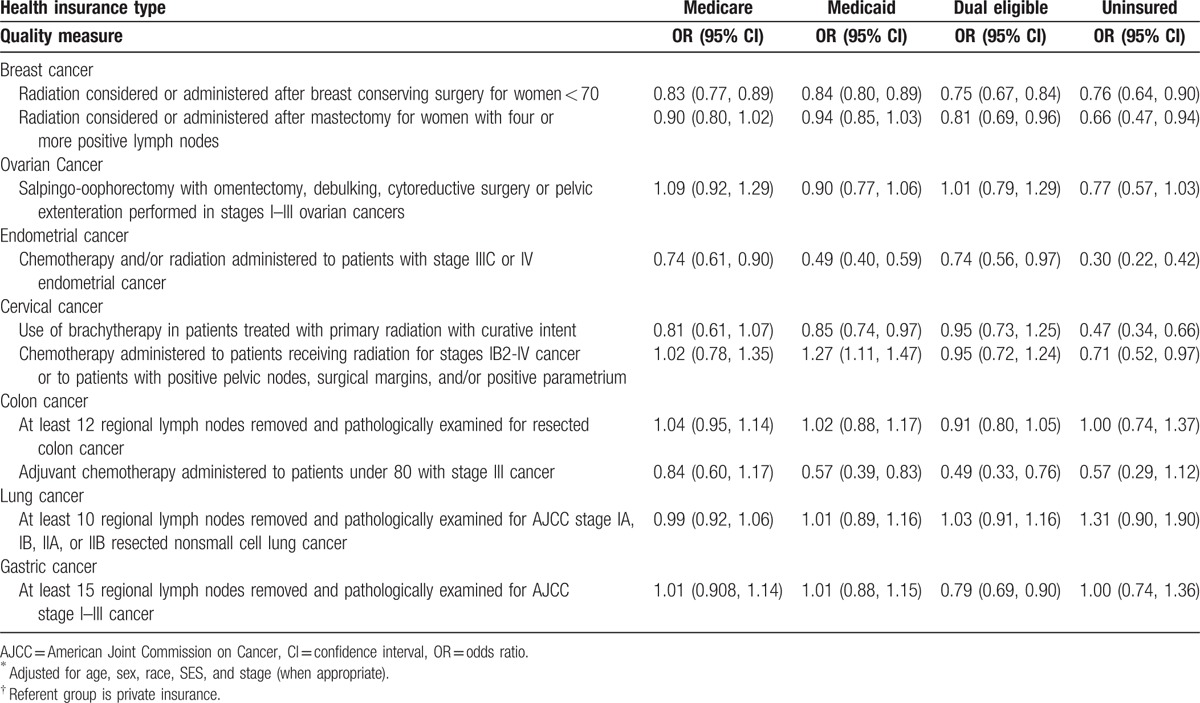
Multivariate analysis of the association between adherence with 2 breast cancer quality performance measures and payer source revealed significant differences by insurance type (Table 2). Breast cancer patients in all other insurance groups had significantly lower odds (16–25%) of receiving radiation after breast conserving surgery (BCS) compared with the privately insured group. Both the dual eligible group (OR = 0.75, 95% CI = 0.67–0.84) and the uninsured (OR = 0.76, 95% CI = 0.64–0.90), were least likely to have had radiation after BCS compared to those with private insurance. Among breast cancer cases with four or more positive lymph nodes, both uninsured (OR = 0.66, 95% CI = 0.47–0.94) and dual eligible patients (OR = 0.81, 95% CI = 0.69–0.96) had significantly lower odds of having radiation considered or administered after mastectomy.
Table 2.
Association between health insurance type and concordance with quality measures by cancer type, 2004–2014, California∗,†.
3.3. Ovarian cancer
No significant differences were found in receipt of appropriate surgery (salpingo-oophorectomy with omentectomy, debulking, cytoreductive surgery or pelvic exenteration) for stages I–III ovarian cancers across insurance groups. Uninsured individuals were 23% less likely to have the appropriate surgery compared to those with private insurance, although this result did not reach statistical significance (OR = 0.77, 95% CI = 0.57–1.03).
3.4. Endometrial cancer
Persons with stage III and IV endometrial cancer who had Medicare or dual Medicare-Medicaid insurance at the time of diagnosis had 26% lower odds of having chemotherapy or radiation administered compared with privately insured cases. Persons with Medicaid coverage were 51% less likely to receive chemotherapy and radiation compared to the group with private insurance. Uninsured persons had the lowest odds of receiving chemotherapy compared to those with private insurance (OR = 0.30, 95% CI = 0.22–0.42).
3.5. Cervical cancer
Cervical cancer cases treated with primary radiation who were on Medicaid at the time of diagnosis had significantly lower odds of having brachytherapy as the treatment modality (OR = 0.85, 95% CI = 0.74–0.97) compared to those with private insurance. The uninsured were 53% less likely than their privately insured counterparts to have had brachytherapy used as the radiation treatment modality (OR = 0.47, 95% CI = 0.34–0.66). The Medicare and dual eligible groups were not significantly different from private insurance in this regard.
3.6. Colon cancer
Among colon cancer patients who had surgical resection, there were no significant differences by health insurance type with respect to the odds of having at least 12 lymph nodes removed and pathologically examined. Individuals with Stage III colon cancer who had Medicaid or were Medicare-Medicaid dual eligible were 43% and 51%, respectively, less likely to receive adjuvant chemotherapy compared to privately insured patients. The results for the Medicare and uninsured groups were suggestive of lower odds of receipt of chemotherapy, but the differences did not reach statistical significance.
3.7. Lung cancer
All groups had similar odds of having at least 10 regional lymph nodes removed and examined for stages IA–IIB resected nonsmall cell lung cancer; there were no significant differences from the group with private insurance.
3.8. Gastric cancer
Dual eligible patients with stages I–III gastric cancer had 21% lower odds of having at least 15 regional lymph nodes removed and examined compared to patients with private insurance. Those with Medicare or Medicaid insurance, as well as the uninsured, were not significantly different from the privately insured with respect to this performance measure.
4. Discussion
Substantial and consistent disparities in quality of care were found among cancer patients with different sources of health insurance in California over the 11-year study period, after accounting for possibly confounding factors such as age, race, sex, and SES. Persons having Medicaid or Medicare-Medicaid dual coverage or having no insurance appear to consistently receive lower quality cancer care than privately insured patients, as indicated by adherence to multiple quality measures across several cancer types. Although the lower quality of care among the uninsured may not be unexpected, the Medicaid and dual eligible groups had results similar to or worse than the uninsured for several types of cancer. The results of this multivariate analysis are consistent with the less granular findings noted in a previous report.[16]
Significant differences in receipt of radiation after BCS were observed across all insurance groups compared to the privately insured; all were significantly less likely to receive radiation. Among those who underwent mastectomy, both the dual eligible and uninsured groups were considerably less likely to receive radiation after BCS or mastectomy compared to their privately insured counterparts. Our results are consistent with previous research about breast cancer treatment, conducted in both state-specific and national populations.[5,8,14,25,26] A study conducted in Florida by Voti et al, found that women with Medicaid insurance at the time of diagnosis were 29% less likely to receive recommended treatment for breast cancer, which is comparable to our findings of 16% and 24% lower odds of receiving radiation for the Medicaid and Medicare-Medicaid dual eligible groups, respectively. Similar findings were observed among late stage endometrial cancer patients in California; all groups had similarly lower odds of receiving chemotherapy or radiation compared to patients with private insurance.[6] A study of cancer patients in Rhode Island reported that significantly lower proportions of breast cancer patients with Medicaid received BCS compared with privately insured patients.[14]
The odds of receiving brachytherapy as the modality for radiation treatment of cervical cancer were significantly lower among Medicaid and uninsured patients. This finding is consistent with the results of a previous study, which analyzed information from the National Cancer Data Base.[27] Benefits of brachytherapy include cost effectiveness, minimization of side effects, and the ability to deliver accurate and targeted treatment doses.[6,27] The reason for this finding may be related to the lack of availability of this specialized treatment at some treatment facilities (e.g., hospitals lacking Commission on Cancer accreditation or nonteaching hospitals), since the Medicaid and uninsured populations tend to have less access to specialists and high volume cancer treatment centers.[28] The declining trend in the use of brachytherapy in favor of newer boost modalities has been documented,[6,27,29] as has the increased risk of mortality, leading many physicians to question this trend.
Colon and gastric cancer patients with Medicare-Medicaid dual eligibility were less likely to have the appropriate minimum number of lymph nodes removed and examined. Previous studies of colon cancer treatment have yielded inconsistent results in this regard.[11] Additionally, Medicaid and dual eligible patients were the only groups significantly less likely than privately insured patients to receive adjuvant chemotherapy. A study using Tennessee cancer registry data found similar rates of adherence to colon cancer treatment guidelines across all insurance groups, but other studies have reported significant associations between hospitals with a high proportion of Medicaid patients and poor performance on evidence-based care.[11]
Our findings suggest that when compared to privately insured persons, the overall quality of care is significantly lower among cancer patients insured by Medicaid and those with Medicare-Medicaid dual coverage, even after accounting for demographics and stage at diagnosis. For multiple cancer types, adherence to quality of care measures for these 2 groups is comparable to or worse than for the uninsured population.
Determining the reasons for the differences in quality of care was beyond the scope of this study, but previous studies have indicated that physician referral patterns differ for patients according to insurance type.[30] Previous research has detected differences in referral rates to high volume cancer treatment hospitals by insurance type, which may also limit the referral networks available to cancer patients with Medicaid and the uninsured.[31,32]
This analysis has some important data limitations that should be considered when interpreting the results. The analysis used only the payer source information available in the CCR. The quality and completeness of this information varies by type of insurance. Particular concerns exist with regard to Medicaid. One previous validation study of payer source data in the CCR database reported poor sensitivity of the Medicaid information (48%), but good specificity (98%).[33] Given these results, it would be reasonable to assume that Medicaid coverage is underestimated in the CCR. The effect of undercounting Medicaid coverage in the CCR cannot be predicted with certainty, although it may well diminish actual differences in outcomes between Medicaid and other insurers. That is, the disparities observed for Medicaid beneficiaries might be greater if Medicaid coverage were more completely captured in the CCR data. Further investigation should be done linking CCR data with Medicaid enrollment and paid claims data.
As CCR collects information only on first course of treatment, the database does not contain uniformly highly reliable information regarding the administration of treatment. A validation study of the Surveillance, Epidemiology, and End Results (SEER) database (which includes CCR data), using Patterns of Care study data indicated reasonably high degrees of accuracy for California data, however. Sensitivity and specificity of CCR data to correctly identify receipt of chemotherapy were 85% and 93%, respectively. Positive and negative predictive value measures for chemotherapy were 91% and 90%, respectively. Sensitivity and specificity of CCR data to correctly identify receipt of radiation were 89% and 91%, respectively. Positive and negative predictive value measures for radiation were 84% and 94% (Anne-Michelle Noone, M.S., e-mail communication, July 2017).
Additionally, information on the timing of treatment across treatment types is somewhat limited in the CCR. In doing the analysis of quality measures, it was assumed that radiation and chemotherapy were delivered within the recommended timeframes. If this assumption were substantially incorrect, then the observed results may have overstated the actual quality of care.
Finally, information on duration of enrollment is not available in the CCR. As a result, we were not able to ascertain whether individuals were enrolled in a given health insurance program before cancer diagnosis or if the diagnosis of cancer precipitated their enrollment in the program. This is particularly relevant to Medicaid, in which patients go on and off being covered relatively frequently. In this regard, it is relevant to note that in a recently completed analysis of utilization of gene expression profiling in breast cancer patients in which CCR and Medicaid eligibility databases were linked, 59% of Medicaid members were enrolled before being diagnosed with breast cancer and 40% were enrolled the same month as or subsequent to their diagnosis.[34]
This study is the first multivariate, population-based assessment of cancer care quality in California across multiple cancers and health insurance types. Despite possible data limitations, the results of the present study are particularly relevant in light of the rapidly changing healthcare environment. As payment models for oncology care evolve, it will be important to understand and address disparities in the quality of care by type of health insurance. Further study is needed to identify the particular factors and mechanisms underlying the identified treatment disparities across sources of health insurance.
Footnotes
Abbreviations: AJCC = American Joint Commission on Cancer, BCS = breast conserving surgery, CCR = California Cancer Registry, COC = Commission on Cancer, FORDS = Facility Oncology Registry Data Standards, HMO = health maintenance organization, PPO = preferred provider organization, SEER = Surveillance, Epidemiology, and End Results, SES = socioeconomic status.
Funding: The collection of cancer incidence data used in this study was supported by the California Department of Public Health as part of the statewide cancer reporting program mandated by California Health and Safety Code Section 103885; the National Cancer Institute's Surveillance, Epidemiology and End Results Program under contracts awarded to the Cancer Prevention Institute of California, the University of Southern California, and the Public Health Institute; and the Centers for Disease Control and Prevention's National Program of Cancer Registries, under agreement awarded to the California Department of Public Health. The ideas and opinions expressed herein are those of the author(s) and endorsement by the State of California, Department of Public Health, the National Cancer Institute, the Centers for Disease Control and Prevention, or their Contractors and Subcontractors is not intended nor should be inferred.
The authors have no conflicts of interest to disclose.
References
- [1].American Cancer Society and California Department of Public Health, California Cancer Registry. California Cancer Facts and Figures 2016. Oakland, CA: American Cancer Society, California Division; 2016. [Google Scholar]
- [2].Chen Y, MacGuire F, Morris C, et al. Cancer Prevalence in California Counties. Sacramento, CA, Institute for Population Health Improvement, UC Davis Health; January 2017. [Google Scholar]
- [3].Institute of Medicine. Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis. Washington, DC: National Academies Press; 2013. [PubMed] [Google Scholar]
- [4].The State of Cancer Care in America, 2014: A Report by the American Society of Clinical Oncology American Society of Clinical Oncology Journal of Oncology Practice 2014;10:2, 119–142. [DOI] [PubMed] [Google Scholar]
- [5].Ali AA, Xiao H, Kiros GE. Health insurance and breast-conserving surgery with radiation treatment. Am J Manag Care 2014;20:502–16. [PubMed] [Google Scholar]
- [6].Grant SR, Walker GV, Koshy M, et al. Impact of insurance status on radiation treatment modality selection among potential candidates for prostate, breast, or gynecologic brachytherapy. Int J Radiat Oncol Biol Phys 2015;93:968–75. [DOI] [PubMed] [Google Scholar]
- [7].Hassett MJ, Schymura MJ, Chen K, et al. Variation in breast cancer care quality in New York and California based on race/ethnicity and Medicaid enrollment. Cancer 2016;122:420–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Walker GV, Grant SR, Guadagnolo BA, et al. Disparities in stage at diagnosis, treatment, and survival in nonelderly adult patients with cancer according to insurance status. J Clin Oncol 2014;32:3118–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Parikh AA, Robinson J, Zaydfudim VM, et al. The effect of health insurance status on the treatment and outcomes of patients with colorectal cancer. J Surg Oncol 2014;110:227–32. [DOI] [PubMed] [Google Scholar]
- [10].Freedman RA, Virgo KS, He Y, et al. The association of race/ethnicity, insurance status, and socioeconomic factors with breast cancer care. Cancer 2011;117:180–9. [DOI] [PubMed] [Google Scholar]
- [11].Rhoads KF, Ngo JV, Ma Y, et al. Do hospitals that serve a high percentage of Medicaid patients perform well on evidence-based guidelines for colon cancer care? J Health Care Poor Underserved 2013;24:1180–93. [DOI] [PubMed] [Google Scholar]
- [12].Silber JH, Rosenbaum PR, Clark AS, et al. Characteristics associated with differences in survival among black and white women with breast cancer. JAMA 2013;310:389–97. [DOI] [PubMed] [Google Scholar]
- [13].Bradley CJ, Given CW, Roberts C. Late stage cancers in a Medicaid-insured population. Med Care 2003;41:722–8. [DOI] [PubMed] [Google Scholar]
- [14].Coburn N, Fulton J, Pearlman DN, et al. Treatment variation by insurance status for breast cancer patients. Breast J 2008;14:128–34. [DOI] [PubMed] [Google Scholar]
- [15].Roetzheim RG, Gonzalez EC, Ferrante JM, et al. Effects of health insurance and race on breast carcinoma treatments and outcomes. Cancer 2000;89:2202–13. [DOI] [PubMed] [Google Scholar]
- [16].Parikh-Patel A, Morris CR, Martinsen R, et al. Disparities in Stage at Diagnosis, Survival, and Quality of Cancer Care in California by Source of Health Insurance. Sacramento, CA: California Cancer Reporting and Epidemiologic Surveillance Program, Institute for Population Health Improvement, University of California Davis; 2015. [Google Scholar]
- [17].International Classification for Diseases for Oncology. Geneva, Switzerland: World Health Organization; 2013. [Google Scholar]
- [18].Commission on Cancer: Quality Measures [October 18, 2016]. Available from: www.facs.org/cancer/qualitymeasures.html. Accessed August 22, 2016. [Google Scholar]
- [19].Kelch D. The Crucial Role of Counties in the Health of Californians: An Overview. California Healthcare Foundation. Oakland, CA. 2011. [Google Scholar]
- [20].James C, Schwartz K, Berndt J. A Profile of American Indians and Alaska Natives and Their Health Coverage. Washington DC: Henry J Kaiser Family Foundation; 2009. [Google Scholar]
- [21].Edge SB, Byrd DR, Compton CC, et al. (editors). AJCC Cancer Staging Manual. 7th ed. France: Springer; 2010. [Google Scholar]
- [22].Commission of Cancer. Facility Oncology Registry Data Standards (FORDS). Available from: https://www.facs.org/∼/media/files/quality%20programs/cancer/coc/fords/fords%202015.ashx. Accessed August 22, 2016. [Google Scholar]
- [23].NAACCR Race and Ethnicity Work Group. NAACCR Asian Pacific Islander Identification Algorithm [NAPIIA v1.2.1]. Springfield, IL: North American Association of Central Cancer Registries; 2011. [Google Scholar]
- [24].Yost K, Perkins C, Cohen R, et al. Socioeconomic status and breast cancer incidence in California for different race/ethnic groups. Cancer Causes Control 2001;12:703–11. [DOI] [PubMed] [Google Scholar]
- [25].Shavers VL, Harlan LC, Stevens JL. Racial/ethnic variation in clinical presentation, treatment, and survival among breast cancer patients under age 35. Cancer 2003;97:134–47. [DOI] [PubMed] [Google Scholar]
- [26].Voti L, Richardson LC, Reis I, et al. The effect of race/ethnicity and insurance in the administration of standard therapy for local breast cancer in Florida. Breast Cancer Res Treat 2006;95:89–95. [DOI] [PubMed] [Google Scholar]
- [27].Gill BS, Lin JF, Krivak TC, et al. National Cancer Data Base analysis of radiation therapy consolidation modality for cervical cancer: the impact of new technological advancements. Int J Radiat Oncol Biol Phys 2014;90:1083–90. [DOI] [PubMed] [Google Scholar]
- [28].Rosenbaum S. Medicaid payments and access to care. N Engl J Med 2014;371:2345–7. [DOI] [PubMed] [Google Scholar]
- [29].Han K, Milosevic M, Fyles A, et al. Trends in the utilization of brachytherapy in cervical cancer in the United States. Int J Radiat Oncol Biol Phys 2013;87:111–9. [DOI] [PubMed] [Google Scholar]
- [30].Spencer CS, Gaskin DJ, Roberts ET. The quality of care delivered to patients within the same hospital varies by insurance type. Health Aff (Millwood) 2013;32:1731–9. [DOI] [PubMed] [Google Scholar]
- [31].Liu JH, Zingmond DS, McGory ML, et al. Disparities in the utilization of high-volume hospitals for complex surgery. JAMA 2006;296:1973–80. [DOI] [PubMed] [Google Scholar]
- [32].Trinh QD, Sun M, Sammon J, et al. Disparities in access to care at high-volume institutions for uro-oncologic procedures. Cancer 2012;118:4421–6. [DOI] [PubMed] [Google Scholar]
- [33].Chan JK, Gomez SL, O’Malley CD, et al. Validity of cancer registry medicaid status against enrollment files: implications for population-based studies of cancer outcomes. Med Care 2006;44:952–5. [DOI] [PubMed] [Google Scholar]
- [34].Cress RD, Chen YS, Morris CR, et al. Underutilization of gene expression profiling for early-stage breast cancer in California. Cancer Causes Control 2016;27:721–7. [DOI] [PMC free article] [PubMed] [Google Scholar]


