Abstract
Interdigital spaces could be an area of affection of a various cutaneous conditions, most of them with benign origin. The spectrum of differential diagnosis of pigmented interdigital lesions with a recent occurrence is not so wide, in contrast. When considering pigmented lesions in the interdigital area, the most harmless differential diagnosis is a traumatic hematoma. But what would happen if we based our therapeutic behaviour or suspicious and unconfirmed harmless diagnosis, instead of considering the real life-threatening once with priority, if we kept in mind that acral lentiginous melanoma has rather an aggressive course and is the main cause of death in skin cancer patients? We present a case of misdiagnosed interdigital melanoma, treated as a hemangioma with curettage, with almost fatal consequences, in regard to uncontrolled tumor progression as a result of the wrong traumatic procedure in one hand, and the lack of adequate screening and follow up, leading to progress of the disease with lymph node metastasis and poor prognosis in general. We want to emphasise the importance of acral lentiginous melanoma with an unusual location in the differential diagnostic plan because, despite the early detection, early eradication with simple excision could save a life, or at least could provide a better prognosis.
Keywords: Melanoma, Hematoma, Dermatoscopy, Misdiagnosis, Sentinel lymph node
Introduction
Interdigital spaces could be an area of affection of a various cutaneous conditions, most of them with the benign origin, including tinea, eczema, pyogenic granuloma, interdigital neuroma, scabies eruption, etc. [1]. Fungal infections are the most commonly among them in elderly, within the spectrum of dermatological diseases [2].
They are usually presented with maceration and desquamation of the plantar surface of the foot, with or without nail involvement and rarely pigmented [2]. The spectrum of differential diagnosis of pigmented interdigital lesions with a recent occurrence is not so wide, in contrast. When considering pigmented lesions in the interdigital area, the most harmless differential diagnosis is a traumatic hematoma [1][3].
But what would happen if we based our therapeutic behaviour or suspicious and unconfirmed harmless diagnosis, instead of considering the real life-threatening once with priority, if we kept in mind that acral lentiginous melanoma has rather an aggressive course and is the main cause of death in skin cancer patients [3]?
Case report
A 58-year-old, otherwise healthy male patient, presented to the dermatologic clinic, because of a dark lesion on his right foot. The patient has noticed the pigmentation five months ago and went to another clinic for diagnosis and treatment. The lesion was diagnosed several times as hematoma and had been treated initially with curettage, according to patient’s history. Four months later, the lesion occurred again and rapidly increased in size. Malaise and loss of appetite were reported as additional subjective complaints. A dark brawn with black uneven coloured irregularly bordered pigmented macule was observed within the clinical examination, affecting the first interdigital space of the right foot and the surrounding skin on the plantar surface of the foot. The lesion was partially ulcerated, covered with yellow crusts and macerated surface right between the great and second toe (Fig. 1a). The conducted paraclinical examination did not reveal significant abnormalities in the total blood count and biochemistry. Ultrasound examination did not detect abdominal organ involvement but enlarged unilateral inguinal lymph nodes. Packages of enlarged lymph nodes were observed in the right inguinal fold, one measuring 19/8mm and two additional (measuring 10/10 mm) with the ultrasonographic characteristic of metastasis. The patient was referred for surgical treatment. The cutaneous lesion was removed by surgical excision under local anaesthesia, with 0.5 cm field of safety margins in all direction (Fig. 1b, Fig. 1c).
Figure 1.
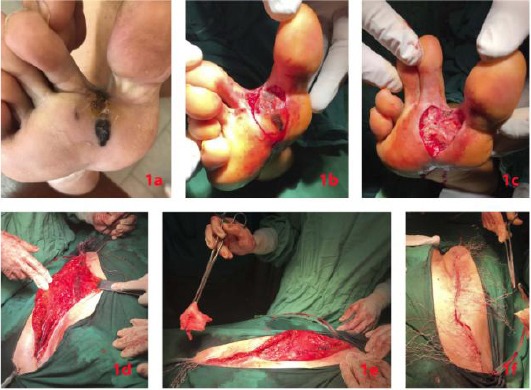
a – Clinical manifestation of interdigital acral lentiginous melanoma, four months after curettage for hematoma; b, c – Intraoperative findings. Surgical excision of the interdigital melanoma, under local anaesthesia; d, e, f – Intraoperative findings of the lymph node dissection. Dark coloured packages of enlarged lymph nodes with a firm texture, measuring 2,5 cm were established intraoperatively. Enlarged lymph nodes were observed in the obturator whole, with the same characteristic. A lymph node was found in the pelvis immediately adjacent to the v. iliaca external, infiltrated the vein wall. A partial resection of the vein was performed, as the same was reconstructed with a single stitch
Lymph node dissection was also performed under general anaesthesia, and retroperitoneal entrance toward the iliac and femoral vessels (Fig. 1d. e). Dark coloured packages of enlarged lymph nodes with a firm texture, measuring 2.5 cm were established intraoperatively. Enlarged lymph nodes were observed in the obturator whole, with the same characteristic. A lymph node was found in the pelvis immediately adjacent to the v. iliaca external, infiltrated the vein wall. A partial resection of the vein was performed, as the same was reconstructed with a single stitch on Karel. Radical lymph dissection was performed in a femoral, obturator and paraphiliac area (Fig. 1f).
Histological examination of the cutaneous lesion revealed moderately atypical cells with vesiculous nuclei, suspicious for melanoma, with tumour thickness 2 mm (Breslow).
Histological examination of the dissected lymph nodes verified total and non-total metastasis from melanoma, some with capsular infiltration, some of them without.
Postsurgical period underwent without complications, as the patient was referred for a PET -Scan in 2 months. In case of negative results for an active metastatic process, a strictly follow up would be recommended. In contrast, in case of a positive result for an active metastatic process, a BRAF testing of metastasis will be performed, considering further BRAF and MEK inhibitors as a therapeutic behaviour in case of subsequent received.
Discussion
Although melanoma is one of the most distributed tumours among the white-skinned population, tumours located on unusual sides are detected early less frequently, which decreased the favourable of the prognosis in these patients [4]. Furthermore, as a subtype of acral lentiginous melanoma, interdigital melanoma, is relatively uncommon in the Caucasian population, in contrast to Asians and Africans, and therefore, it is frequently unrecognised for a prolonged period of time, as a result from its asymptomatic nature and often atypical clinical manifestation [5]. The prognosis for patients’ survival depends on the stage of disease, but tends to be worse than with other subtypes of melanoma [6]. The often misdiagnosis and delay in diagnosis are statistically associated with a poor prognosis and relatively low survival rate, partly as a result from the advanced stage in which the tumor is usually diagnosed [4, 7]. Even histopathologically, the very early signs of acral melanoma are difficult to identify [7]. Dermoscopic criteria are also no always capable to detect early acral lentiginous melanoma, and usually caused confusion in considering further adequate therapeutic managements [8].
We present a case of misdiagnosed interdigital melanoma, treated two times as a hemangioma with curettage, with almost fatal consequences, in regard to uncontrolled tumor progression as a result from the wrong traumatic procedure in one hand, and the lack of adequate screening and follow up, leading to progress of the disease with lymph node metastasis and poor prognosis in general.
We want to emphasise the importance of acral lentiginous melanoma with an unusual location in the differential diagnostic plan, because, despite the early detection, early eradication with simple excision could save a life, or at least could provide a better prognosis.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.Matsumoto T, Chang SH, Izawa N, Ohshiro Y, Tanaka S. Interdigital Neuroma in the Second Intermetatarsal Space Associated with Metatarsophalangeal Joint Instability. Case Rep Orthop. 2016;2016:9575917. doi: 10.1155/2016/9575917. https://doi.org/10.1155/2016/9575917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Diongue K, Ndiaye M, Diallo MA, Seck MC, Badiane AS, Diop A, Ndiaye YD, Déme A, Ndiaye T, Ndir O, Ndiaye D. Fungal interdigital tinea pedis in Dakar (Senegal) J Mycol Med. 2016;26(4):312–316. doi: 10.1016/j.mycmed.2016.04.002. https://doi.org/10.1016/j.mycmed.2016.04.002 PMid:27184614. [DOI] [PubMed] [Google Scholar]
- 3.Myasnyankin MY, Gafton GI, Anisimov VV, Matsko DE, Imyanitov EN, Semiletova YV. Acral lentiginous melanoma:the current state of the problem. Vopr Onkol. 2015;61(4):563–70. PMid:26571823. [PubMed] [Google Scholar]
- 4.Matusiak L, Bieniek A, Wozniak Z, Szepietowski JC. Amelanotic malignant melanoma in an acral location. Acta Dermatovenerol Alp Pannonica Adriat. 2008;17(2):72–4. [PubMed] [Google Scholar]
- 5.Tchernev G, Lozev I, Pidakev I, Mangarov H, Grigorov Y, Cardoso JC, Popchristova E, Patterson JW, Lotti T, Pehlivanov G, Voicu C, Clatici VG, Wollina U. Interdigital melanoma simultaneously affecting two neighboring interdigital spaces :First description in the medical literature. Wien Med Wochenschr. 2017 doi: 10.1007/s10354-017-0558-2. https://doi.org/10.1007/s10354-017-0558-2. [DOI] [PubMed] [Google Scholar]
- 6.Goydos JS, Shoen SL. Acral Lentiginous Melanoma. Cancer Treat Res. 2016;167:321–9. doi: 10.1007/978-3-319-22539-5_14. https://doi.org/10.1007/978-3-319-22539-5_14 PMid:26601870. [DOI] [PubMed] [Google Scholar]
- 7.Fernandez-Flores A, Cassarino DS. Histopathological diagnosis of acral lentiginous melanoma in early stages. Ann Diagn Pathol. 2017;26:64–69. doi: 10.1016/j.anndiagpath.2016.08.005. https://doi.org/10.1016/j.anndiagpath.2016.08.005 PMid:27601330. [DOI] [PubMed] [Google Scholar]


