Abstract
Background:
Both high tibial osteotomy (HTO) and unicompartmental knee arthroplasty (UKA) are well-established treatments for medial knee osteoarthritis (OA). However, it is unclear whether HTO or UKA leads to better clinical outcomes and lower complication rates. This meta-analysis compared the clinical outcomes and complications of HTO and UKA in patients with medial knee OA.
Methods:
All studies comparing the functional outcome, postoperative pain, revision rate to total knee arthroplasty (TKA), postoperative complications, postoperative velocity, and postoperative range of motion (ROM) as assessed with various measurement tools in patients with medial knee OA treated with HTO or UKA were included.
Results:
Sixteen studies were included in the meta-analysis. The proportion of patients who underwent revision to TKA (OR 1.56, 95% CI: 0.61–3.98; P = .35) did not differ significantly between HTO and UKA. In contrast, functional outcome (OR 0.47, 95% CI: 0.24 to 0.95; P = .04), postoperative pain (OR 0.28, 95% CI: 0.12 to 0.62; P = .002), postoperative complications (OR 2.48, 95% CI: 1.26 to 4.90; P = .009), postoperative velocity (95% CI: −0.11 to −0.00; P = .03), and postoperative ROM (95% CI: 2.02 to 15.23; P = .01) were significantly different between the 2 groups.
Conclusions:
There were no significant differences in the revision rate to TKA between HTO and UKA. However, results from subgroup analyses suggested that opening-wedge HTO resulted in a lower revision rate to TKA than did UKA, whereas closing-wedge HTO resulted in a higher revision rate to TKA than did UKA. In addition, UKA resulted in significantly better functional outcomes and postoperative velocity, along with less postoperative pain, fewer postoperative complications, and lower postoperative ROM. Based on the findings of current meta-analysis, UKA appears to be as efficacious and safe as HTO in the treatment of medial knee OA.
Keywords: knee, meta-analysis, osteoarthritis, osteotomy, unicompartmental
1. Introduction
The goal of treatment for medial knee osteoarthritis (OA) is to restore function, reduce pain, and improve quality of life.[1] Both high tibial osteotomy (HTO) and unicompartmental knee arthroplasty (UKA) are well-established treatments for medial knee OA, even though they are quite different procedures with different philosophies.[2] In general, HTO is appropriate for the treatment of medial knee OA with varus deformity in relatively young, active patients who accept a slight decrease in their physical activity, whereas UKA is appropriate for older, more sedentary patients who need sufficient pain relief.[3] The 2 most commonly used HTO methods, opening-wedge and closing-wedge HTO, aim to preserve the natural joint and provide reliable long-term fixation and functional improvement.[2,4] However, both methods can also lead to unfavorable results because they are technically demanding, which gives rise to several shortcomings, including the lack of precise adjustment and risks of neurologic deficit, proximal tibial bone loss, and correction loss.[5,6] In contrast, UKA is associated with preservation of bone stock, decreased blood loss, faster postoperative recovery, and decreased infection rates. Furthermore, it restores more normal joint kinematics and knee proprioception, leading to improved postoperative satisfaction and function.[7] However, there are also potential concerns with UKA: inaccurate positioning of the component without correction of misalignment can increase the risk of early implant failure and poor function.[8] To date, few studies have directly compared the clinical outcomes and complication rates of HTO and UKA in patients with medial knee OA. Newly comparative studies and 2 meta-analyses have produced inconclusive results.[3,9–12] In addition, previous meta-analyses did not simultaneously compare patients who underwent HTO versus UKA, creating subgroups grounded on HTO methods, opening-wedge and closing-wedge HTO, which may substantially affect clinical outcomes and complication rates in patients undergoing HTO or UKA. It is therefore unclear whether HTO or UKA leads to better clinical outcomes and lower complication rates.
Therefore, we performed a meta-analysis to compare the clinical outcomes and complication rates of HTO and UKA in patients with medial knee OA by evaluating the functional outcome, postoperative pain, revision rate to total knee arthroplasty (TKA), postoperative complications, postoperative velocity, and postoperative range of motion (ROM). It was hypothesized that UKA would lead to better clinical outcomes and lower complication rates than HTO in patients with medial knee OA.
2. Materials and methods
2.1. Data and literature sources
This study followed the Cochrane Review Methods and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses reporting guidelines for the meta-analysis of intervention trials. The study was registered online at PROSPERO (ID: CRD42017067766). Although the present study involved human participants, ethical approval, or informed consent from the participants was not required because all the data were based on previously published studies and analyzed anonymously without any potential harm to the participants. Multiple comprehensive databases, including MEDLINE (January 1, 1976 to June 30, 2016), EMBASE (January 1, 1985 to June 30, 2016), Web of Science (January 1, 1980 to June 30, 2016), SCOPUS (January 1, 1980 to June 30, 2016), and the Cochrane Library (January 1, 1987 to June 30, 2016) were searched for studies that compared the functional outcome, postoperative pain, postoperative velocity, postoperative ROM, revision rate to TKA, and postoperative complications after surgery in medial knee OA treated with HTO and UKA. There were no restrictions on language. Search terms used in the title, abstract, MeSH, and keywords fields included (“knee” [Mesh] OR “osteotomy” [Mesh] OR “unicompartmental” [Mesh] OR “osteoarthritis” [Mesh] OR “high tibial osteotomy” [tiab] OR “unicompartmental knee arthroplasty” [tiab]) AND “unicondylar osteoarthritis” [tiab] OR “unicompartmental osteoarthritis” [tiab] OR “opening-wedge” [tiab] OR “closing-wedge” [tiab]. After the initial electronic search, relevant articles and their bibliographies were searched manually.
2.2. Study selection
From the title and abstract, 2 reviewers independently selected the relevant studies for full review. The full text copy of the article was reviewed if the abstract did not provide enough data to make a decision. Studies were included in the meta-analysis if they assessed functional outcome, postoperative pain, postoperative velocity, postoperative ROM, revision rate to TKA, and postoperative complications after surgery in medial knee OA; reported direct comparisons of surgical outcomes in medial compartment OA through both the HTO and UKA methods; included data on at least 1 of the following 6 parameters: functional outcome, postoperative pain, postoperative velocity, postoperative ROM, revision rate to TKA, and postoperative complications. Functional outcome was based on validated knee function scores, including the British Orthopaedic Association (BOA) score, Baily knee score, Knee Society Score (KSS), Lysholm score, and Hospital for Special Surgery (HSS) knee score; we recorded the proportion of patients with excellent or good results. Postoperative pain was evaluated by recording the proportion of patients with no or mild pain using Borg CR-10 score, Baily knee score, and modified KSS. A postoperative complication was defined as an adverse event of treatment recorded by the author of the study. It included any complication that required surgical intervention in which the components were retained. Postoperative velocity was assessed by a foot-switch method using 5-, 10-, and 13-m long force platforms. Postoperative ROM was passively measured by a long goniometer; fully reported the number of subjects in each group (HTO and UKA groups) and the means and standard deviations for the 6 parameters; and used adequate statistical methods to compare these parameters between groups.
2.3. Data extraction
Two reviewers independently recorded data from each study using a predefined data extraction form. Disagreement between the reviewers was resolved by consensus or by discussion with a third investigator when consensus could not be reached. Variables recorded included those associated with surgical outcomes, such as functional outcome, postoperative pain, postoperative velocity, postoperative ROM, revision rate to TKA, and postoperative complications. Sample size and the means and standard deviations of surgical outcomes in each group were also recorded. If these variables were not included in the articles, the study authors were contacted by email to retrieve further information.
2.4. Assessment of methodological quality
Two reviewers independently assessed the methodological quality of the studies. For prospective RCTs, methodological quality was assessed with the modified Jadad scale, which assesses randomization, blinding, withdrawals and dropouts, inclusion and exclusion criteria, adverse reactions, and statistical analysis. High quality studies have scores of 4 to 8, whereas low quality studies have scores of 0 to 3.[13] For the Newcastle-Ottawa Scale,[14] as recommended by the Cochrane Non-Randomized Studies Methods Working Group, we assessed the studies based on 3 criteria: selection of the study groups, comparability of the groups, and ascertainment of either the exposure or the outcome of interest for case–control and cohort studies. Studies with scores ≥6 points were defined as high quality. Any unresolved disagreements between reviewers were resolved by consensus or by consultation with a third investigator.
2.5. Data synthesis and analysis
The main outcomes of the meta-analysis were the proportion of cases with a good or excellent functional outcome, no or mild postoperative pain, revision to TKA, postoperative complications, the weighted mean difference (WMD) in postoperative velocity, and postoperative ROM. For all comparisons, odds ratios (ORs) and 95% confidence intervals (CIs) were calculated for binary outcomes, while WMD and 95% CI were calculated for continuous outcomes. Heterogeneity was determined by estimating the proportion of between-study inconsistencies due to actual differences between studies, rather than differences due to random error or chance, using the I2 statistic, with values of 25%, 50%, and 75% considered low, moderate, and high heterogeneity, respectively. All statistical analyses were performed with RevMan version 5.2 software. Subgroup analysis was performed only for the revision rate to TKA to explore a potential source of heterogeneity. As a result, 2 subgroups were created: opening-wedge HTO and closing-wedge HTO.
3. Results
3.1. Identification of studies
The details on study identification, inclusion, and exclusion are summarized in Fig. 1. An electronic search yielded 435 studies in PubMed (MEDLINE), 381 in EMBASE, 145 in Web of science, 412 in SCOPUS, and 25 in the Cochrane Library. Two additional publications were identified through manual searching. After removing 506 duplicates, 894 studies remained; of these, 866 were excluded based on reading the abstracts and full-text articles, and an additional 12 studies were excluded because they had unusable information or made inappropriate group comparisons. This eventually resulted in 16 studies that were included in the meta-analysis.[10–12,15–27]
Figure 1.
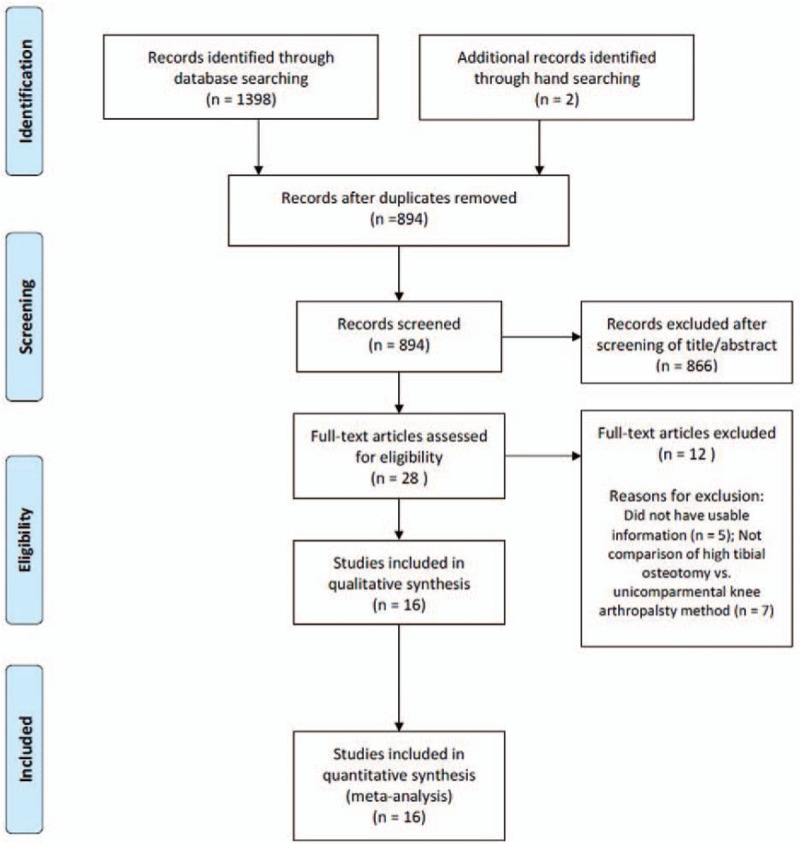
Preferred reporting items for systemic reviews and meta-analyses (PRISMA) flow diagram of literature selection.
3.2. Study characteristics, patient populations, and quality assessment of the included studies
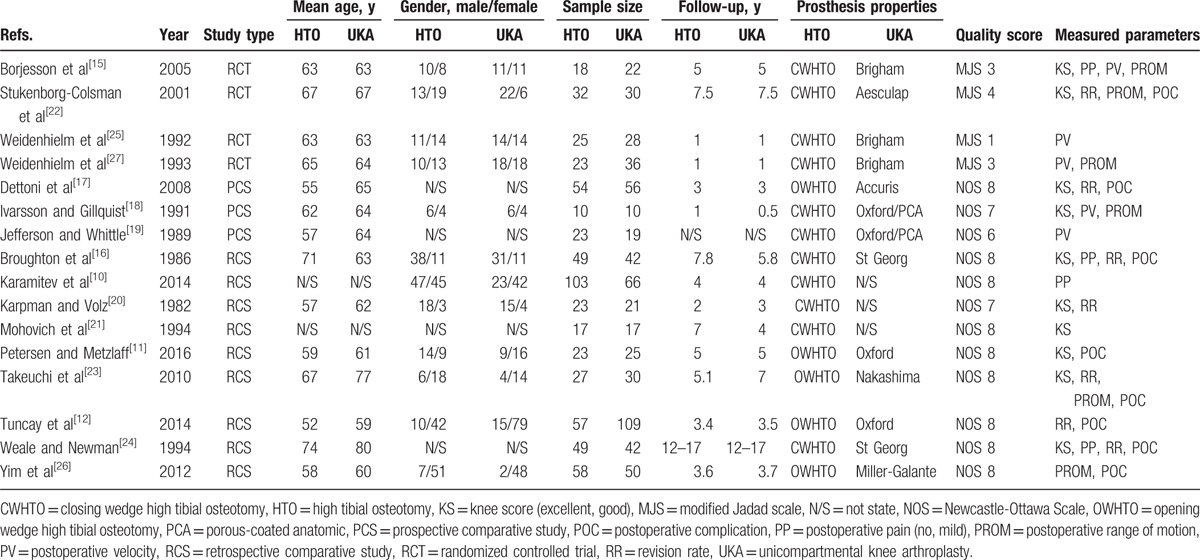
The 16 studies we examined included 591 subjects who underwent surgical treatment for medial knee OA with the HTO method and 603 subjects who underwent surgical treatment for medial knee OA with the UKA method. Six studies (4 RCT and 2 PCS) compared prospectively measured parameters, whereas the other 10 studies compared parameters measured by retrospective chart review. Ten studies compared the functional outcome, 8 compared postoperative complications, 7 compared the revision rate to TKA, 6 compared postoperative ROM, and 4 compared postoperative pain and postoperative velocity (Table 1). The quality of the 16 studies included in the meta-analysis is summarized in Table 1. There was 1 RCT of high quality (modified Jadad scale > 4) and 3 RCTs of low quality (modified Jadad scale < 3). The non-RCTs (3 PCSs and 9 RCSs) were of high quality (Newcastle-Ottawa Scale > 6).
Table 1.
Summary of patient characteristics of the included studies.
3.3. Functional outcome and postoperative pain, velocity, and ROM
Of the 16 studies, 10 compared the functional outcome between the 2 methods, involving 302 subjects treated with HTO and 295 treated with UKA. The proportion of subjects with a good or excellent functional outcome was significantly greater with UKA (250/302) than HTO (223/302; OR 0.47, 95% CI: 0.24–0.95; P = .04; I2 = 46%, Fig. 2). Four studies presented data on postoperative pain. The proportion of subjects with no or mild postoperative pain was significantly greater with UKA (132/172) than (HTO, 134/219; OR 0.28, 95% CI: 0.12–0.62; P = .002; I2 = 37%, Fig. 3). Four studies reported the postoperative velocity and included 76 subjects treated with HTO and 96 treated with UKA. The pooled data showed that mean postoperative velocity was −0.05 m/s faster with UKA than HTO and was significantly different between groups (95% CI: −0.11 to −0.00 m/s; P = .03; I2 = 0%, Fig. 4). Six studies compared postoperative ROM between the 2 methods, involving 168 subjects treated with HTO and 190 treated with UKA. The pooled data showed that mean postoperative ROM was 8.62 degrees (95% CI: 2.02–15.23°; P = .01; I2 = 96%, Fig. 5), indicating that postoperative ROM was significantly greater with HTO than UKA.
Figure 2.
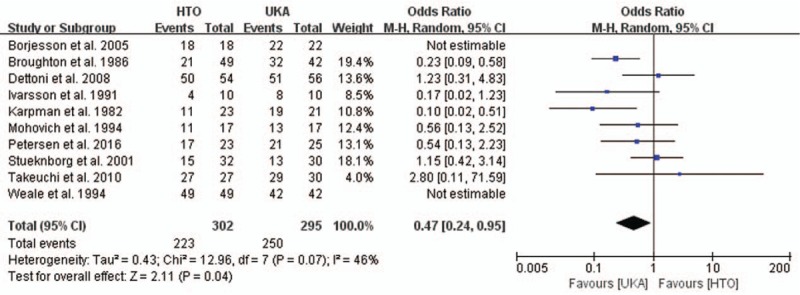
Results of aggregate analysis for comparison of functional outcome according to different surgical methods. HTO = high tibial osteotomy, UKA = unicompartmental knee arthroplasty.
Figure 3.
Results of aggregate analysis for comparison of postoperative pain according to different surgical methods. HTO = high tibial osteotomy, UKA = unicompartmental knee arthroplasty.
Figure 4.
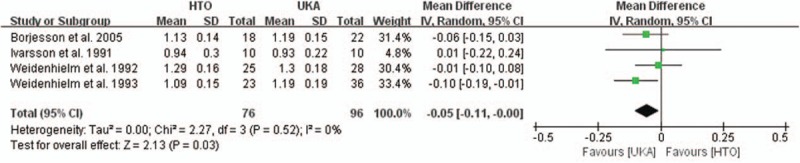
Results of aggregate analysis for comparison of postoperative velocity according to different surgical methods. HTO = high tibial osteotomy, UKA = unicompartmental knee arthroplasty.
Figure 5.
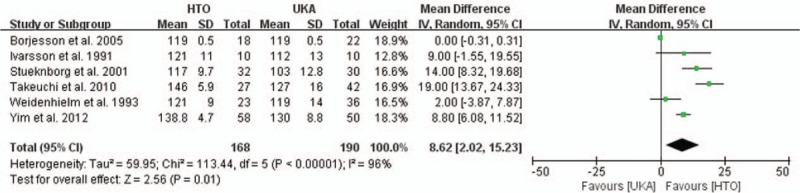
Results of aggregate analysis for comparison of postoperative range of motion according to different surgical methods. HTO = high tibial osteotomy, UKA = unicompartmental knee arthroplasty.
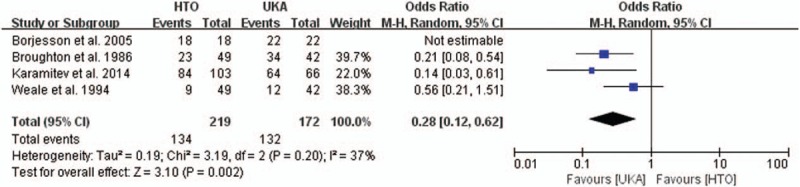
3.4. Revision rate to TKA and postoperative complications
Of the 16 studies, 7 reported the revision rate to TKA and included 291 patients treated with HTO and 330 treated with UKA. The proportion of patients requiring revision to TKA did not differ significantly between HTO (37/291) and UKA (21/330, OR 1.56, 95% CI: 0.61–3.98; P = .35; I2 = 41%, Fig. 6). Four studies reported results for closing-wedge HTO, and 3 reported results for opening-wedge HTO. In subgroup analysis, opening-wedge HTO had a lower revision rate to TKA than did UKA, although this difference was not statistically significant (HTO, 0/138; UKA, 5/195, OR 0.24, 95% CI: 0.03–2.00; P = .19; I2 = 0%, Fig. 6). In contrast, closing-wedge HTO had a significantly higher revision rate to TKA than did UKA (HTO, 37/153; UKA, 16/135, OR 2.38, 95% CI: 1.05–5.42; P = .04; I2 = 26%, Fig. 6). Eight studies presented data on the proportion of subjects who developed postoperative complications, with significant difference between treatments, indicating that HTO had a significantly higher complication rate than did UKA (HTO, 49/349; UKA, 20/384; OR 2.48, 95% CI: 1.26–4.90; P = .009; I2 = 17%, Fig. 7).
Figure 6.
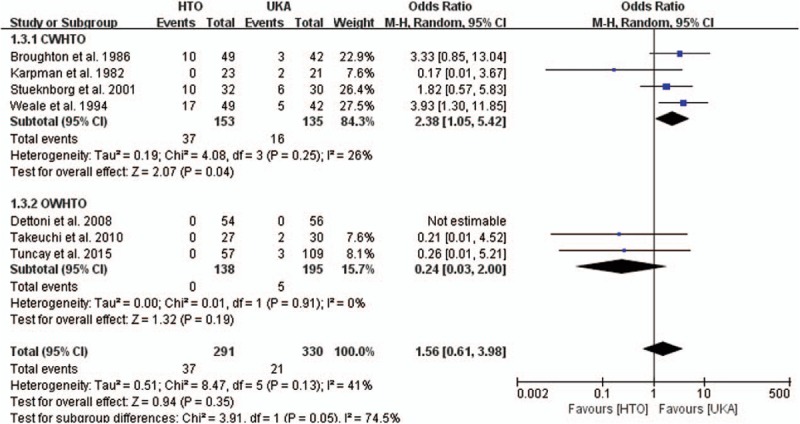
Results of aggregate analysis for comparison of revision to total knee arthroplasty according to different surgical methods, including subgroup analysis by CWHTO and OWHTO. CWHTO = closing-wedge high tibial osteotomy, HTO = high tibial osteotomy, OWHTO = opening-wedge high tibial osteotomy, UKA = unicompartmental knee arthroplasty.
Figure 7.
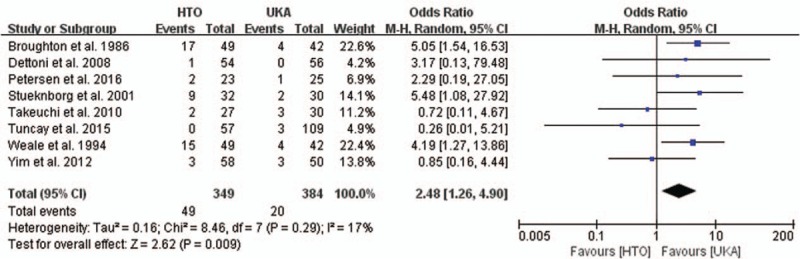
Results of aggregate analysis for comparison of postoperative complications according to different surgical methods. HTO = high tibial osteotomy, UKA = unicompartmental knee arthroplasty.
4. Discussion
The most important finding of this meta-analysis was that the revision rate to TKA did not differ significantly between the 2 treatment methods, HTO and UKA, for medial knee OA. However, subgroup analysis revealed that opening-wedge HTO resulted in a lower revision rate to TKA than did UKA, whereas closing-wedge HTO resulted in a significantly higher revision rate to TKA than did UKA. In addition, UKA resulted in better outcomes than HTO in terms of the functional outcome, postoperative velocity, postoperative pain, and postoperative complications, however postoperative ROM was lower.
A recent study comparing clinical outcomes between UKA and HTO with a follow-up of 4 years showed that UKA leads to rapid functional recovery of the knee joint and is thus a reasonable alternative to HTO in the treatment of medial knee OA.[10] Unfortunately, not all patients who undergo UKA experience excellent clinical outcomes, despite improved surgical techniques and modern prosthetic designs. A combination of factors, such as inappropriate patient selection and technical errors in alignment among surgeons performing a lower volume of UKAs, may explain poor clinical outcomes of UKA.[28,29] However, the current meta-analysis found a significantly better functional outcome with UKA than HTO. It is possible that technical errors with UKA are not that common because methods have been developed to achieve slight undercorrection of varus alignment and adequate polyethylene thickness.[26,30] In addition, HTO may lead to greater progression of medial knee OA than UKA after 10 years, even with accurate correction.[31,32]
Our meta-analysis also revealed that patients walked more slowly and had more pain postoperatively with the HTO method than the UKA method, even though patients who had UKA were slightly older and had more severe OA according to the Ahlback's classification. The HTO method requires a long-leg cast for 6 weeks or longer during recovery, which may contribute to more postoperative pain and slower restoration of the extensor mechanism.[33,34] However, it is also possible that the faster walking speed with UKA is explained by careful patient selection that excluded patients with problems in the contralateral knee apart from their operated knee and those with minor progression of OA, including development of subchondral sclerosis and osteophytes with no clinical importance.[35,36] Therefore, postoperative walking speed may not always be related to age or stage of OA, and may often be faster than when compared with individual factors. Rather, an improved postoperative rehabilitation program is needed to achieve better postoperative walking speed.[23] Indeed, a recent study found that UKA increases maximal walking speed and single stance phase 6 months postoperatively compared to HTO.[18]
Despite the functional advantages of UKA, this meta-analysis found that UKA was associated with less postoperative ROM than was HTO. Patients treated with HTO may have had better ROM because HTO allowed patients to maintain a higher level of activity without potential wear of arthroplasty components.[11] These results are consistent with those of Stukenborg-Colsman et al,[22] who evaluated 32 knees after HTO and 30 knees after UKA and found that the average ROM at 7.5 years postoperatively was greater with HTO than UKA.
Many studies have reported that polyethylene wear, loosening of components, and progression of OA with UKA lead to higher revision rates to TKA. Revision to TKA is also associated with increased bone loss management and inferior results compared to primary TKA.[37] However, a study evaluating 39 consecutive patients with TKA after failed UKA found that bone loss on the tibial side was not surgically challenging, and good-to-excellent results were obtained in all patients after 24 to 120 months of follow-up.[38] Previous studies investigating exposure difficulties and alterations in knee anatomy after failed HTO have reported early failure within 5 years of primary arthroplasty because of the loss of metaphyseal bone stock and the use of a revision tibial component with a canal-filling stem, which prevents accurate placement of the tibial component.[39,40] However, another study found no difference in long-term results between TKA after failed HTO and primary TKA.[41] Our meta-analysis revealed no significant difference between HTO and UKA in the revision rate to TKA. However, results from subgroup analysis found that opening-wedge HTO was associated with a lower revision rate to TKA than was UKA, but closing-wedge HTO was associated with a higher revision rate to TKA than was UKA. There are 3 possible explanations for these findings. First, compared to UKA, HTO is performed in younger patients who want a higher level of activity, which can accelerate the progression of OA in other compartments. Second, opening wedge HTO has minimal risk of bone loss, no risk of patellar alta, and no risk of impingement between the tibial stem and anterior tibial cortex; in addition, this technique uses angular stable locking plates that diminish the risk of nonunion and correction loss and promote rapid bone healing. In contrast, closing-wedge HTO with the traditional technique involves wide dissection of the lateral soft tissue and fibular osteotomy.[2,42] Third, indications for UKA are expanding to include younger and more active patients. This could contribute to greater prosthesis wear and failure and poorer survival outcomes.[43] Based on the best evidence now available, it appears that surgeons may select UKA in patients who need sufficient pain relief and faster recovery in their physical activity for the treatment of medial knee OA with indications for both HTO and UKA, as there do appear to be substantial or obvious differences between the 2 procedures with respect to functional outcome or postoperative pain, velocity, complications.
This study had several limitations. Of the 16 studies, 12 were observational, resulting in some inherent heterogeneity due to uncontrolled bias, even though the studies had high quality scores. In addition, the heterogeneity of the included studies could be explained by slight differences in other factors affecting clinical outcomes, including the use of a wide variety of fixation devices and variability in functional and pain scores. Finally, we did not perform subgroup analysis for the different bearing designs, including mobile and fixed designs, in UKA because we did not find a significant difference in the mid-term survival rate between the 2 designs.[44,45]
5. Conclusion
In summary, there were no significant differences in the revision rate to TKA between HTO and UKA. However, results from subgroup analysis revealed that opening-wedge HTO had a lower revision rate to TKA than did UKA, but closing-wedge HTO had a significantly higher revision rate to TKA than did UKA. In addition, UKA led to significantly better results than HTO in terms of the functional outcome, postoperative velocity, postoperative pain, and postoperative complications, however postoperative ROM was lower. Based on the findings of current meta-analysis, UKA appears to be as efficacious and safe as HTO in the treatment of medial knee OA.
Footnotes
Abbreviations: CI = confidence interval, HTO = high tibial osteotomy, OA = osteoarthritis, OR = odds ratio, ROM = range of motion, TKA = total knee arthroplasty, UKA = unicompartmental knee arthroplasty.
Research of this study was performed at Veterans Health Service Medical Center.
S-BH, H-SK contributed equally to this work.
The authors have no conflicts of interest to disclose.
References
- [1].Amin AK, Patton JT, Cook RE, et al. Unicompartmental or total knee arthroplasty?: Results from a matched study. Clin Orthop Relat Res 2006;451:101–6. [DOI] [PubMed] [Google Scholar]
- [2].Dettoni F, Bonasia DE, Castoldi F, et al. High tibial osteotomy versus unicompartmental knee arthroplasty for medial compartmentarthrosis of the knee: a review of the literature. Iowa Orthop J 2010;30:131–40. [PMC free article] [PubMed] [Google Scholar]
- [3].Spahn G, Hofmann GO, von Engelhardt LV, et al. The impact of a high tibial valgus osteotomy and unicondylar medial arthroplasty on the treatment for knee osteoarthritis: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 2013;21:96–112. [DOI] [PubMed] [Google Scholar]
- [4].Kyung HS. High tibial osteotomy for medial knee osteoarthritis. Knee Surg Relat Res 2016;28:253–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Parker DA, Viskontas DG. Osteotomy for the early varus arthritic knee. Sports Med Arthrosc 2007;15:3–14. [DOI] [PubMed] [Google Scholar]
- [6].Staubli AE, De Simoni C, Babst R, et al. TomoFix: a new LCP-concept for open wedge osteotomy of the medial proximal tibia-early results in 92 cases. Injury 2003;34:55–62. [DOI] [PubMed] [Google Scholar]
- [7].Engh GA. Orthopaedic crossfire®—can we justify unicondylar arthroplasty as a temporizing procedure? In the affirmative. J Arthroplasty 2002;17:54–5. [DOI] [PubMed] [Google Scholar]
- [8].Ko YB, Gujarathi MR, Oh KJ. Outcome of unicompartmental knee arthroplasty: a systematic review of comparative studies between fixed and mobile bearings focusing on complications. Knee Surg Relat Res 2015;27:141–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Fu D, Li G, Chen K, et al. Comparison of high tibial osteotomy and unicompartmental knee arthroplasty in the treatment of unicompartmental osteoarthritis: a meta-analysis. J Arthroplasty 2013;28:759–65. [DOI] [PubMed] [Google Scholar]
- [10].Karamitev SS, Stavrev VP, Chifligarov AG. Comparative analysis of the results obtained after unicondylar knee arthroplasty and high tibial osteotomy in isolated gonarthrosis. Folia Med 2014;56:11–9. [DOI] [PubMed] [Google Scholar]
- [11].Petersen W, Metzlaff S. Open wedge high tibial osteotomy (HTO) versus mobile bearing unicondylar medial joint replacement: five years results. Arch Orthop Trauma Surg 2016;136:983–9. [DOI] [PubMed] [Google Scholar]
- [12].Tuncay İ, Bilsel K, Elmadağ M, et al. Evaluation of mobile bearing unicompartmental knee arthroplasty, opening wedge, and dome-type high tibial osteotomies for knee arthritis. Acta Orthop Traumatol Turc 2014;49:280–7. [DOI] [PubMed] [Google Scholar]
- [13].Griffin D, Parsons N, Shaw E, et al. Operative versus non-operative treatment for closed, displaced, intra-articular fractures of the calcaneus: randomised controlled trial. BMJ 2014;349:g4483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Wells GA, Shea B, O’connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2016;Available at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed Jul 1, 2016. [Google Scholar]
- [15].Borjesson M, Weidenhielm L, Mattsson E, et al. Gait and clinical measurements in patients with knee osteoarthritis after surgery: a prospective 5-year follow-up study. Knee 2005;12:121–7. [DOI] [PubMed] [Google Scholar]
- [16].Broughton NS, Newman JH, Baily RA. Unicompartmental replacement and high tibial osteotomy for osteoarthritis of the knee. A comparative study after 5–10 years’ follow-up. J Bone Joint Surg Br 1986;68:447–52. [DOI] [PubMed] [Google Scholar]
- [17].Dettoni F, Maistrelli GL, Rossi P, et al. UKA versus HTO: clinical results at short term follow up. 2008;75th AAOS Annual Meeting, San Francisco, CA. [Google Scholar]
- [18].Ivarsson I, Gillquist J. Rehabilitation after high tibial osteotomy and unicompartmental arthroplasty. A comparative study. Clin Orthop Relat Res 1991;266:139–44. [PubMed] [Google Scholar]
- [19].Jefferson R, Whittle M. Biomechanical assessment of unicompartmental knee arthroplasty, total condylar arthroplasty and tibial osteotom. Clin Biomech 1989;4:232–42. [Google Scholar]
- [20].Karpman RR, Volz RG. Osteotomy versus unicompartmental prosthetic replacement in the treatment of unicompartmental arthritis of the knee. Orthopedics 1982;5:989–91. [DOI] [PubMed] [Google Scholar]
- [21].Mohovich H, Sciaccaluga M, Cavallera S, et al. [Medial arthrosis of the knee. Comments regarding surgical treatment]. Minerva Ortop Traumatol 1994;45:65–8. (In Italian). [Google Scholar]
- [22].Stukenborg-Colsman C, Wirth C, Lazovic D, et al. High tibial osteotomy versus unicompartmental joint replacement in unicompartmental knee joint osteoarthritis: 7-10-year follow-up prospective randomised study. Knee 2001;8:187–94. [DOI] [PubMed] [Google Scholar]
- [23].Takeuchi R, Umemoto Y, Aratake M, et al. A mid term comparison of openwedge high tibial osteotomy vs unicompartmental knee arthroplasty for medial compartment osteoarthritis of the knee. J Orthop Surg Res 2010;5:65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Weale AE, Newman JH. Unicompartmental arthroplasty and high tibial osteotomy for osteoarthrosis of the knee. A comparative study with a 12- to 17-year follow-up period. Clin Orthop Relat Res 1994;302:134–7. [PubMed] [Google Scholar]
- [25].Weidenhielm L, Svensson O, Broström LÅ, et al. Change in adduction moment about the knee after high tibial osteotomy and prosthetic replacement in osteoarthrosis of the knee. Clin Biomech 1992;7:91–6. [DOI] [PubMed] [Google Scholar]
- [26].Yim JH, Song EK, Seo HY, et al. Comparison of high tibial osteotomy and unicompartmental knee arthroplasty at a minimum follow-up of 3years. J Arthroplasty 2013;28:243–7. [DOI] [PubMed] [Google Scholar]
- [27].Weidenhielm L, Olsson E, Broström L, et al. Improvement in gait one year after surgery for knee osteoarthrosis: a comparison between high tibial osteotomy and prosthetic replacement in a prospective randomized study. Scand J Rehabil Med 1993;25:25–31. [PubMed] [Google Scholar]
- [28].Griffin T, Rowden N, Morgan D, et al. Unicompartmental knee arthroplasty for the treatment of unicompartmental osteoarthritis: a systematic study. ANZ J Surg 2007;77:214–21. [DOI] [PubMed] [Google Scholar]
- [29].Robertsson O, Knutson K, Lewold S, et al. The routine of surgical management reduces failure after unicompartmental knee arthroplasty. J Bone Joint Surg Br 2001;83:45–9. [DOI] [PubMed] [Google Scholar]
- [30].Cartier P, Sanouiller JL, Grelsamer RP. Unicompartmental knee arthroplasty surgery. 10-year minimum follow-up period. J Arthroplasty 1996;11:782–8. [DOI] [PubMed] [Google Scholar]
- [31].Flecher X, Parratte S, Aubaniac JM, et al. A 12-28-year followup study of closing wedge high tibial osteotomy. Clin Orthop Relat Res 2006;452:91–6. [DOI] [PubMed] [Google Scholar]
- [32].Stuart MJ, Grace JN, Ilstrup DM, et al. Late recurrence of varus deformity after proximal tibial osteotomy. Clin Orthop Relat Res 1990;260:61–5. [PubMed] [Google Scholar]
- [33].Andriacchi TP, Galante JO, Fermier RW. The influence of total knee-replacement design on walking and stair-climbing. J Bone Joint Surg Am 1982;64:1328–35. [PubMed] [Google Scholar]
- [34].Weinstein JN, Andriacchi TP, Galante J. Factors influencing walking and stair climbing following unicompartmental knee arthroplasty. J Arthroplasty 1986;1:109–15. [DOI] [PubMed] [Google Scholar]
- [35].Goodfellow JW, Kershaw CJ, Benson MK, et al. The Oxford Knee for unicompartmental osteoarthritis. The first 103 cases. J Bone Joint Surg Br 1988;70:692–701. [DOI] [PubMed] [Google Scholar]
- [36].Hannan MT, Felson DT, Pincus T. Analysis of the discordance between radiographic changes and knee pain in osteoarthritis of the knee. J Rheumatol 2000;27:1513–7. [PubMed] [Google Scholar]
- [37].Padgett DE, Stern SH, Insall JN. Revision total knee arthroplasty for failed unicompartmental replacement. J Bone Joint Surg Am 1991;73:186–90. [PubMed] [Google Scholar]
- [38].McAuley JP, Engh GA, Ammeen DJ. Revision of failed unicompartmental knee arthroplasty. Clin Orthop Relat Res 2001;392:279–82. [DOI] [PubMed] [Google Scholar]
- [39].Callaghan JJ, O’Rourke MR, Saleh KJ. Why knees fail: lessons learned. J Arthroplasty 2004;19:31–4. [DOI] [PubMed] [Google Scholar]
- [40].Conditt MA, Parsley BS, Alexander JW, et al. The optimal strategy for stable tibial fixation in revision total knee arthroplasty. J Arthroplasty 2004;19:113–8. [DOI] [PubMed] [Google Scholar]
- [41].van Raaij TM, Reijman M, Furlan AD, et al. Total knee arthroplasty after high tibial osteotomy. A systematic review. BMC Musculoskelet Disord 2009;10:88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Coventry MB, Ilstrup DM, Wallrichs SL. Proximal tibial osteotomy. A critical long-term study of eighty-seven cases. J Bone Joint Surg Am 1993;75:196–201. [DOI] [PubMed] [Google Scholar]
- [43].Vince KG, Cyran LT. Unicompartmental knee arthroplasty: new indications, more complications? J Arthroplasty 2004;19:9–16. [DOI] [PubMed] [Google Scholar]
- [44].Akizuki S, Mueller JK, Horiuchi H, et al. In vivo determination of kinematics for subjects having a Zimmer Unicompartmental High Flex Knee System. J Arthroplasty 2009;24:963–71. [DOI] [PubMed] [Google Scholar]
- [45].Whittaker JP, Naudie DD, McAuley JP, et al. Does bearing design influence midterm survivorship of unicompartmental arthroplasty? Clin Orthop Relat Res 2010;468:73–81. [DOI] [PMC free article] [PubMed] [Google Scholar]


