Abstract
Objective
Identify characteristics associated with hospital readmission due to bacterial respiratory tract infections (bRTI) after tracheotomy.
Study design
Retrospective study of 8009 children 0–17 years undergoing tracheotomy from 2007–2013 at 48 children’s hospitals in the Pediatric Health Information System database. The primary outcome was first hospital admission after tracheotomy for bRTI (i.e. primary diagnosis of bRTI or a primary diagnosis of bRTI symptom and secondary diagnosis of bRTI). We used Cox-proportional hazard modeling to assess associations between patient demographic and clinical characteristics and bRTI hospital readmission.
Results
Median age at tracheotomy admission was 5 months [interquartile range (IQR): 1–50 months]. Thirty-six percent (n=2,899) had at least one bRTI admission. Median time-to-readmission for bRTI was 275 days (IQR: 141–530). Factors independently associated with increased risk for bRTI readmission were younger age [e.g., age <30 days vs. 13–17 years (aHR 1.32; 95% CI: 1.11–1.58)], Hispanic race/ethnicity (vs. non-Hispanic White; aHR: 1.34; 95% CI: 1.20–1.50), government insurance (vs. private; aHR 1.21; 95% CI: 1.10–1.33), >2 complex chronic conditions (vs. zero; aHR 1.96; 95% CI: 1.34–2.86) and discharge to home (vs. post-acute care setting; aHR 1.19; 95% CI: 1.08–1.32). Trauma diagnosis at tracheotomy (aHR 0.83; 95% CI: 0.69–1) and ventilator dependency (aHR 0.88; 95% CI: 0.81–0.97) were associated with decreased risk.
Conclusions
Young, Hispanic children with multiple complex chronic conditions who use Medicaid insurance and are not discharged to post-acute care are at the highest risk for hospital readmission for bRTI post-tracheotomy. Future research should investigate strategies to mitigate this risk for these children.
Keywords: Tracheotomy, children with medical complexity, readmissions
Introduction
Each year, because of anatomic abnormalities, progression of respiratory insufficiency, or acute traumatic events, over 4000 U.S. children undergo tracheotomy.1,2 While tracheotomy improves oxygenation and ventilation, it also bypasses the upper airway defenses (e.g., upper airway humidification, cilia, mucous membrane defense mechanisms), thereby increasing the likelihood of pathogen transmission to the lower airways and bacterial respiratory tract infections (bRTI; e.g., bacterial tracheitis and pneumonia). Bacterial pneumonia is the most common reasons for hospital admission in children with tracheostomy, accounting for over 2000 admissions and $100 million in U.S. hospital charges in 2009.3
Despite being the most common reason for hospital admission, there is little information on the timing and risk factors for the development of bRTIs in pediatric patients after tracheotomy. Because tracheostomy complications impact patient and family mental and physical health4–7, identifying bRTI risk factors may inform bRTI prevention strategies to decrease antibiotic exposure, bacterial antibiotic resistance and hospital readmission. One recent single-center study of 240 pediatric patients showed that a few factors, including Hispanic ethnicity and Pseudomonas aeruginosa acquisition, were associated with increased odds of bRTI readmission post-trachetomy.8 However, previous study findings were limited by small sample sizes to explore many risk factors. Given these previous limitations, we utilized existing administrative data to create a multicenter cohort of over 8000 patients at 48 United States children’s hospitals to assess which patient characteristics are associated with hospital readmission due to a bRTI after tracheotomy.
Patients and Methods
Study Design and Setting
This is a multicenter, retrospective cohort study of administrative data from the Pediatric Health Information System (PHIS) database. The database contains inpatient, emergency department, ambulatory surgery and observation utilization data (e.g. pharmaceuticals, imaging) from 48 not-for-profit, pediatric hospitals in the United States and represents 15% of the national and 46% of all children's hospital’s admissions. Data are de-identified at the time of submission to PHIS.9 Through use of encrypted medical record numbers, the database allows for longitudinal patient tracking across multiple healthcare encounters within the same hospital. This project was deemed exempt by the Children’s Hospital Los Angeles Institutional Review Board (per 45 CFR 46.101[b][4]).
Study population
We identified all patients aged 0–17 years that underwent tracheotomy at one of the 48 PHIS participating hospitals and discharged with tracheostomy in place between 1/1/2007 and 12/31/2013 with at least one follow-up visit in the PHIS database. We identified tracheotomy by using International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) procedure codes (30.3, 30.4, 31.1, 31.2, 31.21 and 31.29) validated in prior studies examining pediatric tracheotomy.1,10 We excluded any patient who died during the index hospitalization where tracheotomy occurred or who underwent tracheostomy decannulation during initial hospitalization (ICD-9-CM procedure codes 31.72, 31.75, 97.37), as this precluded the subsequent outcome of a tracheostomy-associated bRTI.
Main Outcome Measure
The first bacterial respiratory tract infection-related (bRTI) hospital readmission following index hospitalization was identified in patients with all three of the following:
An ICD-9-CM diagnosis code consistent with tracheostomy status;
An ICD-9-CM code consistent with a primary diagnosis of bRTI or a primary diagnosis of a symptom of a RTI or viral infection with a secondary diagnosis of bRTI (E-Table 1; online); and,
Receipt of antibiotics on hospital day 0 or 1.
Tracheostomy status was identified by using ICD-9-CM codes (V44.0, V55.0, 519.00, 519.01, 519.02, and 519.09) used in previous studies examining tracheostomy outcomes with administrative data1,3,10. We used the tracheostomy diagnosis code as a criterion for subsequent respiratory infection hospital readmissions. This was to minimize including patients that underwent decannulation at a non-PHIS hospital and who were readmitted for a bRTI but did not have a current tracheostomy in place. bRTI were identified by modifying strategies based upon previous PHIS work in ICD-9-CM codes for bacterial pneumonia and aspiration pneumonia11–16; given the patient population, we also added acute tracheitis (464.1×) codes. Administration of antibiotics was identified on hospital day 0 or 1 using billing data. We assessed all subsequent discharges through December 31, 2014 for meeting our outcome criteria, making the maximum follow-up period seven years for the cohort.
Patient Demographic Characteristics
We assessed the association of several patient demographic characteristics on the likelihood of bRTI hospital readmission, including admission age at tracheotomy hospitalization (<30 days, 30 days-12 months, 1–4 years, 5–12 years, and 13–17 years), race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, and other), payer status (private, government and other). We also assessed discharge disposition [home (with or without home nursing) versus post-acute care facility] and discharge quarter of the year (January–March, April–June, July–September and October–December) to account for possible differences in bRTI hospitalization rates in the winter months.
Patient Clinical Characteristics
We used ICD-9-CM codes previously used in pediatric tracheotomy studies using administrative data to identify indications for tracheotomy as well as comorbid conditions. Indication categories included upper airway obstruction/vascular anomaly (including hemangioma, vocal cord paralysis, cleft lip/palate), chronic lung disease (e.g. cystic fibrosis, bronchopulmonary dysplasia), neurological (including muscular dystrophy, anoxic brain injury, encephalopathy), trauma (including intracranial injury, quadriplegia), and prematurity/low birth weight.1,2
We used Feudtner et al.’s complex chronic condition (version 2) classification system17 to describe medical diagnosis groupings expected to last longer than 12 months. We defined the presence of a gastrostomy tube as having an ICD-9-CM procedure codes 43.0, 43.1×, and 97.02 or ICD-9-CM diagnoses codes v44.1, v55.1, and 536.4×, as defined in previous studies.18,19 We defined ventilator dependence as having an ICD-9-CM diagnosis code of V46.1X. Given preliminary data associating congenital heart surgery with increased rates of post-tracheotomy bRTI admissions, to assess congenital heart surgery repair during the hospitalization where tracheotomy occurs, we used the Risk Adjustment for Congenital Heart Surgery (RACHS). The RACHS score stratifies congenital heart surgery repair based upon increasing risk of in-hospital mortality into one of six groups with higher RACHS scores associated with higher in-hospital mortality risk.20
Statistical analysis
We conducted bivariate analyses to assess the relationship between bRTI hospital readmission and patient characteristics. Patients who did not experience a bRTI hospital readmission were censored at their last visit recorded in PHIS (emergency room, ambulatory surgery center, hospitalization), at their subsequent death, or at the time where, in a subsequent follow-up visit, they had a decannulation procedure code. We used the log-rank test to compare single independent variables (e.g. neuromuscular disease) on time to first post-tracheotomy hospital readmission for bRTI (dependent variable). After conducting the bivariate analyses, we derived a multivariable Cox proportional hazards model to assess the specific contribution of independent variables (e.g. patient demographic variables, patient clinical characteristics) on the time to first hospital readmission for bRTI. Given possible confounding based upon previous preliminary data and hypothesized relationships, all variables evaluated in the unadjusted model of hospital readmission for a tracheostomy-associated bRTI were included in the multivariable Cox proportion hazard model. In addition to the covariates entered, we also tested an interaction term between ventilator dependence and discharge disposition because previous studies have found that patients who were ventilator-dependent were more likely to be discharged to a post-acute care facility21, thus potentially decreasing readmission risk. We also tested for collinearity between the gastrostomy tube procedure codes (representing new procedures) and diagnostic codes (representing pre-existing gastrostomy). Data were clustered by hospital for all analyses by adding hospital as a random effect to the multivariable model. All analyses used two-tailed tests with a significance level of 0.05. Statistical analysis was carried out using SAS software (version 9.4; SAS Institute, Inc, Cary, NC).
Results
Study Population
Of the 9314 unique patients discharged alive with a tracheostomy tube, 8009 (86.0%) were retained for analysis with a least one follow-up visit after discharge from the index hospitalization where tracheotomy occurred (Figure 1). The cohort was primarily male (n=4618, 57.7%), White (n=3873, 48.4%) and with government insurance (n=4940, 61.7%; Table 1). Over 58.9% (n=4715) were 12 months of age or younger upon index hospitalization where tracheotomy occurred. Comorbidities associated with tracheotomy include prematurity (n=1353, 16.9%), upper airway obstruction (n=2989, 37.3%), chronic lung disease (n=3904, 48.7%), neurologic impairment (n=3762, 47.0%) and trauma (n=519, 6.5%). Just over 10% (n=806) underwent cardiac surgery and 47.3% (n=3792) underwent gastrostomy tube placement during the tracheotomy index hospitalization. Patients were highly complex, with 69.9% (n=5595) having three or more complex chronic conditions and 22.8% (n=1826) with ventilator dependency. After the index hospitalization, 23% (n=1845) were discharged to post-acute care facilities. Thirty-six percent (n=2899) had a subsequent hospital readmission for a bRTI. The median time-to-hospital readmission for a bRTI was 275 days (IQR: 141–530 days).
Figure 1.
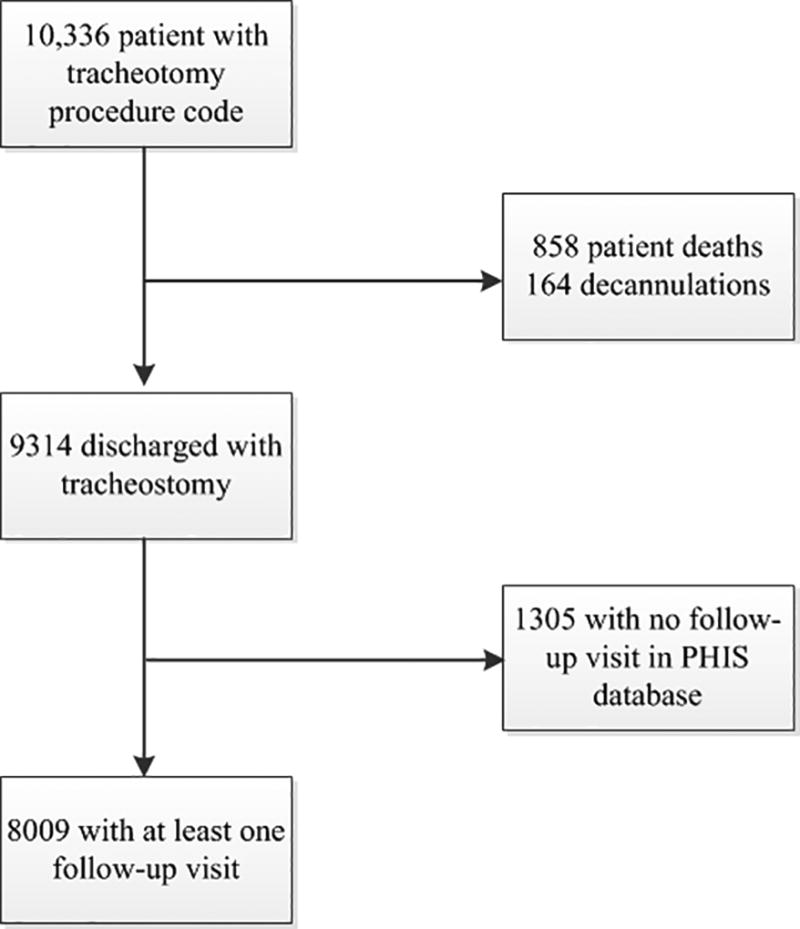
Patient flow diagram of the patients included in the current study.
Table 1.
Demographic and clinical characteristics of pediatric patients undergoing tracheotomy at a PHIS hospital between 2007 and 2013 with at least one follow-up status for any visit (emergency room, ambulatory surgery or inpatient/observation hospitalization; n=8,009)
| Variable | Total N (%) | No bRTI readmission (n=5110) |
bRTI readmission (n=2899) |
p-value |
|---|---|---|---|---|
| Gender | ||||
| Female | 3391 (42.3%) | 2158 (42.2%) | 1233 (42.5%) | 0.79 |
| Male | 4618 (57.7%) | 2952 (57.8%) | 1666 (57.5%) | |
| Admission Age | ||||
| < 30 days | 1979 (24.7%) | 1209 (23.7%) | 770 (26.6%) | < 0.001 |
| 30 days to 12 months | 2736 (34.2%) | 1659 (32.5%) | 1077 (37.2%) | |
| 1 to 4 years | 1465 (18.3%) | 904 (17.7%) | 561 (19.4%) | |
| 5 to 12 years | 918 (11.5%) | 627 (12.3%) | 291 (10%) | |
| 13 to 17 years | 911 (11.4%) | 711 (13.9%) | 200 (6.9%) | |
| Race/Ethnicity | ||||
| Non-Hispanic White | 3873 (48.4%) | 2623 (51.3%) | 1250 (43.1%) | < 0.001 |
| Non-Hispanic Black | 1703 (21.3%) | 1062 (20.8%) | 641 (22.1%) | |
| Hispanic | 1388 (17.3%) | 730 (14.3%) | 658 (22.7%) | |
| Other | 1045 (13%) | 695 (13.6%) | 350 (12.1%) | |
| Payer | ||||
| Private | 2482 (31%) | 1757 (34.4%) | 725 (25%) | < 0.001 |
| Government | 4940 (61.7%) | 2980 (58.3%) | 1960 (67.6%) | |
| Other Payer | 587 (7.3%) | 373 (7.3%) | 214 (7.4%) | |
| Discharge Location | ||||
| To home | 6164 (77%) | 3886 (76%) | 2278 (78.6%) | 0.01 |
| To post-acute care | 1845 (23%) | 1224 (24%) | 621 (21.4%) | |
| Discharge Season | ||||
| January–March | 1952 (24.4%) | 1202 (23.5%) | 750 (25.9%) | 0.10 |
| April–June | 2046 (25.5%) | 1306 (25.6%) | 740 (25.5%) | |
| July–September | 1898 (23.7%) | 1228 (24%) | 670 (23.1%) | |
| October–December | 2113 (26.4%) | 1374 (26.9%) | 739 (25.5%) | |
| Complex Chronic Conditions (CCC) | ||||
| 0 | 223 (2.8%) | 194 (3.8%) | 29 (1%) | < 0.001 |
| 1 | 758 (9.5%) | 590 (11.5%) | 168 (5.8%) | |
| 2 | 1433 (17.9%) | 934 (18.3%) | 499 (17.2%) | |
| 3 or more | 5595 (69.9%) | 3392 (66.4%) | 2203 (76%) | |
| Specific CCCs | ||||
| Technology dependency | 7112 (88.8%) | 4456 (87.2%) | 2656 (91.6%) | < 0.001 |
| Respiratory | 6185 (77.2%) | 3872 (75.8%) | 2313 (79.8%) | < 0.001 |
| Gastrointestinal | 5621 (70.2%) | 3378 (66.1%) | 2243 (77.4%) | < 0.001 |
| Neurologic and neuromuscular | 3280 (41%) | 1914 (37.5%) | 1366 (47.1%) | < 0.001 |
| Cardiovascular | 3060 (38.2%) | 1929 (37.7%) | 1131 (39%) | 0.26 |
| Other congenital or genetic defect | 2623 (32.8%) | 1574 (30.8%) | 1049 (36.2%) | < 0.001 |
| Neonatal | 2070 (25.8%) | 1253 (24.5%) | 817 (28.2%) | < 0.001 |
| Renal and urologic | 1066 (13.3%) | 693 (13.6%) | 373 (12.9%) | 0.38 |
| Metabolic | 935 (11.7%) | 581 (11.4%) | 354 (12.2%) | 0.26 |
| Hematology and immunodeficiency | 534 (6.7%) | 346 (6.8%) | 188 (6.5%) | 0.62 |
| Malignancy | 440 (5.5%) | 327 (6.4%) | 113 (3.9%) | < 0.001 |
| Transplantation | 167 (2.1%) | 133 (2.6%) | 34 (1.2%) | < 0.001 |
| Any Cardiac Surgery | 806 (10.1%) | 503 (9.8%) | 303 (10.5%) | 0.38 |
| Risk Adjustment for Congenital Heart Surgery (RACHS) Score | ||||
| RACHS Score unassigned | 285 (3.6%) | 174 (3.4%) | 111 (3.8%) | 0.78 |
| Lower risk (1 through 3) | 361 (4.5%) | 226 (4.4%) | 135 (4.7%) | |
| Higher risk (4 through 6) | 160 (2%) | 103 (2%) | 57 (2%) | |
| Underlying Medical Conditions Associated with Tracheotomy | ||||
| Chronic Lung Disease | 3904 (48.7%) | 2390 (46.8%) | 1514 (52.2%) | < 0.001 |
| Neurologic | 3762 (47%) | 2214 (43.3%) | 1548 (53.4%) | < 0.001 |
| Upper Airway Obstruction | 2989 (37.3%) | 1834 (35.9%) | 1155 (39.8%) | < 0.001 |
| History of Prematurity | 1353 (16.9%) | 844 (16.5%) | 509 (17.6%) | 0.23 |
| Trauma | 519 (6.5%) | 380 (7.4%) | 139 (4.8%) | < 0.001 |
| Other Underlying Medical Conditions | ||||
| Gastrostomy tube | 5272 (65.8%) | 3158 (61.8%) | 2114 (72.9%) | < 0.001 |
| Gastrostomy tube diagnosis code | 2232 (27.9%) | 1295 (25.3%) | 937 (32.3%) | < 0.001 |
| Gastrostomy tube procedure code | 3792 (47.3%) | 2323 (45.5%) | 1469 (50.7%) | < 0.001 |
| Ventilator dependency | 1826 (22.8%) | 1122 (22%) | 704 (24.3%) | 0.02 |
Demographic characteristics and bRTI hospital readmission (Table 2)
Table 2.
Cox proportional hazard model of factors associated with hospitalizations for a bacterial respiratory tract infection after tracheotomy.
| Unadjusted Hazard Ratio (95% CL) |
p-value | Adjusted Hazard Ratio (95% CL) | p-value | |
|---|---|---|---|---|
| Gender | ||||
| Female | 0.98 (0.91–1.05) | 0.56 | 0.99 (0.92–1.07) | 0.85 |
| Male | REF | REF | ||
| Admission Age | ||||
| < 30 days | 1.11 (0.95–1.30) | 0.20 | 1.32 (1.11–1.58) | 0.002 |
| 30 days to 12 months | 1.24 (1.06–1.44) | 0.006 | 1.45 (1.24–1.71) | <0.001 |
| 1 to 4 years | 1.30 (1.11–A1.53) | 0.001 | 1.34 (1.14–1.58) | <0.001 |
| 5 to 12 years | 1.02 (0.85–1.22) | 0.82 | 1.02 (0.85–1.23) | 0.81 |
| 13 to 17 years | REF | REF | ||
| Race/Ethnicity | ||||
| Non-Hispanic White | REF | REF | ||
| Non-Hispanic Black | 1.13 (1.03–1.24) | 0.01 | 1.11 (1–1.23) | 0.06 |
| Hispanic | 1.52 (1.38–1.67) | < 0.001 | 1.34 (1.2–1.5) | < 0.001 |
| Other | 1.02 (0.91–1.15) | 0.70 | 1.02 (0.9–1.15) | 0.81 |
| Payer | ||||
| Private | REF | REF | ||
| Government | 1.41 (1.30–1.54) | < 0.001 | 1.21 (1.1–1.33) | < 0.001 |
| Other Payer | 1.15 (0.99–1.34) | 0.07 | 0.99 (0.84–1.17) | 0.93 |
| Discharge Status | ||||
| Home | 1.04 (0.95–1.13) | 0.42 | 1.19 (1.08–1.32) | 0.001 |
| Post-acute care facility | REF | REF | ||
| Discharge Season | ||||
| January–March | REF | REF | ||
| April–June | 0.97 (0.88–1.08) | 0.59 | 0.98 (0.88–1.08) | 0.62 |
| July–September | 0.97 (0.88–1.08) | 0.62 | 1.02 (0.91–1.13) | 0.78 |
| October–December | 1 (0.90–1.11) | 1 | 1.01 (0.91–1.11) | 0.93 |
| # Complex Chronic Conditions | ||||
| 0 | REF | REF | ||
| 1 | 1.43 (0.96–2.12) | 0.08 | 1.48 (1–2.2) | 0.05 |
| 2 | 1.96 (1.35–2.85) | < 0.001 | 1.87 (1.28–2.73) | 0.001 |
| 3 or more | 2.16 (1.49–3.11) | < 0.001 | 1.96 (1.34–2.86) | < 0.001 |
| Risk Adjustment for Congenital Heart Surgery Score | ||||
| No Cardiac Surgery | REF | REF | ||
| RACHS Score unassigned | 0.95 (0.79–1.15) | 0.63 | 0.94 (0.77–1.15) | 0.56 |
| Lower risk (1 through 3) | 0.87 (0.73–1.04) | 0.12 | 0.84 (0.7–1) | 0.05 |
| Higher risk (4 through 6) | 0.96 (0.74–1.24) | 0.74 | 1 (0.76–1.31) | 0.99 |
| Underlying Medical Conditions | ||||
| History of Prematurity | 0.90 (0.82–0.99) | 0.03 | 0.99 (0.89–1.11) | 0.91 |
| Upper Airway Obstruction | 1.04 (0.96–1.12) | 0.37 | 1.01 (0.93–1.1) | 0.76 |
| Chronic Lung Disease | 0.99 (0.92–1.06) | 0.71 | 0.95 (0.87–1.03) | 0.19 |
| Neurologic | 1.39 (1.29–1.49) | < 0.001 | 1.29 (1.19–1.4) | < 0.001 |
| Trauma | 0.86 (0.73–1.02) | 0.09 | 0.83 (0.69–1) | 0.04 |
| Gastrostomy tube Diagnosis Code | 1.23 (1.14–1.33) | < 0.001 | 1.15 (1.05–1.26) | 0.002 |
| Gastrostomy tube Procedure Code | 1.04 (0.96–1.11) | 0.34 | 1.04 (0.95–1.13) | 0.39 |
| Ventilator dependency | 0.99 (0.91–1.07) | 0.72 | 0.88 (0.81–0.97) | 0.01 |
In unadjusted analysis, patient demographic characteristics associated with increased risk for bRTI readmission included admission age less than five years old, Hispanic or non-Hispanic Black race/ethnicity, and government payer status. In multivariable Cox proportion model analysis, certain demographic variables continued to be independently associated with increased risk for hospital readmission due to a bRTI; these included admission age less than five years [e.g., <30 days (aHR 1.3; 95% CI 1.1–1.6)], Hispanic race/ethnicity (aHR 1.3; 95% CI 1.2–1.5), and government payer status (aHR 1.2; 95% CI 1.1–1.3).
Discharge characteristics and bRTI hospital readmission (Table 2)
While not associated on unadjusted analysis, when controlling for other variables, discharge to home, when compared to post-acute care facility, was associated with increased hazard for hospital readmission for a bRTI (aHR=1.2; 95% CI 1.1–1.3). There was no differential association between discharge location and bRTI hospital readmission risk, as the interaction term for ventilator dependency and discharge to a post-acute care facility was not significant (p=0.99). Discharge season was not associated with bRTI hospital readmission on unadjusted or adjusted analyses.
Clinical comorbidities and bRTI hospital readmission (Table 2)
With respect to the relationship between clinical comorbidities and bRTI readmission, specific underlying medical conditions were associated with differential risk of bRTI readmission. For example, on adjusted analyses, neurologic comorbidity (aHR 1.3; 95% CI 1.2–1.4) and gastrostomy tube dependency prior to the index hospitalization (aHR 1.2; 95% CI 1.1–1.3) were associated with higher risk of bRTI hospital readmission, while having a comorbid trauma diagnosis (aHR 0.83; 95% CI 0.69–1) and ventilator dependency (aHR 0.88; 95% CI 0.81–0.97) were associated with decreased risk. Interestingly, history of prematurity was associated with decreased risk for hospital readmission for a bRTI on bivariate analysis; however, this relationship did not continue in multivariable analysis. When examining the association between cardiac surgery and differential bRTI hospital readmission risk, patients who underwent lower risk cardiac surgery (RACHS score 1–3) had lower risk for post-tracheotomy bRTI hospital readmission (aHR 0.84; 95% CI 0.7–1). Other comorbidities associated with indication for tracheotomy (e.g., upper airway obstruction, chronic lung disease) were not associated with hospital readmission for a tracheostomy-associated bRTI on unadjusted or adjusted analyses.
Discussion
In this multicenter study of pediatric patients undergoing tracheotomy at freestanding U.S. children’s hospitals, subsequent hospital readmission for a bRTI was common. Specific risk factors associated with increased risk for readmission due to a bRTI included the demographic factors of younger age, Hispanic ethnicity, government payer status and discharge to home post-tracheotomy, as well as clinical characteristics of multiple complex chronic conditions, neuromuscular comorbidity and presence of gastrostomy tube. Some factors were associated with decreased risk for readmission for a bRTI, including congenital heart surgery repair during the index hospitalization, trauma comorbidity, and chronic ventilator dependence. The observed median time for bRTI hospital readmission in the current study was longer than a previous, single-center study of post-tracheotomy bRTI readmission.8
Increased risk of hospital readmission for a bRTI and poorer outcomes in children with younger age, Hispanic ethnicity and government payer status complements findings of previous studies8,12,14,15,22–24 and highlight potential opportunities to optimize outpatient care access and management of this complex patient population. For example, because frequent hospitalizations may impact attendance at outpatient preventative care visits for vaccinations, opportunities may exist to increase vaccination coverage rates by giving age-appropriate vaccinations on the inpatient setting or at subspecialty outpatient appointments. Unfortunately the PHIS database does not provide vaccination status, limiting our ability to explore this association. Additionally, younger patients at hospital admission for tracheotomy may have increased risk for bRTI-related hospital readmissions due to lower pulmonary reserves, smaller airways and tracheostomy size that impact airway clearance, immature immune systems, or a lower threshold of hospitalization when experiencing respiratory illness.
The differential risk for Hispanic patients seen in our study may be influenced by differential access to consistent outpatient care, language barriers, or other factors. Previous literature has demonstrated health care disparities in Latino/Hispanic population, including that they are more likely to be uninsured or sporadically insured25,26, less likely to have a usual source of care25,26, and have decreased odds of having had a physician visit in the previous year25. Additionally, language barriers may impact quality of care, as previous literature has demonstrated that language is the single greatest barrier to care for Latino/Hispanic children27 and that Latino patients were most likely to need interpreters for communication with primary providers26. Further exploration of the intersection between demographic factors and subsequent bRTI hospital readmission risk in children undergoing tracheotomy is warranted to better understand these issues.
Findings of increased readmission risk for those discharged home, when compared to post-acute care facilities, complements additional emerging evidence that these post-discharge health services, such as increased access to sub-acute and skilled nursing facilities, might help prevent subsequent acute-care hospitalizations in children with medical complexity, particularly in patients post-tracheotomy10. Previous studies have demonstrated that post-acute care use in pediatric patients is uncommon, even for CMC21,28,29. Additionally, Hispanic ethnicity has also been associated with decreased use of post-acute care facilities in pediatric patients21,28,29. Our results may support future research to examine the association between availability and use of post-acute care facilities to prevent future bRTI hospital readmissions in this patient population.
There are several reasons that might explain why specific medical comorbidities may be associated with differential risk bRTI hospital readmission. Through respiratory muscle weakness, impairment of the cough reflex, and restrictive lung disease caused by kyphoscoliosis, neuromuscular disease increases the risk of respiratory disease, aspiration and lung atelectasis.30,31 In children with neurological disorders, previous studies have demonstrated increased risk of respiratory-infection related hospitalizations,32 respiratory failure,33 and ICU admission.34 In contrast, medical comorbidities associated with lower risk of readmission for a bRTI included lower risk congenital heart surgery repair during the index admission and chronic ventilator dependency. Although previous studies have demonstrated that congenital heart disease is associated with increased risk for in-hospital mortality after tracheotomy,1 RACHS scoring was not used in these studies to evaluate the association between severity of congenital heart disease lesions and mortality. We suspect that repair of lower-mortality risk cardiac lesions (e.g., patent ductus arteriosus, ventricular septal defect) may restore appropriate cardiac blood flow and systemic oxygenation, decreasing the risks of hospitalization for respiratory-related illness, while those with more severe lesions (e.g., hypoplastic left heart) remain at high risk of hospital readmission for bRTIs. With respect to the finding of lower risk of bRTI hospital readmission for patients on positive-pressure ventilation, we hypothesize that, as a closed system, positive-pressure ventilation may decrease exposure to aerosolized microbes and decrease atelectasis and lower airway plugging through forced lung expansion. Additionally, those on chronic positive-pressure mechanical ventilation may be more likely to have closer outpatient follow-up with lower threshold for starting outpatient antibiotics for suspected bRTIs.
There are several limitations to the current study. The retrospective nature limited the specific data available for analysis and only allows for identification of associations of variables of interest and our primary outcome. Thus, there are likely unmeasured confounders not captured in PHIS (e.g., bacterial colonization, home medications), for which prior studies have accounted8 and that may influence the association between predictors and subsequent bRTI hospital readmission. Because the PHIS database only contains administrative data from 48 children’s hospitals, we do not have any information about hospitalizations or other encounters at non-PHIS participating hospitals. Therefore, our study sample is not representative of all children with tracheostomy and may contain more severely ill, medically complex or publicly-insured patients. There are likely unidentified respiratory infections hospital readmissions, as some patients included in the analysis may have had bRTI hospital readmissions at non-PHIS regional hospitals. For example, some children may have been discharged to a long-term care facility with an established relationship with a non-PHIS hospital. However, one recent study demonstrated that pediatric patients with respiratory complex chronic indicator ICD-9-CM diagnosis codes were less likely to experience readmission to a different hospital35. Additionally, the identified factors for bRTI-related hospital readmission may predict all-cause hospital readmission in the pediatric post-tracheotomy population and, therefore, may not be specific to respiratory infection-related hospital readmission. For example, previous studies have demonstrated similar associations between younger age, chronic mechanical ventilation and 30-day all-cause readmission after tracheotomy10.
Perhaps the largest limitation of the current study the reliance on accurate coding of bRTIs in the PHIS database. To define our outcome of interest, we only labeled follow-up visits as due to a bRTI if they had appropriate ICD-9-CM codes and treatment with antibiotics used in previous studies11–16. Unfortunately, PHIS does not provide any microbiology testing results and we are unable to detect bacterial culture or gram stain results, limiting our ability to assess for acute infection versus chronic colonization. We also recognize the possibility that our study may have misclassified some patients with viral respiratory infections as having bacterial respiratory tract infections. However, in previous studies, the vast majority of the population included in the current study have a bacterial respiratory culture sent upon admission for a suspected bRTI,16 increasing identification of a bacterial respiratory pathogen and decreasing the likelihood of misclassification. While we recognize that hospitalizations for viral respiratory tract infections also represent resource utilization, in contrast to bacterial infections, there are fewer antimicrobial interventions (e.g., antibiotics) that might prevent worsening disease if initiated early. Further, on additional query of the PHIS database, pediatric patients with tracheostomy discharged with only a viral lower respiratory tract primary ICD-9-CM code (and no secondary bacterial respiratory tract code) represent less than 10% of all RTI admissions.
Conclusions
We have demonstrated that young, Hispanic children with multiple complex chronic conditions who use Medicaid insurance and are discharged home are at the highest risk for post-tracheotomy bacterial respiratory tract infections hospital readmission. Physicians, including pediatric intensivists, neonatologists, otorhinolaryngologists and pediatric hospitalists, in consultation with other members of the multidisciplinary teams, may use this information for patients with tracheostomy to counsel about risk of bRTI hospitalization post-tracheotomy. Given the overall high rate of readmission for bRTI post-tracheotomy, future research should investigate prevention strategies in patient populations at higher risk for bRTI. In addition to primary bRTI prevention, future research should explore care delivery to Hispanic pediatric patients with tracheostomy and explore specific factors that contribute to the disparities identified in this study.
Supplementary Material
Supplemental Table 1. ICD-9-CM codes used for patient inclusion.
Acknowledgments
Funding source: Dr. Russell is a KL2 Scholar awarded under the KL2 Mentoring Research Career Development Award through Southern California Clinical and Translational Science Institute at University of Southern California, Keck School of Medicine. The project described was supported by the National Center for Advancing Translational Sciences, National Institutes of Health (NIH), through Grant Award Number KL2TR000131 and through the Academic Pediatric Association’s Young Investigator Award. The content is solely the responsibility of the author(s) and does not necessarily represent the official view of the NIH.
Abbreviations
- aHR
adjusted hazard ratio
- bRTI
bacterial respiratory tract infection(s)
- ICD
International Classification of Diseases
- ICU
intensive care unit
- IQR
interquartile range
- LOS
length of stay
- PHIS
Pediatric Health Information System
Footnotes
Financial Disclosure: The authors have no financial relationships relevant to this article to disclose.
Conflicts of Interest: The authors have no conflicts of interest relevant to this article to disclose.
Contributors’ Statement:
Dr. Russell conceptualized and designed the study, drafted the analytic plan and the initial manuscript, and approved the final manuscript as submitted.
Drs. Thurm and Hall created the database, conducted the statistical analyses, revised the manuscript and approved the final manuscript as submitted.
Drs. Simon, Neely and Berry conceptualized the study, reviewed and critically revised the manuscript and approved the final manuscript as submitted.
References
- 1.Berry JG, Graham RJ, Roberson DW, Rhein L, Graham DA, Zhou J, O'Brien J, Putney H, Goldmann DA. Patient characteristics associated with in-hospital mortality in children following tracheotomy. Arch Dis Child. 2010;95(9):703–710. doi: 10.1136/adc.2009.180836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lewis CW, Carron JD, Perkins JA, Sie KC, Feudtner C. Tracheotomy in pediatric patients: a national perspective. Arch Otolaryngol Head Neck Surg. 2003;129(5):523–529. doi: 10.1001/archotol.129.5.523. [DOI] [PubMed] [Google Scholar]
- 3.Zhu H, Das P, Roberson DW, Jang J, Skinner ML, Paine M, Yuan J, Berry J. Hospitalizations in children with preexisting tracheostomy: a national perspective. Laryngoscope. 2015;125(2):462–468. doi: 10.1002/lary.24797. [DOI] [PubMed] [Google Scholar]
- 4.Carnevale FA, Alexander E, Davis M, Rennick J, Troini R. Pediatrics. Vol. 117. United States; 2006. Daily living with distress and enrichment: the moral experience of families with ventilator-assisted children at home; pp. e48–60. [DOI] [PubMed] [Google Scholar]
- 5.Hartnick CJ, Bissell C, Parsons SK. The impact of pediatric tracheotomy on parental caregiver burden and health status. Arch Otolaryngol Head Neck Surg. 2003;129(10):1065–1069. doi: 10.1001/archotol.129.10.1065. [DOI] [PubMed] [Google Scholar]
- 6.Mah JK, Thannhauser JE, Kolski H, Dewey D. Parental stress and quality of life in children with neuromuscular disease. Pediatr Neurol. 2008;39(2):102–107. doi: 10.1016/j.pediatrneurol.2008.04.011. [DOI] [PubMed] [Google Scholar]
- 7.Mah JK, Thannhauser JE, McNeil DA, Dewey D. Being the lifeline: the parent experience of caring for a child with neuromuscular disease on home mechanical ventilation. Neuromuscul Disord. 2008;18(12):983–988. doi: 10.1016/j.nmd.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 8.Russell CJ, Simon TD, Mamey MR, Newth CJL, Neely MN. Pseudomonas aeruginosa and post-tracheotomy bacterial respiratory tract infection readmissions. Pediatr Pulmonol. 2017;52(9):1212–1218. doi: 10.1002/ppul.23716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pennington A, Dobies CG. PHIS Description when Referenced as Data Source. 2014 [Google Scholar]
- 10.Berry JG, Graham DA, Graham RJ, Zhou J, Putney HL, O'Brien JE, Roberson DW, Goldmann DA. Predictors of clinical outcomes and hospital resource use of children after tracheotomy. Pediatrics. 2009;124(2):563–572. doi: 10.1542/peds.2008-3491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brogan TV, Hall M, Williams DJ, Neuman MI, Grijalva CG, Farris RW, Shah SS. Variability in processes of care and outcomes among children hospitalized with community-acquired pneumonia. Pediatr Infect Dis J. 2012;31(10):1036–1041. doi: 10.1097/INF.0b013e31825f2b10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Neuman MI, Hall M, Gay JC, Blaschke AJ, Williams DJ, Parikh K, Hersh AL, Brogan TV, Gerber JS, Grijalva CG, Shah SS. Readmissions among children previously hospitalized with pneumonia. Pediatrics. 2014;134(1):100–109. doi: 10.1542/peds.2014-0331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hirsch AW, Monuteaux MC, Fruchtman G, Bachur RG, Neuman MI. Characteristics of Children Hospitalized With Aspiration Pneumonia. Hosp Pediatr. 2016;6(11):659–666. doi: 10.1542/hpeds.2016-0064. [DOI] [PubMed] [Google Scholar]
- 14.Thomson J, Hall M, Ambroggio L, Stone B, Srivastava R, Shah SS, Berry JG. Aspiration and Non-Aspiration Pneumonia in Hospitalized Children With Neurologic Impairment. Pediatrics. 2016;137(2):1–10. doi: 10.1542/peds.2015-1612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thomson J, Hall M, Berry JG, Stone B, Ambroggio L, Srivastava R, Shah SS. Diagnostic Testing and Hospital Outcomes of Children with Neurologic Impairment and Bacterial Pneumonia. J Pediatr. 2016;178:156–163.e151. doi: 10.1016/j.jpeds.2016.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Russell CJ, Mack WJ, Schrager SM, Wu S. Care Variations and Outcomes for Children Hospitalized With Bacterial Tracheostomy-Associated Respiratory Infections. Hosp Pediatr. 2017;7(1):16–23. doi: 10.1542/hpeds.2016-0104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Feudtner C, Feinstein JA, Zhong W, Hall M, Dai D. Pediatric complex chronic conditions classification system version 2: updated for ICD-10 and complex medical technology dependence and transplantation. BMC Pediatr. 2014;14:199. doi: 10.1186/1471-2431-14-199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barnhart DC, Hall M, Mahant S, Goldin AB, Berry JG, Faix RG, Dean JM, Srivastava R. Effectiveness of fundoplication at the time of gastrostomy in infants with neurological impairment. JAMA Pediatr. 2013;167(10):911–918. doi: 10.1001/jamapediatrics.2013.334. [DOI] [PubMed] [Google Scholar]
- 19.Srivastava R, Berry JG, Hall M, Downey EC, O'Gorman M, Dean JM, Barnhart DC. Reflux related hospital admissions after fundoplication in children with neurological impairment: retrospective cohort study. Bmj. 2009;339:b4411. doi: 10.1136/bmj.b4411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jenkins KJ, Gauvreau K, Newburger JW, Spray TL, Moller JH, Iezzoni LI. Consensus-based method for risk adjustment for surgery for congenital heart disease. J Thorac Cardiovasc Surg. 2002;123(1):110–118. doi: 10.1067/mtc.2002.119064. [DOI] [PubMed] [Google Scholar]
- 21.Berry J, Wilson K, Dumas H, Simpser E, O'Brien J, Whitford K, May R, Mittal V, Murphy N, Steinhorn D, Agrawal R, Rehm K, Marks M, Traul C, Dribbon M, Haines C, Hall M. Use of Post-Acute Facility Care in Children Hospitalized With Acute Respiratory Illness. J Hosp Med. 2017;12(8):626–631. doi: 10.12788/jhm.2780. [DOI] [PubMed] [Google Scholar]
- 22.Lu S, Kuo DZ. Hospital charges of potentially preventable pediatric hospitalizations. Acad Pediatr. 2012;12(5):436–444. doi: 10.1016/j.acap.2012.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Leyenaar JK, Lagu T, Shieh MS, Pekow PS, Lindenauer PK. Variation in resource utilization for the management of uncomplicated community-acquired pneumonia across community and children's hospitals. J Pediatr. 2014;165(3):585–591. doi: 10.1016/j.jpeds.2014.04.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pati S, Lorch SA, Lee GE, Sheffler-Collins S, Shah SS. Health insurance and length of stay for children hospitalized with community-acquired pneumonia. J Hosp Med. 2012;7(4):304–310. doi: 10.1002/jhm.959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Flores G, Tomany-Korman SC. Racial and ethnic disparities in medical and dental health, access to care, and use of services in US children. Pediatrics. 2008;121(2):e286–298. doi: 10.1542/peds.2007-1243. [DOI] [PubMed] [Google Scholar]
- 26.Flores G, Lin H. Trends in racial/ethnic disparities in medical and oral health, access to care, and use of services in US children: has anything changed over the years? Int J Equity Health. 2013;12:10. doi: 10.1186/1475-9276-12-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Flores G, Abreu M, Olivar MA, Kastner B. Access barriers to health care for Latino children. Arch Pediatr Adolesc Med. 1998;152(11):1119–1125. doi: 10.1001/archpedi.152.11.1119. [DOI] [PubMed] [Google Scholar]
- 28.Berry JG, Hall M, Dumas H, Simpser E, Whitford K, Wilson KM, O'Neill M, Mittal V, Agrawal R, Dribbon M, Haines CJ, Traul C, Marks M, O'Brien J. Pediatric Hospital Discharges to Home Health and Postacute Facility Care: A National Study. JAMA Pediatr. 2016;170(4):326–333. doi: 10.1001/jamapediatrics.2015.4836. [DOI] [PubMed] [Google Scholar]
- 29.Phillips CD, Truong C, Kum HC, Nwaiwu O, Ohsfeldt R. Post-acute care for children with special health care needs. Disabil Health J. 2017 Sep 8; doi: 10.1016/j.dhjo.2017.08.010. pii: S1936-6574(17)30164-4. [DOI] [PubMed] [Google Scholar]
- 30.Seddon PC, Khan Y. Respiratory problems in children with neurological impairment. Arch Dis Child. 2003;88(1):75–78. doi: 10.1136/adc.88.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Weir KA, McMahon S, Taylor S, Chang AB. Oropharyngeal aspiration and silent aspiration in children. Chest. 2011;140(3):589–597. doi: 10.1378/chest.10-1618. [DOI] [PubMed] [Google Scholar]
- 32.Havers F, Fry AM, Chen J, Christensen D, Moore C, Peacock G, Finelli L, Reed C. Hospitalizations Attributable to Respiratory Infections among Children with Neurologic Disorders. J Pediatr. 2016;170 doi: 10.1016/j.jpeds.2015.11.030. 135-141.e131-135. [DOI] [PubMed] [Google Scholar]
- 33.Keren R, Zaoutis TE, Bridges CB, Herrera G, Watson BM, Wheeler AB, Licht DJ, Luan XQ, Coffin SE. Neurological and neuromuscular disease as a risk factor for respiratory failure in children hospitalized with influenza infection. Jama. 2005;294(17):2188–2194. doi: 10.1001/jama.294.17.2188. [DOI] [PubMed] [Google Scholar]
- 34.Millman AJ, Finelli L, Bramley AM, Peacock G, Williams DJ, Arnold SR, Grijalva CG, Anderson EJ, McCullers JA, Ampofo K, Pavia AT, Edwards KM, Jain S. Community-Acquired Pneumonia Hospitalization among Children with Neurologic Disorders. J Pediatr. 2016;173:188–195.e184. doi: 10.1016/j.jpeds.2016.02.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Khan A, Nakamura MM, Zaslavsky AM, Jang J, Berry JG, Feng JY, Schuster MA. Same-Hospital Readmission Rates as a Measure of Pediatric Quality of Care. JAMA Pediatr. 2015;169(10):905–912. doi: 10.1001/jamapediatrics.2015.1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Table 1. ICD-9-CM codes used for patient inclusion.


