Abstract
AIM:
Hidradenitis suppurativa (HS) is a chronic inflammatory disease, commonly characterized by painful, deep dermal abscesses and chronic draining sinus tracts. Recently, laser and light-based therapies have become more commonly used in the management of HS.
MATERIAL AND METHODS:
We report 20 HS patients treated with a 1064 nm wavelength, emitted from a diode laser, launched in an optical fibre through intracavitary modalities.
RESULTS:
Each patient underwent four laser sessions, one every two weeks. we recorded a significative reduction (31%) of Sartorius score from 28.55 ± 13.04 to 19.75 ± 12.29 after 4 laser sessions (p < 0.05). No one has had a worsening of the disease.
CONCLUSION:
Intralesional diode laser 1064 nm can be a good treatment option for patients with moderate and localized hidradenitis suppurativa, because it is minimally invasive, doesn’t have significant complications and provides a rapid post-treatment recovery.
Keywords: diode laser, 1064 nm, hidradenitis suppurativa, human treatment, chronic inflammatory disease
Introduction
Hidradenitis suppurativa (HS) is a chronic inflammatory disease, commonly characterized by painful, deep dermal abscesses and chronic draining sinus tracts [1][2]. Classically, pharmacologic agents ranging from antibiotics, isotretinoin, acitretin, anti-androgens and various biological agents such as Adalimumab and Infliximab, and surgical therapies have been effective for reducing lesion activity, and inflammation and have been shown to be helpful to treat the disease [3][4]. In several cases, these medications provide only transitory results, and they cannot act in the prevention of future recurrences or disease progression. No single agent has been proved to show overwhelmingly positive outcomes [5][6][7]. Recently, laser and light-based therapies have become more commonly used in the management of HS. Different kinds of laser-based therapies have been studied over the last years. The laser can act in 2 different modalities, selective and ablative. Intense Pulsed Light (IPL) and lasers like NdYag, Alexandrite and Diode act selectively and are considered the most useful in Hurley stage I-II, because of their ability to reduce the number of hair follicles, sebaceous glands, and consequently to reduce the bacterial load; the CO2 laser acts in ablative modality and seems to be more useful in Hurley stage II-III [8][9].
We report 20 HS patients treated with a 1064 nm wavelength, emitted from a diode laser, launched in an optical fibre through intracavitary modalities.
Materials and Methods
Twenty patients were recruited at the University Federico II of Naples, Section of Dermatology, from May 2016 to January 2017. The authors declare that their research complied with the guidelines for human studies and welfare regulation and the subjects participating in the research have given their informed consent. All patients were recommended to a wash-out period from any topical and systemic medications.
We excluded patients with significant comorbidities and those who were pregnant.
Each patient underwent four laser sessions, one every two weeks.
Hurley stage, Sartorius score and PGA were registered before starting laser therapies and at the end of these (after eight weeks - 4 sessions). Responses were classified as complete (improved by 65% or more), good (between 40% and 65%), partial (between 15% and 40%) and no response (less than 15%). Hidradenitis Suppurativa Clinical Response (HiSCR) was used as another tool to evaluate clinical response to the treatment.
Dermatology Quality of Life Index (DLQI) was recorded to judge the impact on the quality of life of HS patients before starting treatment and two weeks after the end of the study.
A diode laser with a wavelength of 1064nm in pulsed operation, launched in fibre from 300-600 μm (coated glass fibre polycarbonate) was used for the clinical study. This laser was supplied by Eufoton.
A standard energy fluence of 250 J/cm2 has been used, employing different diameters fibres depending on the type of the lesion and its anatomical localisation. In any case, the energy thresholds of 2500J on 10 cm2 were never exceeded.
Energy is delivered by a micro-variable pulse train from 150 to 350 milliseconds by the selected power energy.
The fibre size (400-600 microns) and the energy power selected (6 - 8 - 10 Watts) took into account the physiological condition of the lesion and the surrounding skin.
Local anaesthetic (Mepivacaine hydrochloride with epinephrine) was injected directly into the anatomical area involved by the disease, at the superficial subcutaneous plane.
A 30 G needle was used, and approximately 1 ml anaesthetic solution per cm2 was administered.
The infiltration was practised until obtaining tumescence of the concerned area. This procedure, particularly effective in controlling pain, was made possible thanks to the low water absorption for the wavelength of the laser.
Performed anaesthesia, the intervention included the identification of the orifices of suppurating lesions, the introduction of the optical fibre inside them and the subsequent decontamination-denaturing by the direct action of the laser on the pathological tissue. From the day of the laser-surgical procedure, all patients were subjected to an oral antibiotic treatment with azithromycin 500 mg once daily for three days. Four treatment sessions were performed, one every two weeks.
Results
The open clinical study was conducted in twenty patients aged between 18 and 44 years (mean age 26.6 ± 7.84) suffering from HS; anatomical sites involved by HS were the axillae, the groin, buttocks, the brisket and the infra-mammary fold (Table 1).
Table 1.
The open clinical study was conducted in twenty patients aged between 18 and 44 years (mean age 26.6 ± 7.84) suffering from HS; anatomical sites involved by HS were the axillae, the groin, buttocks, the brisket and the infra-mammary fold

50% of patients had a Hurley stage I, while the remaining subjects had a Hurley stage II; no patient with Hurley stage III was recruited.
All results are showed in Table 2. In summary, we recorded a significative reduction (31%) of Sartorius score from 28.55 ± 13.04 to 19.75 ± 12.29 after 4 laser sessions (p < 0.05).
Table 2.
Fifty percentages (50%) of patients had a Hurley stage I, while the remaining subjects had a Hurley stage II; no patient with Hurley stage III was recruited. We recorded a significative reduction (31%) of Sartorius score from 28.55 ± 13.04 to 19.75 ± 12.29 after four laser sessions (p<0.05). In particular, we registered the following clinical response: 1 patient with a complete response (improved by 65% or more); 7 patients with a good response (between 40% and 65%); 10 patients with a partial response (between 15% and 40%); 2 no response (less than 15%). No one has had a worsening of the disease. HiSCR, which is considered a useful tool in detecting changes after treatment, was achieved in 13 patients (65% of patients). Most notably HiSCR was achieved in 60% of patients with Hurley II and 80% patients with Hurley I
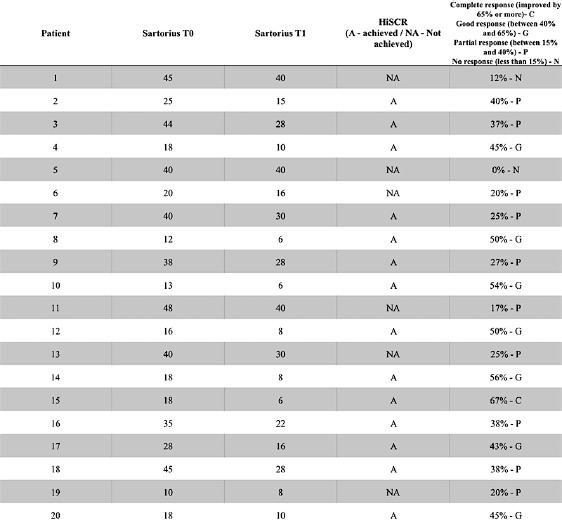
In particular, we registered the following clinical response:
One patient with a complete response (improved by 65% or more)
Seven patients with a good response (between 40% and 65%
Ten patients with a partial response (between 15% and 40%
Two no response (less than 15%).
No one has had a worsening of the disease.
HiSCR, which is considered a useful tool in detecting changes after treatment, was achieved in 13 patients (65% of patients). Most notably HiSCR was achieved in 60% of patients with Hurley II and 80% patients with Hurley I.
In parallel with clinical improvement, we registered a marked improvement in the quality of life of patients undergoing the treatment, showed by DLQI values reduction (p = 0.0307).
Most patients (18 of 20) tolerated the procedure without any symptoms. Adverse effects included postoperative pain, erythema, and mild swelling. One patient complained of fever and an influenza-like illness, which resolved itself. Serious adverse side effects, suppuration or infections did not occur.
Discussion
In several cases of HS patients, medical therapy is unsatisfactory, and it is very difficult to identify the way to stop the progression of the disease.
Laser treatment could represent an alternative therapy for the early stages of HS. Selective lasers, such as NdYag, Alexandrite and Diode, can be very useful in the early stage of disease [9][10]. On the other hand, ablative lasers are usually used in the worst cases. There are very few data in literature focused on the use of diode laser to improve symptoms of HS. The rational of the diode laser can be explained by the reduction in the number of hair follicles.
Downs et al. achieved a partial improvement of hidradenitis suppurativa with a sweating reduction following four treatments with a 1450 nm diode laser [11].
In 2011 Sehgal et al. reported favourable outcomes in a case report of Axillary HS using diode laser 800 nm after six sessions at an interval of 3 – 4 months (energy 34 J/cm 2, pulse duration 110 – 140 ms) [12].
Valladares-Narganes LM and colleagues reported twenty-seven patients affected by hidradenitis suppurativa treated with intralesional photodynamic therapy using a diode laser attached to an optical cable. They recorded very good results in almost 80% patients with best results achieved in isolated fistulas, axillary, sacral and breast locations, where the majority of cases are found [13].
A histopathological survey demonstrated the mechanism of action of the 1064 nm Nd: Yag laser in the treatment of HS: this type of laser penetrates the follicular unit and, through a selective photothermolysis, causes the destruction of organized inflammatory lesions in the superficial to mid dermis. The wavelength 1064 nm in the near-infrared electromagnetic spectrum selectively targets hair shafts and follicles via absorption by the melanin chromophore [15].
The wavelength used in our research can perform similarly and to get stackable results. Recently has been published an experience on 7 HS patients treated with photodynamic therapy with intralesional methylene blue and a 635 nm light-emitting diode lamp. After six months, five patients (71%) maintained remission of the disease in the treated area. Photodynamic therapy has been used for its ability to reduce bacterial biofilms, which is a common finding in hidradenitis lesions [16].
Also, some published clinical and histopathological data suggested that the Nd: YAG microsecond pulsed laser in optical glass fiber was able to sterilize by selective photoantisepsis all the affected areas and was also able to decrease the inflammation in the surrounding tissue [17]. Laser treatment proposed in our survey conjugate the laser action (1064 nm wavelength able to destroy follicular unit and organized inflammatory lesions) with the intralesional application of the light that allows reaching different depths (from the superficial to mild dermis). Treatment efficacy has been proved by the reduction of Sartorius score and by HiSCR. It is important to underline that only 4 patients had a marginal improvement and no one got worse.
Moreover, in comparison to surgery, our laser is less invasive; it has been performed under local anaesthesia and therefore does not require hospitalization. Also, the treatment is well tolerated by patients with very few adverse events, which don’t limit patient’s life (days of absence from work). This laser can be a good alternative for those patients that are not responsive to medical therapy. It can be performed in patients undergoing biologic treatment because it doesn’t increase the risk of immunosuppression and does not induce autoantibodies formation, therefore can repeatedly be used without complications.
The main restrictions of our survey are the small sample, but it is important to underline that prevalence remains uncertain and HS is frequently misdiagnosed as a simple infection.
In conclusion, the intralesional Diode laser 1064 nm can be a good treatment option for patients with moderate and localized hidradenitis suppurativa, because it is minimally invasive, doesn’t have significant complications and provides a rapid post-treatment recovery.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.Naik HB. Hidradenitis suppurativa, introduction. Semin Cutan Med Surg. 2017;36(2):41. doi: 10.12788/j.sder.2017.025. https://doi.org/10.12788/j.sder.2017.025 PMid:28538741. [DOI] [PubMed] [Google Scholar]
- 2.Hoffman LK, Ghias MH, Garg A, Hamzavi IH, Alavi A, Lowes MA. Major gaps in understanding and treatment of hidradenitis suppurativa. Semin Cutan Med Surg. 2017 Jun;36(2):86–92. doi: 10.12788/j.sder.2017.024. https://doi.org/10.12788/j.sder.2017.024 PMid:28538750. [DOI] [PubMed] [Google Scholar]
- 3.Kimball AB, Kerdel F, Adams D, Mrowietz U, Gelfand JM, Gniadecki R, Prens EP, Schlessinger J, Zouboulis CC, van der Zee HH, Rosenfeld M, Mulani P, Gu Y, Paulson S, Okun M, Jemec GB. Adalimumab for the treatment of moderate to severe Hidradenitis suppurativa:a parallel randomized trial. Ann Intern Med. 2012;157(12):846–55. doi: 10.7326/0003-4819-157-12-201212180-00004. https://doi.org/10.7326/0003-4819-157-12-201212180-00004 PMid:23247938. [DOI] [PubMed] [Google Scholar]
- 4.Kimball AB, Sobell JM, Zouboulis CC, Gu Y, Williams DA, Sundaram M, Teixeira HD, Jemec GB. HiSCR (Hidradenitis Suppurativa Clinical Response):a novel clinical endpoint to evaluate therapeutic outcomes in patients with hidradenitis suppurativa from the placebo-controlled portion of a phase 2 adalimumab study. Journal of the European Academy of Dermatology and Venereology. 2016;30(6):989–94. doi: 10.1111/jdv.13216. https://doi.org/10.1111/jdv.13216 PMid:26201313 PMCid:PMC5034809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Orenstein LA, Micheletti RG. Medical management of hidradenitis suppurativa. Semin Cutan Med Surg. 2017;36(2):62–66. doi: 10.12788/j.sder.2017.021. https://doi.org/10.12788/j.sder.2017.021 PMid:28538746. [DOI] [PubMed] [Google Scholar]
- 6.Scuderi N, Monfrecola A, Dessy LA, Fabbrocini G, Megna M, Monfrecola G. Medical and Surgical Treatment of Hidradenitis Suppurativa:A Review. Skin Appendage Disord. 2017;3(2):95–110. doi: 10.1159/000462979. https://doi.org/10.1159/000462979 PMid:28560220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hurley HJ. Axillary hyperhidrosis, apocrine bromhidrosis, hidradenitis suppurativa, and familial benign pemphigus:surgical approach. In: Roenigk RK, Roenigk HH, editors. Dermatologic Surgery. New York: Marcel Dekker; 1996. pp. 623–645. [Google Scholar]
- 8.Hamzavi IH, Griffith JL, Riyaz F, Hessam S, Bechara FG. Laser and light-based treatment options for hidradenitis suppurativa. J Am Acad Dermatol. 2015;73(5 Suppl 1):S78–81. doi: 10.1016/j.jaad.2015.07.050. https://doi.org/10.1016/j.jaad.2015.07.050 PMid:26470622. [DOI] [PubMed] [Google Scholar]
- 9.Sartorius K, Lapins J, Emtestam L, Jemec GB. Suggestions for uniform outcome variables when reporting treatment effects in hidradenitis suppurativa. Br J Dermatol. 2003;149(1):211–3. doi: 10.1046/j.1365-2133.2003.05390.x. https://doi.org/10.1046/j.1365-2133.2003.05390.x PMid:12890229. [DOI] [PubMed] [Google Scholar]
- 10.Finlay AY, Khan GK. Dermatology Life Quality Index (DLQI)--a simple practical measure for routine clinical use. Clin Exp Dermatol. 1994;19(3):210–6. doi: 10.1111/j.1365-2230.1994.tb01167.x. https://doi.org/10.1111/j.1365-2230.1994.tb01167.x. [DOI] [PubMed] [Google Scholar]
- 11.Downs AMR. Smoothbeam TM laser treatment may help improve hidradenitis suppurativa but not Hailey-Hailey disease. J Cosmet Laser Ther. 2004;6(3):163–164. doi: 10.1080/14764170410003002. https://doi.org/10.1080/14764170410003002. [DOI] [PubMed] [Google Scholar]
- 12.Sehgal VN, Verma P, Sawant S, Paul M. Contemporary surgical treatment of hidradenitis suppurativa (HS) with a focus on the use of the diode hair laser in a case. Journal of Cosmetic and Laser Therapy. 2011;13(4):180–90. doi: 10.3109/14764172.2011.594066. https://doi.org/10.3109/14764172.2011.594066 PMid:21714587. [DOI] [PubMed] [Google Scholar]
- 13.Valladares-Narganes LM, Rodríguez-Prieto MA, Blanco-Suárez MD, Rodriguez-Lage C, García-Doval I. Treatment of hidradenitis suppurativa with intralesional photodynamic therapy using a laser diode attached to an optical cable:a promising new approach. Br J Dermatol. 2015;172(4):1136–9. doi: 10.1111/bjd.13385. https://doi.org/10.1111/bjd.13385 PMid:25196140. [DOI] [PubMed] [Google Scholar]
- 14.Xu LY, Wright DR, Mahmoud BH, Ozog DM, Mehregan DA, Hamzavi IH. Histopathologic study of hidradenitis suppurativa following long-pulsed 1064-nmNd:YAG laser treatment. Arch Dermatol. 2011;147(1):21–8. doi: 10.1001/archdermatol.2010.245. https://doi.org/10.1001/archdermatol.2010.245 PMid:20855672. [DOI] [PubMed] [Google Scholar]
- 15.John H, Manoloudakis N, Stephen Sinclair J. A systematic review of the use of lasers for the treatment of hidradenitis suppurativa. J Plast Reconstr Aesthet Surg. 2016;69(10):1374–81. doi: 10.1016/j.bjps.2016.05.029. https://doi.org/10.1016/j.bjps.2016.05.029 PMid:27496291. [DOI] [PubMed] [Google Scholar]
- 16.Agut-Busquet E, Romaní J, Gilaberte Y, García-Malinis A, Ribera-Pibernat M, Luelmo J. Photodynamic therapy with intralesional methylene blue and a 635 nm light-emitting diode lamp in hidradenitis suppurativa:a retrospective follow-up study in 7 patients and a review of the literature. Photochem Photobiol Sci. 2016;15(8):1020–8. doi: 10.1039/c6pp00082g. https://doi.org/10.1039/C6PP00082G PMid:27417568. [DOI] [PubMed] [Google Scholar]
- 17.Zerbinati N, D'Este E, Ini L, Baruffato A, Premoli V, Calligaro A, Paulli M. Clinical and histological changes in Hidradenitis suppurativa following 1064 nm nd:YAG intralesional laser treatment. J Biol Regul Homeost Agents. 2017;31(2 Suppl. 2):131–140. PMid:28702973. [PubMed] [Google Scholar]


