Abstract
BACKGROUND:
Porokeratosis is characterised by one or more atrophic patches surrounded by a distinctive peripheral keratotic ridge, typically found on sun-exposed areas, with several clinical variants and typical histological findings. Despite ultraviolet radiation, varies antibody - related autoimmune disease treated with systemic steroids and other immunosuppressive conditions such as chronic liver disease, HIV and organ transplantations have been implicated in its etiopathology.
CASE REPORT:
We present a case of porokeratosis, associated with idiopathic thrombocytopenia in 74 - year old, otherwise healthy male patient, as we discuss the previously reported associated disorders.
CONCLUSION:
Regarding all of the polymorphism of clinical presentation, associated disorders and treatment responses, we could conclude that disseminated porokeratosis is still an unknown well disorder, which will continue to surprise the physicians in future. The screening and follow up of the patients is mandatory in all cases because as we see, porokeratosis has multiple unexpected faces, which require circumstantial clinical and paraclinical behaviour.
Keywords: Porokeratosis, Acitretin, Betamethasone, Outcome, Therapy, Cryosurgery
Introduction
Porokeratosis represents a clonal disorder of keratinisation, first described in 1983 as a chronic parakeratotic skin disorder [1]. The condition is characterised by one or more atrophic patches, typically found on sun-exposed areas, surrounded by a distinctive peripheral keratotic ridge, called the cornoid lamella [1][2]. Several clinical variants have been described, as the most common among them include classic porokeratosis of Mibelli (PM), disseminated superficial actinic porokeratosis (DSAP) and its nonactinic variant disseminated superficial porokeratosis (DSP), linear porokeratosis, porokeratosis palmaris et plantaris disseminata (PPPD), punctate porokeratosis, which might represent a variant of PPPD [1][2][3].
Much less commonly reported clinical subtypes include porokeratosis ptychotropica (a verrucous variant localised in the gluteal region) [3], porokeratoma, also referred to as porokeratotic acanthoma [4], porokeratotic adnexal ostial nevus (PAON) - a rare congenital disorder of keratinization with eccrine and hair follicle involvement [5]. Although aetiology is not well - established, exposure to ultraviolet radiation, organ transplantation, chemotherapy, repetitive trauma, liver failure, chronic renal failure, hepatitis C, HIV, and other diseases associated with immunosuppression are considered risk factors which activate abnormal clones of keratinocytes [3]. Gene mutations in mevalonate pathway enzymes have also been implicated in etiopathology, such as mevalonate kinase (MVK), phosphomevalonate kinase (PMVK), mevalonate decarboxylase (MVD), and farnesyl diphosphate synthase (FDPS), as c.746 T > C and c.875A > G of the MVD gene are most common mutations [1][6]. Beside the immunosuppression variety of disorders associated with the condition, disseminated superficial porokeratosis has been reported in systemic lupus erythematosus (SLE) patient with long-term corticosteroid treatment [7], patients with diabetes mellitus [8] and associated with haematological disorders such as Hodgkin’s disease and B-cell lymphoma [9].
Here we present a patient with disseminated porokeratosis, associated with idiopathic thrombocytopenia. To the best of our knowledge, this is the first report of disseminated superficial porokeratosis, associated with idiopathic thrombocytopenia.
Case report
A 74 – year - old male patient presented with 2 - months history of erythematous rash on the lower legs, accompanied by itching. The clinical examination revealed multiple individual erythematous, slightly atrophic macules and papules, with brownish discolouration, surrounded by peripheral keratotic ridge, resembling cornoid lamella, disseminated on the chest, back and lower extremities (Fig. 1 a, b, c, d).
Figure 1.

a, b – Clinical presentation of disseminated porokeratosis on chest and back in 74-year-old male patient; c, d – Clinical presentation of disseminated porokeratosis on lower legs, with closer view of cornoid lamella
Multiple excoriations and linear defects, from scratching, were also established. The conducted paraclinical blood examinations revealed decreased plated cells count (107.0 10^9/l) and increased cholesterol (8.4 mmol/l: HDL - 2.43, LDL - 5.33 mmol/l). The performed imaging diagnostic screening did not reveal organ pathologies. The histopathological examination after performed biopsies obtained focal absence of the granular layer, dyskeratotic cells observed in the subjacent upper spinous layer.
A mild lymphocytic infiltrate were seen around an increased number of capillaries in the underlying dermis.
Dermis showed a non-specific inflammatory cell infiltrate. Epithelium deep to the tier was vacuolated and devoid of a granular cell layer (Fig. 2 a, b). Dyskeratotic cells were observed in the subjacent upper spinous layer (Fig. 2 c). Keratin-filled epidermal invagination with an angulated, parakeratotic tier (cornoid lamella) (Fig. 2 d).
Figure 2.
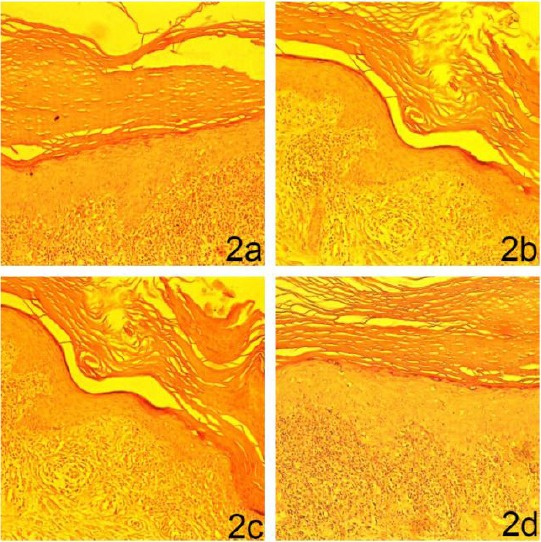
Histological findings; a, b - Focal absence of the granular layer, dyskeratotic cells observed in the subjacent upper spinous layer. A mild lymphocytic infiltrate were seen around an increased number of capillaries in the underlying dermis. Dermis showed a non-specific inflammatory cell infiltrate. Epithelium deep to the tier was vacuolated and devoid of a granular cell layer; c - Dyskeratotic cells were observed in the subjacent upper spinous layer; d - Keratin-filled epidermal invagination with an angulated, parakeratotic tier (cornoid lamella)
The diagnosis of disseminated superficial porokeratosis, associated with idiopathic thrombocytopenia was made, based on the clinical examination, laboratory and histological findings. A systemic administration of acitretin 10 mg was initiated with local application of vitamin D3 analogue (calcipotriol) and corticosteroid (betamethasone), combined in one commercial product as a gel, without a satisfactory therapeutic response within the following two weeks. Cryotherapy was initiated in combination with systemic acitretin and calcipotriol, combined with a corticosteroid. Regarding the thrombocytopenia, the dose of acitretin was not increased. The satisfactory therapeutic response was achieved in one month.
Discussion
Porokeratosis is considered as an autosomal dominant inherited disorder with the variable clinical presentation, but unified histological characteristics of cornoid lamella [1][2]. The approximate age of onset is 45 - 50 years, although the reported cases range between 27 - 84 years [1][2]. Although it is believed that the sun-exposed areas are mainly affected, the most common regions of occurrence are extremities, the buttocks, and genitogluteal region, while facial lesions are rare [2][4]. It is believed that ultraviolet radiation is the triggering factors in genetically predisposed individuals [2]. On the other hand, various antibody-related autoimmune diseases treated with systemic steroids and other immunosuppressive conditions such as chronic liver disease, HIV and organ transplantations have also been implicated in its etiopathology [11]. Despite that, our literature review established cases of association between disseminated porokeratosis and pyoderma gangrenosum [10], a case of dermatomyositis [12], scleroderma [13], Sjogren syndrome [14] and rheumatoid arthritis [15]. Authors suggest that immunosuppressant therapy is the reason for the occurrence of the porokeratosis [10][11]. Although disseminated superficial porokeratosis has rarely been reported in association with internal malignancy, its occurrence in patients with hepatitis C virus-related hepatocellular carcinoma, cholangiocarcinoma, and ovarian cancer suggests a paraneoplastic nature of the cutaneous disease [16]. Furthermore, porokeratotic lesions can give raise of bowenoid lesions and squamous cell carcinoma as precancerosis trigger with aggressive behaviour and poor prognosis [17]. A porokeratotic lesion, showing histological changes during his disease, including cellular atypia, dysplasia, and invasive squamous cell carcinoma is known as “malignant superficial porokeratosis” [18]. Sporadic case reports in the literature represents porokeratosis in patient with polycythemia rubra vera [19], pseudoxanthoma elasticum [20], multiple myeloma [21] and myelodysplastic syndrome [22][23]. Although rare, benzylhydrochlorothiazide - induced porokeratotic lesions in stable porokeratosis of Mibelli accompanied by eosinophilic spongiosis have also been reported [24].
Although hematologic disorders are not uncommonly accompanied by disseminated porokeratosis, we couldn’t find a case of porokeratosis associated with idiopathic thrombocytopenia (as in the presented case) within our thorough literature revue, encompassing the available reported cases between 1984 and present date. Although various treatment options have been implicated with various degrees of success, including topical diclofenac, vitamin D 3 analogs, 5-fluorouracil, retinoids, 5% imiquimod, photodynamic therapy, carbon dioxide laser and oral retinoids, therapy with good response is rather poor [1][2]. Reports of disseminated superficial actinic porokeratosis treated with vitamin D 3 analogs are rare in general; with no satisfactory enough effect obtained with calcipotriol monotherapy [25][26]. Simultaneous application of vitamin D3 analog (calcipotriol) and corticosteroid (betamethasone), combined in a one commercial product as a gel is reported as a promising, more effective new entity, because of the simultaneous synergetic effects of the substations, which normalize the proliferation of the keratinocytes by calcipotriol on one hand, and the reducing of the inflammation by the corticosteroid, on another [27].
Considering the polymorphism of clinical presentation, the variety of associated disorders and the differences in the treatment responses, we could conclude that disseminated porokeratosis is still an unknown well disorder, which will continue to surprise the physicians in future. The screening and follow up of the patients is mandatory in all cases because as we see, porokeratosis has multiple unexpected faces, which require circumstantial clinical and paraclinical behaviour.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.Sun RF, Chen H, Zhu W, Lian S. Dermoscopic Features and Gene Mutation in the Mevalonate Pathway of Five Sporadic Patients with Porokeratosis. Chin Med J. 2017;130:1747–8. doi: 10.4103/0366-6999.209905. https://doi.org/10.4103/0366-6999.209905 PMid:28685731 PMCid:PMC5520568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anderson I1, Routt ET2, Jim On SC. Disseminated superficial actinic porokeratosis treated with ingenol mebutate gel 0.05. Cutis. 2017;99(3):E36–E39. PMid:28398427. [PubMed] [Google Scholar]
- 3.Tebet AC, Oliveira TG, Oliveira AR, Moriya FS, Oliveira J Filho, Cucé LC. Porokeratosis ptychotropica. An Bras Dermatol. 2016;91(5 suppl 1):134–136. doi: 10.1590/abd1806-4841.20164399. https://doi.org/10.1590/abd1806-4841.20164399 PMid:28300921 PMCid:PMC5325020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Walsh SN, Hurt MA, Santa Cruz DJ. Porokeratoma. Am J Surg Pathol. 2007;31(12):1897–901. doi: 10.1097/PAS.0b013e31806910c7. https://doi.org/10.1097/PAS.0b013e31806910c7 PMid:18043046. [DOI] [PubMed] [Google Scholar]
- 5.Llamas-Velasco M, Hilty N, Kempf W. Porokeratotic adnexal ostial naevus:review on the entity and therapeutic approach. J Eur Acad Dermatol Venereol. 2015;29(10):2032–7. doi: 10.1111/jdv.12732. https://doi.org/10.1111/jdv.12732 PMid:25255914. [DOI] [PubMed] [Google Scholar]
- 6.Li X, Zhou Q, Zhu L, Zhao Z, Wang P, Zhang L, Zhang G, Wang X. Analysis of clinical and genetic features of nine patients with disseminated superfacial actinic porokeratosis. Zhonghua Yi Xue Yi Chuan Xue Za Zhi. 2017;34(4):481–485. doi: 10.3760/cma.j.issn.1003-9406.2017.04.003. PMid:28777842. [DOI] [PubMed] [Google Scholar]
- 7.Robak E, Wozniacka A, Sysa-Jedrezejowska A, Biernat W, Robak T. Disseminated superficial actinic porokeratosis in a patient with systemic lupus erythematosus. Br J Dermatol. 1999;141:759–761. doi: 10.1046/j.1365-2133.1999.03134.x. https://doi.org/10.1046/j.1365-2133.1999.03134.x PMid:10583141. [DOI] [PubMed] [Google Scholar]
- 8.Nakamura M, Fukamachi S, Tokura Y. Acute onset disseminated superficial porokeratosis associated with exacerbation of diabetes mellitus due to development of anti-insulin antibodies. Dermatoendocrinol. 2010;2(1):17–8. doi: 10.4161/derm.2.1.11816. https://doi.org/10.4161/derm.2.1.11816 PMid:21547143 PMCid:PMC3084960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Diluvio L, Campione E, Paterno EJ, et al. Acute onset disseminated superficial porokeratosis heralding diffuse large B-cell lymphoma. Eur J Dermatol. 2008;18:349–350. doi: 10.1684/ejd.2008.0409. PMid:18474476. [DOI] [PubMed] [Google Scholar]
- 10.di Meo N, Fluehler C, Perkan V, Trevisan G. Disseminated superficial porokeratosis and pyoderma gangrenosum. Dermatol Online J. 2010;16(10):15. PMid:21062609. [PubMed] [Google Scholar]
- 11.Mundi JP, Cerullo L, Cotliar J. Porokeratosis in a patient with hepatitis of unclear etiology. J Drugs Dermatol. 2010;9(3):258–60. PMid:20232588. [PubMed] [Google Scholar]
- 12.Monteagudo-Sánchez B, Ginarte M, Durana C, Labandeira J, de las Heras C, Cacharrón JM. Porokeratosis in a patient with dermatomyositis. Actas Dermosifiliogr. 2006;97(10):650–2. doi: 10.1016/s0001-7310(06)73487-1. https://doi.org/10.1016/S0001-7310(06)73487-1. [DOI] [PubMed] [Google Scholar]
- 13.Kluger N, Guilpain P, Leclerc-Mercier S, Emilie S, Guillevin L, Mouthon L. Superficial porokeratosis of the lower limbs during systemic scleroderma. Presse Med. 2009;38(1):146–8. doi: 10.1016/j.lpm.2008.06.023. https://doi.org/10.1016/j.lpm.2008.06.023 PMid:18990541. [DOI] [PubMed] [Google Scholar]
- 14.Terranova M, Amato L, Massi D, Fabbri P. Disseminated superficial actinic porokeratosis in a patient with Sjögren syndrome. Skinmed. 2003;2(6):390–1. doi: 10.1111/j.1540-9740.2003.02261.x. https://doi.org/10.1111/j.1540-9740.2003.02261.x PMid:14673257. [DOI] [PubMed] [Google Scholar]
- 15.Jung JY, Yeon JH, Ryu HS, Youn SW, Park KC, Huh CH. Disseminated superficial porokeratosis developed by immunosuppression due to rheumatoid arthritis treatment. J Dermatol. 2009;36(8):466–7. doi: 10.1111/j.1346-8138.2009.00678.x. https://doi.org/10.1111/j.1346-8138.2009.00678.x PMid:19691753. [DOI] [PubMed] [Google Scholar]
- 16.CannavóSP Borgia F, Adamo B, Guarneri B. Simultaneous development and parallel course of disseminated superficial porokeratosis and ovarian cancer:Coincidental association or true paraneoplastic syndrome? J Am Acad Dermatol. 2008;58(4):657–60. doi: 10.1016/j.jaad.2007.12.030. https://doi.org/10.1016/j.jaad.2007.12.030 PMid:18258333. [DOI] [PubMed] [Google Scholar]
- 17.Rongioletti F1, Rebora A. Disseminated porokeratosis with fatal metastatic squamous cell carcinoma:an additional case of “malignant disseminated porokeratosis”. Am J Dermatopathol. 2002;24(2):144–8. doi: 10.1097/00000372-200204000-00007. https://doi.org/10.1097/00000372-200204000-00007. [DOI] [PubMed] [Google Scholar]
- 18.Brodkin RH, Rickert RR, Fuller FW, Saporito C. Malignant disseminated porokeratosis. Arch Dermatol. 1987;123(11):1521–6. https://doi.org/10.1001/archderm.1987.01660350121027 PMid:3674910. [PubMed] [Google Scholar]
- 19.Kanitakis J, Arbona-Vidal E, Faure M. Porokeratosis in patients with polycythemia rubra vera:a new side effect of hydroxyurea? J Eur Acad Dermatol Venereol. 2012;26(8):1040–1. doi: 10.1111/j.1468-3083.2011.04202.x. https://doi.org/10.1111/j.1468-3083.2011.04202.x PMid:21812837. [DOI] [PubMed] [Google Scholar]
- 20.Torchia D, Romanelli P, Schachner LA. Disseminated superficial actinic porokeratosis associated with pseudoxanthoma elasticum. Eur J Dermatol. 2011;21(4):600–1. doi: 10.1684/ejd.2011.1376. PMid:21616751. [DOI] [PubMed] [Google Scholar]
- 21.Benmously Mlika R, Kenani N, Badri T, Ben Romdhane S, Debbiche A, Souissi A, Ben Ayed M, Mokhtar I, Fenniche S. Localized genital porokeratosis in a female patient with multiple myeloma. J Eur Acad Dermatol Venereol. 2009;23(5):584–5. doi: 10.1111/j.1468-3083.2008.02967.x. https://doi.org/10.1111/j.1468-3083.2008.02967.x PMid:18759788. [DOI] [PubMed] [Google Scholar]
- 22.Luelmo-Aguilar J, Gonzalez-Castro U, Mieras-Barcelo C, Castells-Rodellas A. Disseminated porokeratosis and myelodysplastic syndrome. Dermatology. 1992;184(4):289. doi: 10.1159/000247571. https://doi.org/10.1159/000247571 PMid:1498397. [DOI] [PubMed] [Google Scholar]
- 23.Levin RM, Heymann WR. Superficial disseminate porokeratosis in a patient with myelodysplastic syndrome. Int J Dermatol. 1999;38(2):138–9. doi: 10.1046/j.1365-4362.1999.00504.x. https://doi.org/10.1046/j.1365-4362.1999.00504.x. [DOI] [PubMed] [Google Scholar]
- 24.Inamoto N, Watanabe T, Nakamura K. Porokeratosis of Mibelli:benzylhydrochlorothiazide-induced new lesions accompanied by eosinophilic spongiosis. J Am Acad Dermatol. 1984;11(2 Pt 2):357–61. doi: 10.1016/s0190-9622(84)70172-1. https://doi.org/10.1016/S0190-9622(84)70172-1. [DOI] [PubMed] [Google Scholar]
- 25.Nakamura Y, Yamaguchi M, Nakamura A, Muto M. Calcipotriol and adapalene therapy for disseminated superficial actinic porokeratosis. Indian J Dermatol Venereol Leprol. 2014;80:373–4. doi: 10.4103/0378-6323.136981. https://doi.org/10.4103/0378-6323.136981 PMid:25035379. [DOI] [PubMed] [Google Scholar]
- 26.Böhm M, Luger TA, Bonsmann G. Disseminated superficial actinic porokeratosis:treatment with topical tacalcitol. J Am Acad Dermatol. 1999;40(3):479–80. doi: 10.1016/s0190-9622(99)70502-5. https://doi.org/10.1016/S0190-9622(99)70502-5. [DOI] [PubMed] [Google Scholar]
- 27.Tchernev G, Chokoeva AA, Ivanova B, Mangarov H, Vidolova NG. Disseminated superficial actinic porokeratosis (DSAP):significant improvement after local administration of calcipotriol/betamethasone gel? Wien Med Wochenschr. 2017;167(3-4):85–88. doi: 10.1007/s10354-016-0484-8. https://doi.org/10.1007/s10354-016-0484-8 PMid:27468973. [DOI] [PubMed] [Google Scholar]


