Abstract
Rationale:
Solitary extramedullary plasmocytoma may arise in any organ, either as a primary tumor or as part of a systemic myeloma; if it rarely affects bladder, it presents with urinary symptoms. We describe the first case of asymptomatic BP occasionally diagnosed in a patient with ascites.
Patient concerns:
A 74-year-old woman with hepatitis C virus (HCV)-related liver cirrhosis presented with ascites and no urinary or other symptoms.
Diagnoses:
Routine blood tests were within normal ranges, except for mild elevation of transaminases due to chronic hepatitis. Abdominal ultrasound and computed tomography (CT) scanning showed multiple liver nodules suspected for carcinomas and, incidentally, a 18 mm solid lesion of right bladder wall.
Outcomes:
She underwent transurethral resection of the bladder tumor and percutaneous liver biopsies; final diagnosis was solitary bladder plasmocytoma (BP) and hepatocellular carcinoma (HCC), respectively. She was given chemoembolization of the main HCC nodule but no adjuvant treatment for BP. At 3-month follow-up, total-body CT showed no signs of bladder disease nor distant metastases; unfortunately, she died one month later due to liver failure.
Lessons:
This is the first reported case of asymptomatic BP. This rare neoplasm may pose difficulties in differential diagnosis with both bladder metastases and the plasmocytoid variant of bladder transitional cell carcinoma. We also highlighted lack of factors predicting disease outcome as well as response to potential adjuvant treatments.
Keywords: bladder cancer, extramedullary plasmocytoma, urothelial cancer
1. Introduction
Plasmocytoma is a rare neoplastic disorder arising from B-lymphocytes. It usually presents as the generalized disease multiple myeloma (MM); in less than 5% of cases, however, it may present with either a single bone lesion (solitary bone plasmocytoma—SBP) or, even more rarely, as a soft tissue mass of monoclonal plasma cells (solitary extramedullary plasmocytoma [EMP]—SEP).[1]
Most SEPs are localized in the head and neck, especially the upper respiratory tract; the second most frequent site is the gastrointestinal tract.[2] Conversely rare sites include the central nervous system, thyroid, breast, testes, parotid glands, or urinary bladder.[3] Bladder plasmocytoma (BP) is extremely uncommon, with only 22 cases having been reported so far; 8 of them had a history of MM while five had lymphadenopathy at presentation.[4] One case occurred in a renal transplant recipient[5] and the most recent one was associated with a high-grade T1 transitional cell carcinoma (TCC) of the bladder.[6] All cases reported so far presented with urinary symptoms, including hematuria, dysuria, and urinary frequency.
Herein we describe the first case of asymptomatic BP occasionally diagnosed in a patient with ascites.
2. Case
A 74-year-old woman with hepatitis C virus (HCV)-related liver cirrhosis presented with ascites. Apart from liver cirrhosis and diabetes mellitus under oral treatment, there was no relevant data in her past medical history. Routine blood tests were within normal ranges, including serum leukocytes and platelets counts, except for mild elevation of transaminases due to chronic hepatitis. Abdominal ultrasounds (US) pointed out multiple liver nodules, the larger about 70 mm in diameter, signs of cirrhosis, and an 18 mm lesion of the right bladder wall. Abdominal computed tomography (CT) scanning confirmed signs of liver cirrhosis and multiple liver nodules with nonhomogeneous contrast enhancement, thus suspected for carcinomas, the larger measuring 68 mm and with a central necrosis area (Fig. 1A). As for the urinary tract, CT confirmed the presence of the bladder neoplasm (Fig. 1B) and also showed an 11 mm stone in the inferior calyx of the left kidney.
Figure 1.
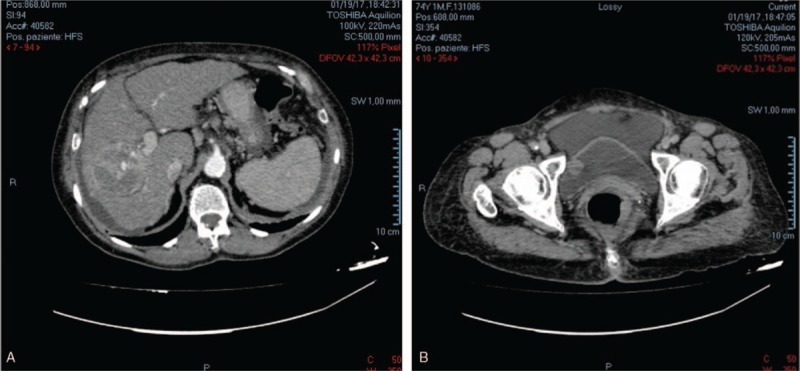
Abdominal computed tomography (CT) scanning showing: (A) a 68 mm liver nodule with nonhomogeneous contrast enhancement and a central necrosis area suspected for carcinoma; (B) an 18 mm bladder neoplasm of right bladder wall.
After having signed a written informed consent (ethical approval was not necessary because it was a standard procedure), the patient underwent transurethral resection of bladder tumor (TURBT) and percutaneous liver biopsies. As for the bladder lesion, pathology revealed a massive and widespread infiltration of cuboidal cells with bland atypical features, featuring the following immunophenotype: pan-cytokeratin negative, vimentin positive, CD138 positive with kappa light chain restriction, consistent with plasma cell neoplasm. As for the liver biopsy, pathology disclosed a well-differentiated hepatocellular carcinoma (HCC) (G1 of Edmundson).
The patient was scheduled for chemoembolization of the main HCC nodule and bone marrow biopsy. The latter was hypocellular with overall regular maturation and a plasma cell count of 15%, showing no light chain restriction. The final laboratory tests revealed clinically significant abnormalities: hemoglobin 8.8 g/dL, leukocytes 8.23 × 103/μL, platelet count of 88 × 103/μL, total bilirubin 4.87 mg/dL, AST 127 U/L, ALT 57 U/L, gamma-GT 75 U/L, albumin 2.42 g/dL, high level of serum IgG-Kappa e IgG-lambda paraproteins with 2.2 K/L ratio and no Bence Jones protein levels. Such findings ruled out MM and were consistent with solitary BP.
In view of her liver disease, no adjuvant chemo- or radiotherapy was planned for BP. At 3-month follow-up, total-body CT showed no signs of bladder disease nor distant metastases; also cystoscopy showed no evidence of recurrent bladder disease. Unfortunately, 1 month later she developed liver failure and died of cardiac arrest.
3. Discussion
SEP may arise in any organ, either as a primary tumor or as part of a systemic myeloma. It is less common than SBP and it is usually associated with better prognosis and higher cure rate. BP is an extremely rare form of SEP, with only 22 cases having been reported so far. As mentioned above, 8 of them had a history of MM while 5 had lymphadenopathy at presentation,[7] somehow providing further evidence for the ability of this neoplasm to progress to MM. Moreover, all cases reported so far presented with urinary symptoms suggestive for a bladder neoplasm, such as hematuria, dysuria, and urinary urgency. Our patient had no concomitant lymphadenopathy, no concomitant MM and, importantly, no urinary symptoms, with BP being occasionally diagnosed by a CT scan performed in the assessment of liver HCC.
Apart from clinical diagnostic criteria for BP,[8] histological diagnosis is based on specific immunohistochemical findings (CD138 expression and lack of cytokeratins). BP must be differentiated from plasmocytoid-type TCC, which is a highly aggressive malignancy associated with a poor prognosis; this differentiation is sometimes difficult.[9] The plasmocytoid-type TCC is an invasive epithelial malignancy. Histologically, it can be seen extending from the urothelium into the lamina propria, whereas plasmocytoma is noninvasive and is only found in the lamina propria. Moreover, plasmocytoid TCC, like all other TCCs, is clearly visible at cystoscopy whereby plasmocytoma, like bladder metastases, usually is a bladder mass seen on imaging but not on initial flexible cystoscopy, with resection being necessary to obtain the diagnosis. Plasmocytoid carcinomas are not always of transitional cell origin, and the differential diagnosis with secondary neoplasms must be always considered.[10–13]
It is worth mentioning that BP, like all other SEPs, may progress to MM in as much as 30% of patients. Therefore, like for high risk bladder cancer, whereby great efforts have been made to identify molecular markers that may predict disease outcome or even represent novel therapeutic targets,[14–20] prognostic and predictive markers of BP outcome are awaited. To date research has identified microvessel density as a reliable risk factor for disease progression[7]; unfortunately, no attempt has been done to test the role of molecular markers, probably also due to rarity of this disease.
Due to the above-mentioned risk of progression, adjuvant radio- or chemotherapy are usually recommended. Reported treatment options specifically include systemic chemotherapy,[21] immunotherapy combined with chemotherapy,[5] radium implants,[22] cystectomy,[9] and radiotherapy.[23,24] Given the radiosensitivity of EMP in other anatomical sites, radiotherapy remains the mainstay of treatment in patients with no evidence of systemic disease[25]; in such cases, the local recurrence rate is less than 5%.[26] Adjuvant chemotherapy is preferred in patients with lymphadenopathy or with radiation resistant tumors.[2] Though no specific long-term follow-up data are available, patients with systemic disease obviously have poorer outcome.
4. Conclusions
This is the first reported case of asymptomatic BP. This rare tumor may be difficult to differentiate from bladder metastases and from the plasmocytoid variant of bladder TCC. The risk of progression to systemic disease would recommend adjuvant treatment. Radiotherapy remains the preferred option but efforts should be made to determine which treatment should be given to which patient.
Footnotes
Abbreviations: BP = bladder plasmocytoma, CT = computed tomography, HCC = hepatocellular carcinoma, HCV = hepatitis C virus, MM = multiple myeloma, SEP = solitary extramedullary plasmocytoma, TCC = transitional cell carcinoma, TURBT = transurethral resection of the bladder tumor, US = ultrasound.
LC and VM contributed equally to this work.
The authors have no conflicts of interest to disclose.
References
- [1].Moulopoulos LA, Dimopoulos MA, Weber D, et al. Magnetic resonance imaging in the staging of solitary plasmacytoma of bone. J Clin Oncol 1993;11:1311–5. [DOI] [PubMed] [Google Scholar]
- [2].Soutar R, Lucraft H, Jackson G, et al. Guidelines on the diagnosis and management of solitary plasmacytoma of bone and solitary extramedullary plasmacytoma. Clin Oncol (R Coll Radiol) 2004;16:405–13. [DOI] [PubMed] [Google Scholar]
- [3].Dimopoulos MA, Kiamouris C, Moulopoulos LA. Solitary plasmacytoma of bone and extramedullary plasmacytoma. Hematol Oncol Clin North Am 1999;13:1249–57. [DOI] [PubMed] [Google Scholar]
- [4].Khaliq W, Uzoaru I, Konchanin RP, et al. Solitary Extramedullary plasmacytoma of the bladder: a case report and literature. Oncology (Williston Park) 2010;24:832–5. [PubMed] [Google Scholar]
- [5].Takahashi R, Nakano S, Namura K, et al. Plasmacytoma of the urinary bladder in a renal transplant recipient. Int J Hematol 2005;81:255–7. [DOI] [PubMed] [Google Scholar]
- [6].Wadhwa K, Singh R, Solomon LZ. Bladder extramedullary plasmacytoma and synchronous bladder urothelial transitional cell carcinoma: a case report and review of the literature. Open Access J Urol 2011;3:25–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Kumar S, Fonseca R, Dispenzieri A, et al. Prognostic value of angiogenesis in solitary bone plasmacytoma. Blood 2003;101:1715–7. [DOI] [PubMed] [Google Scholar]
- [8].Rajkumar SV, Dispenzieri A, Kyle RA. Monoclonal gammopathy of undetermined significance, Waldenstrom macroglobulinemia, AL amyloidosis, and related plasma cell disorders: diagnosis and treatment. Mayo Clin Proc 2006;81:693–703. [DOI] [PubMed] [Google Scholar]
- [9].Lopez A, Mendez F, Puras-Baez A. Extramedullary plasmacytoma invading the bladder: case report and review of the literature. Urol Oncol 2003;21:419–23. [DOI] [PubMed] [Google Scholar]
- [10].Sanguedolce F, Landriscina M, Ambrosi A, et al. Bladder metastases from breast cancer: managing the unexpected. A systematic review. Urol Int 2017;doi: 10.1159/000481576. [DOI] [PubMed] [Google Scholar]
- [11].Sanguedolce F, Loizzi D, Sollitto F, et al. Bladder metastases from lung cancer: clinical and pathological implications: a systematic review. Oncology 2017;92:125–34. [DOI] [PubMed] [Google Scholar]
- [12].Cormio L, Sanguedolce F, Di Fino G, et al. Asymptomatic bladder metastasis from breast cancer. Case Rep Urol 2014;2014:672591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Cormio L, Sanguedolce F, Di Fino G, et al. Bladder metastasis from lung adenocarcinoma: a difficult differential diagnosis with primary bladder adenocarcinoma. World J Surg Oncol 2014;12:90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Bufo P, Sanguedolce F, Tortorella S, et al. Expression of mitotic kinases phospho-aurora A and aurora B correlates with clinical and pathological parameters in bladder neoplasms. Histol Histopathol 2010;25:1371–7. [DOI] [PubMed] [Google Scholar]
- [15].Sanguedolce F, Bufo P, Carrieri G, et al. Predictive markers in bladder cancer: do we have molecular markers ready for clinical use? Crit Rev Clin Lab Sci 2014;51:291–304. [DOI] [PubMed] [Google Scholar]
- [16].Cormio L, Sanguedolce F, Cormio A, et al. Human epidermal growth factor receptor 2 expression is more important than Bacillus Calmette Guerin treatment in predicting the outcome of T1G3 bladder cancer. Oncotarget 2017;8:25433–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Cormio L, Tolve I, Annese P, et al. Altered p53 and pRb expression is predictive of response to BCG treatment in T1G3 bladder cancer. Anticancer Res 2009;29:4201–4. [PubMed] [Google Scholar]
- [18].Cormio L, Tolve I, Annese P, et al. Retinoblastoma protein expression predicts response to bacillus Calmette-Guerin immunotherapy in patients with T1G3 bladder cancer. Urol Oncol 2010;28:285–9. [DOI] [PubMed] [Google Scholar]
- [19].Cormio A, Sanguedolce F, Musicco C, et al. Mitochondrial dysfunctions in bladder cancer: exploring their role as disease markers and potential therapeutic targets. Crit Rev Oncol Hematol 2017;117:67–72. [DOI] [PubMed] [Google Scholar]
- [20].Sanguedolce F, Cormio A, Bufo P, et al. Molecular markers in bladder cancer: novel research frontiers. Crit Rev Clin Lab Sci 2015;52:242–55. [DOI] [PubMed] [Google Scholar]
- [21].Matsumiya K, Kanayama Y, Yamaguchi S, et al. Extramedullary plasmocytoma (EMP) of urinary bladder. Urology 1992;40:67–70. [DOI] [PubMed] [Google Scholar]
- [22].Gorfain AD. Extramedullary plasmocytoma of the bladder with local metastasis. Calif Med 1949;71:147–8. [PMC free article] [PubMed] [Google Scholar]
- [23].Mokhtar GA, Yazdi H, Mai KT. Cytopathology of extramedullary plasmocytoma of the bladder: a case report. Acta Cytol 2006;50:339–43. [DOI] [PubMed] [Google Scholar]
- [24].Shpilberg O, Raviv G, Ramon J, et al. Massive haematuria due to extramedullary plasmacytoma invading the bladder. Med Pediatr Oncol 1993;21:67–9. [DOI] [PubMed] [Google Scholar]
- [25].Alexiou C, Kau RJ, Dietzfelbinger H, et al. Extramedullary plasmacytoma: tumor occurrence and therapeutic concepts. Cancer 1999;85:2305–14. [PubMed] [Google Scholar]
- [26].Dimopoulos MA, Moulopoulos LA, Maniatis A, et al. Solitary plasmacytoma of bone and asymptomatic multiple myeloma. Blood 2000;96:2037–44. [PubMed] [Google Scholar]


