Abstract
OBJECTIVE:
To describe the benefits and safety of using Carbon Dioxide Laser in multi-pulse modalities when performing labiaplasty and anatomical variants approach for functional and cosmetic indications.
DESIGN:
This is a prospective, descriptive case series study.
SETTING:
Private Practice Quirofano Calculaser Megacentro Pinares Pereira Colombia.
POPULATION:
One Hundred and twelve women seeking labia minora labiaplasty for functional and cosmetic reasons were enrolled in the study protocol from June 2013 to June 2016. Labia minora labioplasty and anatomical variants approach were performed with Carbon Dioxide laser Multi-pulse modalities DEKA M.EL.A Florence Italy
MAIN OUTCOME MEASURES:
Good Cosmetic results, functional and sexuality improvement
RESULTS:
Dramatic changes in the VAS and VSQ were detected after the surgical procedure. All the participants reported a high degree of satisfaction, felt more confident with their partners during sexual encounters, and the procedure was well tolerated.
CONCLUSION:
Laser Carbon Dioxide Laser with a new pulse profile and shape seems to be a safe and precise surgical tool to perform this type of procedures, optimal biophysical and bio stimulative laser-tissue interactions allow delicate vulvar tissues to shorten downtime.
Keywords: labia minora hypertrophy, labial reduction, vulvar surgery, dermatologic cosmetic gynecologic surgery, labiaplasty, nymphoplasty, Carbon Dioxide Laser CO2
Introduction
Increasing number of patients are seeking medical attention, due to concerns about labia minora hypertrophy related to cosmetic, functional, and sexual concerns [1]. Gynecologists from around the world are nowadays confronted with an increasing demand for labia reduction surgery, the National Health Service (NHS) in the United Kingdom reported at least the doubling of the number of labia reductions carried out in the UK in 2004 compared with 1998 [2].
Hodgkinson was one of the firsts to publish a description of a labiaplasty procedure in 1983 [3]. Rouzier and colleagues presented their experience with a large series of patients [4]. Labiaplasty technique has also been described by many other authors, such as Munhoz [5], Maas [6], Giraldo [7], and Rauso [8]. These techniques were performed with common surgical techniques, without the aid of energy source or laser devices. Pardo and colleagues reported hemostatic advantages of using laser devices when performing this procedure, with high rates of patient satisfaction and few rate of complications [9].
Laser energy sources have been used in gynaecology for more than three decades [10]. There are many described advantages, such as bactericidal, bio-regenerative and bio-stimulating effects on tissues, which allows better healing, faster recovery, less pain and better aesthetic results.
This study aimed to demonstrate the benefits and safety of multi-pulsed CO2 Laser when performing a labiaplasty procedure and to demonstrate with histological samples the lateral thermal damage between the different pulses.
Materials and Methods
In the present study protocol, were enrolled one hundred and twelve women aged between 15 and 62 years (mean 32.63) attending a private cosmetic gynaecology unit from January 2013 to January 2016, seeking labia minora labiaplasty for functional and cosmetic indications. The main indications for labiaplasty were identified as: functional (40%), cosmetic (30%), sexual (20%), and cultural (10%).
The Gonzalez Labia Minora Hypertrophy Classification was used to determine the degree of hypertrophy and to choose the best technique to be performed in each patient [11]. The Visual Analog Scale (VAS) was used to compare the degree of satisfaction and comfort with sexual partners during intercourse. The Vulvovaginal Symptom Questionnaire (VSQ) was used to measure symptoms, emotions, life-impact, and sexual-impact before and after surgery. The first seven questions of the VSQ comprise symptoms subscale (itching, burning, hurting, irritation, dryness, discharge, and odour). Women who answered “Yes” to any of the first seven symptoms questions were considered to have vulvovaginal symptoms, and sexual impact (Yes to ≥1 out of 4 sexual impact subscale items).
Statistical analysis was performed using SPSS 11.5.1 (SPSS, Chicago, Illinois. the USA). Quantitative variables deal with the following parameters: mean, median, and standard deviation before and after surgery.
Labiaplasty was performed with a Carbon Dioxide Laser 10,600 nm (Deka M.E.LA., Florence, Italy) in different pulse modes, profile, and shape, to achieve efficient cutting and coagulation during the procedure. Labiaplasty was carried out in the surgical room under regional or general anaesthesia; meantime procedure was about 60 minutes. The surgeon preferred technique was the Grees technique [12], which allows the appropriate approach of common vulvar anatomical variants.
Results
Outcomes were analyzed with validated tools: Vulvovaginal Symptom Questionnaire (VSQ) and Visual Analog Scale (VAS) before and at least one month after CO2 Laser labiaplasty. An image report has been carried out (Fig. 1).
Figure 1.

a) Labia minora hypertrophy II-A-A (Gonzalez Classification); b) Pre-surgery markings; c) Immediate post-surgery; Right side DP mode; Left side SP mode; d) 2-month post-surgery
All the patients completed the study, scores for overall satisfaction and comfort with partners during sexual intercourse were dramatically improved after surgery in both groups respectively 7.3 ±1.6 to 2.3 ± 0.89, and 7.4 ± 1.0 to 1.89 ± 0.74 (Tables 1 and 2).
Table 1.
Visual Analogue Scale (VAS) for overall satisfaction, before and after surgery, expressed as mean value standard deviation

Table 2.
Visual Analogue Scale (VAS) for self-confidence during intercourse, before and after surgery, expressed as mean value standard deviation

Overall Vulvovaginal Symptom Questionnaire (VSQ) before surgery was 7.0 ± 0.79 and after Labiaplasty 0.65 ± 0.63.
For women reporting one or more vulvovaginal symptom, before surgery 70.5% (n = 79/112) reported emotional impact (Yes to ≥1 out of 4 emotional impact subscale items) and 94.6% (n = 106/112) reported lifestyle impact (Yes to ≥1 out of 5 lifestyle impact subscale items) from these symptoms. For sexually active women reporting vulvovaginal symptoms, 83% (n = 93/112) reported sexual impact (Yes to ≥1 out of 4 sexual impact subscale items).
One month after surgery the percentage was found to be dramatically lower as follows: for women reporting one or more vulvovaginal symptom, after surgery 10% (n = 11/112) reported emotional impact (Yes to ≥1 out of 4 emotional impact subscale items), and 8% (n = 7/112) reported lifestyle impact (Yes to ≥1 out of 5 lifestyle impact subscale items) from these symptoms.
For sexually active women reporting vulvovaginal symptoms, 7% (n = 6/112) reported sexual impact (Yes to ≥ 1 out of 4 sexual impact subscale items) (Table 3).
Table 3.
Domains of vulvovaginal symptoms from the Vulvo Vaginal Symptom Questionnaire (VSQ), expressed as a percentage. n is the correlated number of women over the total 112 enrolled ones

Biopsies of the excess skin of the vulva were obtained to corroborate histological changes after CO2 Laser Labiaplasty (Fig. 2). Lateral thermal damage (TRT) was measured in millimetres with traditional staining methods Hematoxylin and Eosin (Fig. 3).
Figure 2.
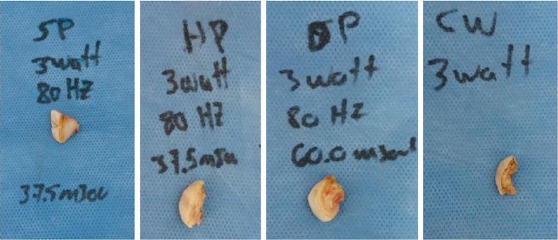
Samples cut with different modes (3W, 80 Hz): SP, HP, DP, CW
Figure 3.
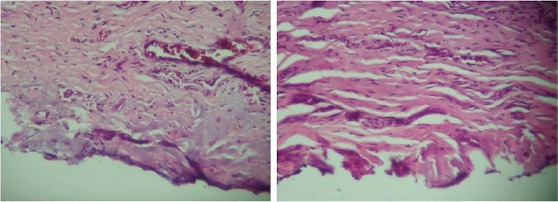
Samples stained using Hematoxylin and Eosin. Left) DP cutting mode TRT 1.3 mm. Right) SP cutting mode TRT 1.1 mm
Discussion
Vulvovaginal symptoms are common and present in an important percentage of patients with labia minora hypertrophy. Many of these patients have emotional, lifestyle, and sexual discomforts due to these symptoms. A labiaplasty with the right indication and performed by a high skilled cosmetic gynaecology surgeon can improve sexuality, self-esteem and overall satisfaction in symptomatic patients suffering from this condition.
CO2 Laser with new pulse profile and shape seems to be a safe and precise surgical tool to perform this type of procedure. Optimal biophysical and bio-stimulating laser-tissue interactions allow delicate vulvar tissues to shorten downtime.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.Miklos JR, Moore RD. Labiaplasty of the labia minora:patients'indications for pursuing surgery. J Sex Med. 2008;5:1492–5. doi: 10.1111/j.1743-6109.2008.00813.x. https://doi.org/10.1111/j.1743-6109.2008.00813.x PMid:18355172. [DOI] [PubMed] [Google Scholar]
- 2.Liao LM, Creighton SM. Requests for cosmetic genitoplasty:how should healthcare providers respond? BMJ. 2007;334(7603):1090–2. doi: 10.1136/bmj.39206.422269.BE. https://doi.org/10.1136/bmj.39206.422269.BE PMid:17525451 PMCid:PMC1877941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hodgkinson DJ, Hait G. Aesthetic vaginal labioplasty. Plast Reconstr Surg. 1984;74(3):414–6. doi: 10.1097/00006534-198409000-00015. https://doi.org/10.1097/00006534-198409000-00015. [DOI] [PubMed] [Google Scholar]
- 4.Rouzier R, Louis-Sylvestre C, Paniel BJ, Haddad B. Hypertrophy of labia minora:experience with 163 reductions. Am J Obstet Gynecol. 2000 Jan;182(1 Pt 1):35–40. doi: 10.1016/s0002-9378(00)70488-1. https://doi.org/10.1016/S0002-9378(00)70488-1. [DOI] [PubMed] [Google Scholar]
- 5.Munhoz AM, Filassi JR, Ricci MD, Aldrighi C, Correia LD, Aldrighi JM, Ferreira MC. Aesthetic labia minora reduction with inferior wedge resection and superior pedicle flap reconstruction. Plast Reconstr Surg. 2006;118(5):1237–47. doi: 10.1097/01.prs.0000237003.24294.04. discussion:1248-50. https://doi.org/10.1097/01.prs.0000237003.24294.04 PMid:17016196. [DOI] [PubMed] [Google Scholar]
- 6.Maas SM, Hage JJ. Functional and aesthetic labia minora reduction. Plast Reconstr Surg. 2000;105(4):1453–6. doi: 10.1097/00006534-200004040-00030. PMid:10744241. [DOI] [PubMed] [Google Scholar]
- 7.Giraldo F, González C, de Haro F. Central wedge nymphectomy with a 90-degree Z-plasty for aesthetic reduction of the labia minora. Plast Reconstr Surg. 2004;113(6):1820–5. doi: 10.1097/01.prs.0000117304.81182.96. discussion:1826-7. [DOI] [PubMed] [Google Scholar]
- 8.Rauso R, Tartaro G, Salti G, Zerbinati N, Colella G. Utilization of Needles in the Surgical Reduction of Labia Minora:A Simple and Cost-Effective Way to Reduce Operating Time. Aesthet Surg J. 2016;36(10):NP310–2. doi: 10.1093/asj/sjw159. https://doi.org/10.1093/asj/sjw159 PMid:27625031. [DOI] [PubMed] [Google Scholar]
- 9.Pardo J, Sola V, Ricci P, Guilloff E. Laser labioplasty of labia minora. Int J Gynecol Obstet. 2006;93:38–43. doi: 10.1016/j.ijgo.2006.01.002. https://doi.org/10.1016/j.ijgo.2006.01.002 PMid:16530764. [DOI] [PubMed] [Google Scholar]
- 10.Aggish MS. Carbon dioxide laser treatment for condyloma acuminata venereal infections. Obstetrics and Gynecology. 1980;5:711–5. [PubMed] [Google Scholar]
- 11.Gonzalez P. Labia Minora Hypertrophy Classification. Consideration of a multiple component approach. Surgical Tech Inter. 2015;27:191–4. PMid:26680395. [PubMed] [Google Scholar]
- 12.Grees S. Composite Reduction Labiaplasty. Aesth Plast Surg. 2013;37:674–83. doi: 10.1007/s00266-013-0149-6. https://doi.org/10.1007/s00266-013-0149-6 PMid:23728471. [DOI] [PubMed] [Google Scholar]


