Abstract
Idiopathic scrotal calcinosis is a rare disorder presenting with firm and painless nodules on the scrotal skin. The most common site is the frontal aspect of the scrotum whereas the dorsal aspect with the transition to the perineum is rarely involved. Surgery is the gold standard of treatment.
Keywords: Scrotum, Idiopathic calcinosis, Scrotal cysts, Surgery, Histopathology
Introduction
Inguinoscrotal disorders can be chronic disorders or emergencies like testicular trauma or torsions [1].
Scrotal nodules and cysts are rare findings. If they are asymptomatic, the diagnostic delay may be for several years or even decades. Table 1 provides an overview of scrotal cysts and tumours [2].
Table 1.
Scrotal cysts and tumours
| Entity | Remarks |
|---|---|
| Epidermal Cyst | Stratified lining epithelium, filled with keratin and debris |
| May occur in Gardner syndrome | |
| Can lead to secondary calcinosis | |
| Cancerization is very rare | |
| Cutaneous ciliated cyst | Rare benign lesion, very rare in males |
| Female predominance (here on the legs) | |
| Steatocystoma multiplex | Uncommon benign tumours of the pilosebaceous unit |
| Stratified squamous epithelium without granular layer | |
| Filled with sebum | |
| Mutations in KRT17 gene | |
| Eruptive vellus hair cyst | Stratified squamous epithelium with granular layer |
| Multiple vellus hair shafts inside | |
| Pilomatricoma | Rarely on scrotal skin |
| Firm nodules, mostly single tumours | |
| Islands of epithelial cells composed of ghost cells in the centre surrounded by basaloid cells | |
| Idiopathic scrotal calcinosis | No epithelial lining |
We report on a rare case of extensive idiopathic scrotal calcinosis treated surgically.
Case report
A 46-year-old male patient presented with asymptomatic nodules of the scrotal skin for diagnosis and treatment. He reported the slow development of multiple lesions within the last ten years. He was otherwise healthy and did not have any medications or allergies.
On examination, we observed more than 30 firm subcutaneous cysts of variable size attached to the scrotal skin. On palpation, they were firm but painless. Their size varied form 3 mm to 4 cm (Fig. 1). Inguinal lymph nodes were impalpable. We performed surgical excision in general anaesthesia.
Figure 1.

Multiple scrotal tumours – idiopathic scrotal calcinosis of the anterior aspect of the scrotum
The tumours were subjected to histopathological examination. On examination, pseudocystic formations with a fibrotic tissue around calcium deposits of variable size could be seen. There was no epithelial lining (Fig 2).
Figure 2.
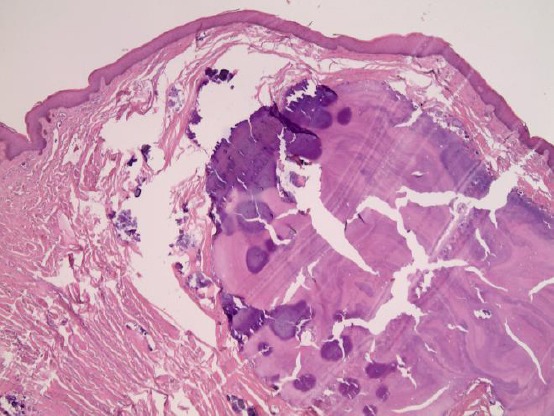
Histopathology of idiopathic scrotal calcinosis with coarse calcifications (hematoxylin-eosin x 10)
Healing was unremarkable. The patient was discharged on the second day after surgery.
Discussion
Firm nodules of the scrotal skin are rare. They can arise from pre-existing cysts like sebaceous cysts or steatocystoma multiplex or develop de novo. The latter is designated idiopathic scrotal calcinosis. The major difference to calcified cysts is the complete absence of a lining epithelium [3]. Surgery is the treatment of choice.
The senior author of this paper (UW) noted during his decades of experience in clinical dermatology that idiopathic calcinosis and scrotal cysts are mainly localised an the anterior aspect of scrotal skin. Scrotal skin is a product of cloacal membrane ectoderm forming the labioscrotal folds [4].
There are some differential diagnoses to idiopathic scrotal calcinosis (Table 1). Multiple epidermal cysts of the scrotum [5][6][7], sebaceous cysts [8], steatocystoma multiplex [9]. Larger cysts need surgery; smaller ones can be subjected to laser therapy with either carbon dioxide or diode laser [10][11][12]. A linear nick with a radiofrequency electrode works well in enucleating the cysts intact as long as they are not melded together with the surrounding tissue [12].
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.Guerra L, Leonard M. Inguinoscrotal pathology. Can Urol Assoc J. 2017;11(1-2 Suppl 1):S41–S46. doi: 10.5489/cuaj.4336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Redondo Martínez E, Rey López A, Sánchez Lobo V. Surgical pathology of the scrotum. An analysis of a series of 56 cases. Arch Esp Urol. 1999;52(1):11–6. PMid:10101882. [PubMed] [Google Scholar]
- 3.Killedar MM, Shivani AA, Shinde U. Idiopathic scrotal calcinosis. Indian J Surg. 2016;78(4):329–30. doi: 10.1007/s12262-016-1463-4. https://doi.org/10.1007/s12262-016-1463-4 PMid:27574356 PMCid:PMC4987564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yiee JH, Baskin LS. Penile embryology and anatomy. Scientific World Journal. 2010;10:1174–9. doi: 10.1100/tsw.2010.112. https://doi.org/10.1100/tsw.2010.112 PMid:20602076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Prasad KK, Manjunath RD. Multiple epidermal cysts in the scrotum. Indian J Med Res. 2014;140(2):318. PMid:25297369 PMCid:PMC4216510. [PMC free article] [PubMed] [Google Scholar]
- 6.Ząbkowski T, Wajszczuk M. Epidermoid cyst of the scrotum:a clinical case. Urol J. 2014;11(3):1706–9. PMid:25015622. [PubMed] [Google Scholar]
- 7.Solanki A, Narang S, Kathpalia R, Goel A. Scrotal calcinosis:pathogenetic link with epidermal cyst. BMJ Case Rep. 2015;2015 doi: 10.1136/bcr-2015-211163. pii:bcr2015211163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Angus W, Mistry R, Floyd MS, Jr, Machin DG. Multiple large infected scrotal sebaceous cysts masking Fournier's gangrene in a 32-year-old man. BMJ Case Rep. 2012;2012 doi: 10.1136/bcr.11.2011.5253. pii:bcr1120115253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rahman MH, Islam MS, Ansari NP. Atypical steatocystoma multiplex with calcification. SRN Dermatol. 2011;2011:381901. doi: 10.5402/2011/381901. https://doi.org/10.5402/2011/381901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bakkour W, Madan V. Carbon dioxide laser perforation and extirpation of steatocystoma multiplex. Dermatol Surg. 2014;40(6):658–62. doi: 10.1111/dsu.0000000000000013. PMid:24852470. [DOI] [PubMed] [Google Scholar]
- 11.Wollina U. Three hundred patients treated with ultrapulsed 980 nm diode laser for skin disorders. Indian J Dermatol. 2016;61(5):540–4. doi: 10.4103/0019-5154.190111. https://doi.org/10.4103/0019-5154.190111 PMid:27688445 PMCid:PMC5029241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kamra HT, Gadgil PA, Ovhal AG, Narkhede RR. Steatocystoma multiplex-a rare genetic disorder:a case report and review of the literature. J Clin Diagn Res. 2013;7(1):166–8. doi: 10.7860/JCDR/2012/4691.2698. PMid:23449619 PMCid:PMC3576779. [DOI] [PMC free article] [PubMed] [Google Scholar]


