Highlights
-
•
The set of tests presented good reliability for the lumbopelvic region.
-
•
Reference values may contribute for clinical practice assessments.
-
•
SEM, TEM and MDC values confirm the set of tests’ usage in clinical practice.
Keywords: Hand held dynamometer, Physical endurance, Spine, Hip, Physical therapy
Abstract
Background
Assessing the lumbopelvic region is useful for detecting many musculoskeletal dysfunctions and also performance deficits. Several clinical tests are used to assess this region, however, reference values and results related to method, reliability and error measurements of these tests have not been reported.
Objectives
To establish reference values and determine reliability, standard error of measurement (SEM), typical error of measurement (TEM) and minimum detectable change (MDC) of a set of clinical tests used for assessing the lumbopelvic region in subjects divided by gender, age group and physical activity levels.
Methods
An observational study was conducted. For reference values, 152 subjects performed eight clinical tests (isometric strength of hip muscles; deep abdominal function and endurance tests) used to assess the lumbopelvic region. Reliability analyses were assessed using the Intraclass Correlation Coefficient (ICC2,1) and error measurements were calculated by using the SEM, TEM and the MDC.
Results
Reference values were established for each group and results showed significant (p < 0.05) differences concerning gender, age group and physical activity levels in clinical tests. All tests presented good reliability indices with an ICC higher than 0.80 for reliability; MDC values were greater than mean of SEM in all tests, confirming its usage for clinical practice assessments.
Conclusion
Reference values are necessary in the evaluation of subjects and these results can contribute for clinical practice, providing clinical training targets. Also, evaluation of reliability and error measurements in this set of tests allows its use in clinical practice.
Introduction
Interventions concerning exercise rehabilitation have been extensively studied and results confirm that exercise plays an important role in rehabilitation.1 Also, results of endurance and instability tests appear to be related to pain and the disability in many conditions affecting the musculoskeletal system,2 which makes measures of function a subject of great importance for clinicians and researchers. In addition, concerning low back pain patients, there is a subgroup that despite being asymptomatic for daily life activities, report pain while performing high levels of physical activity. It is necessary to study ways to assess these patients, so clinical training targets can be established. One possible cause is impairment of movement systems’ endurance, strength and power,3 not only in the low back, but also hip and core muscles. For that reason, there is a need for an assessment composed by a set of tests compiled to optimize these patients’ performance for higher levels of physical activities, and detect muscle deficits that can contribute to the symptoms.
McGill et al. stated that using healthy subjects’ endurance results for low back exercises could be useful for patient evaluation and for providing clinical training targets.4 However, conflicting results concerning test reliability have been reported5, 6 compromising clinical usage due to difficulties in identifying deficits of assessed individuals in follow-up scenarios.7, 8 Results concerning differences between subjects’ performance according to gender, age, and physical activity levels are discussed9, 10 mostly in athletes,11 but inconsistent in a non-athlete population. To the best of our knowledge, there is no evidence of reference values, reliability and error measurement values for tests compiled for lumbopelvic assessment in different groups.
Physical therapists should use reliable measures for assessing patients to assure if clinically meaningful changes have occurred during treatment period.12 For clinical practice usage, hand held dynamometry, pressure biofeedback units (PBU) and static endurance positions are gaining considerable interest, since these are more portable, easier to perform and less expensive when compared to other options available such as isokinetic testing13 and electromyography.14 Several tests have been proposed to assess the lumbopelvic region15 but to be clinically useful, must demonstrate good reliability and well-defined testing standards.16, 17, 18
It is crucial to consider a combination of strength, muscle activity and endurance tests which are reliable, easy to manage and affordable to be incorporated in everyday clinical practice. Therefore, the aim of the present study is to present reference values and also intra and interrater reliability, SEM, TEM and MDC of a set of tests for lumbopelvic assessment using measures of muscle strength, activity and endurance in asymptomatic subjects stratified by gender, age group and physical activity levels.
Methods
Subjects
One hundred eighty five subjects were recruited for this study from a local university setting and the community. For reference values, 152 subjects (79 men, 73 women) divided by gender, age group and physical activity levels were assessed. Sample size for reference values was calculated on the G*Power software (version 3.2.1), based on data from a pilot study, considering α = 5% and 95% power, resulting in a minimum of 16 individuals per group. For reliability, 33 subjects (15 men, 18 women) were recruited. Sample size was estimated by the study of Walter et al.,19 resulting in a minimum of 33 individuals.
This observational study was approved by the Ethical Committee of Ribeirão Preto Medical School, Universidade de São Paulo (USP), Ribeirão Preto, SP, Brazil (n° 6037/2015).
Inclusion criteria were: ability to give informed consent, ages between 18 and 65 years and ability to write and comprehend Portuguese. Subjects had to be asymptomatic without one year history of neurological or musculoskeletal diseases, back pain, injury, or surgery in the lumbar spine, hip, shoulder or knee. Women who were in their period were rescheduled to a more appropriate stage of the menstrual cycle20 and pregnant women were excluded from the study. All subjects gave full informed consent before the experiments.
Testing procedure
Testing procedure took approximately 90 min and required a hand held dynamometer (HHD) for maximum strength measurements (Lafayette Instrument Company, 01165, Lafayette, IN, USA); a PBU to evaluate the activity of the transversus abdominis muscle (TrA) indirectly (Stabilizer®, Chattanooga Group Inc., Hixson, TN, USA); a stopwatch for time measurements; a goniometer for test positioning; an examination table; a wedge support with an angle of 60°; belt straps made from an inelastic material were used for better positioning of the HHD and avoiding potential compensations by subjects during hip abductors, extensors and flexors test performance.
For maximum voluntary isometric contraction (MVIC) tests, which were measured bilaterally, examiners maintained verbal encouragement during measurements, asking subjects to push as hard as possible against the device. Examiners placed hands on the HHD to enhance the devices’ stabilization during the test, but no manual resistance was applied during testing. Three MVIC were performed on each test, with 20 s for rest; the shaft of the HHD was held perpendicular to the tested limb, with the display kept away from the subjects’ sight. To account for individual or group differences in body mass, all strength data were normalized using the following equation: [(kg force/kg body mass) × 100].21 During all endurance tests, subjects were reminded to maintain the position for as long as possible.
Sex, age and anthropometric characteristics (height, mass, body mass index [BMI]) were recorded. Subjects were verbally encouraged while holding the positions and not provided with any clues to their scores until the conclusion of the test.
Measurement procedures
Reference values
For reference values, the main examiner, who had three years of clinical practice and testing procedures conducted the set of tests in subjects who met the inclusion criteria. The Portuguese version of the International Physical Activity Questionnaire (IPAQ) – Short Version was applied to characterize subjects according to their physical activity levels.22 To minimize differences between test results which could be due to randomization, the set of tests were performed using a pre-established order: MVIC of hip abductors, extensors and flexors, deep abdominal function, prone and lateral bridges (right and left sides), trunk flexors and extensors.
Reliability
Two trained raters with 30 h of training in testing procedures and devices participated in the reliability testing. All three evaluations had to be performed within a week period and followed the Consensus-based Standards for the selection of health Measurement Instruments (COSMIN).18 For the interrater reliability, subjects were evaluated by both examiners with 24 h of rest period. Intrarater reliability was conducted by the main examiner with a minimum of three and a maximum of seven days apart. Test procedures were explained to all subjects before the experiments and the informed consent was signed. The set of tests were performed in random order, by drawing the tests from a black bag before the beginning of the assessment. IPAQ was also applied to characterize subjects according to physical activity levels,22 and the sample was composed by active and inactive individuals oriented not to change their physical activity routines during testing period.
Test descriptions
Muscle strength testing
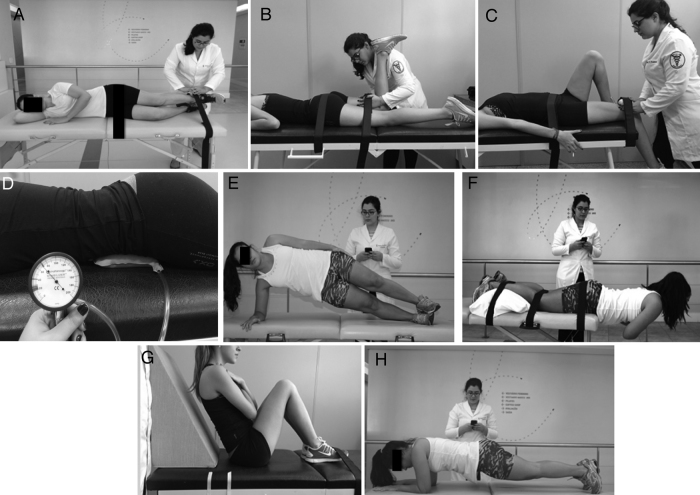
Abductors strength was evaluated with the subject side lying on the examination table. The limb to be evaluated was positioned by the examiner at approximately 20° of abduction, 10° of extension, and hip neutral rotation; HHD was positioned superior to the lateral malleolus (Fig. 1A).23 Hip extensors were assessed with the subject in prone on the table, knee flexed at 90° and hip in slight lateral rotation; HHD was positioned on the distal posterior thigh region (Fig. 1B).23 Hip flexors strength was evaluated with the subject lying supine, hands holding onto the edges of the examination table and knee of the limb to be evaluated bending over its edge; HHD was positioned superior to the distal anterior thigh region, superior to the patella; the contralateral limb was placed with the foot on the table, knee flexed (Fig. 1C).24
Figure 1.
Set of clinical tests performed for lumbopelvic functional assessment. Strength measurement for (A) hip abductors, (B) hip extensors, (C) hip flexors, (D) position for the TrA muscle activity test, (E) side bridge, (F) prone bridge, (G) trunk flexors endurance test, and (H) trunk extensors endurance test.
Deep abdominal function testing
The inflatable part of the PBU (Stabilizer®, Chattanooga Group Inc., Hixson, TN, USA) was placed centrally beneath the abdomen with the lower edge at the level of the anterior superior iliac spines, below the navel (Fig. 1D).25 The unit was inflated to a baseline of 70 mmHg to calculate changes in pressure readings and subjects were instructed how to contract their TrA using an abdominal drawing-in maneuver. Due to movement patterns and familiarization with the device participants were allowed to practice, but no more than three practice tries were allowed in an attempt to prevent premature fatigue. During practice, patients were corrected by therapists concerning the movement to be performed during the drawing in maneuver, in order to achieve the best contraction possible: maintenance of a neutral spine position was reinforced, but pressure or muscle tension in the lower ribs, rectus abdominis and/or pressure through the lower limbs were not encouraged. Readings were taken at the start and finish of a 10-second contraction, over three consecutive contractions.
Endurance testing
Side bridge test (Fig. 1E)4 consisted of subjects side lying on the examination table with legs extended. Subjects were instructed to support themselves lifting their hips off the examination table to maintain a straight line over their full body length, supporting on their forearms and their feet. Test ended when the straight line could not be maintained and hips returned to the examination table.
For the prone bridge test, subjects began lying prone in the examination table, propped on the elbows. The elbows were spaced shoulder-width apart, and the feet were set with a narrow base, but not touching. Subjects raised the pelvis from the floor so that only the forearms and the toes were in contact with the examination table. Shoulders, hips, and ankles were maintained in a straight line (Fig. 1F)26; position was held until fatigue prevented maintenance of the test position, (body straight line and limbs).
The flexor endurance test (Fig. 1G)4 required subjects to sit on the examination table and place the upper body against a wedge support with an angle of 60° from the examination table. Knees and hips were flexed, arms folded across the chest with hands placed on the opposite shoulder and toes under straps. Subjects were instructed to maintain body position while the support was pulled back 10 cm to begin the test. The test ended when the subject could not maintain the initial upper body position.
The extensor endurance test (Fig. 1H) was modified from the Biering–Sorensen test.27 Subjects laid prone with the lower body fixed to the test bed at the ankles, knees, and hips and the upper body extended over the edge of an examination table.
Subjects rested their upper bodies on the floor before the exertion. At the beginning of the exertion the upper limbs were held across the chest with the hands resting on the opposite shoulders, and the upper body was lifted off the floor until the upper torso was horizontal to the floor. Subjects were instructed to maintain the horizontal position as long as possible. Endurance time was manually recorded in seconds with a stopwatch from the point at which the subject assumed the horizontal position until the upper body came in contact with the floor.
Statistical analysis
For reference values, data distribution was verified by the Shapiro–Wilk test and homoscedasticity by the Levene test. Characterization variables of the sample were analyzed by ANOVA Three-Way. Then, for the analysis of the dependent variables on the study, logarithmic transformations were applied to the data (Log 10) to minimize deviations in the normality of distribution and homogeneity of data variance. Data were analyzed by ANCOVA Three-Way [2 (Gender: Male vs. Female) × 2 (Age Range: 18–40 years vs. 41–65 years) × 2 (Physical Activity Level: Active vs. Sedentary)] being used as covariate the BMI. When significant interactions and main effects were found univariate analyses were conducted followed by Sidak's post hoc tests where appropriate. Due to the large number of possible comparisons, the interactions were analyzed from largest (triple) to lowest complexity, and the results concerning significant interactions or main effects composed of the largest number of factors were described. The significance level was 5% (p < 0.05). All analyses were conducted in SPSS software statistic 18.0 (SPSS Inc., Chicago, USA).28
Reliability was assessed by using Intraclass Correlation Coefficient (ICC) with 95% confidence interval (CI). Intra and interrater reliability were assessed using ICC2,1 model (two way mixed model analysis of variance). ICC values of 0.75 and above represent good reliability, values between 0.40 and 0.74 represent moderate reliability and those below 0.40 indicate poor reliability.29 Standard error measurement (SEM), typical error of measurement (TEM), and minimal detectable change (MDC) at 95% of the CI were determined for each test score by the formulas: , where SD stands for the standard deviation of mean from measurements and ICC2,1 value was obtained from test–retest reliability29; ,30 where SDdiff is the standard deviation of differences test–retest; and .31
Results
Demographic characteristics of the study population for subjects assessed for reference values are provided in Table 1.
Table 1.
Demographic characteristics of the study population for reference values; mean (SD).
| Groups | n | Age (years) | Mass (kg) | Height (m) | BMI (kg/m2) |
|---|---|---|---|---|---|
| Active Male 18–40 yo | 24 | 28 (8) | 79.2 (6.8) | 1.81 (0.05) | 25.0 (2.6) |
| Active Female 18–40 yo | 20 | 25 (5) | 63.0 (7.7) | 1.66 (0.05) | 23.1 (2.0) |
| Inactive Male 18–40 yo | 20 | 30 (5) | 80.9 (10.8) | 1.79 (0.09) | 25.3 (2.8) |
| Inactive Female 18–40 yo | 19 | 27 (4) | 65.7 (12.7) | 1.66 (0.06) | 24.3 (4.7) |
| Active Male 41–65 yo | 17 | 52 (7) | 85.6 (6.5) | 1.82 (0.07) | 25.9 (1.6) |
| Active Female 41–65 yo | 17 | 51 (7) | 71.2 (8.0) | 1.66 (0.04) | 25.8 (2.7) |
| Inactive Male 41–65 yo | 18 | 51 (8) | 84.1 (9.0) | 1.82 (0.07) | 25.5 (2.4) |
| Inactive Female 41–65 yo | 17 | 53 (7) | 67.8 (7.9) | 1.66 (0.06) | 24.6 (2.1) |
yo, years old; BMI, body mass index.
Concerning reliability, 33 individuals were assessed (15 men, 18 women; age: 22.87SD4.41 years; BMI: 24.44SD3.27 kg/m2) and the results were good, with an ICC > 0.80 for intrarater and interrater reliability. The higher ICCs for intrarater and interrater reliability were found on the trunk extensors endurance and left lateral bridge, respectively. The SEM ranged from 1.24 to 2.06 kgf in MIVC tests, from 4.79 to 9.38 s in endurance tests and was 1.50 mmHg in the deep abdominal function test. The MDC indices varied from 3.44 to 5.70 kgf in MVIC tests, from 13.28 to 26.00 s in endurance tests and 4.14 mmHg in the deep abdominal function test (Table 2).
Table 2.
Reliability and error measurements of clinical tests used in the lumbopelvic assessment.
| Test | Mean (SD) | Intrarater reliability (95% CI) | Interrater reliability (95% CI) | Standard error measurement (SEM) | Minimal detectable change (MDC) | Typical error of measurement (TEM) | |
|---|---|---|---|---|---|---|---|
| Hip abductors strength (kgf) | Right | 20.64 (4.36) | 0.92 (0.84–0.96) | 0.82 (0.74–0.94) | 1.24 | 3.44 | 1.45 |
| Left | 19.15 (3.91) | 0.86 (0.71–0.93) | 0.91 (0.56–0.97) | 1.47 | 4.08 | 0.74 | |
| Hip extensors strength (kgf) | Right | 25.62 (5.95) | 0.92 (0.84–0.96) | 0.90 (0.80–0.95) | 1.66 | 4.61 | 2.75 |
| Left | 25.10 (5.66) | 0.94 (0.87–0.97) | 0.86 (0.72–0.93) | 1.41 | 3.91 | 2.50 | |
| Hip flexors strength (kgf) | Right | 36.52 (8.24) | 0.95 (0.91–0.97) | 0.83 (0.66–0.92) | 1.77 | 4.90 | 2.95 |
| Left | 35.22 (8.33) | 0.94 (0.87–0.97) | 0.93 (0.82–0.97) | 2.06 | 5.70 | 1.50 | |
| Side bridge (s) | Right | 56.62 (17.99) | 0.91 (0.81–0.95) | 0.924 (0.85–0.96) | 5.46 | 15.13 | 4.68 |
| Left | 54.87 (19.39) | 0.93 (0.86–0.97) | 0.96 (0.92–0.98) | 5.06 | 14.02 | 4.38 | |
| Prone bridge (s) | 84.17 (18.37) | 0.93 (0.85–0.98) | 0.95 (0.90–0.97) | 4.79 | 13.28 | 16.58 | |
| TrA muscle activity (mmHg) | 9.23 (3.36) | 0.80 (0.76–0.90) | 0.86 (0.71–0.93) | 1.50 | 4.14 | 2.03 | |
| Trunk flexors endurance (s) | 154.19 (44.21) | 0.95 (0.91–0.98) | 0.95 (0.89–0.97) | 9.38 | 26.00 | 31.03 | |
| Trunk extensors endurance (s) | 118.63 (37.74) | 0.96 (0.92–0.98) | 0.84 (0.60–0.93) | 7.73 | 21.44 | 34.07 |
TrA, transversus abdominis.
SD stands for “standard deviation” and CI stands for “confidence interval”
Table 3 shows the reference values of clinical tests according to gender, age group and physical activity levels.
Table 3.
Reference values and group effects for clinical tests used in the lumbopelvic assessment; mean (SD) [miminum–maximum value].
| Tests | Young adults (18–40 yo) |
Older adults (41–65 yo) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Male |
Female |
Male |
Female |
||||||
| Active (n = 24) | Inactive (n = 20) | Active (n = 20) | Inactive (n = 19) | Active (n = 17) | Inactive (n = 18) | Active (n = 17) | Inactive (n = 17) | ||
| MIVC hip abductors (kgf)a,b | Right | 23.8 (6.9)‡,* | 23.9 (5.9)‡ | 23.4 (5.4)* | 20.4 (6.7) | 21.7 (4.0)‡,* | 20.4 (4.7)‡ | 20.2 (3.9)* | 19.0 (4.9) |
| MIVC hip abductors (kgf) | Left | 22.4 (6.1) | 22.5 (4.6) | 22.1 (6.2) | 18.1 (7.4) | 21.1 (4.0) | 20.6 (4.6) | 19.9 (4.2) | 18.1 (4.3) |
| MIVC hip extensors (kgf)b | Right | 33.3 (13.2)‡ | 30.7 (6.9)‡ | 31.9 (10.0) | 26.9 (11.1) | 33.4 (5.0)‡ | 29.9 (5.7)‡ | 27.1 (6.3) | 24.3 (6.1) |
| MIVC hip extensors (kgf)d | Left | 32.8 (13.4)‡ | 32.1 (7.7)‡ | 31.1 (9.0)* | 26.2 (11.6) | 32.7 (5.0)‡ | 30.6 (6.3)‡ | 27.1 (6.2)* | 24.3 (6.9) |
| MIVC hip flexors (kgf)a,b | Right | 50.2 (16.9)‡,* | 45.2 (9.7)‡ | 45.4 (22.6)* | 34.8 (9.2) | 44.3 (7.7)‡,* | 41.3 (7.4)‡ | 32.1 (6.0)* | 30.9 (7.9) |
| MIVC hip flexors (kgf)a,b | Left | 48.8 (16.4)‡,* | 43.8 (9.1)‡ | 44.2 (21.1)* | 33.2 (11.5) | 44.2 (8.0)‡,* | 40.7 (6.8)‡ | 32.2 (6.3)* | 30.0 (7.1) |
| Side bridge (s)f | Right | 89.3 (33.7)†,* | 70.3 (16.2)† | 85.7 (21.9)† | 72.3 (6.8)† | 63.2 (8.5)* | 51.7 (9.6)‡ | 62.2 (13.6)* | 40.4 (7.0) |
| Side bridge (s)f | Left | 88.5 (35.8)†,* | 71.0 (22.1)† | 84.8 (22.3)† | 72.1 (12.4)† | 63.4 (10.4)* | 49.5 (7.4)‡ | 60.8 (12.6)* | 40.8 (6.8) |
| Prone bridge (s)b,c | 115.6 (35.9)†,* | 100.3 (24.9)† | 108.5 (22.5)†,* | 87.3 (13.1)† | 81.2 (11.7)* | 68.5 (11.6) | 77.4 (11.8)* | 68.1 (12.5) | |
| TrA muscle activity (mmHg)e | 13.3 (6.4)‡,† | 12.0 (6.5)‡,† | 6.9 (5.1) | 7.7 (4.0) | 5.5 (2.2) | 6.4 (2.4) | 6.6 (2.3) | 7.2 (1.9) | |
| Trunk flexors endurance (s)b | 284.4 (198.2)* | 219.8 (56.9) | 254.2 (56.7)* | 213.5 (111.1) | 133.1 (40.5)* | 106.2 (13.7) | 110.4 (19.5)* | 105.9 (22.7) | |
| Trunk extensors endurance (s)f | 194.9 (105.8)† | 167.3 (54.8)† | 182.1 (62.4)† | 161.6 (51.4)† | 100.3 (18.3)* | 69.5 (14.4)‡ | 93.8 (27.0) | 82.5 (19.7) | |
TrA, transversus abdominis.
SD stands for “standard deviation”, yo for “years old” and MIVC for “maximum isometric voluntary contraction”
Significant main effects and interactions:
Gender main effect.
Physical Activity Level main effect.
Age Group main effect.
Gender*Physical Activity Level interaction.
Gender*Age Group interaction.
Gender*Physical Activity Level*Age Group interaction.
Difference related to Physical Activity Level (p < 0.05).
Difference related to Age Group (p < 0.05).
Difference related to Gender (p < 0.05).
Concerning gender, male were stronger than female in both age groups and physical activity levels, presenting longer endurance times and also better TrA muscle activity. Active individuals were stronger than inactive individuals, presented longer endurance times and better deep abdominal function in both genders. Also, young adults presented higher strength, endurance and TrA muscle activity test values when compared to the same group of older adults. Our results show main effects, interactions and significant (p < 0.05) differences according to gender, age groups and physical activity levels in clinical tests.
Discussion
Results of the present study show that reference values for a set of tests compiled for lumbopelvic assessment were possible to be established in asymptomatic individuals and also its reliability and error measurements made them viable for use in clinical practice. Reference values for hip strength, TrA muscle activity and static back endurance in asymptomatic subjects have been studied in different populations21, 32, 33 and isolated results for the tests presented in this study have been advocated for use in recent literature. However, presenting stratified reference values could lead to a more accurate and specific set of data, since several studies already stated how much these variables can affect test results.34, 35, 36, 37
Concerning MIVC tests, results presented by this study are similar to current literature38, 39 which demonstrated that HHD presented good reliability (>0.80) for assessing strength in intrarater measurements and showed that younger male subjects exhibit higher strength values when compared to female or older male subjects40; however these tests were conducted in different positions, specific populations, strength values were not normalized to body weight and did not use verbal encouragement or stabilizing belt straps to stabilize and prevent the subject from overpowering the examiner. Previous reliability values regarding the lateral bridges, lumbar flexors and extensors are consistent with our results, but these studies were conducted with smaller sample sizes.4, 26, 27
The PBU has been initially developed to educate patients in retraining of muscle activity providing visual biofeedback during rehabilitation.14 Although current evidence shows that measuring TrA muscle activity with a biofeedback unit is poorly correlated to surface electromyography41 and ultrasound imaging42 and clinical questions about its measurement properties are yet to be answered,43 recent studies consider this device the most useful tool for assessing deep abdominal muscles44 in clinical practice due to its low cost and manageability. This device also presented good reliability in patients with chronic nonspecific LBP45 and, similar to our results, asymptomatic subjects as well.23, 46
Also, there are cases of individuals whose pain is triggered only by movement system fatigue. These patients are relatively asymptomatic and may have no flexibility or motor control deficits, but struggle when they have to perform intense strength and endurance tasks.3 Normative data of asymptomatic subjects in this set of tests should optimize these individuals assessment, contributing to the decision making process on rehabilitation programs and also return to higher levels of physical activities, demanded by their job or sports practice.
These tests measure different attributes with different determinants, emphasizing the importance of careful test selection. The assessment methods proposed present limitations when compared to the gold standards, such as correlation between devices and bias related to change of the position of patient, the examiner or the setting, and especially concerning the use of the PBU. Also due to the high range of the age groups in which patients were divided into, external validity of these results are restricted, since they should only be considered as reliable and possible to be used as reference values for this determined population, and in assessments which followed test procedures presented.
To our knowledge, our research group is the first to put together this set of tests and with the attempt of approximating some of the studies previously conducted4 of clinical practice, Future studies should consider developing reference values for these tests in symptomatic subjects, in order to facilitate comparisons between individuals and also detect asymptomatic subjects who are likely to develop any dysfunction of this region, such as LBP.
Conclusion
The present study is clinically important for treatment program development and return to function offering a reliable, more portable, easier to be conducted alternative for assessing strength and endurance of the lumbopelvic region in clinical practice.
Conflicts of interest
The authors declare no conflicts of interest.
References
- 1.Long A., Donelson R., Fung T. Does it matter which exercise? A randomized control trial of exercise for low back pain. Spine (Phila Pa 1976) 2004;29(23):2593–2602. doi: 10.1097/01.brs.0000146464.23007.2a. PMID: 15564907. [DOI] [PubMed] [Google Scholar]
- 2.Vanti C., Conti C., Faresin F., Ferrari S., Piccarreta R. The relationship between clinical instability and endurance tests, pain, and disability in nonspecific low back pain. J Manipulative Physiol Ther. 2016;39(5):359–368. doi: 10.1016/j.jmpt.2016.04.003. PMID: 27167368 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 3.Alrwaily M., Timko M., Schneider M. Treatment-based classification system for low back pain: revision and update. Phys Ther. 2015 doi: 10.2522/ptj.20150345. PMID: 26637653 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 4.McGill S.M., Childs A., Liebenson C. Endurance times for low back stabilization exercises: clinical targets for testing and training from a normal database. Arch Phys Med Rehabil. 1999;80(8):941–944. doi: 10.1016/s0003-9993(99)90087-4. PMID: 10453772. [DOI] [PubMed] [Google Scholar]
- 5.Judd D.L., Dennis D.A., Thomas A.C., Wolfe P., Dayton M.R., Stevens-Lapsley J.E. Muscle strength and functional recovery during the first year after THA. Clin Orthop Relat Res. 2014;472(2):654–664. doi: 10.1007/s11999-013-3136-y. PMID: 23817756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Scott D.A., Bond E.Q., Sisto S.A., Nadler S.F. The intra- and interrater reliability of hip muscle strength assessments using a handheld versus a portable dynamometer anchoring station. Arch Phys Med Rehabil. 2004;85(4):598–603. doi: 10.1016/j.apmr.2003.07.013. PMID: 15083436. [DOI] [PubMed] [Google Scholar]
- 7.Bohannon R.W. Reference values for extremity muscle strength obtained by hand-held dynamometry from adults aged 20 to 79 years. Arch Phys Med Rehabil. 1997;78:26–32. doi: 10.1016/s0003-9993(97)90005-8. [DOI] [PubMed] [Google Scholar]
- 8.Kelln B.M., McKeon P.O., Gontkof L.M., Hertel J. Hand-held dynamometry: reliability of lower extremity muscle testing in healthy, physically active, young adults. J Sport Rehabil. 2008;17:160–170. doi: 10.1123/jsr.17.2.160. [DOI] [PubMed] [Google Scholar]
- 9.Jalayondeja W., Kraingchieocharn S. Trunk extensor, flexor and lateral flexor endurance time in sedentary workers aged 20–49 years. J Med Assoc Thai. 2015;98(suppl 5):S23–S28. PMID: 26387407. [PubMed] [Google Scholar]
- 10.Roth S.M., Martel G.F., Ferrell R.E., Metter E.J., Hurley B.F., Rogers M.A. Myostatin gene expression is reduced in humans with heavy-resistance strength training: a brief communication. Exp Biol Med (Maywood) 2003;228(6):706–709. doi: 10.1177/153537020322800609. PMID: 12773702. [DOI] [PubMed] [Google Scholar]
- 11.Evans K., Refshauge K.M., Adams R. Trunk muscle endurance tests: reliability, and gender differences in athletes. J Sci Med Sport. 2007;10(6):447–455. doi: 10.1016/j.jsams.2006.09.003. PMID: 17141568 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 12.Noteboom J.T., Allison S.C., Cleland J.A., Whitman J.M. A primer on selected aspects of evidence-based practice to questions of treatment, Part 2: Interpreting results, application to clinical practice, and self-evaluation. J Orthop Sports Phys Ther. 2008;38(8):485–501. doi: 10.2519/jospt.2008.2725. PMID: 18678961 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 13.Stark T., Walker B., Phillips J.K., Fejer R., Beck R. Hand-held dynamometry correlation with the gold standard isokinetic dynamometry: a systematic review. PM R. 2011;3(5):472–479. doi: 10.1016/j.pmrj.2010.10.025. PMID: 21570036 [review] [DOI] [PubMed] [Google Scholar]
- 14.Cairns M.C., Harrison K., Wright C. Pressure biofeedback: a useful tool in the quantification of abdominal muscular dysfunction? Physiotherapy. 2000;86(3):127–138. [Google Scholar]
- 15.Villafañe J.H., Gobbo M., Peranzoni M. Validity and everyday clinical applicability of lumbar muscle fatigue assessment methods in patients with chronic non-specific low back pain: a systematic review. Disabil Rehabil. 2016;5:1–13. doi: 10.3109/09638288.2015.1107777. PMID: 26732899 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 16.Corin G., Strutton P.H., McGregor A.H. Establishment of a protocol to test fatigue of the trunk muscles. Br J Sports Med. 2005;39(10):731–735. doi: 10.1136/bjsm.2004.015537. PMID: 16183769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leggin B.G., Michener L.A., Shaffer M.A., Brenneman S.K., Iannotti J.P., Williams G.R., Jr. The Penn shoulder score: reliability and validity. J Orthop Sports Phys Ther. 2006;36(3):138–151. doi: 10.2519/jospt.2006.36.3.138. PMID: 16596890. [DOI] [PubMed] [Google Scholar]
- 18.Mokkink L.B., Prinsen C.A., Bouter L.M., Vet H.C., Terwee C.B. The COnsensus-based Standards for the selection of health Measurement INstruments (COSMIN) and how to select an outcome measurement instrument. Braz J Phys Ther. 2016;20(January (2)):105–113. doi: 10.1590/bjpt-rbf.2014.0143. PMID: 26786084, PubMed Central PMCID: PMC4900032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Walter S.D., Eliasziw M., Donner A. Sample size and optimal designs for reliability studies. Stat Med. 1998;17(1):101–110. doi: 10.1002/(sici)1097-0258(19980115)17:1<101::aid-sim727>3.0.co;2-e. PMID: 9463853. [DOI] [PubMed] [Google Scholar]
- 20.Barbosa M.B., Montebelo M.I.L., Guirro E.C.O. Determinação dos limiares de percepção sensorial e de resposta motora nas diferentes fases do ciclo menstrual. Braz J Phys Ther. 2007;11(6):443–449. [Google Scholar]
- 21.Magalhães E., Fukuda T.Y., Sacramento S.N., Forgas A., Cohen M., Abdalla R.J. A comparison of hip strength between sedentary females with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2010;40(10):641–647. doi: 10.2519/jospt.2010.3120. PMID: 20508327. [DOI] [PubMed] [Google Scholar]
- 22.Matsudo S., Araújo T., Matsudo V. Questionáro Internacional de Atividade Física (IPAQ): estudo de validade e reprodutibilidade no Brasil. Rev Bras Ativ Fís Saúde. 2001;6(2):5–12. [Google Scholar]
- 23.Piva S.R., Goodnite E.A., Childs J.D. Strength around the hip and flexibility of soft tissues in individuals with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2005;35(12):793–801. doi: 10.2519/jospt.2005.35.12.793. [DOI] [PubMed] [Google Scholar]
- 24.Meldrum D., Calahane E., Conroy R., Fitzgerald D. Maximum voluntary isometric contraction: reference values and clinical application. Amyotroph Lateral Scler. 2007;8(1):47–55. doi: 10.1080/17482960601012491. [DOI] [PubMed] [Google Scholar]
- 25.Lima P.O., Oliveira R.R., Moura Filho A.G., Raposo M.C., Costa L.O., Laurentino G.E. Concurrent validity of the pressure biofeedback unit and surface electromyography in measuring transversus abdominis muscle activity in patients with chronic nonspecific low back pain. Rev Bras Fisioter. 2012;16(5):389–395. doi: 10.1590/s1413-35552012005000038. PMID: 22832703 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 26.Schellenberg K.L., Lang J.M., Chan K.M., Burnham R.S. A clinical tool for office assessment of lumbar spine stabilization endurance: prone and supine bridge maneuvers. Am J Phys Med Rehabil. 2007;86(5):380–386. doi: 10.1097/PHM.0b013e318032156a. PMID: 17303961. [DOI] [PubMed] [Google Scholar]
- 27.Latimer J., Maher C.G., Refshauge K., Colaco I. The reliability and validity of the Biering–Sorensen test in asymptomatic subjects and subjects reporting current or previous nonspecific low back pain. Spine (Phila Pa 1976) 1999;24(20):2085–2089. doi: 10.1097/00007632-199910150-00004. discussion 2090. PMID: 10543003. [DOI] [PubMed] [Google Scholar]
- 28.Cohen J. 2nd ed. Erlbaum; Hillsdale, NJ: 1988. Statistical Power Analysis for the Behavioral Sciences. [Google Scholar]
- 29.Fleiss J.L. The Design and Analysis of Clinical Experiments. John Wiley & Sons; New York, NY: 1986. Reliability of measurement; pp. 1–32. [Google Scholar]
- 30.Hopkins W.G. Measures of reliability in sports medicine and science. Sports Med. 2000;30(July (1)):1–15. doi: 10.2165/00007256-200030010-00001. PMID: 10907753. [DOI] [PubMed] [Google Scholar]
- 31.Weir J.P. Quantifying test–retest reliability using the intraclass correlation coefficient and the SEM. J Strength Cond Res. 2005;19(1):231–240. doi: 10.1519/15184.1. PMID: 15705040 [review] [DOI] [PubMed] [Google Scholar]
- 32.Ambegaonkar J.P., Mettinger L.M., Caswell S.V., Burtt A., Cortes N. Relationships between core endurance, hip strength, and balance in collegiate female athletes. Int J Sports Phys Ther. 2014;9(5):604–616. PMID: 25328823. [PMC free article] [PubMed] [Google Scholar]
- 33.França F.R., Burke T.N., Caffaro R.R., Ramos L.A., Marques A.P. Effects of muscular stretching and segmental stabilization on functional disability and pain in patients with chronic low back pain: a randomized, controlled trial. J Manipulative Physiol Ther. 2012;35(4):279–285. doi: 10.1016/j.jmpt.2012.04.012. PMID: 22632587. [DOI] [PubMed] [Google Scholar]
- 34.Ropponen A. Studies in Sport, Physical Education and Health. University of Jyvaskyla; Jyvaskyla: 2006. The role of heredity, other constitutional structuraland behavioral factors in back function tests; p. 78. [Google Scholar]
- 35.Marras W.S., Jorgensen M.J., Granata K.P., Wiand B. Female and male trunk geometry: size and prediction of the spine loading trunk muscles derived from MRI. Clin Biomech (Bristol, Avon) 2001;16(1):38–46. doi: 10.1016/s0268-0033(00)00046-2. PMID: 11114442. [DOI] [PubMed] [Google Scholar]
- 36.Decker M.J., Torry M.R., Wyland D.J., Sterett W.I., Richard Steadman J. Gender differences in lower extremity kinematics, kinetics and energy absorption during landing. Clin Biomech (Bristol, Avon) 2003;18(7):662–669. doi: 10.1016/s0268-0033(03)00090-1. PMID: 12880714. [DOI] [PubMed] [Google Scholar]
- 37.Alaranta H., Luoto S., Heliövaara M., Hurri H. Static back endurance and the risk of low-back pain. Clin Biomech (Bristol, Avon) 1995;10(6):323–324. doi: 10.1016/0268-0033(95)00002-3. PMID: 11415574. [DOI] [PubMed] [Google Scholar]
- 38.Bohannon R.W. Test–retest reliability of hand-held dynamometry during a single session of strength assessment. Phys Ther. 1986;66(2):206–209. doi: 10.1093/ptj/66.2.206. PMID: 3945674. [DOI] [PubMed] [Google Scholar]
- 39.Keller A., Hellesnes J., Brox J.I. Reliability of the isokinetic trunk extensor test, Biering–Sørensen test, and Astrand bicycle test: assessment of intraclass correlation coefficient and critical difference in patients with chronic low back pain and healthy individuals. Spine (Phila Pa 1976) 2001;26(7):771–777. doi: 10.1097/00007632-200104010-00017. PMID: 11295899. [DOI] [PubMed] [Google Scholar]
- 40.Andrews A.W., Thomas M.W., Bohannon R.W. Normative values for isometric muscle force measurements obtained with hand-held dynamometers. Phys Ther. 1996;76(3):248–259. doi: 10.1093/ptj/76.3.248. PMID: 8602410. [DOI] [PubMed] [Google Scholar]
- 41.Lederman E. The myth of core stability. J Bodyw Mov Ther. 2010 Jan;14(1):84–98. doi: 10.1016/j.jbmt.2009.08.001. PMID: 20006294 [review; Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 42.Giggins O.M., Persson U.M., Caulfield B. Biofeedback in rehabilitation. J Neuroeng Rehabil. 2013;10:60. doi: 10.1186/1743-0003-10-60. PMID: 23777436 [review] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.de Paula Lima P.O., de Oliveira R.R., Costa L.O., Laurentino G.E. Measurement properties of the pressure biofeedback unit in the evaluation of transversus abdominis muscle activity: a systematic review. Physiotherapy. 2011;97(June (2)):100–106. doi: 10.1016/j.physio.2010.08.004. PMID: 21497243 [review; Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 44.Figueiredo M.K., Chaves-Junior I.P., Figueiredo V.G.C., Costa L.O.P., Costa LdaC. Estudo da confiabilidade intra e entre examinadores da unidade de biofeedback pressórico na medida da contracão do músculo transverso abdominal. Rev Bras Ciênc Mov. 2005;13:93–100. [Google Scholar]
- 45.Azevedo D.C., Lauria A.C., Pereira A.R. Intraexaminer and interexaminer reliability of pressure biofeedback unit for assessing lumbopelvic stability during 6 lower limb movement tests. J Manipulative Physiol Ther. 2013;36(1):33–43. doi: 10.1016/j.jmpt.2012.12.008. PMID: 23380212. [DOI] [PubMed] [Google Scholar]
- 46.Hodges P., Richardson C., Jull G. Evaluation of the relationship between laboratory and clinical tests of transversus abdominis function. Physiother Res Int. 1996;1(1):30–40. doi: 10.1002/pri.45. PMID: 9238721. [DOI] [PubMed] [Google Scholar]