India is home to the third largest number of people living with HIV (PLWH) in the world, with the epidemic disproportionately affecting men who have sex with men (MSM) and transgender women (TGW; AVERT, 2016). In 2013, HIV prevalence among Mumbai MSM (9.91%) was 10 times higher than in the general Mumbai population (< 1%). While there are state-funded HIV prevention interventions for MSM and TGW in India, including efforts by India’s National AIDS Control Organization (NACO), few programs have specifically focused on antiretroviral therapy (ART) uptake and adherence for MSM or TGW living with HIV (Ministry of Health and Family Welfare Government of India, 2013a). Although India has made great strides toward addressing the HIV epidemic, with a 57% decline in infection rates between 2001 and 2011, the focus of these efforts remains on containment, with significantly less attention to care and support for PLWH (Ministry of Health and Family Welfare Government of India, 2013a).
Of the estimated 2.1 million PLWH in India, only 36% are taking ART (Joint United Nations Programme on HIV/AIDS, 2013). To support treatment scale-up, prevent ART resistance, and prevent new HIV infections (based on the treatment-as-prevention paradigm), robust support is needed for ART uptake and adherence by those already living with HIV (Machtinger & Bangsberg, 2005; Rodger et al., 2016). No studies have specifically examined factors affecting ART use in MSM or TGW living with HIV in India. To address this, we conducted a survey study to better understand factors associated with ART adherence and inform interventions to optimize HIV treatment outcomes at a community based organization (CBO) serving sexual and gender minority populations in Mumbai, India.
Methods
Design and Setting
We conducted a cross-sectional, interviewer-administered survey study to MSM and TGW living with HIV and accessing services from a PLWH support program at the Humsafar Trust (HST), one of India’s first CBOs focusing on gender and sexual minority populations located in Mumbai, India. HST provides a broad array of social and health services, including onsite HIV and syphilis testing and counseling, sexually transmitted infection (STI) treatment, basic primary care services, and mental health counseling. HST also houses Sanjeevani, a PLWH support group that provides linkage-to-treatment, basic navigation, and social support services. Surveys were conducted between July and September 2014. During this time ART eligibility in India included either a CD4+ T cell lower than 350 cells/mm3 or a clinical stage III or IV according to the World Health Organization (Ministry of Health and Family Welfare Government of India, 2013b). The institutional review boards of Albert Einstein College of Medicine and the HST approved the study.
Participants
Inclusion criteria for participants in the study were (a) living with HIV infection, (b) MSM or hijra/transgender individual, (c) greater than 18 years of age, (d) ever had sexual contact with other men or hijra/transgender women, (e) registered client of HIV support program, (f) on ART, and (g) able to provide informed consent.
Recruitment and Procedures
Potential participants were identified by peer outreach staff from Sanjeevani, who then contacted them by phone or in-person to verify inclusion criteria, provide information about the study, and schedule research visits. Research visits were conducted in private rooms at a separate satellite location operated by HST to maintain confidentiality. After obtaining informed consent, two trained PLWH outreach workers administered surveys in Hindi, which took approximately 25 minutes. Participants were compensated 200 rupees (approximately $3.50 USD) as an incentive, an amount deemed appropriate by the peer outreach staff and HST’s Institutional Review Board. All participants had the opportunity to meet with adherence counselors after survey completion.
Survey Development
We iteratively developed the survey by first identifying potential factors affecting ART adherence in other populations in India (Joglekar et al., 2011; Logie, Newman, Chakrapani, & Shunmugam, 2012; Patel, Mayer, & Makadon, 2012; Steward et al., 2008; Thomas et al., 2005) and in MSM/TGW in other developing countries (Mills, Nachega, Bangsberg, et al., 2006; Mills, Nachega, Buchan, et al., 2006). Next, HST’s HIV counseling staff and peer outreach workers (n = 4) ranked each identified potential factor according to its perceived impact on adherence. We then pilot tested the survey with feedback from peer staff members. The survey and informed consent forms were translated from English into Hindi by a professional translation company, and the translated versions were reviewed and revised for conceptual synchrony, comprehension, and acceptability by bilingual HST staff (all native Hindi speakers).
Outcome Measures
ART eligibility and uptake
To evaluate antiretroviral uptake, we tabulated data from a registry of clients accessing the HIV support program at HST. We determined the number of clients currently served, number eligible for ART, and number currently taking ART.
ART adherence
We measured self-reported adherence in the previous month and in the previous 3 months using the questions: Please think back at the last MONTH. Please tell me how many pills have you missed? and In the last 3 MONTHS, about how many pills have you missed? We defined non-adherence, our primary outcome, as missing any doses (i.e., < 100% adherence) for each time period (Ekstrand, Chandy, Heylen, Steward, & Singh, 2010)
Factors Associated with Adherence
Participant characteristics
We collected data on age, gender, education, income, marital status (specifically, if currently married to a cis-gender woman), treatment access (government ART center or other), years on ART, and current medication side effects. We also measured sexual identity specific to the Indian context: MSM or gay, bisexual, kothi (MSM with traditionally more passive/receptive role), panthi (MSM with traditionally more dominant/insertive role), double-decker (MSM who practice both insertive and receptive intercourse), and hijra (often but not always considered to be a transgender person; Asthana & Oostvogels, 2001; Khan & Khan, 2006; Shinde, Setia, Row-Kavi, Anand, & Jerajani, 2009)
Psychological factors
We measured four psychological factors thought to impact adherence: (a) depressive symptoms, using the well-validated Center for Epidemiological Studies Depression Scale (CES-D 10; Cronbach’s alpha = 0.81), with scores of 10 or higher considered positive for clinically significant depression; (b) medication beliefs, using the Beliefs About Medicines Questionnaire (Cronbach’s alpha = 0.78; Horne, Weinman, & Hankins, 1999), with higher scores indicating more negative beliefs; (c) adherence-related self-efficacy, using the HIV Treatment Adherence Self-Efficacy Scale (Cronbach’s alpha = 0.86; Johnson et al., 2007) with higher scores indicating more self-efficacy; and (d) internalized homophobia, using the Internalized Homophobia Scale, modified to have transgender inclusive language (Cronbach’s alpha = 0.60), with higher scores representing more internalized stigma (Meyer, 1995).
Reasons for Non-Adherence
If a participant was non-adherent, at either 1 or 3 months, we asked those individuals about five common reasons for non-adherence, as indicated by the counseling staff, to understand why the participant may have missed a dose: (a) unable to obtain medication refills in time, (b) insufficient funds, (c) not having medications with them while travelling, (d) drinking alcohol, or (e) feeling healthy enough to skip medications. We also asked an open-ended question to elicit other reasons for non-adherence.
Data Analysis
To characterize the HIV care continuum in this sample, we calculated descriptive statistics to evaluate the proportion of the clients who were: (a) eligible for ART, (b) taking ART, (c) adherent at 1 month, and (d) adherent at 3 months. We then used chi-square and ANOVA tests to assess differences between those who were adherent and those who were non-adherent (using p < 0.10 to define significance due to the small sample size and exploratory nature of the study). We tabulated frequencies to describe reasons for non-adherence.
Results
ART Uptake and Adherence
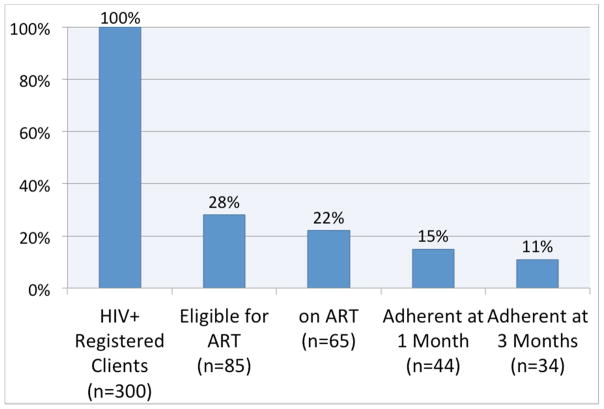
Of the 300 individuals registered for and accessing HST’s HIV support services at the time of the study, 28% (85/300) were eligible for ART through government ART centers and 22% (65/300) were using ART at the time of the study. Of those eligible for ART, 76% (65/85) were taking ART. Non-adherence was common, however, with only 68% (44/65) reporting adherence in the previous 1 month and 52% (34/65) reporting adherence in the previous 3 months (Figure 1).
Figure 1.
HIV care continuum among men who have sex with men and transgender women with HIV at a lesbian, gay, bisexual, transgender, and questioning community based organization in Mumbai, India.
Note. Percentage of registered clients with HIV at the community based organization, the Humsafar Trust, which is then further divided into those eligible for antiretroviral therapy, those receiving antiretroviral therapy, and those who were adherent during the previous 1 and 3 months.
Table 1 summarizes participant characteristics, stratified by past 3-month adherence status (non-adherent vs. adherent), for all 65 persons on ART. Their mean age was 38.4 (SD = 8.6) and almost all (97%) received free ART through government clinics and had been on ART for a mean of 4 years (SD = 8.6). Most were men (83%), with about half identifying as gay or MSM (46%); many were married to a woman (40%), and most had completed secondary school (75%). The majority of participants (68%) screened positive for depression and 42% reported experiencing medication side effects.
Table 1.
Participant Characteristics and Correlates of ART Adherence at 3 months
| Characteristic | Totala (n = 65) | Non-Adherent (n = 31) | Adherent (n = 34) |
|---|---|---|---|
| * Age (mean +/− SD) | 38.4 +/− 8.6 | 35.8 +/− 7 | 40.8 +/− 9.2 |
| Years on ART (mean ± SD) | 4 +/− 2.5 | 3.5 +/− 2.2 | 4.4 +/− 2.7 |
| Received Government-Funded ART | 63 (96.9%) | 30 (96.8%) | |
| Gender | |||
| Male | 54 (83.1%) | 27 (87.1%) | 27 (79.4%) |
| Transgender | 11 (16.9%) | 4 (12.9%) | 7 (20.6%) |
| Sexual Identity | |||
| Gay/MSM | 30 (46.2%) | 14 (45.2%) | 16 (27.1%) |
| Bisexual | 9 (13.9%) | 6 (19.4%) | 3 (8.8%) |
| Kothi | 9 (13.8%) | 3 (9.7%) | 6 (17.7%) |
| Panthi | 2 (3.1%) | 1 (3.2%) | 1 (2.9%) |
| Double Decker | 4 (6.2%) | 3 (9.7%) | 1 (2.9%) |
| Hijra | 11 (16.9%) | 4 (12.9%) | 7 (20.6%) |
| Married to a woman | 25 (40.3%) | 12 (38.7%) | 13 (38.2%) |
| Highest School Level Completed | |||
| Primary | 15 (25%) | 8 (25.8%) | 7 (20.6%) |
| Secondary or greater | 45 (75%) | 19 (61.3%) | 26 (76.5%) |
| Monthly Income (mean +/− SD) | Rs. 9,041 +/−5,842 | Rs. 8,216 +/− 5,603 | Rs. 9,794 +/− 6035 |
| Side-Effects | 27 (42.2%) | 12 (38.7%) | 15 (44.1%) |
| * Medication Beliefs (mean ± SD)b | 12.3 +/− 2.8 | 13.1 +/− 2.6 | 11.5 +/− 2.7 |
| Depression (CES-D 10 score mean ± SD)c | 12.9 +/− 5.2 | 13 +/− 4.9 | 12.9 +/− 5.6 |
| Internalized Homophobia (mean ± SD)d | 12.5 +/− 3.1 | 12.7 +/− 3.3 | 12.4 +/− 3.1 |
| Self-Efficacy (mean ± SD)e | 97 +/− 15.8 | 96.7 +/− 17.7 | 97.3 +/− 14.8 |
Note: ART = antiretroviral therapy; MSM = men who have sex with men; SD = standard deviation; Rs. = rupees.
p < 0.05 for difference between non-adherent and adherent groups
Not all categories add up to 100% due to missing data
Perceived medications beliefs using Beliefs About Medicines Questionnaire
Report of depression using Center for Epidemiological Studies Depression (CESD) scale
Report of internalized stigma using Internalized Homophobia Scale, modified to have transgender inclusive language
Report of self-efficacy using HIV Treatment Adherence Self-Efficacy Scale
Ranges: Medication beliefs (0–36)/CESD-10 (0–30)/Internalized homophobia (5–25)/Self-Efficacy (0–110)
Factors Associated with Adherence
In bivariate analyses, non-adherence at 3 months was associated only with younger age (35.8 ± 7 years vs. 40.8 ± 9.2 years, p = 0.015) and having more negative beliefs about ART medications (Beliefs About Medicines Questionnaire = 13.1 ± 2.6 vs. 11.5 ± 2.7, p = 0.017). Results were similar when the analyses were repeated for adherence in the previous 1 month (data not shown).
Reasons for Non-Adherence
Of participants missing any doses (n = 31) in the previous 1 month or 3 months, 10/31 (32.2%) reported skipping doses due to drinking alcohol (i.e., not wanting to mix medications with alcohol), 9/31 (29%) indicated simply forgetting, 22.6% (7/31) indicated running out of medications before being able to obtain refills, 4/31 (12.9%) reported feeling healthy enough to skip doses, and 2/31 (3.1%) missed doses due to not having enough money.
Discussion
In this survey of MSM and TGW living with HIV infection and accessing support services at a CBO in Mumbai, India, we found relatively low rates of ART use and adherence by self-report. Overall, 28% were eligible for ART through government ART centers and only 22% were using ART at the time of the study. However, of those eligible for ART based on CD4+T cell count or World Health Organization stage, a high percentage (76%) were taking ART, but non-adherence was very common, with only 68% and 52% reporting adherence in the previous 1 and 3 months, respectively.
Another recent study of MSM in 12 Indian cities found ART uptake, among those who were eligible, to be approximately 16%, which was substantially lower than the 76% we observed (Mehta et al., 2015). Although this variation may likely be due to sampling differences, it may also be partly attributable to participants in our study, who were recruited through an HIV support program at a CBO for MSM/TGW that facilitated ART uptake by eligible clients.
Despite relatively high ART uptake by those who were eligible, we also noted potentially modifiable factors that could have impacted adherence. These included alcohol use, feeling healthy (i.e., decreased risk perception), and having negative attitudes toward ART medications, findings similar to those in other populations in India (Venkatesh et al., 2010). These findings support the need for routine screening for alcohol and substance use and dependence, and to associate counseling and treatment with these problems to help improve ART adherence and achieve better health outcomes. We also found that younger age was associated with non-adherence, consistent with other studies of adherence in India and globally (Gari et al., 2013). Possible reasons for non-adherence among younger individuals included not having experienced negative health consequences from HIV, not being used to taking medications regularly for any reason, having privacy concerns, having less of a regular day-to-day routine, or having other priorities, issues that are all potentially amenable to counseling.
This was an exploratory study and there were important limitations. First, we used self-reported adherence data. Second, the small sample size did not allow for multivariate analysis, and may potentially have masked correlates of adherence and differences between MSM and TGW. Lastly, our participants were from a pool of individuals accessing services at a lesbian, gay, bisexual, transgender, and questioning CBO and the sample may not have been representative of the larger population of MSM and TGW living with HIV and using ART in Mumbai. Given that participants in our study were a part of a support network for MSM and TGW living with HIV, rates of ART use and adherence may have been higher in our sample than in those not connected in this way.
Conclusion
This is one of the first studies to examine ART uptake and adherence by Indian MSM and TGW. While more in-depth studies are warranted to better understand factors impacting the HIV care continuum, evidence-based scalable interventions are urgently needed to optimize health outcomes for MSM and TGW living with HIV in India.
Acknowledgments
We would like to acknowledge participants for their time, Sebastian Kohn, MS, and Jeremy Fagan, PhD, for their support during the editing process and manuscript preparation, Santosh Karambe and Harish Kambli for their assistance in data collection. This study was supported in part by the Global Health Scholarship from the Rosenbluth Fund, Einstein’s Global Health Center, and NIH K23-MH102118 (PI: Viraj Patel, MD, MPH).
Footnotes
Disclosures
The authors report no real or perceived vested interests that relate to this article that could be construed as a conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Christopher Piña, Medical resident, Primary Care/Social Internal Medicine residency program, Albert Einstein College of Medicine/Montefiore Health System, Bronx, New York, USA.
Alpana Dange, Research Director, The Humsafar Trust, Mumbai, India.
Shruta Rawat, Research Manager, The Humsafar Trust, Mumbai, India.
Urmi Jadhav, Transgender point of contact and a research assistant, The Humsafar Trust, Mumbai, India.
Julia H. Arnsten, Chief, Division of General Internal Medicine and Professor of Medicine, Psychiatry & Behavioral Sciences, and Epidemiology & Population Health, Albert Einstein College of Medicine/Montefiore Health System, Bronx, New York, USA.
Rosy Chhabra, Research Associate Professor, Department of Pediatrics and faculty researcher, Albert Einstein College of Medicine/Montefiore Health System, Bronx, New York, USA.
Viraj V. Patel, Assistant Professor of Medicine and clinician-investigator, Division of General Internal Medicine, and faculty, Primary Care/Social Internal Medicine residency program, Albert Einstein College of Medicine/Montefiore Health System, Bronx, New York, USA.
References
- Asthana S, Oostvogels R. The social construction of male ‘homosexuality’ in India: Implications for HIV transmission and prevention. Social Science & Medicine. 2001;52(5):707–721. doi: 10.1016/S0277-9536(00)00167-2. [DOI] [PubMed] [Google Scholar]
- AVERT. HIV and AIDS in India. 2016 Retrieved from http://www.avert.org/professionals/hiv-around-world/asia-pacific/india.
- Ekstrand ML, Chandy S, Heylen E, Steward W, Singh G. Developing useful HAART adherence measures for India: The Prerana Study. Journal of Acquired Immune Deficiency Syndromes. 2010;53(3):415–416. doi: 10.1097/QAI.0b013e3181ba3e4e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gari S, Doig-Acuña C, Smail T, Malungo JRS, Martin-Hilber A, Merten S. Access to HIV/AIDS care: A systematic review of socio-cultural determinants in low and high income countries. BMC Health Services Research. 2013;13:198–198. doi: 10.1186/1472-6963-13-198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joint United Nations Programme on HIV/AIDS. Global report: UNAIDS report on the global AIDS epidemic 2013. 2013 Retrieved from http://www.unaids.org/sites/default/files/media_asset/UNAIDS_Global_Report_2013_en_1.pdf.
- Horne R, Weinman J, Hankins M. The beliefs about medicines questionnaire: The development and evaluation of a new method for assessing the cognitive representation of medication. Psychology & Health. 1999;14(1):1–24. doi: 10.1080/08870449908407311. [DOI] [Google Scholar]
- Joglekar N, Paranjape R, Jain R, Rahane G, Potdar R, Reddy KS, Sahay S. Barriers to ART adherence and follow ups among patients attending ART centres in Maharashtra, India. Indian Journal of Medical Research. 2011;134(6):954–959. doi: 10.4103/0971-5916.92642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MO, Neilands TB, Dilworth S, Morin SF, Remien RH, Chesney MA. The role of self-efficacy in HIV treatment adherence: Validation of the HIV treatment adherence self-efficacy scale (HIV-ASES) Journal of Behavioral Medicine. 2007;30(5):359–370. doi: 10.1007/s10865-007-9118-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan S, Khan OA. The trouble with MSM. American Journal of Public Health. 2006;96(5):765–766. doi: 10.2105/AJPH.2005.084665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logie CH, Newman PA, Chakrapani V, Shunmugam M. Adapting the minority stress model: Associations between gender non-conformity stigma, HIV-related stigma and depression among men who have sex with men in South India. Social Science & Medicine. 2012;74(8):1261–1268. doi: 10.1016/j.socscimed.2012.01.008. [DOI] [PubMed] [Google Scholar]
- Machtinger EL, Bangsberg DR. Adherence to HIV antiretroviral therapy. 2005 Retrieved from http://hivinsite.ucsf.edu/InSite?page=kb-03-02-09.
- Mehta SH, Lucas GM, Solomon S, Srikrishnan AK, McFall AM, Dhingra N, … Solomon SS. HIV care continuum among men who have sex with men and persons who inject drugs in India: Barriers to successful engagement. Clinical Infectious Diseases. 2015;61(11):1732–1741. doi: 10.1093/cid/civ669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH. Minority stress and mental health in gay men. Journal of Health and Social Behavior. 1995;36(1):38–56. [PubMed] [Google Scholar]
- Mills EJ, Nachega JB, Bangsberg DR, Singh S, Rachlis B, Wu P, … Cooper C. Adherence to HAART: A systematic review of developed and developing nation patient-reported barriers and facilitators. PLoS Medicine. 2006;3(11):e438. doi: 10.1371/journal.pmed.0030438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills EJ, Nachega JB, Buchan I, Orbinski J, Attaran A, Singh S, … Bangsberg DR. Adherence to antiretroviral therapy in sub-Saharan Africa and North America: A meta-analysis. Journal of the American Medical Association. 2006;296(6):679–690. doi: 10.1001/jama.296.6.679. [DOI] [PubMed] [Google Scholar]
- Ministry of Health and Family Welfare Government of India. Annual Report 2012–13-National AIDS Control Organisation. 2013a Retrieved from http://www.naco.org/resources/naco-annual-report-2012-2013.
- Ministry of Health and Family Welfare Government of India. Antiretroviral therapy guidelines for HIV-infected adults and adolescents. 2013b Retrieved from http://www.hivpolicywatch.org/duremaps/data/guidelines/IndiaAdultARTguidelines2013.pdf.
- Patel VV, Mayer KH, Makadon HJ. Men who have sex with men in India: A diverse population in need of medical attention. Indian Journal of Medical Research. 2012;136(4):563–570. [PMC free article] [PubMed] [Google Scholar]
- Rodger AJ, Cambiano V, Bruun T, Vernazza P, Collins S, van Lunzen J, … Lundgren J. Sexual activity without condoms and risk of HIV transmission in serodifferent couples when the HIV-positive partner is using suppressive antiretroviral therapy. Journal of the American Medical Association. 2016;316(2):171–181. doi: 10.1001/jama.2016.5148. [DOI] [PubMed] [Google Scholar]
- Shinde S, Setia M, Row-Kavi A, Anand V, Jerajani H. Male sex workers: Are we ignoring a risk group in Mumbai, India? Indian Journal of Dermatology, Venereology, and Leprology. 2009;75(1):41–46. doi: 10.4103/0378-6323.45219. [DOI] [PubMed] [Google Scholar]
- Steward WT, Herek GM, Ramakrishna J, Bharat S, Chandy S, Wrubel J, Ekstrand ML. HIV-related stigma: Adapting a theoretical framework for use in India. Social Science & Medicine. 2008;67(8):1225–1235. doi: 10.1016/j.socscimed.2008.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas BE, Rehman F, Suryanarayanan D, Josephine K, Dilip M, Dorairaj VS, Swaminathan S. How stigmatizing is stigma in the life of people living with HIV: A study on HIV positive individuals from Chennai, South India. AIDS Care. 2005;17(7):795–801. doi: 10.1080/09540120500099936. [DOI] [PubMed] [Google Scholar]
- Venkatesh KK, Srikrishnan AK, Mayer KH, Kumarasamy N, Raminani S, Thamburaj E, … Safren SA. Predictors of nonadherence to highly active antiretroviral therapy among HIV-infected south Indians in clinical care: Implications for developing adherence interventions in resource-limited settings. AIDS Patient Care and STDs. 2010;24(12):795–803. doi: 10.1089/apc.2010.0153. [DOI] [PMC free article] [PubMed] [Google Scholar]