Abstract
In sub-Saharan Africa, self-disclosure of HIV-positive status may be a pivotal action for improving access to prevention of mother-to-child transmission services. However, understanding of HIV stigma, disclosure, and their effects on demand for care remains incomplete – particularly in the current context of new antiretroviral therapy guidelines. The purpose of this study was to explore these issues among self-disclosed couples living in southwest Kenya. We conducted 38 in-depth interviews with HIV-positive pregnant or postpartum women and their male partners. Of the 19 couples, ten were HIV seroconcordant and nine were serodiscordant. The textual analysis showed that HIV stigma continues to restrict full participation in community life and limit access to care by promoting fear, isolation, and self-censorship. Against this backdrop, however, the participants’ narratives revealed varying forms and degrees of resistance to HIV stigma, which appeared to both produce and emerge from acts of self-disclosure. Such disclosure enabled participants to overcome fears and gain critical support for engaging in HIV care while further resisting HIV stigma. These findings suggest that programme interventions designed explicitly to stimulate and support processes of HIV stigma resistance and safe self-disclosure may be key to improving demand for and retention in HIV services.
Keywords: HIV, prevention, maternal-to-child transmission, HIV, stigma, disclosure, Kenya
Introduction
Across sub-Saharan Africa, much progress has been made in expanding the availability of services to prevent mother-to-child transmission of HIV and to treat HIV generally. By 2015, 20 out of the region’s 21 priority countries of the Global Plan toward eliminating new HIV infections had adopted the WHO 2013 guideline for Option B+: lifelong antiretroviral therapy (ART) for all HIV-infected pregnant or breastfeeding women, regardless of CD4 count or WHO clinical stage. ART coverage is currently estimated at 77% for pregnant and breastfeeding women, but consistent access to and use of ART among this population is still suboptimal (UNAIDS 2016). Such underuse contributes to inadequate viral suppression, which affects an estimated three-quarters of all HIV-infected adults in the region and results in horizontal as well as vertical transmission (UNAIDS 2013). To respond to this situation adequately, we continue to need a better understanding of the demand-side factors that shape uptake and continuation of prevention of maternal-to-child transmission and HIV care.
One factor that has greatly influenced demand for and access to HIV care is HIV stigma – the devaluing of persons identified as having HIV that reproduces social difference and results in social exclusion (Parker and Aggleton 2003). Adverse effects of HIV stigma are thought to be specifically generated through mechanisms of anticipated, enacted, and internalised stigma (Earnshaw and Chaudoir 2009). A number of theoretical frameworks propose pathways through which HIV stigma determines health behaviour and outcomes (Castro and Farmer 2005; Mbonu, Van den Borne and De Vries 2009; Parker and Aggleton 2003; Turan et al. 2017). In particular, Turan and Nyblade (2013) offer a framework that considers the behavioural effects of HIV stigma at each point along the prevention of maternal-to-child transmission intervention cascade – from accepting HIV testing during antenatal care to practicing high ART adherence and safe breastfeeding following birth. According to this framework, fear and shame from anticipated and internalised stigma can cause HIV-infected individuals to hide their status from those around them, and can prevent many people (regardless of HIV status) from seeking and receiving essential services.
Contrary to this tendency towards secrecy and silence, self-disclosure of HIV-positive status may be a pivotal action for improving the use of prevention of maternal-to-child transmission services, HIV care more generally, and ART adherence. Research in sub-Saharan Africa suggests that such disclosure – particularly to sexual partners but also to family and others – significantly increases the likelihood of women using both prevention of maternal-to-child transmission and maternal health services (Kalembo et al. 2013; Kirsten et al. 2011; Spangler et al. 2014). Conversely, nondisclosure can limit women’s ability to adhere to prevention of maternal-to-child transmission programmes, and prevent HIV transmission to partners with a negative serostatus (Desgrées-du-Loû et al. 2009; Jasseron et al. 2013; Medley et al. 2004). Partner disclosure has been associated with increased risk-reduction behaviour and partner HIV testing, as well as improved mental health and perceived social support (Deribe et al. 2008; King et al. 2008; Maman et al. 2003; Medley et al. 2004). Much of this research indicates that anticipated stigma (i.e., fear of negative consequences such as conflict, separation, and violence) often inhibits disclosure but that the feared outcomes are often not realised once disclosure occurs.
Estimates of HIV-positive status disclosure in sub-Saharan Africa range widely; 22–96% of adults disclose to anybody, 28–91% disclose to sexual partners, 60–75% disclose to family, and 6–43% disclose to friends (Obermeyer, Baijal and Pegurri 2011). This variation may partly result from the complexity of disclosure, which can be deliberate or unintentional, voluntary or imposed, direct or indirect, partial or full, or somewhere between these different dimensions (Obermeyer, Baijal and Pegurri 2011; Pride 2013). Rather than being a discrete event, disclosure appears to unfold as a process that is initiated with a single person and then gradually expands to encompass wider social networks. HIV stigma appears to have a negative effect on this process; for example, one study in Uganda found that people experiencing more internalised stigma were less likely to disclose their HIV-positive status than those experiencing less stigma, and that the magnitude of this association increased with social distance in relationships (Tsai et al. 2013).
Despite a wealth of knowledge regarding HIV stigma and increasing insights into HIV status disclosure, our understanding of these processes and the ways in which they influence each other – as well as participation in HIV services – is still incomplete. Particularly lacking is knowledge about people’s varied responses to stigma and how these responses are produced in the current context of sub-Saharan Africa, which is characterised by new treatment guidelines, new models of service delivery, increased HIV awareness and availability of ART, and improved health outcomes. The purpose of this study was thus to explore current perceptions of HIV stigma, self-disclosure, and their effects on engagement in prevention of maternal-to-child transmission and HIV care among self-disclosed couples in southwest Kenya – an area with an estimated 15% HIV prevalence (National AIDS and STI Control Programme 2012) that was transitioning to Option B+ at the time of data collection.
Methods
To achieve the study objectives, we conducted 40 in-depth interviews at four health facilities in southwest Kenya (Homa Bay, Kisumu and Migori counties) between September and November 2014. These health facilities were selected for their centrality and large client volume. Twenty interviews were conducted with five women from each facility who were at least 18 years old, currently pregnant or postpartum (within six weeks of birth), and had a known HIV-positive status. Women who met these three criteria were identified through facility registers in consultation with health facility staff. Beyond these criteria, sampling was purposive only in the sense that we sought an approximately even number of women in HIV seroconcordant and serodiscordant relationships. Another 20 interviews were conducted with male partners of these women who were at least 18 years old, aware of their own HIV status, and aware of their partner’s HIV status. Women who agreed to participate were asked if they would be willing to have their male partner contacted regarding potential participation in an interview. These men were contacted only if the woman reported that she had already disclosed her HIV status to him, and after getting her explicit permission to contact him. Of the 40 participants, two (one man, one woman) were later found to not be in a partner relationship with any other participant and were therefore excluded from the current analysis, giving a total of 19 self-disclosed married couples.
Before conducting the interviews, a semi-structured interview guide was developed, pretested, and refined by the Kenyan and US investigators. This guide was based on their extensive experience with the study region and topics (including a comprehensive literature review), and was designed specifically to elicit perceptions of HIV stigma, HIV-status disclosure, and facilitators and inhibitors for engagement in prevention of maternal-to-child transmission and HIV care. Each interview was conducted in a private setting (health facility or home) by a gender-matched interviewer in the participant’s preferred language (English, Luo or Kiswahili). The interviewers were all Kenyans with prior experience in qualitative interviewing, who received additional training in study-specific procedures from one of the study investigators (JMT). To allow for free expression of views and for comparison of independently expressed perspectives within the couples, it was decided that each participant would be interviewed individually. Ethical approval for the study was obtained from the Kenya Medical Research Institute (KEMRI) Ethical Review Committee, the Institutional Review Board at the University of Alabama at Birmingham, and the Institutional Review Board at the University of Colorado Denver.
Interview transcripts were coded in the Dedoose qualitative software program (Dedoose Version 5.0.11 2014) by a team of three doctoral-level researchers (SAS, AH, PM) with considerable knowledge of sexual and reproductive health research in Africa, and in qualitative coding using a constant comparative approach (Charmaz 2014). Broad domains and initial codes were agreed upon based on the semi-structured interview guide. Once initial coding was complete, the transcripts were finely coded and themes identified using inductive thematic analysis. Feedback on coding and on developing themes was obtained from local research team members on frequent study calls. Finalised themes were compared and contrasted across all participants in terms of sociodemographic characteristics, as well as among women, among men, and within and between couples (seroconcordant and serodiscordant, monogamous and polygamous). Detailed descriptions of the themes were then written, after which inferences were made and situated within the broader literature.
Results
Participant characteristics are shown in Table 1. Of the women, 12 (63%) were pregnant and seven (37%) were postpartum; nearly three-fourths reported the pregnancy as being unplanned, but only about one-third of the men felt this way. All participants were currently living with their spouse (their partner in this study), and three couples (16%) were in a polygamous marriage. Ten couples (53%) were HIV seroconcordant and nine (47%) were HIV serodiscordant. Overall, our analysis did not reveal highly distinct patterns within or between couples, including couple HIV status (seroconcordant or serodiscordant) and marriage type (monogamous or polygamous). However, the analysis did reveal important patterns among the study participants as a whole and, to some extent, by gender. These results are organised by three domains: perceptions of HIV stigma, self-disclosure of HIV-positive status, and support for engagement in prevention of maternal-to-child transmission and HIV care. The names associated with the selected quotes are pseudonyms that were assigned to each participant to protect their identity.
Table 1.
Characteristics of the study participants; n (%)
| Women n = 19 |
Men n = 19 |
Total n = 38 |
|
|---|---|---|---|
|
| |||
| Pregnancy status | |||
|
| |||
| Pregnant (≥ 14 weeks) | 12 (63.2) | ||
| Postpartum (< 6 weeks) | 7 (36.8) | ||
|
| |||
| Pregnancy intendedness | |||
|
| |||
| Planned | 5 (26.3) | 13 (68.4) | 18 (47.4) |
| Unplanned | 14 (73.7) | 6 (31.6) | 20 (52.6) |
|
| |||
| Age group | |||
|
| |||
| 18-25 years | 14 (73.7) | 4 (21.1) | 18 (47.4) |
| 26-33 years | 4 (21.1) | 6 (31.6) | 10 (26.3) |
| 34-41 years | 1 (5.3) | 7 (36.8) | 8 (21.1) |
| ≥ 42 years | 0 (0.0) | 2 (10.5) | 2 (5.3) |
|
| |||
| Educational level | |||
|
| |||
| Incomplete primary | 11 (57.9) | 6 (31.6) | 17 (44.7) |
| Complete primary | 4 (21.1) | 6 (31.6) | 10 (26.3) |
| Incomplete secondary | 1 (5.3) | 3 (15.8) | 4 (10.5) |
| Complete secondary | 3 (15.8) | 4 (21.1) | 7 (18.4) |
|
| |||
| Occupation | |||
|
| |||
| Agriculture/fishing | 4 (21.1) | 9 (47.4) | 13 (34.2) |
| Housework | 9 (47.4) | 0 (0.0) | 9 (23.7) |
| Skilled labor/artisanal | 1 (5.3) | 8 (42.1) | 9 (23.7) |
| Small business | 5 (26.3) | 2 (10.5) | 7 (18.4) |
|
| |||
| Couple’s marriage type | |||
|
| |||
| Monogamous | 16 (84.2) | 16 (84.2) | 32 (84.2) |
| Polygamous | 3 (15.8) | 3 (15.8) | 6 (15.8) |
|
| |||
| Couple’s HIV status | |||
|
| |||
| Concordant | 10 (52.6) | 10 (52.6) | 20 (52.6) |
| Discordant | 9 (47.4) | 9 (47.4) | 18 (47.4) |
Perceptions of and Responses to HIV Stigma
The prevailing perception among participants was that HIV stigma – anticipated, enacted, and internalised – persists in southwest Kenya and continues to have an adverse impact on people living with this disease. Among the most prominent of these effects was an inability to participate fully in community life. Some participants expressed this theme in terms of being “half dead,” an impaired state that manifested in fears of being excluded from family and community, perceived experiences of this exclusion, and subsequent self-censorship or withdrawal from social activity. A sub-theme representing a fundamental aspect of reduced societal participation was fear of being undesirable to current or future sexual partners. Among men, apprehension related to loss of social standing was also common. Such fears reiterate the complex intersections of HIV stigma with social and material positioning and their respective markers of belonging and not belonging.
The community disrespects people with HIV. Even if you are alive, they believe that you are half dead. They do not consider you in future plans. They do not care if you will be around or not – Fahim, 27 y/o man in seroconcordant couple
People fear being identified with HIV because they will feel isolated from the rest of the community. Once you have this illness, you are waiting for your death. You tend to hide – Amira, 32 y/o woman in serodiscordant couple
We young people especially suffer from stigma. The men think that the young ladies around will find out and reject them, and vice versa – Mashuhuri 23 y/o man in seroconcordant couple
When you are one who has prospered [in the village], your reputation might be watered down. I am forced to keep my HIV status secret from the community so that I can keep my reputation – Juma, 32 y/o man in seroconcordant couple
Regarding HIV stigma and engagement in prevention of maternal-to-child transmission and HIV care, the analysis revealed significant concern over being recognised at the HIV clinic, which allowed knowledge about one’s HIV status to escape into the community outside of one’s control. Participants were overwhelmingly in favour of Option B+, agreeing that lifelong HIV care for pregnant and breastfeeding women was the best way to protect the health of both mothers and children. However, a few women noted that the long-term commitment associated with this regimen might make their disclosure status harder to manage. To prevent unintentional disclosure, participants described behaviours of refusing to attend clinic visits, traveling to distant health facilities, and using traditional therapies. Stigma-related fears involving ART adherence were less prominent than practical issues of timing and convenience. However, participants told many stories of people – either themselves prior to self-disclosure or others who had not yet disclosed – throwing their antiretroviral drugs away, hiding drugs in their homes and workplaces, and delaying or skipping doses if unable to take them privately.
When you go to the hospital and find someone you know, this person might tell others about you. Every time you think of going back to the clinic, the fear of being recognised strikes again. – Semeni, 21 y/o woman in seroconcordant couple
With Option B+, you continue to stay in care. So, there are more opportunities for your status to be known. – Asha, 31 y/o woman in seroconcordant couple
Against this backdrop of challenges posed by ongoing HIV stigma, a more complex picture emerged. Twenty-two (58%) of the participants – eight (42%) of the women and 14 (74%) of the men with varying age, education, and couple HIV status – signalled resistance to stigma, in what appeared to be a process of overcoming fears and remaking a socially devalued identity. A critical perspective that all these participants had adopted at some point in this process was that, as one man commented, “having HIV is normal.” This normalisation of HIV took various forms, reflected in remarks about how commonplace HIV has become, how awareness about it has increased, how alike it is to other illnesses, and how HIV-infected people now have the same physical appearance and capabilities as those without this condition. Among women, the related concept of not being alone in having HIV was particularly powerful for managing stigma and adopting behaviours that supported wellbeing. The role health that workers played in providing this reassurance was readily discernible in the narratives.
This is just a disease – not a bad thing. HIV is everywhere. It can infect anybody – Nabil, 36 y/o man in seroconcordant couple
Now you cannot differentiate between who is HIV-positive and who is not. You can’t easily know because they are just normal in their bodies… In some cases, HIV-positive people look healthier than HIV-negative people – Kiki, 25 y/o woman in seroconcordant couple
We used to fear having a child but the nurses told us we could, so we decided that we would try the way others are trying. We are just normal like other people – Ismael, 36 y/o man in serodiscordant couple
At first, I knew I was as good as dead and there was no need of being alive in the world anymore… But the nurses counselled me that there are many others like me. They told me to be strong, knowing that I am not alone. This has encouraged me to come back and to be courageous – Tausi, 22 y/o woman in serodiscordant couple
Beyond attitudes involving the normalisation of HIV, 10 participants (26%) expressed more rejection or outright defiance of HIV stigma and its consequences. Particularly apparent was a belief that the value of life and health outweighs any negative consequences of stigma. Such demeanours were again more common among men than women (seven of these participants were men), but the three women in this group consistently voiced strong sentiments renouncing the fear, shame, and hiding often associated with HIV stigma. The participants sharing these more highly resistant views did not fit neatly into sociodemographic categories, and only four were in relationships with each other (one concordant and one discordant couple).
If you feel stigmatised, there is no way you will go to the clinic and sit with the others on the bench. I am saying urgently that this should not worry you! Just go to the doctor, get treated, and forget about fear – Mkamba, 28 y/o man in seroconcordant couple
Some people feel ashamed to come here, but they shouldn’t because it is their life on the line! I decided that I would not be ashamed when I come to the clinic and I would just be open about it – Amira, 32 y/o woman in serodiscordant couple
Self-disclosure of HIV-Positive Status to Partners and Others
Perceptions of decisions and actions involving disclosure of HIV-positive status were often tied to perceptions of HIV stigma. All participants indicated that it is still common for people in the community to keep their HIV status unknown to those around them, including spouses and sexual partners, family members, friends, and more distal social relations. However, this perception stood in contrast with their own stories of disclosure, which showed how – much like resistance to HIV stigma and overcoming stigma-related fears – disclosure is a process that occurs in different ways with different people over different periods of time. Because participants did not all share the same level of detail about these experiences, certain aspects of self-disclosure (i.e., decision-making, time of initial diagnosis, time from diagnosis to disclosure) are not uniformly present in the data.
Self-disclosure to spouses and other sexual partners
Of the 29 HIV-infected participants (19 women, 10 men), 14 (74%) of the women and five (50%) of the men disclosed this status to their spouse. The process was typically initiated when one partner tested positive and was then faced with the decision to tell his or her spouse – although four couples used couples counselling and testing for initial diagnosis and mutual disclosure. Anticipated stigma involving relationship damage was common in descriptions of this decision. Ten of the 14 women cited fears about relationship conflict, physical violence, and being abandoned or “chased away” by their husbands. All five men indicated fear over losing their spouse and being blamed for promiscuity, and three expressed fear of losing other sexual partners. In terms of actual consequences, most participants described encounters that were initially stressful but followed by a peaceful resolution. For some, this stress involved fear of conflict that resolved quickly when the partner was immediately supportive. Others described periods of relationship turmoil lasting from a few weeks to a few months, which more gradually settled into mutual acceptance and continuing commitment. Of three women who described significant altercations around disclosure (i.e., heated verbal exchange and temporary separation), none had permanently separated from their partner or reported physical assault or violence.
Some men are violent, and telling them has the potential to bring chaos into the family. I know the type of person I live with, so I weighed the consequences of telling him about my HIV status – Naima, 25 y/o woman in serodiscordant couple
For you to explain such a thing to your wife is a challenge because you feel that you might destabilise the marriage. She might leave and go back to her village, claiming that you brought AIDS into the marriage – Fahim, 27 y/o man in seroconcordant couple
With regards to disclosure timing, at least seven of these 19 participants told their spouse within a week of diagnosis (including those who used couples counselling and testing), and at least three others disclosed within a month. Five participants indicated that it took over six months for partner disclosure to occur. Descriptions of disclosure ranged widely: one woman called her husband from the hospital immediately upon learning her status; one man disclosed several months after diagnosis when his wife discovered his antiretroviral drugs; one woman who was born with HIV disclosed to her partner very early in the relationship, as did both partners of one couple in what turned out to be a second marriage for each. No single mechanism emerged as a primary instigating factor, such as advice from health care workers or peer mentors. However, three women who were aware of their HIV-positive status used couples counselling and testing as a way to inform their husbands. All participants articulated negative feelings about keeping one’s HIV-positive status a secret from one’s spouse/s.
There is what I call a lack of openness… This game of “hide and seek” goes on when one partner feels forced to take the drugs discreetly so that the other doesn’t find out. It is a difficult way to live – Kombo, 54 y/o man in seroconcordant couple
That is wrong! You cannot keep such a thing a secret while married. You already have the virus. It is there. And you stay with this person in the same house. How do you keep such a secret? – Hadiya, 27 y/o woman in seroconcordant couple
As described in the men’s narratives, disclosure to partner afforded the practical benefit of planning for the future, so as to enable family functioning in the face of this illness and continue on with life. Particularly important among women were the psychosocial and emotional benefits of feeling secure in the relationship. Among the participants expressing HIV stigma resistance, these themes usually appeared alongside or embedded within descriptions of this resistance – especially normalisation of HIV and prioritisation of life and health over stigma consequences. The concept of being “free” arose with great frequency in these narratives, both in terms of being free from shame and secrecy associated with HIV-related stigma, and in the interdependent sense of being free with others about one’s HIV-positive status.
Disclosure helps you and your wife make decisions about the future and get on with your life together – Juma, 32 y/o man in seroconcordant couple
Even though I knew my status, I wanted us to get tested together so he could see for himself and make an informed decision. I told myself that if he weren’t comfortable with me, I would just continue living my life… He didn’t blame or mistreat me. We decided to stay together because HIV is common and couldn’t stop our relationship – Naima, 25 y/o woman in serodiscordant couple
People may gossip about me, but I care about my life. If my husband who married me has accepted my status and I have accepted his, then there is no problem – Amira, 32 y/o woman in serodiscordant couple
You fear people will laugh at you or your wife will run away, so you try to persevere in secret. What I know is that finally it has to come to light. Before this happens, it is important that you take your wife to get tested so that both of you are free. …You just become free and take your drugs openly –Salumu, 46 y/o man in seroconcordant couple
Those people who tell their wives or husbands are people who are free – Abedi, 34 y/o man in serodiscordant couple
Self-disclosure to family and community members
Twenty-six (68%) of participants reported disclosing their own and/or their partner’s HIV-positive status to family members; this disclosure occurred either solo or jointly (with partner), and typical targets were parents, siblings, children, and co-wives. Disclosure to family was viewed as a crucial way to ensure future support in the event of disability or death. It also facilitated control of information, which included protecting children and other family members from misunderstanding and confusion about illness symptoms. All 22 participants who expressed resistance to HIV stigma were also among this group who disclosed to family members, and descriptions of this disclosure were again frequently accompanied by themes of stigma resistance.
Only six (21%) of the 29 participants with a positive HIV status described self-disclosure to people beyond family (2 women, 4 men). Each of these individuals indicated that they had come out openly to the public, and each was included among the 10 participants expressing highly resistant attitudes towards HIV stigma. The remaining four participants in this “highly resistant” group had disclosed to family but had not yet reached the point of public disclosure; however, at least two of them indicated their preference for a more open disclosure status, versus one characterised by some amount of hiding. Taken together, acts of self-disclosure appeared to both derive from and contribute to the highly complicated but largely desirable process of resisting stigma and being – or rather, becoming – free.
We decided to disclose to the people we may need support from, like my mother, my brother and his wife, and my mother-in-law – Nabil, 36 y/o man in seroconcordant couple
If you choose to hide, you could leave behind a family that is confused and suffering... They need to understand that this is just HIV and not murder or something of that sort – Hashim, 26 y/o man in serodiscordant couple
Everybody knows I am on ARVs, from my father-in-law to my youngest brother-in-law. They all know that I am here today for my medication. I have learned to live with it and I don’t care anymore about what other people say about me – Hadiya, 27 y/o woman in seroconcordant couple
I will tell anyone that I take drugs to prolong my life. I will tell you whether you like it or not. Don’t complain if you see me taking them because I have already told you –Zenabu, 24 y/o woman in seroconcordant couple
Let us be free so that every person is aware that we are using the drugs, and this will cause us not to fear – Mkamba, 28 y/o man in seroconcordant couple
Social and Emotional Support for Engagement in PMTCT/HIV Care
Given the above descriptions of stigma, shame, and non-disclosure as inhibitors to prevention of maternal-to-child transmission and HIV care and treatment, it is not surprising that resistance to HIV stigma and self-disclosure of HIV-positive status were reported as being facilitators for care. The idea that self-disclosure could free one from having to attend clinic visits in secret, and from hiding antiretroviral drugs, was clearly visible in the narratives. Equally crucial, however, were the social and emotional supports that the participants described receiving from the people to whom they had disclosed. As shown below, this support took various forms that coincided with type and extent of disclosure.
Support from and of spouses
Perhaps the greatest benefit of self-disclosure to spouse was the day-to-day support for HIV care that this disclosure typically afforded. While the extent of support varied, most HIV-positive partners – in both concordant and discordant relationships – described being able to rely on their spouse to help them continue in prevention of maternal-to-child transmission and HIV care and treatment. Enabling a child to be born free of HIV was a motivating factor for women to adhere to care and for men to support women in this regard. However, genuine concern for partner’s wellbeing was also evident. As stated by a woman in a serodiscordant couple that could apply to many of these relationships, “we just decided to stay together and take care of each other.” This support often involved one partner reminding the other to take their drugs or attend clinic visits. For women, it also meant that husbands provide sufficient food and “allow” rest as needed.
You can sit with your wife and talk. “My dear, this drug is helping you. Stopping it will affect your health.” At first you may fear being close to a person who has this illness, but don’t view her as the odd one out. Don’t treat her as if she is not part of your family. Be close to her. Do everything you can for her. –Musa, 38 y/o man in serodiscordant couple
We remind each other to take the drugs on time every day, without fail. –Asha, 31 y/o woman in seroconcordant couple
Sometimes he tells me to stop whatever I am doing and take the drugs. He has been helping me with this. When I am home alone, he makes sure to set the alarm for me. If I am leaving, he reminds me to carry the drugs with me. –Nelusigwe, 21 y/o woman in serodiscordant couple
It is motivating when there is someone like your wife who constantly gives you words of encouragement, especially when you need to go to the clinic. –Mashuhuri, 23 y/o man in seroconcordant couple
Support from and of family and other community members
In agreement with themes developed for disclosure to family, support for prevention of maternal-to-child transmission and HIV care and treatment within family relationships was often a matter of logistics. “Getting help when you need it” from family members was a prominent theme here, both in the context of acute illness as well for ongoing preventive care. Reducing the burden that surviving family members would have to face in the event of disability or loss was also raised as a legitimate motivation for both seeking and providing this support. But beyond the practical matters of acquiring assistance and mitigating hardship, most participants seemed to feel that this support additionally (and perhaps primarily) arose out of authentic concern for their own wellbeing.
I feel it is good if your parents know that you are on drugs. I told mine about it and they encouraged me to keep using them, as HIV is now common and I should not fear taking these drugs to prolong my life – Amira, 32 y/o woman in serodiscordant couple
If I fall sick, my family can take me to the hospital. If I forget my drugs, my co-wife can bring them to me. I think it is good to be free with your family so they can help if you need it – Kisima, 26 y/o woman in seroconcordant couple
My family would prefer that I use the medicine for life. If I stop taking the drugs, I will get sicker and they will have to bear the burden of taking care of me – Tausi, 22 y/o woman in serodiscordant couple
You have to take the drugs for the rest of your life without missing even a single day. It is therefore advisable to inform your children, any other adults in your house, and even neighbours that you are on this medication… – Zenabu, 24 y/o woman in seroconcordant couple
Support for care in wider social networks spanned from assistance from health workers and peer mentors to more general acceptance among friends and other members of the community. The former resources were available regardless of disclosure status, but community support outside of the health system usually required a greater degree of openness about HIV status. Only four women and two men reported ever attending an HIV support group (for reasons of access and availability), but those who had attended described being inspired to continue in care and talk with others about HIV. Participants who considered themselves free – especially in the sense that they were publicly open about their status – frequently expressed desires to assist or advocate for others living with the illness, including speaking out about problems with prevention of maternal-to-child transmission and HIV services or becoming involved in local efforts to improve them.
Sometimes you will find someone who rises up from the crowd and speaks openly, saying, “This isn’t bad. Even as we have this [HIV] let not anyone feel bad about that!” I am here as someone older and yet there is someone even older than me. It is stories like this that touch one’s heart and are motivating – Esta, 38 y/o woman in seroconcordant couple
As for me, I don’t care what people say, or what they want to see. But there are others who are not free. How can we help these people? – Abedi, 34 y/o man in serodiscordant couple
Personally, I am free. HIV can only kill if you ignore it, so you should tell people the truth about your health. You can help another person living in fear. Maybe there is someone who is scared, but when they see you being free with others, they might be encouraged to go to the hospital – Mkamba, 28 y/o man in seroconcordant couple
I want to advise all people living with HIV to be free, because this is the only way to stay healthy – Salumu, 46 y/o man in seroconcordant couple
Discussion
Overall, participant perspectives confirm that HIV stigma continues to exert detrimental impacts on self-disclosure and on engagement in prevention of maternal-to-child transmission and HIV care. The perception of HIV-related stigma resulting in a sort of “social death” has been reported in qualitative studies in other African settings (Egrot 2007; Koka, Ahorlu and Agyeman 2013); the presence of this sentiment in our own work underscores the enduring social impact of HIV-related stigma over time and across countries in this region. Within this climate, however, over half of the study participants demonstrated some amount of resistance to stigma, rather than simply accepting and internalising a devalued position. Parker and Aggleton (2003) argue that, as a social process that produces difference and reinforces existing inequalities, stigma is inextricably linked to wider structures of power and political economy. Drawing on literature that theorises identity as fluid and evolving (versus fixed and static), these authors point to the ability of social actors to resist HIV-related stigma and build new identities that redefine their positioning – and by doing so, seek to achieve the transformation of greater societal structures (Parker and Aggleton 2003).
Our findings reveal resistance to HIV-related stigma as a complex process that entails overcoming stigma-related fears through the adoption of particular ideas and attitudes. This process appears to correspond closely with that of self-disclosure, in that participants who expressed a higher level of resistance had also disclosed their status to people and social networks beyond their partner. More men than women expressed resistant views and reported such disclosure, but further research is needed to discern how gender influences ability to stand against prevailing social constructs and identity valuations. Because this study was not designed to explicitly examine HIV-related stigma resistance (rather, it emerged from a broader line of inquiry), we cannot make specific inferences about how resistance is fully produced, who is likely and unlikely to engage in this process, and the extent to which it can be cultivated directly. Also unclear is the primary pathway by which stigma resistance is linked to self-disclosure: whether an evolving resistance ideology leads to acts of disclosure, or whether disclosure (and ensuing social support) causes one to think and feel differently about HIV status. What this analysis does show is that resistance to HIV stigma and disclosure of HIV-positive status appear to be mutually reinforcing and exist on the same spectrum, where being “half-dead” occurs at one end and being “free” occurs at the other.
As described by the participants, self-disclosure of HIV-positive status facilitated retention in prevention of maternal-to-child transmission and HIV care through particular mechanisms of social and emotional support. Disclosure to spouse was usually the first and most important source of support, followed by family members, friends, and sometimes the voice, action, or example of a stranger. Health workers, peer mentors, and HIV educators also provided meaningful support, especially in promoting the normalisation of HIV and motivating participants to initiate and continue treatment. In the context of Option B+ for prevention of maternal-to-child transmission, support from personal networks and health care systems will likely be critical, as evidence suggests that women initiating ART under this guideline are at least as likely to be lost to follow up as those receiving services under earlier HIV guidelines (Tenthani et al. 2014).
Of course, not all people are in secure and supportive relationships that enable them to be resilient in the face of HIV-related stigma. Indeed, one limitation of this study was that it did not include the perspectives of people who had not disclosed their HIV-positive status to their partner – potentially due to insecure or abusive relationships. While most couples in the study had reached a point of acceptance and support, arriving at this point was not always easy; the stories of stress and conflict that were shared provided a realistic picture of the disclosure process and how it can be worked through to a positive end. Other factors this study did not systematically assess include time from HIV diagnosis and level of HIV knowledge, although the latter is known to be high due to recent large-scale media campaigns.(National Bureau of Statistics-Kenya and International 2015) Lastly, the analysis did not reveal distinct patterns of socioeconomic positioning and particularly age in these processes; this limitation is notable because capacity for stigma resistance and opportunity for identity transformation are not likely distributed evenly across all socioeconomic positions (Goudge et al. 2009). Future studies of resistance to HIV stigma should thus include persons of undisclosed HIV-positive status, and data on HIV-related knowledge, time from diagnosis and initial self-disclosure, health status, and a range of gender, socioeconomic positioning, and community-level factors.
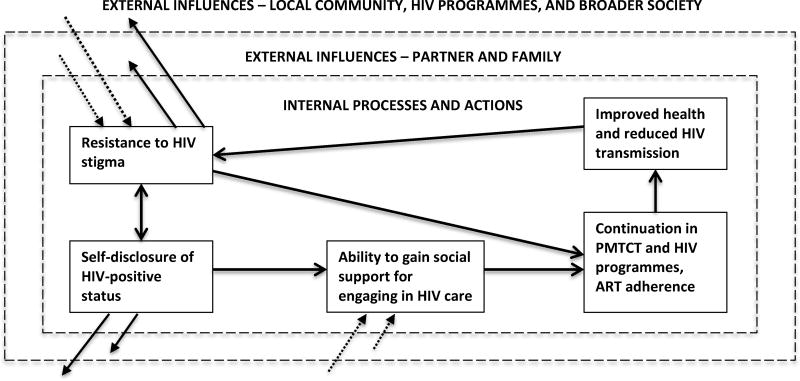
In conclusion, although much is known regarding HIV-related stigma and its negative effects, a great deal is still unknown about resistance to stigma and its links to HIV status disclosure and ultimately health outcomes – as well as implications for HIV programs. The few studies that explicitly examine HIV-related stigma resistance in sub-Saharan Africa (Abrahams and Jewkes 2012; Bond 2010; Goudge et al. 2009; Susser 2009) tend to focus on psychosocial coping or health activism, rather than adherence to ART, retention in HIV services, and actions HIV programmes might take to stimulate and uphold this resistance. To help advance understanding, we developed a conceptual model of resistance to HIV-related stigma that is roughly based on previous frameworks that conceptualise the effect of HIV stigma on participation in HIV care and on health outcomes (Turan and Nyblade 2013; Turan et al. 2017) (see Figure 1). From the current analysis, our contribution is the bi-directional relationship between HIV-related stigma resistance and self-disclosure, and the independent influences of each of these processes on engagement in prevention of maternal-to-child transmission and HIV care. Improved health outcomes then feed back into stigma resistance when the positive achievement of health outweighs the negative consequences of stigma.
Figure 1. Conceptual model of stigma resistance, self-disclosure of HIV-positive status, and engagement in care.
Note: Solid arrows represent internal effects for the person living with HIV, dotted arrows represent external influences
Increasing the availability of prevention of maternal-to-child transmission and HIV services is essential, but is not enough to prevent new infections or ensure access to care. While advanced guidelines and delivery models are scaled up, strategies must be implemented to bring HIV-related stigma down – a challenge that persists despite advances in HIV care and treatment (Stangl et al. 2013). In addition to stronger anti-discrimination policies, there is a continuing need for HIV programs to build local capacity to respond to stigma, or to “unleash the power of resistance” on the part of people living with and affected by HIV (Parker and Aggleton 2003, 21). Examples of possible programmes and interventions include: training health workers to routinely disseminate messages that normalise HIV; creating support groups that reduce feelings of shame and isolation while promoting claims to social belonging and justice; and offering facilitated disclosure services that assist in the disclosure process by increasing knowledge, assuaging fears, and improving communication (Kairania et al. 2010). Such actions may be especially critical for people who are less likely to resist HIV stigma and more likely to internalise a devalued identity or experience discrimination due to gender, socioeconomic positioning, or other marginalising qualities. Understanding local processes of HIV stigma resistance and safe self-disclosure among HIV-positive women and their partners, and then designing and implementing interventions to support these processes, may improve both engagement in prevention of maternal-to-child transmission and HIV-related care and quality of life.
References
- Abrahams N, Jewkes R. Managing and Resisting Stigma: A Qualitative Study among People Living with HIV in South Africa. Journal of the International AIDS Society. 2012;15(2):17330. doi: 10.7448/IAS.15.2.17330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bond VA. 'It is Not an Easy Decision on HIV, Especially in Zambia': Opting for Silence, Limited Disclosure and Implicit Understanding to Retain a Wider Identity. AIDS Care. 2010;22(Suppl. 1):6–13. doi: 10.1080/09540121003720994. [DOI] [PubMed] [Google Scholar]
- Castro A, Farmer P. Understanding and Addressing AIDS-Related Stigma: from Anthropological Theory to Clinical Practice in Haiti. American Journal of Public Health. 2005;95(1):53–59. doi: 10.2105/AJPH.2003.028563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charmaz K. Constructing Grounded Theory. 2. London: SAGE; 2014. [Google Scholar]
- Dedoose Version 5.0.11. web application for managing, analyzing, and presenting qualitative and mixed method research data. Los Angeles, CA: SocioCultural Research Consultants, LLC; 2014. [Google Scholar]
- Deribe K, Woldemichael K, Wondafrash M, Haile A, Amberbir A. Disclosure Experience and Associated Factors among HIV Positive Men and Women Clinical Services Users in Southwest Ethiopia. BMC Public Health. 2008;8:81. doi: 10.1186/1471-2458-8-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desgrées-du-Loû A, Brou H, Traore AT, Djohan G, Becquet R, Leroy V. From Prenatal HIV Testing of the Mother to Prevention of Sexual HIV Transmission within the Couple. Social Science & Medicine. 2009;69(6):892–899. doi: 10.1016/j.socscimed.2009.05.045. [DOI] [PubMed] [Google Scholar]
- Earnshaw VA, Chaudoir SR. From Conceptualizing to Measuring HIV Stigma: A Review of HIV Stigma Mechanism Measures. AIDS & Behavior. 2009;13(6):1160–1177. doi: 10.1007/s10461-009-9593-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egrot M. Renaître d'une Mort Sociale Annoncée: Recomposition du lien Social des Personnes Vivant avec le VIH en Afrique de l'Ouest (Burkina Faso, Sénégal) Cultures & Sociétés. 2007;1(1):49–56. [Google Scholar]
- Goudge J, Manderson L, Ngoma B, Schneider H. Stigma, Identity, and Resistance among People Living with HIV in South Africa. SAHARA-J. 2009;6(3):94–104. doi: 10.1080/17290376.2009.9724937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jasseron C, Mandelbrot L, Dollfus C, Trocme N, Tubiana R, Teglas JP, Faye A, Rouzioux C, Blance S, Warszawski J. Non-Disclosure of a Pregnant Woman's HIV Status to her Partner is Associated with Non-Optimal Prevention of Mother-to-Child Transmission. AIDS & Behavior. 2013;17(2):488–497. doi: 10.1007/s10461-011-0084-y. [DOI] [PubMed] [Google Scholar]
- Kairania RM, Gray RH, Kiwanuka N, Makumbi F, Swankambo NK, Serwadda D, Nalugoda F, Kigozi G, Semanda J, Wawer MJ. Disclosure of HIV Results among Discordant Couples in Rakai, Uganda: A Facilitated Couple Counseling Approch. AIDS Care. 2010;22(9):1041–1051. doi: 10.1080/09540121003602226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalembo FW, Zgambo M, Mulaga AN, Yukai D, Ahmed NI. Association between Male Partner Involvement and the Uptake of Prevention of Mother-to-Child Transmission of HIV (PMTCT) Interventions in Mwanza Distric, Malawi: A Retrospective Cohort Study. PLOS ONE. 2013;8(6):e66517. doi: 10.1371/journal.pone.0066517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King R, Katuntu D, Lifshay J, Packel L, Batamwita R, Nakayiwa S, Abang B, et al. Processes and Outcomes of HIV Serostatus Disclosure to Sexual Partners among People Living with HIV in Uganda. AIDS & Behavior. 2008;12(2):232–243. doi: 10.1007/s10461-007-9307-7. [DOI] [PubMed] [Google Scholar]
- Kirsten I, Sewangi J, Kunz A, Dugange F, Ziske J, Jordan-Harder B, Harms G, Theuring S. Adherence to Combination Prophylaxis for Prevention of Mother-to-Child-Transmission of HIV in Tanzania. PLOS One. 2011;6(6):e21020. doi: 10.1371/journal.pone.0021020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koka E, Ahorlu CK, Agyeman DK. Social Death through HIV and AIDS Stigmatization and Discrimination in Ghana: A Case Study of the Central Regional Hospital, Cape Coast, Ghana. Advances in Applied Sociology. 2013;3(6):231–236. [Google Scholar]
- Maman S, Mbwambo JK, Hogan NM, Weiss E, Kilonzo GP, Sweat MD. High Rates and Positive Outcomes of HIV-Serostatus Disclosure to Sexual Partners: Reasons for Cautious Optimism from a Voluntary Counseling and Testing Clinic in Dar es Salaam, Tanzania. AIDS & Behavior. 2003;7(4):373–382. doi: 10.1023/b:aibe.0000004729.89102.d4. [DOI] [PubMed] [Google Scholar]
- Mbonu NC, Van den Borne B, De Vries NK. A Model for Understanding the Relationship between Stigma and Healthcare Seeking Behaviour among People Living with HIV/AIDS in Sub-Saharan Africa. African Journal of AIDS Research. 2009;8(2):201–212. doi: 10.2989/AJAR.2009.8.2.8.860. [DOI] [PubMed] [Google Scholar]
- Medley A, Garcia-Moreno C, McGill S, Maman S. Rates, Barriers and Outcomes of HIV Serostatus Disclosure among Women in Developing Countries: Implications for Prevention of Mother-to-Child Transmission Programmes. Bulletin of the World Health Organization. 2004;82(4):299–307. [PMC free article] [PubMed] [Google Scholar]
- National AIDS and STI Control Programme, Ministry of Health, Kenya. Guidelines for Prevention of Mother to Child transmission (PMTCT) of HIV/AIDS in Kenya. Nairobi: Ministry of Health, Kenya; 2012. [Google Scholar]
- National Bureau of Statistics-Kenya, and ICF International. KDHS Key Indicators. Rockville, MD: KNBS & ICF International; 2015. [Google Scholar]
- Obermeyer CM, Baijal P, Pegurri E. Facilitating HIV Disclosure Across Diverse Settings: A Review. American Journal of Public Health. 2011;101(6):1011–1023. doi: 10.2105/AJPH.2010.300102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker R, Aggleton P. HIV and AIDS-Related Stigma and Discrimination: a Conceptual Framework and Implications for Action. Social Science & Medicine. 2003;57(1):13–24. doi: 10.1016/s0277-9536(02)00304-0. [DOI] [PubMed] [Google Scholar]
- Pride L. To Tell or Not to Tell: Negotiating Disclosure for People Living with HIV on Antitretroviral Treatment in a South African Setting. SAHARA-J. 2013;10(Suppl. 1):S17–S27. doi: 10.1080/02664763.2012.755320. [DOI] [PubMed] [Google Scholar]
- Spangler SA, Onono M, Bukusi EA, Cohen CR, Turan JM. HIV-Positive Status Disclosure and Use of Essential PMTCT and Maternal Health Services in Rural Kenya. Journal of Acquired Immune Deficiency Syndrome. 2014;67(Suppl. 4):S235–S242. doi: 10.1097/QAI.0000000000000376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stangl AL, Lloyd JK, Brady LM, Holland CE, Baral S. A Systematic Review of Interventions to Reduce HIV-Related Stigma and Discrimination from 2002–2013: How Far Have We Come? Journal of the International AIDS Society. 2013;16(Suppl. 2):18734. doi: 10.7448/IAS.16.3.18734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Susser I. AIDS, Sex, and Culture: Global Politics and Survival in Southern Africa. Malden, MA: Wiley-Blackwell; 2009. [Google Scholar]
- Tenthani L, Haas AD, Tweya H, Jahn A, van Oosterhout J, Chimbwandira F, Chirwa Z, et al. Retention in Care Under Universal Antiretroviral Therapy for HIV Infected Pregnant and Breastfeeding Women ("Option B+") in Malawi. AIDS. 2014;28(4):589–598. doi: 10.1097/QAD.0000000000000143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai AC, Bangsberg DR, Kegeles SM, Katz IT, Haberer JE, Muzoora C, Kumbakumba E, Hunt PW, Martin JN, Weiser SD. Internalized Stigma, Social distance, and Disclosure of HIV Seropositivity in Rural Uganda. Annals of Behavioral Medicine. 2013;46(3):285–294. doi: 10.1007/s12160-013-9514-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turan B, Hatcher AM, Weiser SD, Johnson MO, Rice WS, Turan JM. Framing Mechanisms Linking HIV-Related Stigma, Adherence to Treatment, and Health Outcomes. American Journal of Public Health. 2017;107(6):863–869. doi: 10.2105/AJPH.2017.303744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turan JM, Nyblade L. HIV-Related Stigma as a Barrier to Achievement of Global PMTCT and Maternal Health Goals: A Review of the Evidence. AIDS & Behavior. 2013;17(7):2528–2539. doi: 10.1007/s10461-013-0446-8. [DOI] [PubMed] [Google Scholar]
- UNAIDS. Access to Antiretroviral Therapy in Africa: Status Report on Progress toward the 2015 Targets. Geneva: UNAIDS; 2013. [Google Scholar]
- UNAIDS. Fact Sheet November 2016. Geneva: UNAIDS; 2016. [Google Scholar]