Highlights
-
•
The association of mouth-breathing and postural changes in children is unclear.
-
•
The terminology and bone landmarks used to evaluate posture are poorly described.
-
•
There is lack of reference values describing postural measurements.
-
•
The reliability and validity of the methods used are unclear.
-
•
The association of mouth-breathing and postural deviations in children is low.
Keywords: Mouth breathing syndrome, Oral breathing, Children, Posture, Photography, Kinematics
Abstract
Background
Mouth breathing syndrome can cause sleep disturbances that compromise the performance of children in school. It might also cause postural abnormalities involving the head and cervical spine; however, the association between postural abnormalities and mouth breathing in children is unclear.
Objective
To assess the methodological quality of studies and determine if there is an association between mouth breathing and postural disorders in children.
Methods
Databases comprised MEDLINE, CINAHL, PEDro, LILACS, EMBASE and Cochrane Central Registrar of Controlled Trials. Searches were until March 2016 and included studies that evaluated postural disorders in children diagnosed with mouth breathing. The Downs and Black checklist was used to evaluate the quality of the evidences.
Results
Ten studies were included totaling 417 children from 5 to 14 years. Two studies used the New York State Postural Rating Scale, seven used photography and one used motion capture to measure posture. The methods used to analyze the data included the Postural Analysis Software (SAPO), Fisiometer, ALCimagem and routines in MATLAB program. Quality assessment resulted in low scores (<14) for all the studies. The main areas of weakness were a clear description of the participants, of the methods used to access posture, of the principal confounders and lack of power analysis. External and internal validity were also threatened by the lack of a representative sample and blinding of the participants and assessors, respectively.
Conclusions
The review provides low evidence that mouth-breathing pattern in children between the ages 5–14 years is associated with postural deviations.
Introduction
The mouth-breathing syndrome (MBS) is a clinical condition among school-aged children characterized by mixed or mouth supplementary breathing that replaces an exclusively nasal breathing pattern.1 MBS is associated with disorders of the speech organs and is generally combined with facial deformities, with the potential to progress to cardiorespiratory, endocrine diseases and sleep disturbances that can compromise the behavior and performance of the children in school.2 Furthermore, this syndrome has been related to genetic factors, unhealthy oral habits and nasal obstructions of varying degrees of severity and duration and has also been associated with pediatric allergy-related otorhinolaryngology complaints.2
Studies have also correlated this condition with postural abnormalities3, 4 and suggested that the obstruction or narrowing of the pharyngeal air space would lead to forward head projection to improve the airflow trajectory to the lower respiratory tract, causing further postural adaptations.5, 6 With altered and sustained head positions, adaptations in the scalene, sternocleidomastoid and upper trapezius muscles might occur, which are normally associated with overuse in response to the nasal obstruction necessary to facilitate oral inspiration.7 Despite reports that MBS can cause postural abnormalities,6, 8, 9 the association between postural deviations and MBS is unclear. Some studies have shown that children with mouth breathing present changes in the posture of the head and cervical spine; however, other studies were unable to support such relationships.4, 10, 11
In addition, different tools have been used to evaluate posture in mouth breathing children that vary from a simple observational chart posture, to photographic analysis or to advanced motion capture systems that used passive markers attached to the segments to determine body angles and distances.3, 4, 10, 12 Different methods and marker positioning may lead to discrepancies between study findings. Moreover, forward head position has been described in most studies, however changes in postural alignment beyond the head and neck have also been considered in some studies,13, 14 which can provide insights on the effects of MBS on the whole body postural alignment. For physical therapists, providing information on the association between mouth-breathing condition and postural changes in children is important for clinical decision-making, and this information is lacking on the literature.
Thus, we carried out a systematic review to assess the methodological quality of studies that evaluated postural disorders in children with mouth breathing and determine if there is an association between mouth breathing and postural disorders. The information from this review could help the development of rehabilitation programs focused on helping these children.
Methods
Search strategy
The following electronic databases were searched: MEDLINE, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Physiotherapy Evidence Database (PEDro), LILACS database (Literatura Latino-Americana e do Caribe em Ciências da Saúde) and Excerpta Medica Database (EMBASE), including Cochrane Central Registrar of Controlled Trials. Randomized and non-randomized controlled trials were included in the review. Searches were performed by one of the authors (PN) and the strategy is described in details in Appendix 1. The search results were limited to studies in children (<18 years), reported in English or Portuguese and include all published studies until March 2016.
Study selection
Two authors (PN and PM) independently reviewed the titles and abstracts retrieved from all databases and determined if the studies met the inclusion criteria. A third author (SM) decided on any disagreement. Studies were included if reported participants with mouth breathing and at least one element of postural assessment obtained with photographs, or by a software program or even a postural observational analysis that considered either the head, neck, shoulder, scapula, spine, pelvis, knee and/or foot. Inclusion criteria for mouth breathing children were based on clinical evaluation and video laryngoscopy. Signs and symptoms included the absence of active lip seal, facial features, presence of deleterious oral habits, breathing pattern during the day and overnight, tongue tonus, associated allergies and difficulty concentrating in school. Studies were excluded if reported the use of X-rays due to its invasiveness, presence of associated syndromes, or if the assessment protocol was not described. Due to the limited literature in this area all studies designs were included.
Data extraction and quality assessment
The PRISMA15 checklist was used to document the studies and included information on study design, sample size, subject characteristics, etiology of oral breathing, type of postural assessment, measurement tools and outcomes measures and others. The methodological quality of the studies was conducted using the Downs and Black16 checklist. The Downs and Black16 consists of five sub-scales that examine the reporting to check if the paper has sufficient information for the reader to make and unbiased assessment of the findings, external validity of the findings, study bias that access biases in the measurements of the intervention and outcomes, confounding that access bias in the subject selection, and power analysis. Most of the scores ranged from 0 to 1, except for item five (confounders) at the reporting subscale that ranges from 0 to 2. The total score is 27 (Table 1). A higher score indicates better methodological quality. The following cut-off points have been suggested and adopted in this study to categorize studies by quality: excellent (26–27), good (20–25), fair (15–19) and poor (≤14).17 The Downs and Black checklist has been used previously in systematic reviews with studies of various designs17, 18, 19 and presented high internal consistency (0.89), test–retest (r: 0.88) and inter-rater (r: 0.75) reliability.16
Table 1.
Downs and Black16 quality assessment scores for all studies (n = 10).
| Studies and research designs | Reporting (max 10) | External validity (max 3) | Bias (max 7) | Confound (max 6) | Power (max 1) | Total (maximal score = 27) |
|---|---|---|---|---|---|---|
| Conti et al.11 Cross-sectional |
6 | 3 | 1 | 2 | 0 | 12 |
| Bolzan et al.4 Cross-sectional |
8 | 0 | 2 | 3 | 0 | 13 |
| Okuro et al.12 Cross-sectional |
6 | 3 | 2 | 1 | 0 | 12 |
| Silveira et al.3 Cross-sectional |
4 | 1 | 3 | 0 | 0 | 8 |
| Roggia et al.14 Cross-sectional |
4 | 0 | 2 | 1 | 0 | 7 |
| Neiva et al.10 Cross-sectional |
6 | 1 | 2 | 1 | 0 | 10 |
| Yi et al.13 Cross-sectional |
5 | 3 | 0 | 2 | 0 | 10 |
| Corrêa and Berzin7 Non-randomized clinical trial |
6 | 1 | 2 | 0 | 0 | 9 |
| Lima et al.20 Cross-sectional |
2 | 1 | 2 | 2 | 0 | 7 |
| Krakauer and Gulherme21 Cross-sectional |
3 | 2 | 1 | 0 | 0 | 6 |
Data extraction and study quality were reviewed independently by two investigators (PN and PM or SM), and disagreements were resolved by consensus. The kappa coefficient test used to verify the agreement between reviewers for the final classification of the studies was 0.90 (95% CI = 0.73–1.00) demonstrating an excellent level of agreement between reviewers.
Results
Study selection and characteristics
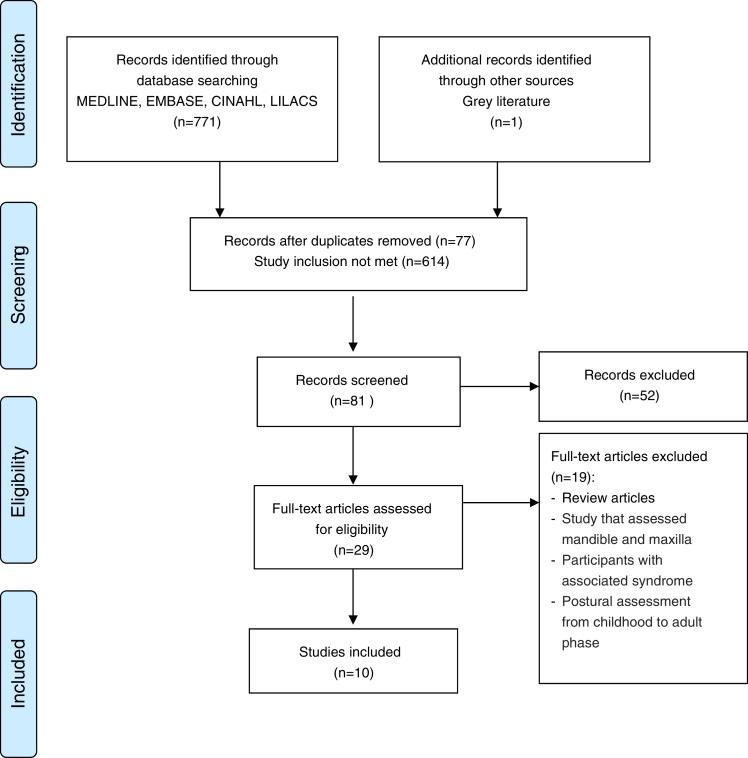
Of the 771 articles found, after deleting the duplicates, 81 remained and were retrieved electronically. Three potentially eligible studies were excluded due to the difficulty in retrieving them and failure of the authors to respond the emails. Therefore, 29 full-text articles were assessed for eligibility, and 10 met the criteria for inclusion (Fig. 1). The study designs investigated included one non-randomized clinical trial7 and nine cross sectional studies.3, 4, 10, 11, 12, 13, 14, 20, 21 A total of 622 mouth breathing children and 369 healthy control children were included.
Figure 1.
PRISMA flow chart of the study.
The participants had a mean age ranging from 5 to 14 years, 56% of the participants were males (n = 227) and 44% females (n = 190). Three studies failed to report the gender of the participants.11, 20, 21 The clinical trial included only mouth breathing children,7 seven studies included mouth breathing children and a control group of nasal breather children,3, 10, 11, 12, 13, 14, 21 and two studies further divided their sample of mouth breathing in obstructive mouth breathing and functional mouth breathing children.4, 20
Methodological quality
The Downs and Black16 checklist for all selected studies ranged from six to 13, below the cut-off point of 14; therefore, the studies presented low quality (Table 1). The lower scores were a result of poor description of the participants in five studies,3, 7, 13, 14, 20 poor postural measurement description in seven studies3, 11, 12, 13, 14, 20, 21 lack of description of the confounders, such as age, sex and types of mouth breathing condition in eight studies3, 7, 10, 12, 13, 14, 20, 21 and if the confounders were similar between the samples in five studies.4, 7, 14, 20, 21 Two questions from the reporting and four from the internal validity subscales were specific for randomized controlled trials, and the only clinical trial7 selected for this review failed to meet the criteria. In addition, sample size calculation was not reported in all studies resulting in a zero score for all studies in this subscale. Other relevant problems were absence of blinding of participants and assessors that affect the internal validity of the study, and lack of estimates in the data, such as standard errors and confidence intervals, which prevented a pooled estimate.
Postural assessment tools
Two studies used the New York State Postural Rating Scale (NYPR)11, 12 six used photogrammetry3, 4, 7, 13, 14 and one used a motion capture system (MOCAP).10 The methods used to analyze images included the Postural Analysis Software (SAPO v0.68®), Fisiometer 3.0® (Fisiometer Ltda, RJ, Brazil), ALCimagem 2-2000 and customer designed program using MATLAB (R2011a). Only one study used a Polaroid Camera21 with no specific method to interpret the data. None of the studies investigated the reliability and accuracy of the postural measures proposed. The psychometric properties described below are based on findings from other studies found in the literature.
The studies by Okuro et al.12 and Conti et al.11 used the New York State Postural Rating Scale (NYPR), which is an observational chart analysis associated with a plumb line to evaluate the alignment of 13 segments of the body.22 Each body segment can be scored as severe, moderate and normal giving a final score of altered or normal general body posture or neck posture. Reliability of the NYPR has been reported for intra- (0.86) and inter-rater (0.92) reliability of forward head posture, however, for other postural measurements the scale is questionable.22
The study by Krakauer and Guilherme21 analyzed observationally photographs taken from a Polaroid camera, without the aid of any method. Photographic images are an important technique to assess posture, but it is known that accuracy increases even further with the use of bony landmarks.23
The studies by Bolzan et al.4, Roggia et al.14 and Yi et al.13 used photographs associated with the Postural Software Analysis (SAPO),24 which is a quantitative method that provides measurements of the alignment of body segments based on photographs of bony landmarks. The method has an excellent inter-rater agreement (>0.90) for measuring forward head posture and scapular symmetries as reported by Santos et al.25 In addition, Ferreira et al.24 reported inter-rater agreement below 0.75 for forward head posture and scapular symmetries with and average error analysis for all the angular and distances measurements of 0.11° and 1.8 mm, respectively. Both studies agreed that the SAPO is a reliable method to obtain postural measurements.
Similarly, Silveira et al.3 applied photography and had the images analyzed by the software Fisiometer 3.0®26 and Corrêa et al.7 and Lima et al.20 by the software ALCimagem 2-2000.27 The information available on the Fisiometer is scarce with one report on a web site stating that the method has excellent intra- and inter-rater reliability for maker positioning at the temporomandibular joint and cervical lordosis.26 For the ALCimagem, Iunes et al.27 reported lower reliability of the method to follow postural changes.
Only the study by Neiva et al.10 applied the Qualisys Pro-Reflex (Medical AB, Gothenburg, Sweden), which is a motion capture system (MOCAP) with high-resolution cameras and passive markers to assess posture. The data was analyzed by a costume designed program in MATLAB. The accuracy and repeatability of the MOCAP system has been reported elsewhere with excellent test-retest reliability and very high accuracy to measure distances and angles.23 For more detailed information the reader should refer to recent published reviews.28, 29
Neck and head posture
Neck, head posture or forward head projection were the terms used to report head position. Using the SAPO postural program and with landmarks over the tragus of the ear, seventh cervical vertebrae (C7) and a horizontal line, Roggia et al.14 reported greater forward head position (smaller angle: 46.95°) in a group of female mouth breathing children compared to nose breathing female children (larger angle: 49.49°). Using the same instrument but with markers over the tragus, C7 and the acromion, Yi et al.13 also reported greater forward head posture in mouth breathing children (larger angle: 60.36°) associated with reduced cervical lordosis compared to nose breathing children (52.27°).
Assessing posture with the ALCimagem software and using the glabella, external acoustic meatus and the manubrium as the landmarks, Lima et al.20 reported that head projection was significantly different between groups but did not report the values. Corrêa et al.7 reported increased forward head for the mouth breathing children (9.21°) at baseline compared to after the treatment (5.99°) using the same tool, but the angle was formed between a plumb line and a line passing over the ear lobe. Silveira et al.3 reported significantly higher head projection on the mouth breathing children, of 14.3 cm, compared to 11.7 cm of nose breathing children using the Fisiometer tool by measuring the distance from a vertical line to a marker placed over the temporomandibular joint. Observationally, using the NYPR scale, Okuro et al.12 reported odds ratios of 4.27 of mouth breathing children to have forward head posture.
Shoulder and scapular position
Shoulder position was reported quantitatively in three studies using the Fisiometer,3 ALCimagem7 and the MOCAP,10 but none of the studies reported altered shoulder position in mouth breathing children. Based on observation of photographs, Krakauer et al.21 reported 60% of shoulder asymmetry in mouth breathing children and 44.4% in nose breathing children between 5 and 8 years; and in 95% and 33.3% in mouth breathing and nose breathing children, respectively, between the ages of 8.1 and 10 years.
Neiva et al.,10 using the MOCAP, investigated the position of the scapulae thoroughly with landmarks at the scapula, clavicle and spine and reported significantly right (mouth breathing 72.39 × nose breathing 81.0 mm) and left (mouth breathing 75.24 mm × nose breathing 82.64 mm) scapular elevation in mouth breathing children. Using the ALCimagem software and using the angle formed between the scapular prominence (not specified) and a vertical line, Corrêa et al.7 reported 9.74° of an abducted scapular angle in mouth breathing children, measured at baseline, and a significant decrease in this angle after physical therapy intervention (8.82°).
Spinal alignment
Silveira et al.3 reported significantly greater neck lordosis in mouth breathing children (7.3 cm) compared to nose breathing children (5.4 cm) assessed with the Fisiometer by measuring the distance from a straight line to markers placed over the neck and lumbar spine. Lima et al.20 using the same instrument, but with markers located at the greater cervical, thoracic and lumbar curvatures reported significantly lateral deviations of the cervical and thoracic spines in mouth breathing children but failed to report the values. Yi et al.13 using the SAPO postural program reported significantly greater lumbar lordosis angles in the mouth breathing group (smaller angle: 102.52°) compared to the nose breathing group (119.84°) through an angle formed between the first lumbar vertebrae, the anterior superior iliac spine and the greater trochanter.
Thoracic kyphosis was reported significantly in two studies10, 13, 20 that used the SAPO postural program. Yi et al.13 measured the angle formed between the acromion and first lumbar and seventh thoracic vertebrae, and reported increased thoracic kyphosis in mouth breathing children (45.89°) compared to nose breathing (41.33°). Lima et al.20 reported significant difference in thoracic convexity between the obstructive mouth breathing and nose breathing groups as well as between the functional mouth breathing and nose breathing groups, but failed to report the landmarks used and the values obtained (Table 2).
Table 2.
Summary of the studies included in the systematic review (n = 10).
| Studies | Sample and type of diagnosis | Instrument | Postural variables measured | Results | Conclusions |
|---|---|---|---|---|---|
| Okuro et al.,12 Cross-sectional |
8–11 years 45 Mouth breathing 16 F–29 M 62 Nose breathing 23 M–39 F Clinical diagnosis |
New York Postural Rating (NYPR) | Neck posture: anterior head position with flexion of the lower portion and extension of the upper portion of the spine Alignment of the head: anterior tilting of the head |
Mouth breathing: 36 (80%) and nose breathing: 30 (48.4%) OR = 4.27 [95% CI: 1.63–11.42], p < 0.001 of having altered head posture. Mouth breathing: 18 (40%) and nose breathing: 33 (53.2%) OR = 0.59 [95% CI: 0.25–1.37], p = 0.176 of having altered body posture |
Mouth breathing children presented cervical postural changes compared to nose breathing children |
| Conti et al.,11 Cross-sectional |
5–14 years 323 Mouth breathing 124 Nose breathing Clinical diagnosis |
New York Postural Rating (NYPR) assessed observationally of 13 body segments and scored as severe, moderate and normal | Full body alignment: posterior and lateral view neck, shoulders, spine, abdomen, hips, feet and arches Detailed description of the measurements were not provided |
Mouth breathing: 60.74% normal posture, 29.63% moderate, 9.63% severe postural abnormalities Nose breathing: 56.20% normal posture, 42.98% moderate posture, 0.83% severe postural abnormalities Posterior view: head, shoulder, feet and arches significantly different between groups (p ≤ 0.0002) Lateral view: thorax, shoulder, spine, trunk and abdomen significantly different between groups (p ≤ 0.0003). Neck posture did not differ between groups in the lateral view (p = 0.260) Odds ratio (95% CI) of the mouth breathing group for the score of full body alignment: Severe × Normal: odds ratio of 24.99 (95% CI: 3.127–194.127) Moderate × Normal: odds ratio of 2.911 (95% CI: 1.775–4.774) |
The study showed an association between mouth breathing and body posture in children and adolescents |
| Bolzan et al.,4 Cross-sectional |
8–11 years 22 Obstructive mouth breathing 10 F–10 M 15 Habitual mouth breathing 9 F–13 M 15 Nose breathing 13 F–2 M Diagnosis by video nasofibroscopy |
Photography Postural Software Analysis (SAPo v0.68®) |
Lateral view: Head posture measured through the angle formed by the tragus, seventh cervical vertebra and the horizontal line |
Head posture: Nose breathing: 46.15° ± 4.27° Obstructive mouth breathing: 45.71° ± 4.34° Habitual mouth breathing: 45.09° ± 5.42° No difference among groups (p = 0.45) |
The study showed that head posture seems to be not influenced by breathing pattern |
| Silveira et al.,3 Cross-sectional |
8–12 years 17 Mouth breathing 7 F–10 M 17 Nose breathing 9 F–11 M Clinical diagnosis |
Photography Postural Software Fisiometer® |
Sagittal view: Head projection: distance from a straight line drawn perpendicular to the ground and passing behind and near to the body to markers placed at temporomandibular joint Shoulder projection: distance from a straight line drawn perpendicular to the ground and passing behind and near to the body to markers placed at the acromioclavicular joint Neck lordosis: distance from a straight line drawn perpendicular to the ground and passing behind and near to the body to markers placed, not clearly specified, on the neck region. Lumbar lordosis: distance from a straight line perpendicular to the ground and passing behind and near to the body to markers placed, not clearly specified, on the lumbar region. |
Head projection: Greater distance between the posterior line and the marker at the temporomandibular joint in the mouth breathing group (14.3 cm) × nose breathing (11.7 cm) group, p = 0.005 Neck lordosis: Greater distance between the posterior line and the neck in the mouth breathing (7.3 cm) × nose breathing (5.4 cm) group, p = 0.016 No differences were found for the shoulder projection distance 13.5 cm × nose breathing 11.1 cm, p = 0.2 and for the lumbar lordosis distance (mouth breathing 6.3 cm × nose breathing 5.9 cm, p = 0.49 |
Mouth breathing children have head projection and neck hyperlordosis |
| Roggia et al.,14 Cross-sectional |
8–12 years 51 Mouth breathing 20 F–31 M 58 Nose breathing 34 F–24 M Clinical diagnosis |
Photography Postural Software Analysis (SAPo v0.68®) |
Full body alignment comparing the right and left sides of the head, pelvis, line of gravity, knee and ankle segments of boys and girls. Horizontal alignment of the head: angle between the tragus, C7 spinous process and the horizontal. The smaller the angle, the greater the forward head posture. Vertical alignment of the body: the angle between acromion, vertical and lateral malleolus. Positive angular measure: body leaning forward, and negative, backward. Horizontal alignment of the pelvis: the angle between the anterior superior iliac spine, posterior–superior and horizontal. Negative angular measurement: concavity close to zero: rectification, less negative closer to normal. Knee angle: angle between the greater trochanter, the knee joint line and lateral malleolus Ankle angle: angle between the knee joint line, lateral malleolus and horizontal. Measure angle >90°: tibia tilted back, if <90°: tibia bending forward |
Full Body alignment left × right views: knee angle statistically different between right and left side views of mouth breathing boys (R side: 3.70 ± 6.28 and L side: −0.41 ± 6.03, p = 0.0143); no difference found in the group of nose breathing boys and mouth breathing and nose breathing girls Comparisons between groups: Females: significantly difference in the horizontal head alignment angle, with greater forward head posture of the female mouth breathing group (46.95° ± 5.65°) × Nose breathing group (49.49° ± 6.01°), p = 0.0486; but no difference in the other measurements Males: significantly difference in ankle angle between males of the Mouth breathing × nose breathing (mouth breathing: 84.74° ± 3.12° and nose breathing: 83.1° ± 2.74°, p = 0.0034); but no difference in the other measurements |
Mouth breathing school boys presented hyperextended knee and decreased ankle angle compared to mouth breathing boys, suggesting an adaptation due to the excess of knee extension Mouth breathing school girls presented forward head posture compared to nose breathing girls |
| Neiva et al.,10 Cross-sectional |
8–12 years 21 Mouth breathing 21 Nose breathing Diagnosis by Video nasofibroscopy |
Qualisys ProReflex system MATLAB for data analysis |
Scapular elevation: obtained from vertical distance in millimeters from the marker positioned over C7 to the centroid point of the scapula. Greater scapular elevation indicated a lesser distance between markers Protrusion of the shoulders: angle obtained from the intersection of a straight line passing through the posterior angle of the acromion and C7 with a straight horizontal line intercepting the posterior acromion on the sagittal plane. An increased angle indicates that the shoulder is projected forward in relation to C7 Anterior tilt of the scapula: angle obtained from the intersection of a straight line passing through C7 and T7 markers and a straight line passing through markers on the posterior angle of the acromion and centroid of the scapula Scapular abduction: corresponds to the horizontal distance in millimeters from the centroid point of the scapula to the spinal column Forward head position: obtained from the angle formed by the intersection of a straight line passing through the marker on the tragus of the ear and C7 and a straight horizontal line intercepting C7 on the sagittal plane. This angle described the position of the head in relation to C7 Thoracic kyphosis: measured as the sum of the angles formed by the intersection of a straight line passing through T2 and the marker positioned 4.5 cm below T2 with a vertical axis and the angle formed by the intersection of a straight line passing through T12 and a marker positioned 4.5 cm above T12 with the same vertical axis Upward rotation of the scapula: angle obtained from the intersection of a straight line passing through the C7 and T7 markers and a line passing through the markers over the medial edge of the root of the scapular spine and the inferior angle of the scapula Internal rotation of the scapula: obtained from the intersection of a horizontal rod positioned in the abdominal region (frontal plane) with a straight line passing through markers located on the root of the scapula spine and the posterior angle of the acromion. |
MB children presented significantly increased superior scapular position of the right (72.39 ± 10.71 mm) and left scapula (75.24 ± 10.45 mm) compared to the right (81.0 ± 9.85 mm) and left scapular position (82.64 ± 8.40 mm) of the nose breathing group (p < 0.05) Shoulder protrusion: no difference in the right (141.54° ± 11.2°) and left (138.31° ± 13.74°) of the mouth breathing group compared to the right (139.02° ± 11.2°) and left (132.63° ± 9.87°) of the nose breathing group (p > 0.05) Anterior tilt of the scapula: no difference in the right (49.56° ± 6.42°) and left (49.27° ± 7.34°) of the mouth breathing group compared to the right (50.8° ± 7.39°) and left (48.46° ± 9.95°) of the nose breathing group (p > 0.05) Scapular abduction: no difference in the right (95.11 ± 7.46 mm) and left (96.13 ± 6.03 mm) of the mouth breathing group compared to the right (96.3 ± 6.3 mm) and left (101.09 ± 10.96 mm) of the nose breathing group (p > 0.05) Forward head position: no difference in the right (48.9° ± 4.4°) and left (48.10° ± 6.8°) of the \mouth breathing group compared to the right (47.59° ± 4.6°) and left (48.50° ± 6.30°) of the nose breathing group (p > 0.05) Thoracic kyphosis: no difference in the mouth breathing group (31.96° ± 10.97) compared to the nose breathing groups (30.82° ± 16.93°) (p > 0.05) Upward rotation of the scapula: no difference in the right (1.01° ± 6.84°) and left (−3.42° ± 6.15°) of the mouth breathing group compared to the right (2.98° ± 3.91°) and left (−2.61° ± 5.86°) of the nose breathing group (p > 0.05) Internal rotation of the scapula: no difference in the right (35.24° ± 4.2°) and left (33.81° ± 5.69°) of the mouth breathing group compared to the right (38.43° ± 6.01°) and left (35.55° ± 6.72°) of the nose breathing group (p > 0.05) |
Increased superior scapular position may be due to the forward head, clinically observed in mouth breathing children, that leads to altered position of the mandible |
| Yi et al.,13 Cross-sectional |
5–12 years 30 Mouth breathing 22 Nose breathing Diagnosis by video nasofibroscopy |
Photography Postural Software Analysis (SAPO) v0.68®) |
Cervical lordosis: angle formed by the tragus of the ear, the acromion and C7. The larger the angle, the further forward the position of the head and the lower the degree of cervical lordosis. Thoracic kyphosis: angle formed by the acromion to L1 and from L1 to T7, where L1 was the apex of the angle. The larger the angle, the greater the degree of thoracic kyphosis. Lumbar lordosis: angle drawn between three anatomic points: L1, ASIS and the greater trochanters, where ASIS was the apex of the angle. The smaller the angle, the greater the degree of lumbar lordosis. Pelvic position: angle drawn between the ASIS, the midpoint of the knee joint on the lateral face and the greater trochanters where the midpoint of the joint line was the apex of the angle. The greater the angle, the greater the pelvic tilt. |
Cervical lordosis: significantly difference between mouth breathing (60.36° ± 9.54°) × nose breathing (52.27° ± 8.58°), p = 0.003, with reduced cervical lordosis found on the mouth breathing group. Lumbar lordosis: significantly difference between mouth breathing (102.52° ± 9.67°) × nose breathing (119.84° ± 5.35°), p = 0.001, with increased lumbar lordosis found on the mouth breathing group. Thoracic kyphosis: significantly difference between mouth breathing (45.89° ± 5.26°) × nose breathing (41.33° ± 4.64°), p = 0.002, with increased thoracic kyphosis found on the mouth breathing group. Pelvic position: significantly difference between mouth breathing (9.98° ± 1.49°) × nose breathing (6.93° ± 1.00°), p = 0.001, with increased anterior tilt of the pelvis found on the mouth breathing group. |
Mouth breathing children project their heads forward to facilitate airflow. In addition, the children presented decreased cervical lordosis due to the forward projection of the head, increased lumbar lordosis, thoracic kyphosis and anterior pelvic till |
| Corrêa & Bezin7 Non-randomized clinical trial |
9–11 years 19 Mouth breathing 8 F–11 M Diagnosed by video nasofibroscopy |
Photography Postural Software ALCimagem |
Lateral view: Forward head: angle formed between the plumb line and a line passing the ear lobe Forward shoulder: angle formed between a plumb line a line passing over the acromion Flexion/extension head: angle formed between the plumb line and a line passing over the mentum Scapula abduction or winged scapula: angle formed between the plumb line and a line passing over the scapular prominence Frontal view: Head Tilt right/left: angle formed between a vertical line drawn through the manubrium and a line passing through the left/right ear lobe Shoulder elevation right/left: angle formed between a vertical line drawn through the manubrium and a line passing through the left/right coracoid process Posterior view: Scapular abduction left/right: angle formed between a line passing the superior scapular angle, C7 and superior scapular angle |
Baseline × Post treatment Forward head: 9.21° ± 4.51° × 5.99° ± 1.49°, p = 0.003 Forward shoulder: 4.18° ± 2.53° × 2.9° ± 3.13°, p = 0.121 Flexion/extension head: 17.68° ± 4.1° × 15.83° ± 3.04°, p = 0.1027 Abducted/winged scapula: 9.74° ± 2.25° × 8.82° ± 2.49°, p = 0.0458 Head tilt right: 30.19° ± 2.6° × 29.66° ± 3.5°, p = 0.379 Head tilt left: 30.96° ± 3.2° × 31.33° ± 2.6°, p = 0.454 Shoulder elevation right: 84.73° ± 3.22° × 86.37° ± 3.53°, p = 0.236 Shoulder elevation left: 85.56° ± 3.14° × 87.07° ± 4.29°, p = 0.113 Scapular abduction right: 47.09° ± 6.61° × 44.14° ± 5.98°, p = 0.0158 Scapular abduction left: 103.89° ± 12.92° × 103.42° ± 10.12°, p = 0.873 |
The exercise program was effective in reducing the forward head posture, scapular abduction, shoulder elevation and internal rotation of the scapula on the right side of mouth breathing children |
| Lima et al.20 Cross-sectional |
8–10 years 17 Obstructive mouth breathing 26 Functional mouth breathing 19 Nose breathing Clinical Diagnosis |
Photography Postural Software ALCimagem |
Lateral view: Chin retraction: angle formed between the glabella, external acoustic meatus and mentum Head forward projection: angle formed between the glabella, external acoustic meatus and manubrium sterni Lateral deviation of the cervical, thoracic and lumbar spine: markers located at greatest cervical, thoracic and lumbar curvatures Pelvis and knee alignment: markers at ASIS, gluteal line, and lateral condyles of the femur Frontal View: Horizontalization of the collarbones: coracoid process, condylar angle and a horizontal line Posterior view: Scapular position: angle between the superior and inferior angle of the scapular and T12 |
Chin retraction (p = 0.014) and head forward projection (p = 0.0036) were significantly different between the obstructive mouth breathing × nose breathing group. The obstructive mouth breathing group showed more chin and head deviations. Cervical deviations were significantly different between obstructive mouth breathing × nose breathing (p = 0.0004) and obstructive mouth breathing × functional mouth breathing (p = 0.0148) Thoracic deviations were significantly different between obstructive mouth breathing × nose breathing (p = 0.0009) and obstructive mouth breathing × functional mouth breathing (p = 0.0073). The authors classified it at altered thoracic convexity. All the other measurements were not significantly different between the three groups. The values of the angles were not reported. |
Obstructive mouth breathing and Functional mouth breathing children presented different spine postural alterations; therefore should be treated differently |
| Krakauer & Guilherme21 Cross-sectional |
5–10 years 30 Nose breathing Clinical diagnosis |
Polaroid Camera Observational analysis of the photos |
Frontal view: symmetry/asymmetry of the shoulder in relation to the ground. Lateral view: head position (anterior, posterior, or normal) in relation to the neck Dorsal view: symmetry/asymmetry of the scapulae in relation to a perpendicular axis passing through the body. |
Frontal view: asymmetry observed in 60% mouth breathing children and 44.4% nose breathing children between 5 and 8 years; and 95% and 33.3% of mouth breathing and nose breathing children, respectively, between the ages of 8.1 and 10 years Lateral view: alteration observed in 80% mouth breathing children and 33.3% nose breathing children between 5 and 8 years; and 100% and 25% of mouth breathing and nose breathing children, respectively, between the ages of 8.1 and 10 years Dorsal view: asymmetry observed in 83.3% mouth breathing children and 44.4% nose breathing children between 5 and 8 years; and 70% and 41.7% of mouth breathing and nose breathing children, respectively, between the ages of 8.1 and 10 years |
Children with nose breathing, age 8 and above present better posture than those who continue mouth breathing beyond age 8 |
M, male; F, female; ASIS, anterior superior iliac spine; T12, twelve thoracic vertebrae; C7, seventh cervical vertebrae.
Full body, knee and pelvis alignment
Severe and moderate full body alignment was observed qualitatively using the NYPR scale by Conti et al.11 in 9.63% (323/31) and 29.63% (323/96) of mouth breathing children, respectively, compared to 0.83% (124/1) and 42.98% (124/53) of severe and moderate body alignment, respectively, in nose breathing children. The authors also reported significant difference in the posterior and lateral views alignment between groups, except for the neck alignment.11
Tibial and pelvis alignment were assessed with the SAPO postural software with an angle formed by a line between the knee joint line, lateral malleolus and a horizontal. Roggia et al.14 reported an increased forward bending of the tibia (of 84.74° meaning the ankle joint was more dorsiflexed) in mouth breathing compared to nose breathing children (83.1°). Yi et al.13 found an increased anterior tilt of the pelvis in mouth breathing children (9.98°) compared to nose breathing (6.93°). The angle was formed by a line passing over the anterior superior iliac spine, midpoint of the knee joint and greater trochanter.
Discussion
This systematic review assessed the association between mouth breathing patterns in children and postural alignment. Ten studies were found that addressed our question, of those, six studies found forward head posture in mouth breathing children, six found a higher percentage of full body misalignment and two studies reported scapular deviations. However, all the studies scored less than 14 on the Downs and Black16 checklist. Therefore, there is low quality evidence suggesting that mouth breathing pattern is associated with postural misalignment in children between the ages of 5–14 years. In addition, the review also highlights the lack of standardized terminology, bone landmarks, reference values and the reliability and validity of the methods and measurement tools used to evaluate posture in mouth breathing children.
The main areas of weakness were a clear description of the participants, of the methods used to access posture and the principal confounders. External validity was threatened by the lack of representative samples in half of the studies as well as internal validity, since none of the studies attempted to blind the participants or assessors. Another important area of concern was the adjustment of confounders for the postural analysis. For example, there are many factors that influence postural assessment such as age, gender, body mass and height, postural coordination and the presence of pain.30 Furthermore, growth spurts occur around 9–12 year and may cause alterations in body shape and dimensions that could affect muscle flexibility.31, 30 As a consequence, postural misalignments would be expected in this age group. Penha et al.32 reported a high frequency of postural alterations in healthy children from 7 to 10 years of age. In addition, Ludwig et al.31 and McEvoy and Grimmer,30 showed the effect of age on standing posture. Therefore, age should be considered when evaluating posture in mouth breathing children.
Measurement errors, such as marker positioning and marker movement are also another important source of errors that should be considered. So far, there is no standard recommendation to measure posture. Photogrammetry has been the choice of measurement being more precise than observational postural assessment.33 However, it is paramount to increase measurement reliability and accuracy. Training of the evaluators for landmark palpation and marker positioning as well as knowledge of the potential device errors are essential. Standardization of the body position and the type of information provided to the participant is also helpful to improve reliability. According to Zabjek et al.34 data collection duration is another important aspect of reliability. The lack of reporting the reliability of the measurements threatens the studies internal validity and credibility of the studies.
The literature supports that forward head posture is a strategy adopted by mouth breathing children to facilitate and accelerate airflow.35 Forward head position is a combination of extension of the upper cervical spine, flexion of the lower cervical and thoracic spine leading to an increase in cervical lordosis.36 Prolonged head forward posture causes increased strain on the extensor muscles of the head and stretches the infrahyoid muscles creating an inferior and posterior traction the hyoid bone. As a consequence, the mandible is pulled in a direction of retraction and depression.36 Therefore, measurements should include bony landmarks at the lower cervical spine or upper thoracic spine and at the mandible to reflect a true forward head posture. For example, an angle formed by the ear lobe, C7 and the mandible would reflect a true head forward, since it would also include mandible retraction. Measurements with landmarks at the trunk and shoulder, as presented by Yi et al.13 and Lima et al.20 might be influenced by the position of these structures. Shoulder elevation would place the acromion slightly higher and would affect the head position angle as proposed by Yi et al.13 On the other hand, trunk rotation would also affect the marker positioning over the manubrium as proposed by Lima et al.20 In addition, measurements that rely on perpendicular lines3, 7 are subject to errors due to the lack of consistent bony landmarks and body motion. Therefore, markers placed over segments that reflect the true head forward measurement might improve the reliability and facilitate comparisons among studies.
Limitations of this review included the heterogeneity of the measurements and tools used to access posture, lack of power and internal and external validity of the studies. In addition, studies in languages other than English or Portuguese were also excluded. There is no evidence that non-English written papers are substantially better than the ones published in English.37, 38 Methodological quality can be improved in future studies by considering effect size and power analysis, controlled designs, appropriate analysis of the reliability and validity of the instruments and landmarks used to access posture, blinding of the examiners, random sampling, and eligibility criteria of the participants by controlling the types of mouth breathing patterns. Understanding the prime alterations of posture in mouth breathing children and being able to reflect on that earlier is important to increase the quality of life of these children.
Conclusion
The result of this review provides low evidence that mouth-breathing pattern in children between the ages 5–14 years is associated with postural deviations. Future studies should consider the methodological issues discussed and attempt to develop standardized methods to assess postural measurements in mouth breathing children.
Conflicts of interest
The authors declare no conflicts of interest.
Acknowledgements
The Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), a Brazilian funding agency, supported the primary author during her partial doctoral program in Canada.
Appendix 1.
The following combination of concepts and Boolean operators were used to retrieve the studies:
| 01 | “mouth breathing”[MeSH Terms] OR mouth breathing[Text Word] |
| 02 | oral breathing |
| 03 | oral respiration |
| 04 | breathing mouth |
| 05 | 1 or 2 or 3 or 4 |
| 06 | postural disorders |
| 07 | posture |
| 08 | postural |
| 09 | postural abnormalities |
| 10 | kinesis |
| 11 | positioning |
| 12 | orthostatic |
| 13 | 6 or 7 or 8 or 9 or 10 or11 |
| 14 | 05 and 13 |
| 15 | “child”[MeSH Terms] OR children[Text Word] |
| 16 | preschool children |
| 17 | adolescent |
| 18 | 15 or 16 or 17 |
| 19 | 14 and 18 |
| 20 | research design |
| 21 | comparative study |
| 22 | 20 or 21 |
| 23 | 19 and 22 |
References
- 1.Barros J.R., Becker H.M., Pinto J.A. Evaluation of atopy among mouth-breathing pediatric patients referred for treatment to a tertiary care center. J Pediatr (Rio J) 2006;82:458–464. doi: 10.2223/JPED.1561. [DOI] [PubMed] [Google Scholar]
- 2.Felcar J.M., Bueno I.R., Massan A.C., Torezan R.P., Cardoso J.R. Prevalence of mouth breathing in children from an elementary school. Cien Saude Colet. 2010;15:437–444. doi: 10.1590/S1413-81232010000200020. [DOI] [PubMed] [Google Scholar]
- 3.Silveira W.D., Mello F.C., Guimaraes F.S., Menezes S.L. Postural alterations and pulmonary function of mouth-breathing children. Braz J Otorhinolaryngol. 2010;76:683–686. doi: 10.1590/S1808-86942010000600002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bolzan G., Souza J., Boton L., Silva A., Corrêa E. Facila type and head posture of nasal and mouth-breathing children. J Soc Brasil Fonoaudiol. 2011;23:315–320. doi: 10.1590/s2179-64912011000400005. [DOI] [PubMed] [Google Scholar]
- 5.Kamper S.J., Henschke N., Hestbaek L., Dunn K.M., Williams C.M. Musculoskeletal pain in children and adolescents. Braz J Phys Ther. 2016;20:275–284. doi: 10.1590/bjpt-rbf.2014.0149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cuccia A.M., Lotti M., Caradonna D. Oral breathing and head posture. Angle Orthod. 2008;78:77–82. doi: 10.2319/011507-18.1. [DOI] [PubMed] [Google Scholar]
- 7.Correa E.C., Berzin F. Efficacy of physical therapy on cervical muscle activity and on body posture in school-age mouth breathing children. Int J Pediatr Otorhinolaryngol. 2007;71:1527–1535. doi: 10.1016/j.ijporl.2007.05.031. [DOI] [PubMed] [Google Scholar]
- 8.Chaves T.C., de Andrade e Silva T.S., Monteiro S.A., Watanabe P.C., Oliveira A.S., Grossi D.B. Craniocervical posture and hyoid bone position in children with mild and moderate asthma and mouth breathing. Int J Pediatr Otorhinolaryngol. 2010;74:1021–1027. doi: 10.1016/j.ijporl.2010.05.031. [DOI] [PubMed] [Google Scholar]
- 9.Malhotra S., Pandey R.K., Nagar A., Agarwal S.P., Gupta V.K. The effect of mouth breathing on dentofacial morphology of growing child. J Indian Soc Pedod Prev Dent. 2012;30:27–31. doi: 10.4103/0970-4388.95572. [DOI] [PubMed] [Google Scholar]
- 10.Neiva P.D., Kirkwood R.N., Godinho R. Orientation and position of head posture, scapula and thoracic spine in mouth-breathing children. Int J Pediatr Otorhinolaryngol. 2009;73:227–236. doi: 10.1016/j.ijporl.2008.10.006. [DOI] [PubMed] [Google Scholar]
- 11.Conti P.B., Sakano E., Ribeiro M.A., Schivinski C.I., Ribeiro J.D. Assessment of the body posture of mouth-breathing children and adolescents. J Pediatr (Rio J) 2011;87:357–363. doi: 10.2223/JPED.2102. [DOI] [PubMed] [Google Scholar]
- 12.Okuro R.T., Morcillo A.M., Sakano E., Schivinski C.I., Ribeiro M.A., Ribeiro J.D. Exercise capacity, respiratory mechanics and posture in mouth breathers. Braz J Otorhinolaryngol. 2011;77:656–662. doi: 10.1590/S1808-86942011000500020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yi L.C., Jardim J.R., Inoue D.P., Pignatari S.S. The relationship between excursion of the diaphragm and curvatures of the spinal column in mouth breathing children. J Pediatr (Rio J) 2008;84:171–177. doi: 10.2223/JPED.1771. [DOI] [PubMed] [Google Scholar]
- 14.Roggia B., Correa B., Pranke G.I., Facco R., Rossi A.G. Postural control of mouth breathing school aged children regarding gender. Pro Fono. 2010;22:433–438. doi: 10.1590/s0104-56872010000400012. [DOI] [PubMed] [Google Scholar]
- 15.Liberati A., Altman D.G., Tetzlaff J. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. 2009;151:W65–W94. doi: 10.7326/0003-4819-151-4-200908180-00136. [DOI] [PubMed] [Google Scholar]
- 16.Downs S.H., Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52:377–384. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Silverman S.R., Schertz L.A., Yuen H.K., Lowman J.D., Bickel C.S. Systematic review of the methodological quality and outcome measures utilized in exercise interventions for adults with spinal cord injury. Spinal Cord. 2012;50:718–727. doi: 10.1038/sc.2012.78. [DOI] [PubMed] [Google Scholar]
- 18.Crow J., Pizzari T., Buttifant D. Muscle onset can be improved by therapeutic exercise: a systematic review. Phys Ther Sport. 2011;12:199–209. doi: 10.1016/j.ptsp.2010.12.002. [DOI] [PubMed] [Google Scholar]
- 19.Huffer D., Hing W., Newton R., Clair M. Strength training for plantar fasciitis and the intrinsic foot musculature: a systematic review. Phys Ther Sport. 2016 doi: 10.1016/j.ptsp.2016.08.008. pii:S1466-853X(16)30075-X. [DOI] [PubMed] [Google Scholar]
- 20.Lima L.C., Barauna M.A., Sologurem M.J., Canto R.S., Gastaldi A.C. Postural alterations in children with mouth breathing assessed by computerized biophotogrammetry. J Appl Oral Sci. 2004;12:232–237. doi: 10.1590/s1678-77572004000300014. [DOI] [PubMed] [Google Scholar]
- 21.Krakauer L.H., Guilherme A. Relationship between mouth breathing and postural alterations of children: a descriptive analysis. Int J Orofacial Myol. 2000;26:13–23. [PubMed] [Google Scholar]
- 22.Arnold C.M., Beatty B., Harrison E.L., Olszynski W. The reliability of five clinical postural alignment measures for women with osteoporosis. Physiother Canada. 2000;52:286–294. [Google Scholar]
- 23.Liu H., Holt C., Evans S. Accuracy and repeatability of an optical motion analysis system for measuring small deformations of biological tissues. J Biomech. 2007;40:210–214. doi: 10.1016/j.jbiomech.2005.11.007. [DOI] [PubMed] [Google Scholar]
- 24.Ferreira E.A., Duarte M., Maldonado E.P., Burke T.N., Marques A.P. Postural assessment software (PAS/SAPO): validation and reliability. Clinics (Sao Paulo) 2010;65:675–681. doi: 10.1590/S1807-59322010000700005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Santos M.M., Silva M.P.C., Sanada L.S., Alves C.R.J. Photogrammetric postural analysis on healthy seven to ten-year-old children: interrater reliability. Rev Bras Fisioter. 2009;13:350–355. [Google Scholar]
- 26.Dias F., Antonio H. Baseado na dissertação de Waleska da Silveira Venturelli. 2006. Relatório de confiabilidade do Fisiometer; pp. 1–22. [Google Scholar]
- 27.Iunes D.H., Castro F.A., Salgado H.S., Moura I.C., Oliveira A.S., Bevilaqua-Grossi D. Confiabilidade intra e interexaminadores e repetibilidade da avaliação postural pelo fotogrametria. Rev Bras Fisioter. 2005;9:327–334. [Google Scholar]
- 28.Fortin C., Feldman D.E., Cheriet F., Labelle H. Clinical methods for quantifying body segment posture: a literature review. Disabil Rehabil. 2011;33:367–383. doi: 10.3109/09638288.2010.492066. [DOI] [PubMed] [Google Scholar]
- 29.Dunk N.M., Lalonde J., Callaghan J.P. Implications for the use of postural analysis as a clinical diagnostic tool: reliability of quantifying upright standing spinal postures from photographic images. J Manip Physiol Ther. 2005;28:386–392. doi: 10.1016/j.jmpt.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 30.McEvoy M.P., Grimmer K. Reliability of upright posture measurements in primary school children. BMC Musculoskelet Disord. 2005;6:35. doi: 10.1186/1471-2474-6-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ludwig O., Mazet C., Mazet D., Hammes A., Schmitt E. Age-dependency of posture parameters in children and adolescents. J Phys Ther Sci. 2016;28:1607–1610. doi: 10.1589/jpts.28.1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Penha P.J., Baldini M., Joao S.M. Spinal postural alignment variance according to sex and age in 7- and 8-year-old children. J Manip Physiol Ther. 2009;32:154–159. doi: 10.1016/j.jmpt.2008.12.009. [DOI] [PubMed] [Google Scholar]
- 33.Iunes D.H., Grossi D.B., Oliveira A.S., Castro F.A., Salgado H.S. Comparative analysis between visual and computerized photogrammetry postural assessment. Rev Bras Fisioter. 2009;13:308–315. [Google Scholar]
- 34.Zabjek K.F., Leroux M.A., Coillard C., Rivard C.H., Prince F. Evaluation of segmental postural characteristics during quiet standing in control and Idiopathic Scoliosis patients. Clin Biomech (Bristol, Avon) 2005;20:483–490. doi: 10.1016/j.clinbiomech.2005.01.003. [DOI] [PubMed] [Google Scholar]
- 35.Solow B. Growth changes in head posture related to craniofacial development. Am J Orthod Dentofac Orthop. 1986;89:132–140. doi: 10.1016/0002-9416(86)90089-8. [DOI] [PubMed] [Google Scholar]
- 36.Neumann D.A. 1st ed. 1 vol. Mosby, Inc.; St. Louis: 2002. Kinesiology of the musculoskeletal system; pp. 1–597. (Foundations for physical rehabilitation). [Google Scholar]
- 37.Mancini M.C., Cardoso J.R., Sampaio R.F., Costa L.C., Cabral C.M., Costa L.O. Tutorial for writing systematic reviews for the Brazilian Journal of Physical Therapy (BJPT) Rev Bras Fisioter. 2014;18:471–480. doi: 10.1590/bjpt-rbf.2014.0077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shiwa S.R., Moseley A.M., Maher C.G., Pena Costa L.O. Language of publication has a small influence on the quality of reports of controlled trials of physiotherapy interventions. J Clin Epidemiol. 2013;66:78–84. doi: 10.1016/j.jclinepi.2012.08.004. [DOI] [PubMed] [Google Scholar]