Abstract
Epidermoid cysts are common benign lesions of hair-bearing, and less often glabrous skin. They can also occur in oral mucosa and internal organs. In case of cutaneous lesions, an epidermal punctum is a clinical diagnostic hallmark. The clinical presentation is variable leading to some differential diagnoses. Diagnosis of epidermoid cysts needs histopathological confirmation – not only of the potential of malignant transformation. The treatment of choice is surgery. We report a retrospective analysis of 2159 epidermoid cysts treated surgically. Most of the cases can be performed under local anaesthesia. The complication rate of 2.2% is low. To avoid relapses, the cyst wall has to be removed completely. Rare genetic disorders with multiple cysts are Gardner and Lowe syndrome.
Keywords: Epidermoid cysts, Pathogenesis, Skin, Surgery, Gardner syndrome, Lowe syndrome
Introduction
Epidermoid cysts are slow-growing benign subcutaneous lesions imposing as nodules or tumours. The lesions can either be congenital or acquired. Histologically, the cysts are lined by stratified epithelium and filled with a keratinous mass. An epidermal punctum is a hallmark of clinical diagnosis. Young males are the most affected subgroup, but any age and gender might be involved [1].
These cysts can develop in any area of the body with about 7% occurring in the head-and-neck region. Extracutaneous development has been observed in the oral cavity and intraosseous, and in various internal organs including the cerebrum [2][3][4]. Secondary infection and inflammation due to wall rupture are possible complications. The cyst wall tends to become thicker after that what implies complete surgical excision [5].
Giant epidermoid cysts > 5 cm in diameter can cause problems, especially in the head-and-neck region but also in other regions such as the sole [6-8]. Malignant transformation of an epidermoid cyst is a rare event but possible. Squamous cell carcinoma, basal cell carcinoma, and Merkel cell carcinoma have been observed [9][10][11].
Material and Methods
We analysed the files of the Department of Dermatology and Allergology, Academic Teaching Hospital of Dresden, during the years 2007-2017. We focused on those patients who were treated surgically. We analysed the anatomical distribution, the occurrence of giant epidermoid cysts defined by a diameter of more than 5 cm, complications and surgical outcome.
Results
We identified 2159 tumours in 1753 patients. The sex ratio was 2.9:1 for males to females. The mean age was 32.5 years (SD ± 18.3 years; range 16 to 83 years). The major localizations were head-and-neck region (73.4%), trunk (15.1%), extremities (9.8%), and genitals (1.7%).
Inflammation and or infection were noted in 16.8%. In these cases, antibiotic drug therapy was performed before surgery. The rupture was noted histologically in 23.7%. Giant epidermoid cysts were observed in 2.1%.
The variability of clinical presentations is illustrated in Fig. 1. This has led to a variety of suspected diagnoses such as lipoma, hidrocystoma, dermoid cyst, trichilemmal cyst, steatocystoma, pyoderma, cutaneous metastasis and benign adnexal tumours of the skin.
Figure 1.
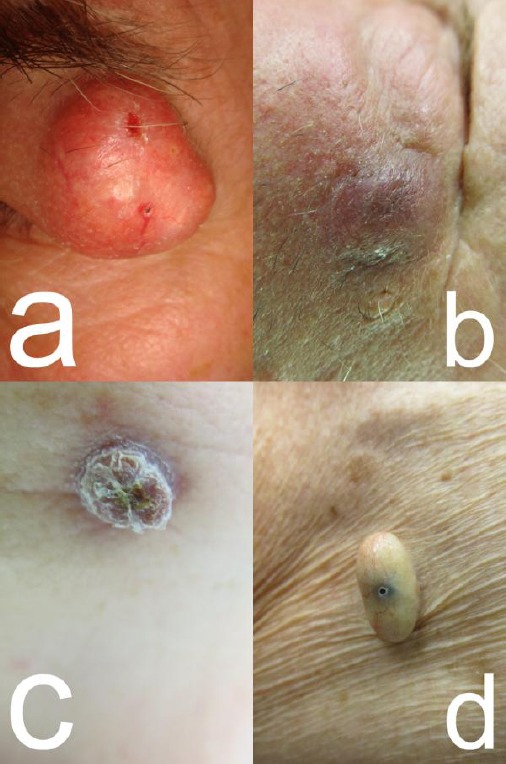
Clinical variability of epidermoid cysts; (a) Large cysts of the lateral brow imposing as a lipoma; (b) Retroauricular inflammatory cyst in a cancer patient – here a cutaneous metastasis was suspected; (c) Ruptured cyst of submandibular localisation; (d) Pediculated cyst on the trunk
Histopathology was performed for all cases removed by surgery. We did not observe a single malignant transformation among our tumours.
Surgery was realised with local anaesthesia in 98.9%; the remaining cases were treated under general anaesthesia. Postsurgical complications were noted in 2.2%, such as wound dehiscence, secondary bacterial infection, or hypertrophic scarring. Infectious complications were more frequent in diabetic patients and patients with iatrogenic immunosuppression.
A selection of clinical presentations and surgery is added (Fig. 2 and 3). To avoid skin sagging after removal of large or giant epidermoid cysts removal of an epidermal sheet is recommended.
Figure 2.

Surgery of a large epidermoid cyst of the glabella. (a) Clinical presentation; (b) Preparation of the cyst after mobilisation. (c) Surgical specimen
Figure 3.
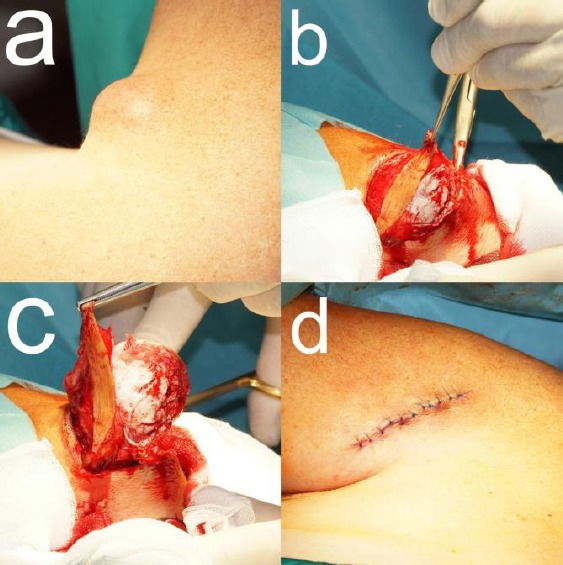
Surgery of a giant epidermoid cyst of the forearm. (a) Clinical presentation; (b) Preparation of the cyst leaving a small epidermal sheet for fixing with the forceps and mobilisation with a small scissor; (c) presentation of the surgical specimen; (d) Defect closure by tissue advancement and tow layered suturing
Discussion
Although the preferred localisation of epidermoid cysts is hair-bearing skin, they have also been seen on the glabrous skin and mucous membranes. Acquired cysts are thought to develop after blunt, penetrating trauma form either hair follicle infundibulum or eccrine sweat ducts [12]. The role of human papilloma virus in epidermoid cyst pathogenesis has been debated [13].
Multiple epidermoid cysts suggest a genetic background. They can occur in Gardner syndrome caused by mutations in the adenomatous polyposis coli gene [14], or in Lowe syndrome, an X-chromosomal oculo-cerebral-renal disorder caused by mutations of the OCLR1-gene [15].
We did not observe these genetic disorders among our patients. Epidermoid cysts of the subcutaneous tissue raise some possible differential diagnoses (Table 1).
Table 1.
Differential diagnoses of subcutaneous epidermoid cysts
| Entity | Remarks |
|---|---|
| Dermoid cysts | Ectodermal cysts may contain squamous epithelium and dermal contents |
| Trichilemmal cysts | Often on the scalp, family history, multiple, trichilemmal keratinisation |
| Pilomatricoma | Common in children, mostly head-and-neck region, hard, painless |
| Lipoma | Common, often soft, composed of mature adipocytes with a fibrous capsule |
While small cysts may be treated by CO2- or erbium-YAG-laser [16][17][18][19], larger cysts need a surgical approach with cold steel [3][7][8]. Since skin sagging is a possible outcome after removal of larger cysts, a small sheet of the epidermis above the cyst is excised. This allows an individualised adaption of the surgical margins. To avoid relapses, complete removal of the cyst wall is mandatory. All epidermoid cysts removed surgically should be subjected to histopathological confirmation, to ensure complete excision and avoid misdiagnosis. Possible malignant transformation, although not seen in our cases, is another important argument for regular histopathologic analysis [20].
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.Plewig G, Landthaler M, Burgdorf W, Hertl M, Ruzicka T. Braun-Falco's Dermatologie, Venerologie und Allergologie. 6th edition. Berlin – Heidelberg: Springer; 2012. https://doi.org/10.1007/978-3-642-24163-5. [Google Scholar]
- 2.Janarthanam J, Mahadevan S. Epidermoid cyst of submandibular region. J Oral Maxillofac Pathol. 2012;16(3):435–7. doi: 10.4103/0973-029X.102511. https://doi.org/10.4103/0973-029X.102511 PMid:23248482 PMCid:PMC3519225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kumar U, Lamba S. Intraosseous epidermal inclusion cyst of the great toe:masquerading as bone tumour. J Clin Diagn Res. 2017;11(6):EJ01–EJ02. doi: 10.7860/JCDR/2017/29249.10100. https://doi.org/10.7860/JCDR/2017/29249.10100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yao PS, Lin ZY, Zheng SF, Lin YX, Yu LH, Jiang CZ, Kang DZ. Coexistence of intracranial epidermoid tumor and multiple cerebral aneurysms:A case report and literature review. Medicine (Baltimore) 2017;96(5):e6012. doi: 10.1097/MD.0000000000006012. https://doi.org/10.1097/MD.0000000000006012 PMid:28151901 PMCid:PMC5293464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Min HJ, Lee JM, Han JK, Kim YJ. Influence factor in thickness of cyst wall of epidermal cysts. J Craniofac Surg. 2017;28(4):e369–72. doi: 10.1097/SCS.0000000000003687. https://doi.org/10.1097/SCS.0000000000003687 PMid:28328606. [DOI] [PubMed] [Google Scholar]
- 6.Ramakrishnaiah SB, Rajput SS, Gopinathan NS. Epidermoid cyst of the sole - a case report. J Clin Diagn Res. 2016;10(11):PD06–PD07. doi: 10.7860/JCDR/2016/23225.8787. https://doi.org/10.7860/JCDR/2016/23225.8787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Utumi ER, Araujo JP, Pedron IG, Yonezaki F, Machado GG, Rocha AC. Extensive epidermoid cyst of the submental region. Autops Case Rep. 2016;6(2):51–4. doi: 10.4322/acr.2016.031. https://doi.org/10.4322/acr.2016.031 PMid:27547744 PMCid:PMC4982785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nishar CC, Ambulgekar VK, Gujrathi AB, Chavan PT. Unusually giant sublingual epidermoid cyst:a case report. Iran J Otorhinolaryngol. 2016;28(87):291–6. PMid:27602342 PMCid:PMC4994990. [PMC free article] [PubMed] [Google Scholar]
- 9.Liau JL, Altamura D, Ratynska M, Verdolini R. Basal cell carcinoma arising from an epidermal cyst:when a cyst is not a cyst. Case Rep Dermatol. 2015;7(1):75–8. doi: 10.1159/000381393. https://doi.org/10.1159/000381393 PMid:26034477 PMCid:PMC4448066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sze S, Richmond I, Bickers A, Saha A. Squamous cell carcinoma arising from a vulval epidermal cyst. J Obstet Gynaecol Res. 2016;42(11):1623–6. doi: 10.1111/jog.13091. https://doi.org/10.1111/jog.13091 PMid:27785896. [DOI] [PubMed] [Google Scholar]
- 11.Aljufairi E, Alhilli F. Merkel cell carcinoma arising in an epidermal cyst. Am J Dermatopathol. 2016 doi: 10.1097/DAD.0000000000000745. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 12.Choi JE, Kwon IH, Seo SH, Kye YC, Ahn HH. Pathogenesis of plantar epidermal cyst:Three-dimensional reconstruction analysis. Ann Dermatol. 2016;28(1):133–5. doi: 10.5021/ad.2016.28.1.133. https://doi.org/10.5021/ad.2016.28.1.133 PMid:26848239 PMCid:PMC4737825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Egawa K, Egawa N, Honda Y. Human papillomavirus-associated plantar epidermoid cyst related to epidermoid metaplasia of the eccrine duct epithelium:a combined histological, immunohistochemical, DNA-DNA in situ hybridization and three-dimensional reconstruction analysis. Br J Dermatol. 2005;152(5):961–7. doi: 10.1111/j.1365-2133.2005.06562.x. https://doi.org/10.1111/j.1365-2133.2005.06562.x PMid:15888153. [DOI] [PubMed] [Google Scholar]
- 14.Koh KJ, Park HN, Kim KA. Gardner syndrome associated with multiple osteomas, intestinal polyposis, and epidermoid cysts. Imaging Sci Dent. 2016;46(4):267–72. doi: 10.5624/isd.2016.46.4.267. https://doi.org/10.5624/isd.2016.46.4.267 PMid:28035305 PMCid:PMC5192025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ikehara S, Utani A. Multiple protrusive epidermal cysts on the scalp of a Lowe syndrome patient. J Dermatol. 2017;44(1):105–7. doi: 10.1111/1346-8138.13444. https://doi.org/10.1111/1346-8138.13444 PMid:27178641. [DOI] [PubMed] [Google Scholar]
- 16.Reynolds N, Kenealy J. Use of a carbon dioxide laser in the treatment of multiple epidermoid cysts. Br J Plast Surg. 2002;55(3):260–1. doi: 10.1054/bjps.2002.3790. https://doi.org/10.1054/bjps.2002.3790 PMid:12041985. [DOI] [PubMed] [Google Scholar]
- 17.Feng CJ, Ma H. Treatment of epidermal cysts with erbium:YAG laser fenestration:an alternative to surgical intervention. Ann Plast Surg. 2015;74(Suppl 2):S89–92. doi: 10.1097/SAP.0000000000000463. https://doi.org/10.1097/SAP.0000000000000463 PMid:25695444. [DOI] [PubMed] [Google Scholar]
- 18.Calderón-Castrat X, Santos-Durán JC, Román-Curto C, Fernández-López E. Carbon dioxide laser:A therapeutic approach for multiple vulvar epidermoid cysts. Dermatol Surg. 2016;42(2):264–7. doi: 10.1097/DSS.0000000000000614. https://doi.org/10.1097/DSS.0000000000000614 PMid:26845541. [DOI] [PubMed] [Google Scholar]
- 19.Wollina U. Erbium-YAG laser therapy –analysis of more than 1,200 treatments. Glob Dermatol. 2016;3(2):268–72. https://doi.org/10.15761/GOD.1000171. [Google Scholar]
- 20.Morritt AN, Tiffin N, Brotherston TM. Squamous cell carcinoma arising in epidermoid cysts:report of four cases and review of the literature. J Plast Reconstr Aesthet Surg. 2012;65(9):1267–9. doi: 10.1016/j.bjps.2012.02.007. https://doi.org/10.1016/j.bjps.2012.02.007 PMid:22364661. [DOI] [PubMed] [Google Scholar]


