Abstract
Rationale:
Contact lens storage cases are known to be contaminated by a significant number of bacteria. However, histamine-producing Raoultella species has not been reported to contaminate contact lens storage case.
Patient concerns:
A 27-year-old woman with keratoconjunctivitis that developed in the left eye owing to a cosmetic contact lens and poor hygiene was referred to our hospital. The corrected visual acuity was hand motion.
Diagnoses:
Corneal infection other than Acanthamoeba keratitis (AK) and corneal hypoxia were excluded.
Interventions:
We initiated empirical therapy for AK, although no cysts or trophozoites were detected in the cornea and in the lens care solution. Analysis of 16S rDNA sequences from the lens care solution yielded the highest homology with Raoultella species, which are histamine-producing bacteria. Histamine was estimated to be 492 ng/mL in the lens care solution.
Outcomes:
Her clinical course was distinct from that of usual AK cases. The corrected visual acuity increased up to (1.2) only 5 days after initiating empirical therapy.
Lessons:
To our knowledge, this is the first report to indicate an association between histamine-producing bacteria and keratoconjunctivitis. We should pay an attention to the microbial contamination of contact lens storage cases by histamine producing bacteria.
Keywords: contact lenses, histamine, keratocunjunctivitis, Raoultella
1. Introduction
The early stages of Acanthamoeba keratitis (AK), significantly associated with wearing contact lenses, are characterized by various morphological corneal manifestations, such as epithelial micro-erosions, irregularities, opacities, microcystic edema, infiltration, pseudodendritica, and radial keratineuritis.[1] Treatment duration is generally lasting months.[2] Corneal hypoxia is a noninflammatory corneal complication caused by the extended contact lens wear and is characterized by corneal edema, infiltrative keratitis, and neovascularization.[3] It has been reported to recover several hours after removing contact lens.[3]
Herein, we report the case of a 27-year-old woman with acute keratoconjunctivitis caused by wearing contact lenses, the slit-lamp microscopy findings of which resembled both the early stage of AK and corneal hypoxia. This case indicates a novel etiology for an adverse event involving bacterial contamination of the storage case of contact lenses.
2. Case report
A 27-year-old woman was referred to our institution with complaints of severe eye pain and decreased visual acuity in the left eye. She had been wearing a cosmetic contact lens for 8 years with poor hygiene. A primary practitioner diagnosed her with fungal keratitis; however, antifungal therapy was not effective. The corrected visual acuity was (1.0) in the right eye and hand motion in the left eye. Intraocular pressure was normal in the right eye and unmeasurable in the left eye because of pain. Slit-lamp microscope revealed diffuse corneal epithelium infiltration, neovascularization, and severe limbitis in the left eye (Fig. 1A). Contact-lens-induced hypoxia was excluded because the patient had already stopped wearing the lens 7 days before her visit to our hospital. Contact-lens-related AK was suspected because the clinical findings resembled those of early-stage AK and the possibility of developing other corneal infections was negligible. To make a rigorous diagnosis and treat her left cornea, roughly 80% of the corneal epithelium was scraped; stained with Gram, Giemsa, and Fungi flora Y staining reagents; and inoculated on several agars. For empirical AK therapy, voriconazole 1.0% eye drops and chlorhexidine 0.04% eye drops were administered hourly in the left eye, and pimaricin ointment 1.0% was administered 4 times daily. Two days after the initiation of treatment, the clinical findings and subjective symptoms were dramatically improved. The visual acuity in the left eye recovered to (1.0) 5 days after the treatment (Fig. 1B).
Figure 1.
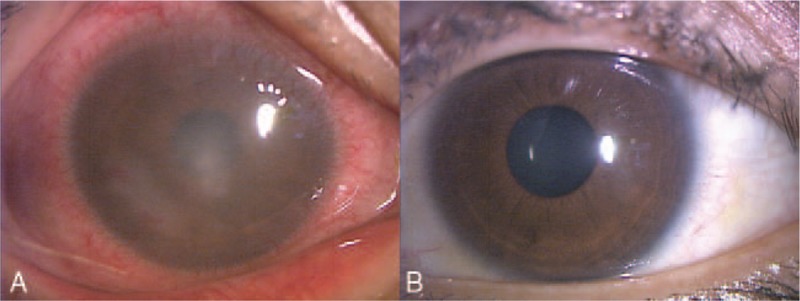
(A) The anterior segment of the eye at the first visit. Inflammation of the conjunctiva and severe corneal opacity were observed. (B) The anterior segment of the eye after treatment. Inflammation of the conjunctiva and corneal opacity disappeared.
2.1. Microbial contamination of the lens storage case
To detect Acanthamoeba cysts or trophozoites, corneal scrapings and solutions in the contact lens storage case were prepared for microscopic examination and were cultivated both on non-nutrient agar (Bacto agar; BD) plates with liquid yeast extract plus glucose and in peptone yeast glucose liquid agar. However, no cysts or trophozites were detected by microscopic examination. Moreover, no cysts or trophozites were detected after cultivations for more than 2 weeks, with examination of all agar plates each day by phase-contrast microscopy. With respect to bacterial contamination of the case, we performed a 16S rDNA clone library analysis with DNA extracted from the solutions the of patient's contact lens storage case under the approval from ethics committee of Kindai University (approval number: 28–138). A BLAST search of high quality 16S rDNA sequences obtained from the 27 clones demonstrated that the patient's contact lens storage case was contaminated with diverse bacteria that included Streptococcus, Rothia, and Staphylococcus species (Fig. 2A). We found 2 16S rDNA sequences that showed the best homology to Raoultella species (Raoultella ornithinolytica and Raoultella planicola). Because these Raoultella species are well-known histamine producers responsible for histamine food poisoning, the histamine level in the patient's contact lens storage cases was quantified using high performance liquid chromatography. As shown in Figure 2B–D, the peak corresponding to histamine was detected and its level was quantified as 492 ng/mL.
Figure 2.
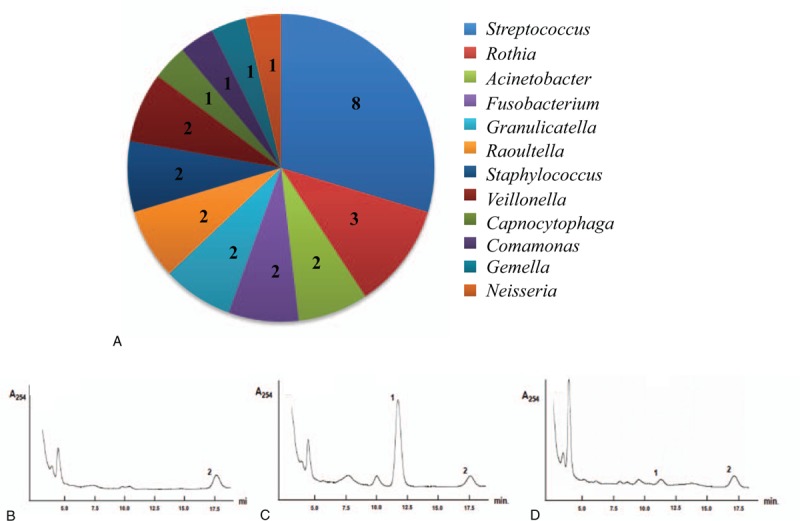
(A) Relative abundance of bacterial taxa detected in contact lens residual liquid in the storage case used by a patient with acute conjunctivitis. The number of reads obtained in 16S rDNA clone library analysis (total 27 reads), which showed the best match to the respective bacterial genera is indicated. (B–D) Chromatograms of histamine in the mobile phase without sample (B), 8 mg/mL histamine standard solution (C), and contact lens care solution used by the current patient 492 ng/mL (D). The peak histamine level in the contaminated lens care solution is displayed as peak 1 in (D). Peak identification: 1 denotes histamine dihydrochloride, 2 denotes 1,7-diaminoheptane.
3. Discussion
Interestingly, in this study, we detected histamine-producing bacteria in the contact lens storage case of a lens wearer with acute keratocunjunctivitis. Raoultella species have been identified as one of the main bacteria responsible for scombroid fish poisoning.[4–6] Fish poisoning is thought to be a symptom caused by histamines. In the current case, we could not isolate a strain of Raoultella possibly because of the disinfectant activity of multi-purpose solutions in the storage case. However, histamine, probably produced by Raoultella species, was accumulated in the contact lens solution. Histamine is known to be biologically active even when the bacteria are killed by heating or freezing.[4,7] Indeed, the level of histamine in the patient's storage case solution was very high (492 ng/mL).
Mean values of histamine levels in the tears of patients with allergic eye diseases have been reported previously. Abelson et al[8,9] reported histamine levels of 10.3 or 5 ng/mL in normal subjects and 38.2 or 16 ng/mL in subjects with vernal keratoconjunctivitis. Allansmith et al[10] reported 7 ng/mL histamine in a soft-contact-lens wearer with giant papillary hypertrophy of the upper tarsal conjunctiva (GPC) and 2 ng/mL histamine in a hard contact lens wearer with GPC. Uchio et al[11] have reported histamine values of 354 pg/mL in individuals with atopic keratoconjunctivitis, and Leonardi et al[12] reported histamine values of 1.1 ng/mL in patients who suffered from seasonal grass pollen allergic conjunctivitis. The current patient self-reported that she had worn the same cosmetic contact lens stored in the same storage case with poor hygiene for several years. Therefore, we presume that repeated exposure of the eye to histamine-contaminated solutions increased the histamine level of this patient's tears to much higher than 492 ng/mL. Although it is unknown whether the high level of histamine in the tears was the cause of the inflammatory eye disease or the result of it, high concentrations of histamine in the solutions of contact lens storage cases may breaks down the barrier integrity of corneal epithelial cells, as reported by Guo et al[13], leading to acute keratoconjunctivitis. Contact lens storage cases are known to be contaminated by a significant number of gram-negative rods, including Klebsiella species.[14] Given that in 2001, several species of Klebsiella were renamed Raoultella,[15] we believe this case substantiates the possibility of a new etiology of bacterial contamination-induced allergic responses in contact-lens wearers. In this case, we initially suspected AK, but neither its cysts nor trophozoites were detected in the patient's sample. Repeated exposure to high-level histamine might be a cause of this eye inflammation.
In conclusions, we reported the first case of acute keratoconjunctivitis in a contact-lens wearer whose lens care solution contained high levels of histamine, probably derived from Raoultella species. Given that histamine is an inflammatory mediator, the rigorous detection of bacteria contaminating contact lens storage cases might help understand the pathological role of bacteria-derived histamine in keratoconjunctivitis related to contact lens use in the future.
Footnotes
Abbreviations: AK = acanthamoeba keratitis, GPC = giant papillary hypertrophy of the upper tarsal conjunctiva.
Funding: Funding for the present work was received from Pfizer Japan Inc, Daiichi, Sankyo Co Ltd, and Novartis Pharma K. K. HE has received grant funding from Pfizer Japan Inc. YS has received grant funding from Pfizer Japan Inc and Daiichi Sankyo Co Ltd. The other authors have no funding to disclose.
The authors have no conflicts of interest to disclose.
References
- [1].Ueki N, Eguchi H, Oogi Y, et al. Three cases of Acanthamoeba keratitis diagnosed and treated in the early stage. J Med Invest 2009;56:166–9. [DOI] [PubMed] [Google Scholar]
- [2].Oidenburg CE, Keenan JD, Cevallos V, et al. Microbiological cure times in acanthamoeba keratitis. Eye (Lond) 2011;25:1155–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Polse KA, Holden BA, Sweeney D. Corneal edema accompanying aphakic extended lens wear. Arch Ophthalmol 1983;101:1038–41. [DOI] [PubMed] [Google Scholar]
- [4].Kanki M, Yoda T, Tsukamoto T, et al. Klebsiella pneumoniae produces no histamine: Raoultella planticola and Raoultella ornithinolytica strains are histamine producers. Appl Environ Microbiol 2002;68:3462–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Ferrario C, Pegollo C, Ricci G, et al. PCR detection and identification of histamine-forming bacteria in filleted tuna fish samples. J Food Sci 2012;77:M115–120. [DOI] [PubMed] [Google Scholar]
- [6].Enache E, Kataoka A, Black DG, et al. Heat resistance of histamine-producing bacteria in irradiated tuna loins. J Food Prot 2013;76:1608–14. [DOI] [PubMed] [Google Scholar]
- [7].Ben-Gigirey B, Vieites Baptista de Sousa JM, Villa TG, et al. Changes in biogenic amines and microbiological analysis in albacore (Thunnus alalunga) muscle during frozen storage. J Food Prot 1998;61:608–15. [DOI] [PubMed] [Google Scholar]
- [8].Abelson MB, Soter NA, Simon MA, et al. Histamine in human tears. Am J Ophthalmol 1977;83:417–8. [DOI] [PubMed] [Google Scholar]
- [9].Abelson MB, Baird RS, Allansmith MR. Tear histamine levels in vernal conjunctivitis and other ocular inflammations. Ophthalmology 1980;87:812–24. [DOI] [PubMed] [Google Scholar]
- [10].Allansmith MR, Baird RS, Higgenbotham EJ, et al. Technical aspects of histamine determination in human tears. Am J Ophthalmol 1980;90:719–24. [DOI] [PubMed] [Google Scholar]
- [11].Uchio E, Miyakawa K, Ikezawa Z, et al. Systemic and local immunological features of atopic dermatitis patients with ocular complications. Br J Ophthalmol 1998;82:82–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Leonardi A, Smith LM, Fregona IA, et al. Tear histamine and histaminase during the early (EPR) and late (LPR) phase of the allergic reaction and the effects of lodoxamide. Eur J Ophthalmol 1996;6:106–12. [DOI] [PubMed] [Google Scholar]
- [13].Guo Y, Ramachandran C, Satpathy M, et al. Histamin-induced myosin light chain phosphrylation breaks down the barrier integrity of cultured corneal epithelial cells. Pharmceu Res 2007;24:1824–33. [DOI] [PubMed] [Google Scholar]
- [14].Gray TB, Cursons RT, Sherwan JF, et al. Acanthamoeba, bacterial, and fungal contamination of contact lens storage cases. Br J Ophthalmol 1995;79:601–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Drancourt M, Bollet C, Carta A, et al. Phylogenetic analyses of Klebsiella species delineate Klebsiella and Raoultella gen. nov., with description of Raoultella ornithineolytica comb. nov., Raoultella terrigena comb. nov. and Raoultella planticola comb. nov. Int J Syst Evol Microbiol 2001;51:925–32. [DOI] [PubMed] [Google Scholar]


