Abstract
Background
The inflatable penile prosthesis (IPP) is typically the preferred implant for Peyronie’s disease (PD) and malleable penile prostheses (MPPs) have been discouraged.
Aims
To evaluate the effectiveness and patient satisfaction of the MPP vs IPP in patients with PD.
Methods
Men with PD and erectile dysfunction who elected for penile implant surgery constituted the study population. Preoperatively, demographic and comorbidity parameters were recorded. Curvature was measured with a goniometer at maximum rigidity after intracavernosal injection of a vasoactive agent. Postoperatively, overall satisfaction was measured at 3, 6, 12, and 24 months on 5-point Likert scale from 1 (dissatisfied) to 5 (very satisfied).
Results
166 men with a mean age of 59 ± 10 years were analyzed. The mean preoperative curvature in the entire cohort was 65° (range = 30–130°). 94% of patients with MPP had total resolution of their curvature at the end of the operation, whereas 8 patients (6%) had residual curvature (25–40°). In the IPP group 25 of 30 (83.3%) had a straight penis at the end of surgery, whereas 5 of 30 (16.7%) had residual curvature, with the mean magnitude being 33° in the MPP group and 30° in the IPP group. 86% of all patients had diabetes. There were no differences between the 2 implant groups in age, hemoglobin A1c, body mass index, or smoking status. The mean patient satisfaction was 4.42 ± 0.70 (range = 2–5) and there was no difference between the 2 groups. The mean follow-up period was 23.4 months (range = 6–29 months).
Conclusion
We found that the MPP is as effective as the IPP in curvature correction in patients with PD, with similar patient satisfaction for the 2 groups.
Habous M, Farag M, Tealab A, et al. Malleable Penile Implant Is an Effective Therapeutic Option in Men With Peyronie’s Disease and Erectile Dysfunction. Sex Med 2018;6:24–29.
Key Words: Erectile Dysfunction, Peyronie’s Disease, Malleable Penile Prosthesis, Inflatable Penile Prosthesis, Penile Deformity, Penile Curvature
Introduction
Implanting a penile prosthesis is often the best treatment for patients with severe erectile dysfunction (ED) that does not respond to pharmacotherapy. Pharmacotherapy often fails in patients with diabetes, radical prostatectomy, Peyronie’s disease (PD), and severe penile fibrosis. Penile prosthetic surgery has high long-term mechanical reliability and patient satisfaction rates higher than 85%.1 Penile prosthesis implantation is the standard procedure for patients with PD and concomitant ED that does not respond to medical treatment.2 20% to 30% of patients with PD have ED refractory to medical therapy and can benefit from a combined procedure addressing these 2 conditions.3 Penile implant placement in these patients can treat the 2 problems by providing penile rigidity and the deformity correction required. Although patients with mild degrees of curvature can have complete penile straightening by placement of the prosthesis alone, many patients have residual curvature requiring intraoperative adjuvant maneuvers, such as modeling and plaque incision with or without grafting.4, 5
Garaffa et al6 reported that of additional straightening procedures, modeling was more successful in achieving straightening when performed on an inflatable penile prosthesis (IPP; 84%) than on a malleable penile prosthesis (MPP; 54%). If the curvature persisted after modeling or the curvature was ventral, straightening was achieved with tunica plications or incision with or without grafting. In another study, Levine et al7 reported on a single-center experience with the IPP and straightening maneuvers as necessary in 90 men with medication-refractory ED and PD. Additional intraoperative maneuvers used to straighten the penis after placement of the prosthesis included manual modeling, plaque incision, and grafting, if the defect created with the incision was large enough (≥2 cm). In their study, IPP placement allowed reliable and satisfactory coitus for the great majority of men (91%).
Although all types of penile implants can be used, implantation of an IPP has been reported to be the most effective and preferred in those patients based on the published data.8, 9, 10 In certain regions of the world, the MPP is the penile implant of choice for ED, often because of economic reasons. However, it has been suggested the MPP is not ideal for patients with PD.10
Our hypothesis was that the MPP would be as effective as the IPP in the management of patients with ED and PD. Our clinical experience suggests that the MPP is an effective strategy in the treatment of patients with combined PD and ED. We compared the outcome and satisfaction rate in patients with PD and ED receiving the MPP compared with those receiving the IPP.
Methods
Study Population
From July 2011 through June 2014, men with PD and ED not responding to medical therapy were counseled regarding penile implant surgery.
Patients who had a favorable clinical response with an intracavernosal injection (ICI) and refused ICI as a therapeutic option for their ED were included in this study. For this analysis, we included only those who had a favorable clinical response to ICI so that we could accurately measure the magnitude of curvature before surgery. Some patients requested penile implantation after they noticed that they had lost significant penile size. Others who had significant deformity did not wish to undergo corrective surgery (eg, Nesbit) with subsequent risk of ED and losing more penile size. They wanted to address their problems with 1 final solution. After good counseling and explaining all therapeutic options, patients who had a favorable clinical response with ICI but who found ICI unpalatable and refused further treatment with ICI were chosen for penile implantation. Penile implant surgery is the treatment of choice in such men in our practice and this is supported by International Consultation on Sexual Medicine guidelines.11
Those who opted for this procedure constituted the study population. The criteria for penile implant surgery in this population included (i) men in a stable relationship, (ii) men with penile curvature of at least 30°, (iii) men with ED refractory to medical therapy, and (iv) stable penile curvature for at least 9 months. Complete medical and sexual history, physical examination, and comorbidities were recorded for all patients. Basic investigational workup included penile duplex ultrasound study with ICI for all patients. The MMP used was the Genesis (Coloplast, Minneapolis, MN, USA) and the IPP used was the Titan OTR (Coloplast). The study was approved by our institutional ethical board committee.
Penile Deformity Assessment
Curvature was measured with a goniometer at maximum rigidity after ICI using an intracavernosal quadri-mix (prostaglandin E1 5 μg, papaverine 15 mg, phentolamine 1 mg, atropine 20 μg per 1 mL of saline). Repeated dosing was administered to ensure full erection in all patients (mean dose = 0.3 mL, range = 0.1–1 mL).
Preoperative Counseling for Implant Type
The preoperative discussion focused on the goal of obtaining “functional straightness” and patients were informed that a residual curvature no greater than 20° in any direction would not compromise sexual activity and that a curvature less than 20° was the goal and further maneuvers would not be used if such a residual curvature existed. Advantages and disadvantages of the MPP and IPP were explained thoroughly for all patients. Choosing the MPP vs the IPP was the patient’s decision. The surgeon’s role was to explain the advantages and disadvantages of each type of implant using educational videos. At our center, most patients choose the MMP, primarily because the patient pays for this procedure (no insurance coverage). The average cost of an MMP in our center is US$1,300 and the total cost of MMP implantation ranges from US$5,500 to US$6,000. In contrast, the cost of a 3-piece IPP is US$5,800 and the total cost of IPP implantation ranges from US$12,000 to US$13,000. Some chose the MPP because of fear of mechanical failure of the IPP and others chose the MMP because of its simplicity of usage. The main reason for choosing the IPP was the likelihood of increased girth compared with the MPP. Concealment was of minor importance in our patient’s decision making. An informed consent was signed by all patients. This consent form included all potential complications for the 2 implant types. This consent included a statement that penile implant surgery is an irreversible surgery, so if the patient decided to remove the implant, he could not have erection again with ICI or oral therapy. When asked, men dissatisfied with their MPP were not likely to change their mind and would not have chosen an IPP. This is multifactorial but cost was a major consideration.
Implant Surgery
This study was conducted at a single center and included patients operated on by 4 high-volume surgeons (≥50 implants/year). The MPP was implanted through the ventral penile approach in all patients. A 4- to 6-cm midline incision was made at the ventral proximal penile shaft. Dissection of the Dartos and Bucks fascia was performed with exposure of the tunica albuginea and corpus spongiosum. The Genesis is the implant used by our center, and the size used is according to the measured length and the diameter used is 1 mm smaller than the largest dilator inserted.
The IPP was implanted using the standard scrotal or penoscrotal approach in all patients. Dilation in these cases used the Brooks dilators proximally and distally. After insertion of the cylinders and maximal inflation, residual curvature was measured as outlined earlier. If residual curvature greater than 20° remained, then the technique of modeling popularized by Wilson and Delk5 was used. For the IPP it was necessary during modeling to initially clamp the cylinder input tubes to protect the pump from backpressure flow. The prosthetic cylinders were inflated to high pressure, the input tube was clamped with rubber-shod clamps, and the penis was grasped with both hands and bent over the inflated cylinders at the region of maximum curvature. Bending was maintained for 90 seconds and then relaxed. For the MPP, if placement of the rods did not adequately straighten the erection, then the modeling procedure was used12; we have found this technique much easier to use in our practice The remaining patients whose modeling failed required additional procedures for residual curvatures, such as plaque incision or excision. At least 1 relaxing transverse incision (H-shape) was made in the plaque using electrocautery. Incisions were made carefully over the existing prosthesis and were limited to the tunica, preserving the underlying cavernosal tissue. In some patients, plaque excision was required to accomplish complete straightening. To access the plaque for patients requiring plaque incision or excision, the neurovascular bundle was routinely elevated. The neurovascular bundle was dissected and mobilized when needed according to standard surgical techniques. The same was done for the corpus spongiosum. After these maneuvers, reassessment of corporal length was conducted to optimize implant length. In some patients, plaque excision was needed and this was performed by extending the corporotomy so that the plaque excision was done under direct vision. The cutting current in electrocautery with the aid of toothed forceps was used to dissect the scarred tissue (plaques) from the wall of the tunica albuginea. Reassessment of corporal length after these maneuvers was done as described earlier, and any extra cylinder length was added as needed using rear-tip extenders.
Questionnaire
The Sexual Health Inventory for Men (SHIM) questionnaire was completed as part of the preoperative evaluation of patients presenting to our clinic complaining of ED. Postoperatively, overall satisfaction was measured at 3, 6, 12, and 24 months on a 5-point Likert scale (1 = dissatisfied, 2 = not satisfied, 3 = moderately satisfied, 4 = satisfied, 5 = very satisfied).
Statistical Analysis
Descriptive statistics are reported. Statistical analysis was done using IBM SPSS Statistics (IBM Corporation, Armonk, NY, USA). Simple independent measures t-tests (2-tailed t-test) were used for satisfaction and SHIM scores, and χ2 tests were used for group comparisons. A P value less than .05 was considered statistically significant.
Results
Patient Population
166 men were included. Patient demographic and comorbidity data are presented in Table 1. 82% received an MPP and 18% received an IPP. In the overall cohort, preoperative penile curvatures were dorsal in 34%, lateral in 31%, ventral in 23%, and multiplanar in 12%. The mean preoperative curvature in the entire cohort was 65° (range = 30–130°; 67° in MPP group, 63° in IPP group; P = .55)
Table 1.
Patient demographic and comorbidity data
| Parameter | Entire cohort (N = 166) | MPP group (n = 136) | IPP group (n = 30) | P value∗ |
|---|---|---|---|---|
| Age (y), mean ± SD (range) | 59 ± 9.8 (24–81) | 58.7 ± 9.7 (24–81) | 59.1 ± 10.0 (29–75) | .75 |
| HbA1c (%), mean ± SD (range) | 8 ± 1.6 | 8.1 ± 1.5 (4.9–12.0) | 7.5 ± 1.6 (5.3–10.7) | .03 |
| BMI (kg/m2), mean ± SD (range) | 30 ± 5 | 30.2 ± 4.7 (20–48) | 30.7 ± 4.8 (16–38) | .61 |
| Preoperative curvature (°), mean (range) | 65 (30–130) | 67 | 63 | .55 |
BMI = body mass index; HbA1c = hemoglobin A1c; IPP = inflatable penile prosthesis; MPP = malleable penile prosthesis.
IPP vs MPP group.
Implant Outcomes
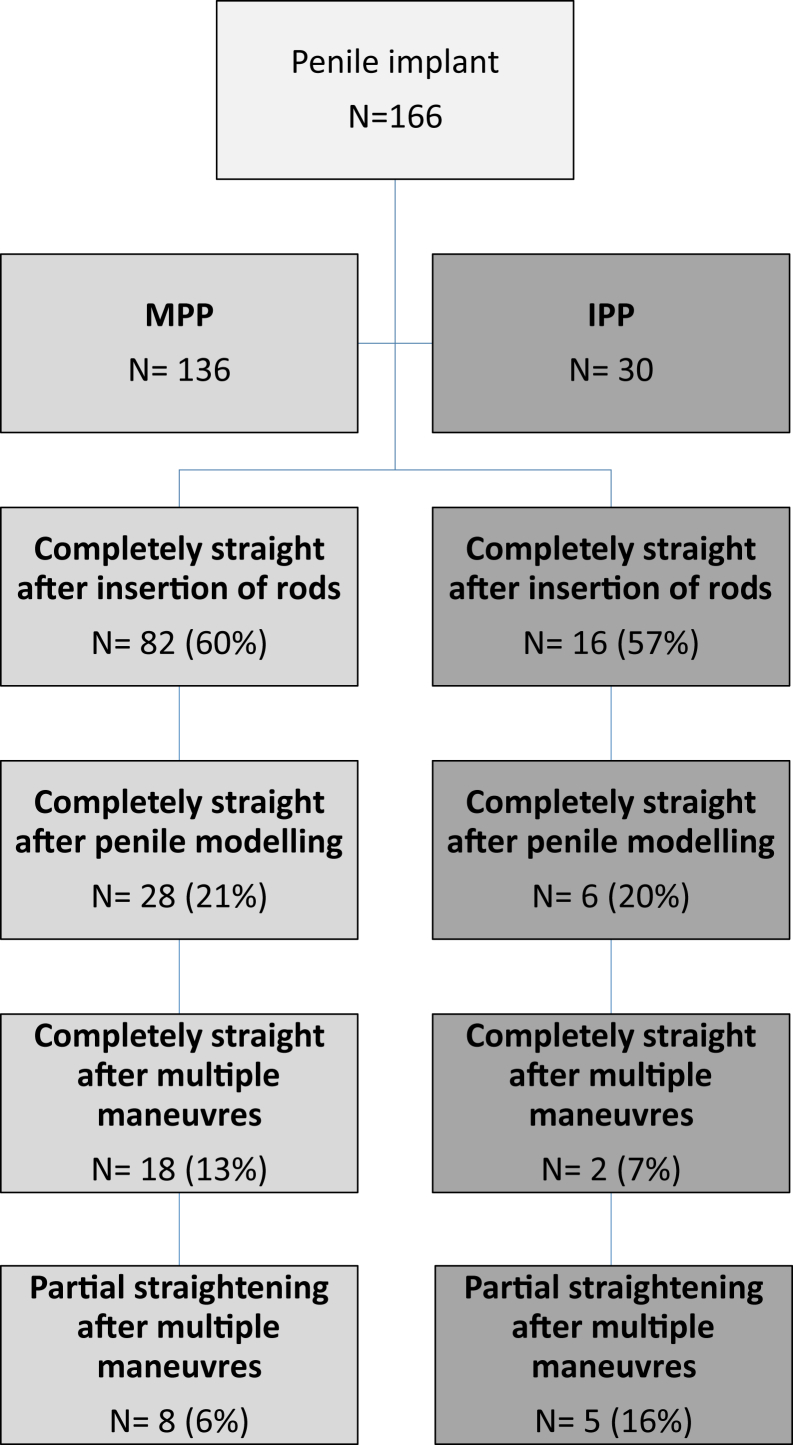
Of the entire cohort, 92% had total resolution of their curvature (0°) and 8% had residual curvature (mean = 32°, range = 25–40°) requiring adjuvant maneuvers (plaque incision and/or excision). Implant outcomes in the 2 groups are presented in Figure 1. At the end of surgery (placement of prosthesis with or without extra maneuvers), curvature was completely fixed in 94% of the MPP group and completely fixed in 83% of the IPP group (P = .48). There was no significant difference in complication rate between the MPP and IPP groups. Major complications included 4 cases with wound infection (3 with MPP and 1 with IPP). All responded well to conservative therapy and achieved complete healing. Minor complications included temporary penoscrotal edema, ecchymosis, and local pain occurred in most men.
Figure 1.
Summary of implant outcomes in the 2 groups. IPP = inflatable penile prosthesis; MPP = malleable penile prosthesis.
Questionnaire Outcomes
There was no statistically significant difference between the MPP and IPP groups in postoperative satisfaction scores or SHIM scores (Table 2). The postoperative SHIM score was obtained 3 months after surgery and repeated at 6, 12, and 24 months. This satisfaction rate was sustained in the 2 groups at a mean follow-up period of 23.4 months (range = 6–29 months).
Table 2.
Questionnaire data outcome
| MPP group | IPP group | P value∗ | |
|---|---|---|---|
| Preoperative SHIM score, mean ± SD (range) | 9.1 ± 2.6 (6–16) | 8.6 ± 2.5 (6–14) | .32 |
| Postoperative SHIM score, mean ± SD (range) | 22.5 ± 2.5 (12–25) | 22.3 ± 2.5 (13–25) | .64 |
| Postoperative satisfaction, mean ± SD (range) | 4.4 ± 0.7 (2–5) | 4.3 ± 0.8 (2–5) | .32 |
IPP = inflatable penile prosthesis; MPP = malleable penile prosthesis; SHIM = Sexual Health Inventory for Men.
IPP vs MPP group.
Discussion
PD prevalence rates of 0.4% to 9% have been published.13 PD is frequently associated with ED and a variety of other comorbid disorders, including diabetes, hypertension, and radical prostatectomy. 2 thirds of patients with PD are likely to have risk factors for arterial disease and therefore worsening long-term erectile function.14 Usta et al15 reported that ED in men with PD ranged from 20% to 54%.
Because PD is associated in many patients with impaired sexual functioning, true sexual dysfunction as a result of the penile deformity must be assessed. Inability of the patient to engage in penetrative sexual intercourse can be related primarily to penile deformity, which physically limits penile penetration; pain (during sexual activity) experienced by the patient or partner as a result of the penile deformity; or ED, by which the penis cannot achieve or maintain the rigidity necessary for the completion of intercourse.16
The purpose of surgery for the treatment of PD is to enable the patient to resume satisfactory sexual activities. This requires a functionally straight and sufficiently rigid penis to enable him to accomplish penetrative intercourse. Penile implantation can address these 2 issues simultaneously.16
Historically, the IPP has been associated with higher functional satisfaction and lower persistent curvature rates. The 3-piece IPP cylinders allow more flexible sizing. It is generally recommended that cylinders that expand in length should be avoided. The 2-piece hydraulic Ambicor IPP (AMS, Minneapolis, MN, USA) can be used in PD when placement of an intra-abdominal reservoir poses a problem. However, these devices do not deflate fully (because they are prefilled) and can be difficult to place when there is some degree of constriction within the corpus cavernosum.7, 12, 17
The MPP also can be used in patients with PD, although some investigators have argued against them.10 Also, the American Urological Association 2015 guidelines for PD state that clinicians should use the IPP for patients undergoing penile prosthetic surgery for the treatment of PD, but this recommendation is based on expert opinion.18 These devices (MPP) are more suitable for patients with impaired manual dexterity and for whom placement of an IPP would prove difficult. Montorsi et al10 reported that placement of an MPP for PD was associated with a significant patient-partner dissatisfaction rate. They assessed the long-term acceptance of and satisfaction with penile implants in patients with PD and their partners. From 1985 to 1987, 50 men with PD and associated ED were treated with an MPP without additional plaque surgery. 48 patients and 29 partners were reassessed at a follow-up of at least 60 months. Only 23 patients (48%) and 12 partners (40%) were totally satisfied with the long-term functional result and would repeat the same operation. For the 25 patients (52%) dissatisfied with the procedure, loss of natural tumescence resulting in a pencil-like penis, decrease in penile sensitivity, poor concealment, and persistence of penile deviation were the major complaints. Of the partners, 17 (60%) were dissatisfied because of poor penile girth, sensation of a cold glans, sensation of unnatural intercourse, and dyspareunia.10 How different the patient or partner satisfaction would have been with the IPP is not known from this study.7
In our study, 94% of our MPP group achieved a completely straight penis at the end of the operation and this continued through the end of the follow-up period. In the MPP group, the mean satisfaction score 3 months postoperatively was comparable to that of the IPP group. This satisfaction rate also was durable, with a mean follow-up period of 23.4 months (6–29 months). We believe that the reason we could achieve such excellent straightening of curvature without adjuvant maneuvers is that during corporal dilation we have to dilate aggressively to create a wide enough space for the MPP. We believe this to be a critical factor in disrupting intracorporal synechiae, which might play some role in curvature in men with PD, to straighten the penis. Optimal outcomes with the MPP could use the modeling procedure used for the IPP. 20% of our patients who received the MPP required this for significant residual curvature after implant placement. Modeling failed to correct the residual curvature in 21% and plaque incision was required for the remainder of the patients who received the MPP. This is comparable to the need for this procedure in the IPP group in our analysis.
In support of our findings, Ghanem et al19 reported their experience in a much smaller group (20 men) with PD who underwent placement of an MPP. They reported complete straightening of the penile shaft in 65% of their patients, whereas the remaining patients had some degree of deviation. They also reported a high rate of satisfaction (87%). They concluded the safety and effectiveness of the MPP in the management of PD associated with ED.
In addition to the lower cost of the MPP, the simplicity of the procedure for the surgeon and patient is a potential significant advantage. Based on our data, we believe that using the MPP is a reasonable approach for patients who have PD and ED. In certain regions of the world where patients pay for the implant (no insurance coverage), the MPP is an excellent choice for those patients. There is little doubt that the cultural milieu and socioeconomic factors have played some role in the acceptance of the MPP. We believe that insurance coverage for penile implant surgery in countries such as the United States has a major role in the domination of the IPP, which might not be the case if it were not covered. However, the fact is the MPP can be used to correct penile curvature in men with PD.
To our knowledge, this is the largest published series assessing the outcome of MPP placement in patients with PD with a comparison of the outcome of IPP placement at the same center. However, this was not a randomized controlled study, although randomized controlled trials in the surgical space are notoriously difficult to conduct. Furthermore, no assessment of postoperative penile length or long-term residual deformity was performed, which would have added value to the study. Moreover, a randomized controlled trial likely would have affected only patient satisfaction outcomes and have little effect on data pertaining to curvature correction with an implant. Other limitations are the medium-term follow-up, a small number of patients receiving the IPP, and lack of a validated instrument for satisfaction after surgery.
Therefore, although a consensus on the ideal surgical method for the reconstruction of penile deformity in men with ED does not exist, current efforts should focus on reaching a consensus on the ideal way to follow these patients in the long term and compare the outcome in all aspects including cost.
Conclusions
We have demonstrated that the ability of MPP to restore functional erections is excellent, as good as the IPP, at least if adjuvant intraoperative maneuvers are used when residual curvature is encountered. Furthermore, there appears to be no difference in satisfaction between patients who received the MPP and those who received the IPP.
Statement of authorship
Category 1
-
(a)Conception and Design
- Mohamad Habous; Alaa Tealab; David Ralph; Saleh Binsaleh; John Mulhall
-
(b)Acquisition of Data
- Mohamad Habous; Alaa Tealab; Mohammed Farag; Tarek Soliman; Saad Mahmoud; Amin Elserafy; Zenhom Mekawi; Abdallah Remeah; Mohammed Nassar; Osama Laban
-
(c)Analysis and Interpretation of Data
- Mohamad Habous; Ben Williamson; Osama Abdelwahab; Simone Giona; John Mulhall
Category 2
-
(a)Drafting the Article
- Mohamad Habous; Alaa Tealab; Mohammed Farag; John Mulhall
-
(b)Revising It for Intellectual Content
- Mohamad Habous; David Ralph; John Mulhall
Category 3
-
(a)Final Approval of the Completed Article
- Mohamad Habous; John Mulhall
Footnotes
Conflicts of Interest: The authors report no conflicts of interest.
Funding: None.
References
- 1.Carson C.C. Penile prostheses: are they still relevant? BJU Int. 2003;91:176–177. doi: 10.1046/j.1464-410x.2003.t01-1-03064.x. [DOI] [PubMed] [Google Scholar]
- 2.Ralph D., Gonzalez-Cadavid N., Mirone V. The management of Peyronie’s disease: evidence-based 2010 guidelines. J Sex Med. 2010;7:2359–2374. doi: 10.1111/j.1743-6109.2010.01850.x. [DOI] [PubMed] [Google Scholar]
- 3.Levine L.A., Larsen S.M. Surgery for Peyronie’s disease. Asian J Androl. 2013;15:27–34. doi: 10.1038/aja.2012.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chaudhary M., Sheikh N., Asterling S. Peyronie’s disease with erectile dysfunction: penile modeling over inflatable penile prostheses. Urology. 2005;65:760–764. doi: 10.1016/j.urology.2004.10.039. [DOI] [PubMed] [Google Scholar]
- 5.Wilson S.K., Delk J.R., II A new treatment for Peyronie’s disease: modeling the penis over an inflatable penile prosthesis. J Urol. 1994;152:1121–1123. doi: 10.1016/s0022-5347(17)32519-3. [DOI] [PubMed] [Google Scholar]
- 6.Garaffa G., Minervini A., Christopher N.A. The management of residual curvature after penile prosthesis implantation in men with Peyronie’s disease. BJU Int. 2011;108:1152–1156. doi: 10.1111/j.1464-410X.2010.10023.x. [DOI] [PubMed] [Google Scholar]
- 7.Levine L.A., Benson J., Hoover C. Inflatable penile prosthesis placement in men with Peyronie’s disease and drug-resistant erectile dysfunction: a single-center study. J Sex Med. 2010;7:3775–3783. doi: 10.1111/j.1743-6109.2010.01971.x. [DOI] [PubMed] [Google Scholar]
- 8.Wilson S.K. Surgical techniques: modeling technique for penile curvature. J Sex Med. 2007;4:231–234. doi: 10.1111/j.1743-6109.2007.00407.x. [DOI] [PubMed] [Google Scholar]
- 9.Carson C.C. Penile prosthesis implantation in the treatment of Peyronie’s disease and erectile dysfunction. Int J Impot Res. 2000;12:122–126. doi: 10.1038/sj.ijir.3900590. [DOI] [PubMed] [Google Scholar]
- 10.Montorsi F., Guazzoni G., Bergamaschi F. Patient-partner satisfaction with semirigid penile prosthesis for Peyronie’s disease: a 5-year follow-up study. J Urol. 1993;150:1819–1821. doi: 10.1016/s0022-5347(17)35904-9. [DOI] [PubMed] [Google Scholar]
- 11.Levine L.A., Becher E., Bella A. Penile prosthesis surgery: current recommendations from the International Consultation on Sexual Medicine. J Sex Med. 2016;13:489–518. doi: 10.1016/j.jsxm.2016.01.017. [DOI] [PubMed] [Google Scholar]
- 12.Mulcahy J.J., Wilson S.K. Management of Peyronie’s disease with penile prostheses. Int J Impot Res. 2002;14:384–388. doi: 10.1038/sj.ijir.3900865. [DOI] [PubMed] [Google Scholar]
- 13.Sommer F., Schwarzer U., Wassmer G. Epidemiology of Peyronie’s disease. Int J Impot Res. 2002;14:379–383. doi: 10.1038/sj.ijir.3900863. [DOI] [PubMed] [Google Scholar]
- 14.Ralph D.J. Long-term results of the surgical treatment of Peyronie’s disease with plaque incision and grafting. Asian J Androl. 2011;13:797. doi: 10.1038/aja.2011.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Usta M.F., Bivalacqua T.J., Tokatli Z. Stratification of penile vascular pathologies in patients with Peyronie’s disease and in man with erectile dysfunction according to age: a comparative study. J Urol. 2004;172:259–262. doi: 10.1097/01.ju.0000132154.38285.c7. [DOI] [PubMed] [Google Scholar]
- 16.Segal R.L., Burnett A.L. Surgical management for Peyronie’s disease. World J Mens Health. 2013;31:1–11. doi: 10.5534/wjmh.2013.31.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kowalczyk J.J., Mulcahy J.J. Penile curvatures and aneurysmal defects with the Ultrex penile prosthesis corrected with insertion of the AMS 700 CX. J Urol. 1996;156:398–401. doi: 10.1097/00005392-199608000-00016. [DOI] [PubMed] [Google Scholar]
- 18.Nehra A., Alterowitz R., Culkin D.J. Peyronie’s disease: AUA guideline. J Urol. 2015;194:745–753. doi: 10.1016/j.juro.2015.05.098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ghanem H.M., Fahmy I., El-Meliegy A. Malleable penile implants without plaque surgery in the treatment of Peyronie’s disease. Int J Impot Res. 1998;10:171–173. doi: 10.1038/sj.ijir.3900324. [DOI] [PubMed] [Google Scholar]