Abstract
Rationale:
Ozone autohemotherapy as an alternative treatment method has been applied to the treatment of several diseases. Here, we report a patient used ozone autohemotherapy to treat her hypertension and diabetes. Nevertheless, the patient occurred sudden dizziness and black haze due to hyperkalemia.
Patient concerns:
A 54-year-old woman who was admitted to our emergency department complaining of sudden dizziness and black haze for 5 hours.
Diagnoses:
The blood potassium test showed hyperkalemia. Upon further inquiry of her medical history, the patient received ozone autohemotherapy to treat hypertension and diabetes for 9 days prior to admission.
Interventions:
The ozone therapy had been asked to stop. Insulin, sodium bicarbonate, and sodium polystyrene sulfonate were administered to the patient.
Outcomes:
After treatment, blood potassium remained in the normal range. After 3 days of treatment, the 24-hour dynamic electrocardiogram revealed sinus rhythm with an average heart rate of 82 beats/min, occasional ventricular premature beats, occasional ventricular premature beats, and no ST segment depression.
Lessons:
Although ozone therapy is widely used in the treatment of several diseases, adverse reactions should be given attention in clinical practice, especially in patients with chronic kidney disease.
Keywords: chronic kidney disease, diabetes, hyperkalemia, hypertension, ozone therapy, treatment
1. Introduction
Ozone autohemotherapy is an alternative treatment method that has been applied to the treatment of several diseases, such as diabetes and heart failure.[1,2] Although a significant effect of ozone therapy has been noted in some diseases, various adverse events have been reported, such as acute coronary syndrome.[3] Herein, we observed sinus arrest in a hypertension patient with chronic kidney disease (CKD) caused by hyperkalemia after ozone therapy. This case report was approved by the institutional review board of Anzhen Hospital.
2. Case presentation
A 54-year-old woman was admitted to our emergency department for complaints of sudden dizziness and black haze for 5 hours. She experienced a short period of unconsciousness (lasting for 2–3 seconds) with sweating. Physical examination revealed that her blood pressure (BP) was 158/76 mmHg, respiration was 28 beats/min, heart rate was 40 beats/min, and blood oxygen saturation was 98%. Arrhythmia was noted, and no other positive signs were found. The electrocardiogram revealed sinus arrest with junctional escape beat rhythm and T wave tip (Fig. 1A). The electrocardiogram revealed no obvious abnormality half a month prior to admission (Fig. 1B).
Figure 1.
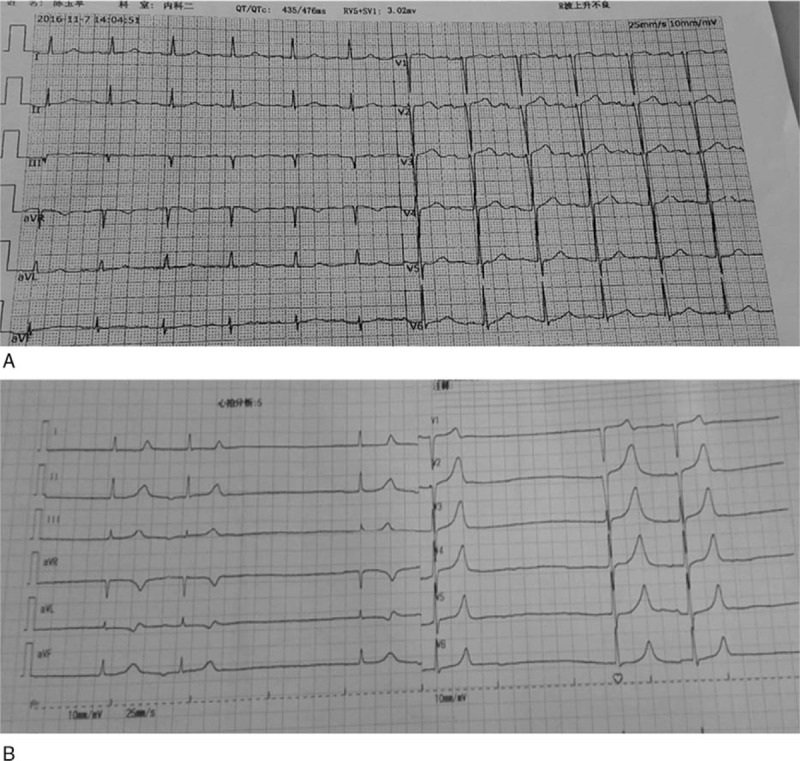
The electrocardiogram before and after admission (2016-11-07). A: before admission. B: after admission (2016-11-19).
The common cause of sinus arrest is organic heart disease, such as coronary heart disease, acute myocarditis, and cardiomyopathy. Therefore, the past history of the patient was taken, revealing a 30-year history of hypertension and 20-year history of diabetes. All the above diseases were being treated with drugs. Primary sinus arrest was excluded based on medical history and clinical examination. Because she had not taken any anti-arrhythmia drugs, the patient could be excluded from anti-arrhythmia drug overdose or poisoning, such as digitalis poisoning, which causes sinus arrest. In addition, the patient did not experience an increase in vagal tone or carotid sinus hypersensitivity, such as carotid sinus massage or trachea intubation; hence, these conditions could be excluded. However, abnormal potassium could also cause sinus arrest. The emergency blood potassium was 6.8 mmol/L, which confirmed that hyperkalemia caused sinus arrest. Hyperkalemia is mainly triggered by an excessive intake of potassium, reduced potassium excretion, and transport of intracellular k+ to the extracellular area. However, the patient had no previous history of taking drugs with potassium or history of trauma that could cause metastatic hyperkalemia by damaging tissue. Routine blood tests were normal: red blood cells (RBC), 3.67 T/L; hemoglobin, 101 g/L; hematocrit, 30%; and mean corpuscular volume, 81.7 fl. This information helped exclude that hyperkalemia was caused by intravascular hemolysis.
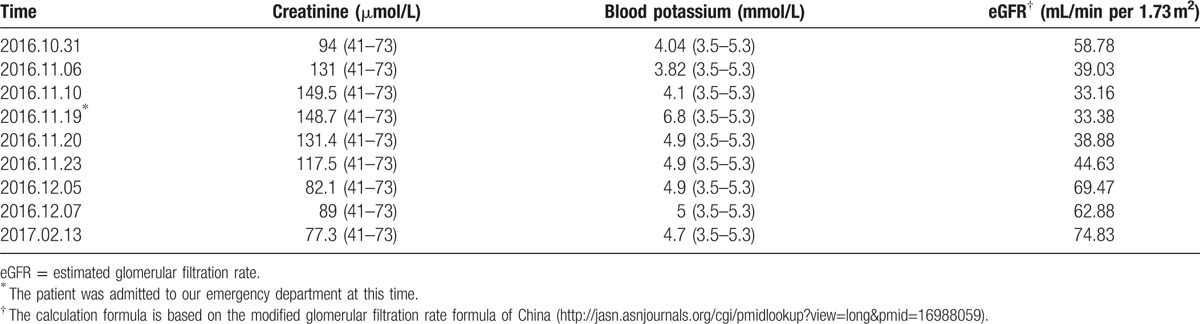
Given that CKD could result in a reduction in potassium excretion, we further discovered that this patient had been diagnosed with CKD for half a year. The laboratory tests are presented in Table 1. She did not have any clinical manifestations of acute exacerbation of CKD or acute renal insufficiency. Her creatinine rapidly increased from 94 to 131 μmol/L between October 31st and November 6th, but no difference in her potassium level was noted. However, creatinine and potassium levels were increased on November 19th when the patient was admitted to our emergency department. Upon further inquiry of her medical history, the patient received ozone autohemotherapy to treat hypertension and diabetes for 9 days prior to admission. The treatment method as described by the patient involved combining 100 mL of extracted blood with ozone (the dose was unknown) at a 1:1 ratio. Then, the combination was directly intravenously infused back to the patient. Ozone autohemotherapy is equivalent to the input of red blood cells in vitro. Ozone autohemotherapy may aggravate renal insufficiency and induce elevated serum potassium in patients with chronic renal insufficiency. Therefore, we considered that the cause of hyperkalemia was ozone therapy. Insulin, sodium bicarbonate, and sodium polystyrene sulfonate were administered to the patient. After treatment, blood potassium remained in the normal range (Table 1). After 3 days of treatment, the 24-hour dynamic electrocardiogram revealed sinus rhythm with an average heart rate of 82 beats/min, occasional ventricular premature beats, occasional ventricular premature beats, and no ST segment depression.
Table 1.
Creatinine and blood potassium levels at different times.
3. Discussion
In recent years, ozone therapy has been used in a wide variety of clinical fields. Given the potent antioxidant capacity of human plasma[4] and the use of ozone concentrations within the therapeutic range (10–80 mg/mL of gas per mL of blood or 0.21–1.68 mM per mL of blood), the use of ozone therapy during the past 3 decades has been effective with few side effects. Therefore, ozone therapy is widely used in most public hospitals in India, China, Russia, and Germany.
The main mechanisms of ozone therapy may include the following: upregulation of the synthesis of antioxidant enzymes, such as superoxide dismutase[5]; anti-inflammation by regulating the NLRP3 inflammasome, caspase-1-p10, and IL-1β[6]; and antimicrobial function. Ozone therapy is useful for decontamination of the root canal in teeth contaminated with Pseudomonas aeruginosa, Enterococcus faecalis, and Staphylococcus aureus, suggesting that ozone might have antimicrobial efficacy.[7] Hence, diseases characterized by a chronic oxidative stress or chronic inflammation might be benefited from ozone therapy.
In this case, the patient had multiple conditions: diabetes, hypertension, and CKD. Therefore, we hypothesized that this case of hyperkalemia may be associated with ozone therapy based on the following factors: the patient denied taking drugs that influenced blood potassium, and other causes of hyperkalemia were excluded; the deformability of red blood cells was badly compared with those of health people and red cells will be died easily because both diabetes and CKD reduce the deformability of red blood cells[8]; studies investigating the effects of ozone therapy on RBC flexibility, membrane, and deformability are controversial.[9] However, under complex conditions, such as diabetes plus hypertension, autohemotherapy may cause hyperkalemia according to a study showed that RBC transfusion is associated with an elevated risk of hyperkalemia and heart failure in patients with advanced CKD.[10]
Although ozone therapy is widely used in the treatment of several diseases, adverse reactions should be given attention in clinical practice, especially in patients with chronic kidney disease.
Acknowledgments
The authors thank the support of based clinical research cooperation projects, Capital Medical University (No. 16JL42) the Presidential Foundation of Beijing Anzhen Hospital Affiliated with Capital Medical University (No. 2016P01), and Youth Science Foundation Project of Jiangxi province (20171BAB215004).
Footnotes
Abbreviations: BP = blood pressure, CKD = chronic kidney disease.
W-JT and LJ are co-first authors.
The authors have no conflicts of interest to disclose.
References
- [1].Zhang J, Guan M, Xie C, et al. Increased growth factors play a role in wound healing promoted by noninvasive oxygen-ozonetherapy in diabetic patients with foot ulcers. Oxid Med Cell Longev 2014;2014:273475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Buyuklu M, Kandemir FM, Set T, et al. Beneficial effects of ozone therapy on oxidative stress, cardiac functions and clinical findings in patients with heart failure reduced ejection fraction. Cardiovasc Toxicol 2017;17:426–33. [DOI] [PubMed] [Google Scholar]
- [3].Üreyen ÇM, Baş CY, Arslan Ş. Myocardial infarction after ozone therapy: is ozone therapy Dr. Jekyll or Mr. Hyde? Cardiology 2015;132:101–4. [DOI] [PubMed] [Google Scholar]
- [4].Rice-Evans C, Miller NJ. Total antioxidant status in plasma and body fluids. Methods Enzymol 1994;234:279–93. [DOI] [PubMed] [Google Scholar]
- [5].Zanardi I, Borrelli E, Valacchi G, et al. Ozone: a multifaceted molecule with unexpected therapeutic activity. Curr Med Chem 2016;23:304–14. [DOI] [PubMed] [Google Scholar]
- [6].Yu G, Bai Z, Chen Z, et al. The NLRP3 inflammasome is a potential target of ozone therapy aiming to ease chronic renal inflammation in chronic kidney disease. Int Immunopharmacol 2017;43:203–9. [DOI] [PubMed] [Google Scholar]
- [7].Nogales CG, Ferreira MB, Montemor AF, et al. Ozone therapy as an adjuvant for endondontic protocols: microbiological - ex vivo study and citotoxicity analyses. J Appl Oral Sci 2016;24:607–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Lee S, Lee MY, Nam JS, et al. Hemorheological approach for early detection of chronic kidney disease and diabetic nephropathy in Type 2 diabetes. Diabetes Technol Ther 2015;17:808–15. [DOI] [PubMed] [Google Scholar]
- [9].Aydogan S, Artis AS. Artis AS. How ozone treatment affects erythrocytes. Hemodynamics - New Diagnostic and Therapeuric Approaches. Rijeka: InTech; 2012. 69–84. [Google Scholar]
- [10].Gill K, Fink JC, Gilbertson DT, et al. Red blood cell transfusion, hyperkalemia, and heart failure in advanced chronic kidney disease. Pharmacoepidemiol Drug Saf 2015;24:654–62. [DOI] [PubMed] [Google Scholar]


