Abstract
The purpose of our study was to explore the social determinants of health for Black mothers living with HIV in the Southeastern region of the United States. In this exploratory study, we used qualitative methods of in-depth interviewing and photo elicitation at 3 time points to provide a comprehensive examination of the meaning that the constructs held for participants (n = 18). The social determinants of health, identified primarily as positive health determinants by the participants, included social support, religion, animal companions, and the physical environment. The social determinants of health identified as mixed determinants, having both positive and negative qualities, were transportation and housing. Each of these social determinants is presented with definitions and exemplars. Additionally, aspects of each determinant of health that may be meaningfully addressed through process and structural level interventions are explored.
Keywords: African American/Black, HIV, mothers, photo elicitation, social determinants of health, strength based
The magnitude of the disease burden and the disparity in health outcomes for African American/Black (hereafter referred to as Black) mothers living with HIV in the southeastern United States are of significant concern across racial (Centers for Disease Control and Prevention [CDC], 2017a), gender (CDC, 2017b), and socioeconomic groups (DiNenno, Oster, Sionean, Denning, & Lansky, 2012; U.S. Census Bureau, 2012). Women, many of whom are of childbearing age (15–44 years), now represent approximately one quarter of all people living with HIV (PLWH) in the United States, and 61% of the total number of women living with diagnosed HIV are Black women (CDC, 2017b). The racial and gender health gaps in the HIV epidemic are closely linked to racial and gender wealth gaps in the United States (Robinson & Moodie-Mills, 2012). Women of color are overrepresented among people living in poverty (U.S. Census Bureau, 2012), and socioeconomic status is not only a significant precipitating factor for HIV infection (DiNenno et al., 2012), but also a major determinant of higher morbidity of non-White women in the Southeastern region of the United States (Meditz et al., 2011).
Focused attention on the needs of mothers living with HIV, in addition to elimination of maternal-to-child HIV transmission, has only recently gained momentum on the global stage (Joint United Nations Programme on HIV/AIDS [UNAIDS], 2011). Prior to the release of the 2011 Global Plan Towards the Elimination of New HIV Infections among Children by 2015 and Keeping their Mothers Alive (UNAIDS, 2011), the interventions specifically aimed at improving health outcomes for mothers living with HIV and reaching beyond just the prevention of maternal and child transmission were few. Indeed, such interventions did not appear in the literature until 2000 (Jirapaet, 2000), almost 20 years after HIV was first described in the literature. In addition, none of the interventions for mothers living with HIV to date have been based on a clear understanding of their social determinants of health.
Social determinants of health encompass the health care systems and the conditions in which people are born, grow up, live, work, and age, as well as how the hierarchies of race, gender, and class jointly create meaning and interact to produce health inequities (Commission on the Social Determinants of Health, 2008; Hankivsky, 2012). The health experiences of Black mothers living with HIV are fashioned by individual strengths and vulnerabilities as well as a complex configuration of social determinants and inequalities such as race and gender inequality (Caiola, Docherty, Relf, & Barroso, 2014); however, most of the interventions aimed at PLWH have focused on individual risk behaviors (Adimora & Auerbach, 2010). Understanding the dynamic social environment and contextual social determinants of health for Black mothers living with HIV is an essential shift away from historical approaches of individual risk behavior interventions if we are to address disparate health outcomes and inform future prevention and treatment efforts (Adimora & Auerbach, 2010; Bailey et al., 2017; Commission on the Social Determinants of Health, 2008; Robinson & Moodie-Mills, 2012).
To date, health researchers have not clearly delineated the specific social determinants of health as understood by this population of women. The purpose of our study, therefore, was to explore the social determinants of health for Black mothers living with HIV in the southeastern region of the United States. To explore these social constructs, we developed a conceptual model of social determinants of health specific to Black mothers living with HIV (Caiola et al., 2014) and used qualitative methods of in-depth interviewing and photo elicitation to provide a comprehensive examination of the meaning of the constructs for participants (Harper, 2002). These methods engaged participants as they described their own strengths and vulnerabilities in everyday life and illuminated the implications of social and economic contexts for health.
Methods
We used a qualitative descriptive design employing in-depth interviews and photo elicitation across an 8-week period. Qualitative description is a research method that can have varying approaches to sampling, data collection, and data analysis, but does require the researcher to produce interpretive products closer to the data as it is given by participants (Sandelowski, 2010). We felt remaining data-near was an ideal approach when using a visual method such as photo elicitation. Photo elicitation is a qualitative interviewing technique in which the researcher uses photographs during the research interview to elicit information from participants (Bugos et al., 2014; Harper, 2002). Photo elicitation is an essential element of the community-based participatory action research method called Photovoice, which is grounded in feminist and critical theory (Wang & Burris, 1997). The use of Photovoice and photo eliciation with PLWH is steadily growing and has been shown to be effective in detailing the realities of living with HIV, stimulating community dialogue, and successfully maintaining participant confidentiality (Mignone et al., 2015; Rhodes, Hergenrather, Wilkin, & Jolly, 2008; Teti, French, Bonney, & Lightfoot, 2015; Teti, Murray, Johnson, & Binson, 2012; Teti, Pichon, Kabel, Farnan, & Binson, 2013). Photo elicitation and Photovoice both offer elements of participant control and engagement in the research process, create an adjunct to verbal methods of data elicitation, and allow participants to be active members in the research process (Guillemin & Drew, 2010; Harper, 2002; Wang, 1999).
Full details of the study methods and procedures, including sampling and efforts to assure the trustworthiness of the results, can be found elsewhere (Caiola, Barroso, & Docherty, 2017). This article presents those data that relate to the photographs and photo elicitation method only. Data collection occurred at three time points, and digital audio recordings were made of all interviews. Each participant signed a voluntary consent and our university institutional review board for human subject research reviewed and approved all phases of this study.
Each interview served a different purpose: (a) Baseline - building rapport with participants, obtaining basic demographic data (e.g., gender, age, sexual orientation), and introducing the goals and use of photo elicitation; (b) Week 6 - examining the content of the photographs; and (c) Week 8 - further exploring the various social and economic complexities of the mothers’ lives. Each successive interview added to the depth of the knowledge gained by interacting with the participants and to the trustworthiness of the analysis of data collected over time. During the first interview, we asked broad, open-ended questions regarding the women’s lives as mothers to build rapport and encourage participants to use a narrative storytelling style. We also gave each participant a 27-exposure disposable camera, discussed ethical and technical issues related to using the camera, and asked her to take photos she believed best represented the social and economic complexities affecting her health. Participants were instructed during the consent process to avoid taking pictures of any identifiable persons. If the participants wished to identify certain people in their lives as health determinants, they were encouraged to take photographs of objects such as toys or clothing representing those people.
The overall goals of the photo elicitation method (“taking pictures”) were described to participants as follows: (a) to picture or capture the social and economic experience of your daily life that negatively impact your health or ability to care for your HIV, and (b) to picture or capture the social and economic experiences of your daily life that positively impact your health or ability to care for your HIV. The initial interview also included a discussion about the social determinants of health in lay terms, including examples, and a brainstorming activity to help participants identify potential images of strengths and vulnerabilities related to their health that they might wish to capture (Wang, 1999). Participants were given time between the first two interviews (6 weeks) to take photographs; the disposable camera was then mailed back to the first author via U.S. mail using a self-addressed stamped envelope. The photographs were developed under the first author’s name rather than the participant’s name and then used during the second interview to stimulate dialogue regarding how these factors affected their health-related experiences (Wang, 1999). Each of the photographs was identified by the participant’s unique identifying number and a photograph number.
Data Analysis
We performed descriptive statistics to detail participant demographic characteristics, and we used content analysis to explore their descriptions of the photographs. Digital recordings of the interviews were transcribed verbatim by a professional transcriptionist, proofed for accuracy by the first author, and kept electronically on a secure computer server. Copies of the digital images from a CD-ROM provided by the photo processor were transferred to the same secure computer server. We began the analysis by importing all photographic and associated text data into Atlas.ti (2015), a qualitative data analysis software program that helps researchers organize and analyze non-numerical data, including digital photographs. We read each transcribed interview in its entirety to get a sense of its essential features, noting specific references to photographs, and wrote a brief abstract of the distinctive elements (Sandelowski, 1995). We then used descriptive coding to help assess participant perceptions of the social determinants of health as they identified them in each photograph (Saldana, 2013). Descriptive coding is an inductive form of coding in which the code was derived from the data itself and the topic about which the participant was talking or writing (Saldana, 2013). The rationale for using descriptive coding was that some of the data, particularly those data elicited from participant photographs, may not be explained or easily coded by the conceptual framework (Caiola et al., 2014) and we wanted to capture any novel determinants of health that the conceptual framework did not predict. Once descriptive codes from the first cycle of coding were complete, we reanalyzed the data and developed larger categories of data using pattern coding (Saldana, 2013). Pattern coding is a second level of coding used to organize and group initial codes that are similar or share some common characteristics together so that major themes from the data can be developed (Saldana, 2013).
Results
We completed a total of 48 interviews with the 18 participants. Per the participants’ preferences, 15 of the participant interviews occurred in a private room at the university campus and the remaining 33 occurred at the participants’ homes or a shelter where the participant was residing. Each participant identified herself as being African American/Black, female, living with HIV, and living below the federally designated poverty level, or qualifying for public assistance or Medicaid. Other demographic characteristics are noted in Table 1.
Table 1.
Participant Demographics (n = 18)
| Characteristic | Mean | Range |
|---|---|---|
| Age (years) | 41.5 | 25–57 |
| Years living with HIV | 13 | 5–32 |
| Education attainment (years) | 12.56 | 11–16 |
| Number of Dependent Children | 1.6 | 1–5 |
Two of the participants were lost to follow-up after the first time point; therefore, we were only able to complete the second interview utilizing the photo elicitation method with 16 of the 18 participants. The total number of usable photographs submitted by the 16 participants was 184 and ranged from 4 to 25 photographs per participant. Photographs were considered usable if (a) they did not contain images of identifiable persons, (b) the photograph quality was sufficient to distinguish the photograph content when developed, and (c) the photographs were taken by the participant themselves. Five of the participants reported that their children had inadvertently accessed their disposable cameras and taken at least some of their photographs. The photographs that were not usable were shredded per the study protocol.
At a 3:1 ratio, the participants chose to photograph positive health determinants (154) as opposed to negative health determinants (49), identifying a total of 203 health determinants. The total number of determinants identified was greater than the actual number of photographs (184) taken because some of the photographs were coded as more than a single determinant per participant descriptions. Not all photographs depicted determinants of health that were categorized as social determinants. For example, participants depicted several individual behavior determinants of health such as eating habits and physical exercise in their photographs. Using an iterative and continuous process, we identified six broad themes of social determinants of health. The social determinants of health identified primarily as positive health determinants by the participants included social support, religion, animal companions, and the physical environment. The social determinants of health identified as mixed determinants, having both positive and negative qualities, were transportation and housing. Each of these social determinants is presented with definitions and exemplars below.
Social Support
Participants photographed people or objects representing the people in their social networks that they felt cared for them and/or offered assistance when needed. Several of the photographs of people had to be shredded because the subject could be identified, but the descriptions of these photographs were still analyzed. The photographs of objects representing people were also retained and discussed.
Participants primarily described how their family members and significant others offered emotional support and encouraged them to care for themselves and their health. One participant took a photograph of her husband’s work shirt (Figure 1) and stated:
It’s a picture of my husband’s work shirt…and it symbolizes him, you know, just being a strong individual in my life and giving me the support that I need…yeah because he’s- he encouraged me a lot to keep up my health.
Figure 1.

Social support photograph
The support person in one participant’s life was also portrayed as a role model for health. She took a photograph of her uncle who lived with her and stated:
I see someone positive, always been a positive role model. Um…I don’t care he does dialysis, 3 days a week. And I, if I didn’t know him, I would have never tell it, he never complains…You know, he lifts me up a whole lot.
Support people in the lives of participants offered encouragement, provided emotional support, or served as role models; they were portrayed as helping the participants cope with the HIV diagnosis and positively impacting their health.
Religiosity
The participants photographed objects that represented their spiritual beliefs in a higher power and described the beliefs as positively impacting their health. In this sample, the participants commonly described their affiliation with Black churches (churches serving primarily Black people) and photographed objects associated with Christian religious practices, including Bibles, Christian churches, a daily devotion book, prayers imprinted on a plaque and a pillow, a church piano, a guardian angel figurine, and a church bulletin. They described how their spiritual and religious beliefs positively affected their health in several ways. They explained that their beliefs offered guidance, additional social support, and opportunities to serve others.
Several participants described the ways in which their religious beliefs gave them guidance in coping with HIV and life in general. They used words such as “balance,” “focus,” “enlightenment,” and “encouragement” to describe the impact of the guidance provided by religious faith. For example, one participant explained her photograph (Figure 2) of a guardian angel figurine. She said that she believed her guardian angel was her grandmother, and stated that her guardian angel guided her in the following way: “Um, [a guardian angel] gives you guidance and, you know, understanding, pretty much. You know - even though you got this disease, don’t let it overcome you.”
Figure 2.

Religiosity photograph 1
Other participants described their religious practices as the means for accessing additional social support, which they said positively impacted their health. One participant photographed a church bulletin and reported that her church offered her a welcoming, nonjudgmental community in which to participate. She stated, “…they don’t judge you. They don’t look at the color of your skin, your race, or I mean nothing and your health - sick or bad - they welcome. They welcome you [with] open hands.” Another participant took a picture of her Bible cover and stated, “I’ve been in the church since I was a baby (laughs). You know I’ve been - it’s been my whole life through - church. Church - I think church - my church family and God has kept me alive.”
Affiliation with a religious community was also described as offering participants the opportunity to serve others. For example, one participant took a picture of her church (Figure 3) and listed the many church activities she participated in, such as tutoring children and providing food for others. She explained that these ministries and serving others positively impacted her health in the following way:
… so, my church is my life now. So that’s a good strength…because I don’t focus on my illness. Um, I don’t have any… what do they call ‘em? Side effects from the medication so I don’t really think about it.
Figure 3.

Religiosity photograph 2
Participants considered their religious and spiritual practices as having a positive effect on their health. Guidance, additional social support, and opportunities for service to others were all aspects of why participants deemed these practices as positive social determinants of health.
Animal Companions
In addition to their social networks, many of the participants photographed and described the relationships and support they received from animal companions. Almost one third of the participants (5 of 16) chose to photograph one or more pets. One participant was saddened and tearful when she first saw the photograph she had taken of one of her dogs because she had recently had to euthanize the dog (Figure 4). She described their companionship and the positive impact her pet had on her health and her life by saying, “…they don’t talk, but if something’s wrong or…uh…mainly when something’s wrong, they’ll come up to you, they make you play. Yeah [crying].” Another participant took photographs of her pets and described how her dog positively impacted her health:
You can talk to ‘em; they don’t talk back to you…they are very smart…I don’t run much, but I leave ‘em at the house and they’ll chase me. You know what I am saying? Working on my legs and stuff and keeping the weight off of him. He’ll run back and forth, all around the house. He likes to play. And I think it is - I think that with my health it’s just – it’s, um, keeping me less stressed.
Figure 4.
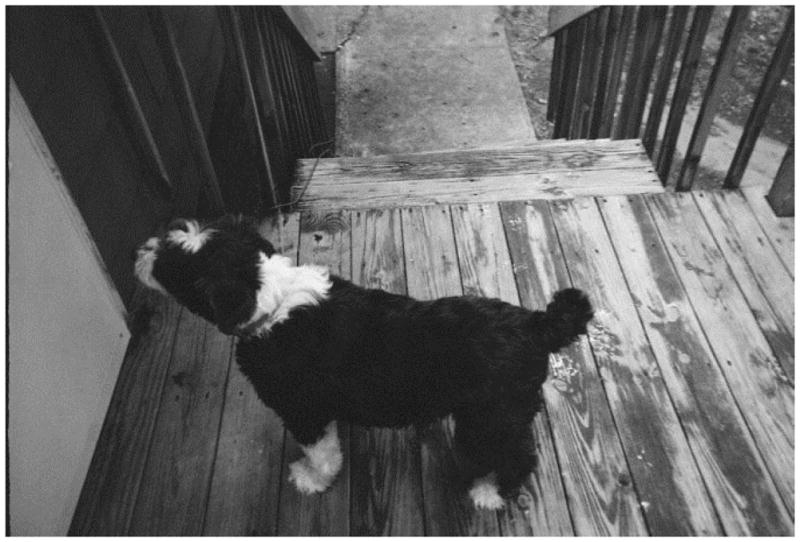
Animal companions photograph
Participants described their pets as members of their family and talked about the joy they brought, how they decreased stress levels, the opportunities they provided for getting physical exercise.
Physical Environment
The participants photographed several outdoor scenes or paintings/prints of outdoor scenes and described the numerous ways that the physical environment and nature positively affected their health. The scenes included wooded areas, parks, waterfalls, walking trails, and participants’ backyards. They explained that their physical environments and nature offered them opportunities for relaxation, reflection, exercise, and recreation, which all had positive health benefits.
Many participants described the ways in which their surrounding physical environments provided a chance to relax and reflect on their life circumstances. They used descriptions such as “getaway oasis,” “peaceful,” “cleansing,” and “relaxing” to describe these areas and the positive effects on their mental and physical health. Participants also reported that the natural environment prompted them to reflect on their life circumstances and noted that living with HIV had heightened their appreciation of the outdoors (Figure 5). For example, one participant explained:
Yeah, it was just nature. Something I can still enjoy…Well, I kind of started appreciating it more after knowing, you know, I was diagnosed. I kind of appreciate a lot of things more and nature was one of - flowers, trees, the sky.
Figure 5.
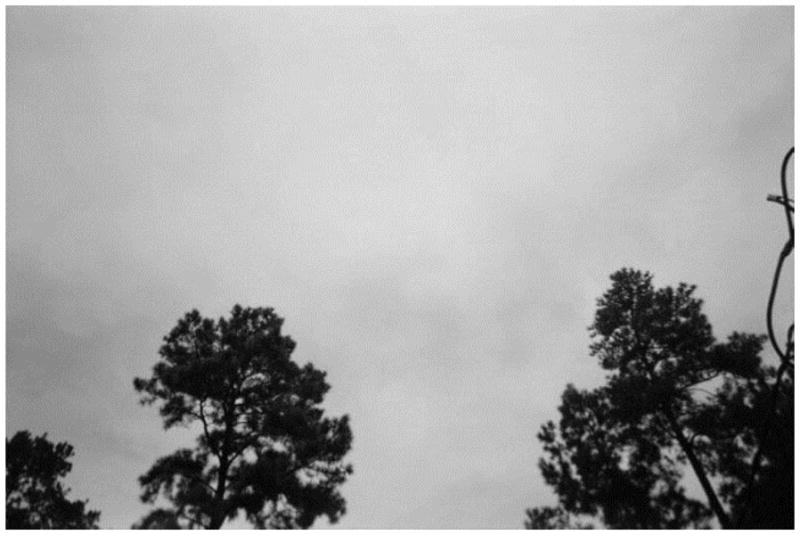
Physical environment photograph
In addition to the mental and emotional benefits of their physical environments, participants also conveyed its importance for physical health. They photographed the walking trails and parks where they enjoyed recreation and exercise. Relaxation, reflection, exercise, and recreation were all positive health benefits identified by the participants as they photographed and described their physical environments.
Transportation
The modes of transportation used by participants varied (private vehicles vs. public transportation such as buses and medical transport van services) along with the health benefits and deficits they associated with each; this suggested that transportation was an important social determinant of health. Some participants described the positive aspects of their private vehicles such as independence and reliability in accessing health care services, while other participants described the financial and mental stress of maintaining their vehicles or using public transportation. For example, one participant had acquired a car while participating in the study (Figure 6) and she excitedly described the benefits of her new mode of transportation and no longer having to take medical transportation:
Some days, they didn’t even pick me up, you know, even though I called in and I had the appointment so some days they didn’t even show up because they was too booked, too busy, and they were just way behind. So, I just missed that appointment and had to reschedule.
Figure 6.
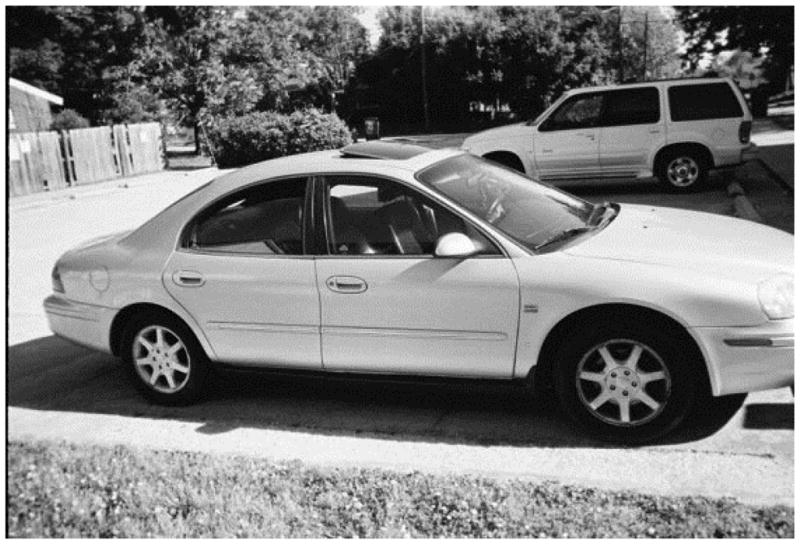
Transportation photograph 1
Another participant also identified her car as a social determinant of health, but focused on the negative aspects. She discussed the problems with attempting to maintain a private vehicle on a limited income and the tradeoffs of living in a place where one needs a private vehicle for transportation versus public transportation:
That’s my mode of transportation. And that’s important to me because that gets me to my appointments, it gets me to pick up my kids, it gets me to where I need to go. Um, it’s also a concern. Because you have to keep it up. Keep up the maintenance. And keep it up and that’s not easy to do. Um, so you know, and being on a fixed income…
Public transportation was generally described by participants as unreliable, inaccessible, or inconvenient; in other words, it was viewed as a negative social determinant of health. One participant described her experience using the bus system (Figure 7) while she was recovering from major hip surgery and using a walker. She stated:
So…the bus system in [city] is crazy… you have to all go to this one place which is downtown then get another bus and it’s spread out. And if you have to go somewhere else there is no connection. You have to come back downtown and then go again… it’s time consuming.
Figure 7.
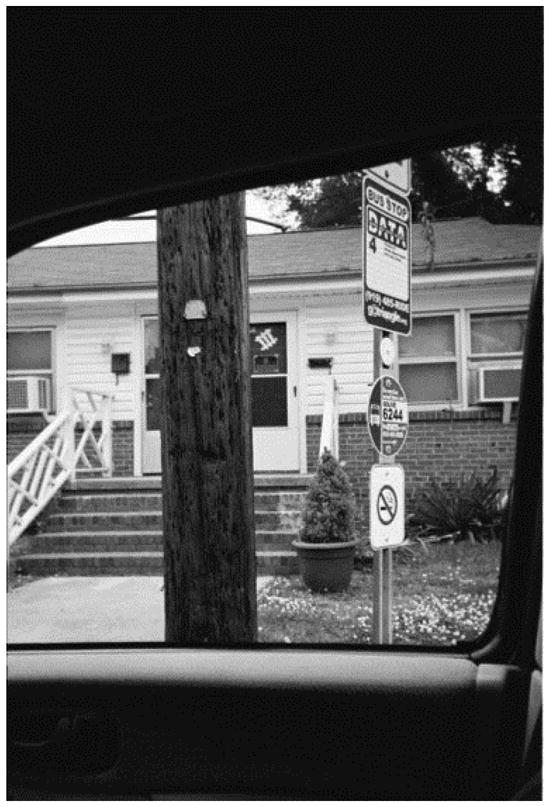
Transportation photograph 2
While private transportation was the mode preferred by participants over public transportation, it was also financially inaccessible to many. The participants identified both positive and negative aspects of the various forms of transportation and the associated health implications, but reliability, accessibility, and affordability clearly emerged as the most important qualities of any of the modes of transportation noted.
Housing
Of all the social determinants of health, housing was the most tenuous as described by participants in the photo elicitation data. One participant reported a previously unsafe housing situation, two participants reported previous homelessness, one participant and her children were residing in a homeless shelter while she was enrolled in the study, and one participant was lost to follow-up due to homelessness. The participant lost to follow-up due to homelessness was contacted via her cellular telephone to schedule her second interview but she reported she was no longer in a stable living situation, repeatedly cancelled, or failed to show up for scheduled follow-up interviews, and ultimately, did not complete the study.
Participants described their housing situations as extremely important in maintaining their health status, but several of the women had experienced unstable housing situations. One participant reported extreme gratitude for the assistance she received in acquiring an apartment for herself and her family through a state voucher program (Figure 8). When asked how her current housing situation impacted her health, she seemed to be laughing at the absurdity of the question when she responded:
[laughs] Um…that impacts a great deal. Because if I was homeless, um, of course, wouldn’t have pretty much access to water, wouldn’t be able to feed myself, to cook in my own kitchen rather… I can’t say I’ve never been homeless because I know that part of the fence … so you know I’m just really grateful.
Figure 8.
Housing photograph
A stable housing situation was viewed as a positive social determinant of health by the participants, but many clearly provided examples of its tenuous nature for those living in poverty.
Discussion
The health experiences of Black mothers living with HIV in our study operated at the intersection of multiple social determinants. We analyzed data derived from in-depth interviews, which included photo elicitation interviewing methods, and sought to explain how social determinants influenced health experiences of Black mothers living with HIV in the southeastern region of the United States. Using the participatory visual methods described, six primary social determinants of health were identified by the participants: social support, religion, animal companions, the physical environment, transportation, and housing. Each of these added to the literature about social determinants of health relevant to Black mothers living with HIV and identified aspects of the problem that may be addressed through process and structural level interventions in a meaningful way.
Social Determinants of Health
The social determinants of health identified by participants in our study individually offered opportunities to either capitalize on the strengths of Black mothers living with HIV to enhance their health or intervene where specific vulnerabilities were clearly at work. To be sure, some of the social determinants identified by the participants also functioned as indicators of broader social determinants already identified in the literature; for example, housing and transportation stability function as key indicators of income inequality or poverty in this population. Nonetheless, our findings demonstrated that, when the experiential aspects of daily life with HIV are considered, a broader and more complete conceptual approach is likely to emerge.
Social support
In the era of antiretroviral therapy, HIV has shifted from being an acute, fatal disease to a chronic illness in the United States. Concomitantly, the importance of social support for PLWH has become increasingly recognized as a critical factor as they live longer and healthier lives (Mignone et al., 2015). Higher levels of perceived social support have been associated with longer HIV survival rates for parents living with HIV (Lee & Rotheram-Borus, 2001), and having a diverse social network has also been associated with longevity for those living with chronic illnesses (Cohen & Janicki-Deverts, 2009). Moreover, the findings from a qualitative study of Black mothers living with HIV found that the mothers viewed their children as a significant source of social support facilitating medication adherence and positive health-seeking behaviors (Edwards, 2006), suggesting an interesting intersection between motherhood and social support.
The finding of social support as a significant positive social determinant of health for participants in our study supports this literature. Whether the support people in the lives of participants offered encouragement to perform health-seeking behaviors, provided emotional support, or acted as role models, the participants perceived them as positively impacting their health and helping them cope with the HIV diagnosis. Much of the work examining social support and health outcomes, however, is correlational, not causal, and a number of mechanisms, such as the amount of social contact and the diversity of the network with whom a person has contact, may be influencing these associations (Cohen & Janicki-Deverts, 2009). Nonetheless, the findings from our study offer additional empirical evidence of the need to further examine the association, while offering an opportunity to consider how social support may specifically function as a positive social determinant of health for Black mothers living with HIV. Structural approaches are also needed to generate healthier environments that create increased social support (Cohen & Janicki-Deverts, 2009).
Religiosity
Consistent with research on the centrality of organizational and non-organizational religiosity in the lives of Blacks people, Chatters, Taylor, Bullard, and Jackson (2009) reported higher levels of religious participation than other racial groups in the United States. Additionally, community-based partnerships can potentiate traditional health care setting interventions for HIV: the strategic plan of the CDC (2007), Heightened National Response to Address the HIV/AIDS Crisis among Blacks, urged faith-based organizations and faith leaders to collaborate with health partners to scale up HIV intervention strategies for Blacks. While not enacted and fixed at the committee level, the National Black Clergy for the Elimination of HIV/AIDS Act was introduced to Congress in both 2009 and 2011 to support Black churches with resources for HIV intervention initiatives (Civic Impulse, 2017).
Studies have demonstrated the potential effectiveness of faith-based and public health partnerships in HIV intervention initiatives (Berkely-Patton et al., 2010; Griffith, Campbell, Allen, Robinson, & Stewart, 2010). Our findings also support the centrality of religion in the lives of Black mothers living with HIV and the critical need for faith-based, public health partnerships. Participants identified their religious beliefs and associations with the Black Church as influential in their lives and the lives of their children, acting as positive social determinants of health by offering guidance, additional social support, and opportunities for service to others. Black churches have a history of mobilizing social change in their communities (Berkely-Patton et al., 2010), and faith-based, public health partnerships offer potential as an important structural approach for change in the racial disparities noted in the HIV epidemic. This will require further investment in support tools, capacity building for faith leaders, and community-based intervention research (Berkely-Patton et al., 2010).
Animal companions
Our literature search revealed only three studies that explored the potential health effects of animal companionship for PLWH and each found that animal companions had a positive effect on emotional and physical wellbeing. Kruger, Stern, Anstead, and Finley (2014) found that dog ownership increased perceived wellbeing in military veterans living with HIV by acting as a stress reliever and increasing opportunities for physical activity, companionship, and responsibility. When examining the caregiving and social networks of PLWH, Mignone et al. (2015) found that nearly half of their participants were living with pets and identified their pets as sources of strength, resiliency, and social support. Although older, the findings from the large 1991 Multicenter AIDS Cohort study showed positive mental health benefits of pet ownership for persons diagnosed with AIDS. Those participants reported less depression, particularly when they also reported fewer social support persons (Siegal, Angulo, Detels, Wesch, & Mullen, 1999).
Our finding that animal companions served as a significant positive social determinant of health supports this literature. Whether the animals offered companionship, helped to provide joy, decreased stress levels, or offered opportunities for physical exercise, the participants perceived them as positively impacting their health and helping them cope with the HIV diagnosis. This empirical evidence points to the need for further exploration of the influence of pet ownership on the health and wellbeing of PLWH. This could include research about animal-assisted intervention strategies as well. In a recent literature review assessing the empirical evidence for the broader health benefits of animal companionship on cardiovascular health, quality of life, and longevity, the researchers advocated for animal-assisted therapy in the clinical setting. They described the process-level efforts at the Mayo Clinic in Rochester, Minnesota to implement animal-assistance in therapeutic environments that were based on the consistent volume of data substantiating positive health benefits (Creagan, Bauer, Thomley, & Borg, 2015).
Physical environment
In a comprehensive literature review exploring health benefits associated with human contact with nature, the researchers found that park environments held promise for enhancing human health and wellbeing for urban-dwelling residents (Maller, Townsend, Pryor, Brown, & St. Leger, 2005). The researchers also advocated for structural interventions focused on public parks and natural areas as a broad upstream population health promotion strategy (Maller, et al., 2005). Many health benefits are associated with human contact with nature in public spaces and man-made surroundings such as parks and neighborhoods, including more opportunities for physical activity, stress reduction, coping, and enhanced recovery from illness and injury (Cohen et al., 2007; Coombes, Jones, & Hillsdon, 2010; Maller et al., 2005). As a result, national health organizations such as the Institute of Medicine, the U.S. Department of Health and Human Services, and the CDC have recommended greater investment and government planning for public spaces (CDC, 2011; Institute of Medicine and National Research Council, 2009; National Prevention Council, 2011). When examining the caregiving and social networks of PLWH, Mignone et al. (2015) found that PLWH described contact with nature and caring for plants and animals as sources of support, strength, resilience, and a welcome diversion to the hardships in their lives. Our findings also support the significance of a connection with one’s physical environment and nature in promoting health for Black mothers living with HIV. Whether interaction with the physical environment offered opportunities for relaxation, reflection, exercise, or recreation, the participants perceived these opportunities as positively impacting their health and helping them cope with HIV. However, disparities have been noted across racial/ethnic and socioeconomic status when park availability is considered, along with factors such as cleanliness and physical condition (Bruton & Floyd, 2014). Findings such as ours may help inform policy, design, and maintenance of parks located in more communities such as those where Black mothers living with HIV and in poverty are more likely to reside (Bruton & Floyd, 2014).
Transportation
In a recent qualitative meta-synthesis examining the social determinants of health for Blacks living with HIV in the rural southeast region of the United States, transportation issues were found to be a significant social determinant of health. The issues included maintenance of and fuel for personal vehicles and the affordability and accessibility of public transport (Abbott & Williams, 2015). A systematic review of the literature examining transportation barriers and access to health care found that, without exception, poorer individuals experienced greater transportation barriers to health care access leading to gaps in chronic illness management (Syed, Berber, & Sharp, 2013).
The means of transportation used by participants in our study varied (private vehicles vs. public transport such as buses and medical transport van services), and participants identified both positive and negative aspects of the various forms of transportation and their associated health implications. These findings support existing literature, and the reliability, accessibility, and affordability of transportation was noted as an important social determinant of health for Black mothers living with HIV. The findings of our study also add to the impressive body of research prompting the American Public Health Association (APHA, 2015) to craft public health and transportation equity principles meant to guide transportation policies and structural interventions that prioritize health and equity in American communities. These principles advocate for policies, interventions, and research aimed at funding community-based transportation programs that expand options for vulnerable populations, conducting health impact assessments to guide policy, involving community members in transportation planning and development, and establishing performance measures (APHA, 2015).
Housing
Results from the pioneering 2005 National Housing and HIV/AIDS Research Summit involving core research and policy experts indicated that stable housing was a foundation of both HIV prevention and treatment (National AIDS Housing Coalition, 2005). Specifically, for women living with HIV in the southeastern region of the United States, stable housing was correlated with emotional wellbeing, positive physical health indicators, risk reduction behaviors, and medication adherence (Delavega & Lennon-Dearing, 2015). The findings from our study complement the empirical evidence pointing to the importance of housing as a social determinant of health. Fortunately, a growing body of evidence has suggested that structural interventions such as strategies to meet housing needs were effective for PLWH and could impact physical health by increasing survival and promoting intact immunity (Buchanan, Kee, Sadowski, & Garcia, 2009). The National AIDS Housing Coalition has offered further guidance for policy, research, and intervention strategies aimed at broadening the concept of housing as health care for all persons, but specifically for PLWH (National AIDS Housing Coalition, 2005). Other initiatives include advocacy for the provision of affordable housing and micro-financing programs to decrease economic dependency for women living with HIV and in poverty (Adimora & Auerbach, 2010).
A Case for Strength-Based Approaches
Overall, the participants primarily chose to identify positive social determinants of health, or what they deemed to be strengths, as they cared for themselves and their HIV. This important finding supported those of other research studies using photography in which participants tended to focus on positive aspects of their lives. One possible explanation is that the prevailing social convention of photography is to depict what Guillemin and Drew (2010) described as “happy snaps” (p. 180), portraying ideal representations of our social lives. Other researchers have suggested that it may be due to the sensitivity of negatively portraying one’s life, the difficulty of capturing visual images reflecting negative emotions, and that taking such pictures was just not an enjoyable process (Zartler & Richter, 2014).
In the context of our study, it was particularly important to acknowledge any potential power differentials in the research process that may have influenced participants to represent their lives in a primarily positive light. While participatory visual methods have the potential to democratize the research process by asking participants to co-create knowledge, the methods in and of themselves do not reduce existing power imbalances of a dominant culture (Packard, 2008). Despite the intentional steps we took in the study design to limit such power differentials, it is important that we acknowledge the longstanding sociocultural context in which this study took place. We were a White research team working with Black women and we were asking the participants to openly report their vulnerabilities in a research setting that has historically been wrought with unbalanced power differentials such as racism. Thus, asking people to expose themselves and their vulnerabilities in such a context was a challenge and might be an explanation for participant emphasis on positive social determinants of health.
The power exerted by the research community, ourselves included, in categorizing specific populations as vulnerable was also important to consider. Too often we approach health research from a deficit perspective rather than examining health-promoting (positive) social determinants of health (Thygeson, 2013). A mother whose health experience was primarily one of strength and resilience, rather than vulnerability, would likely choose to represent that lived experience. As such, this particular finding offers a case for more strengths-based approaches to health research and practice. It is incumbent upon health researchers to acknowledge these strengths and make every attempt to create social environments that enhance these capacities. The International Association of Physicians in AIDS Care support this finding; they released guidelines based on a review of interventions for enhancing linkage and retention in HIV care. They recommended strength-based case management framed with a strength-based theory of cognitive therapy, a process level intervention, for all newly diagnosed patients (Okeke, Ostermann, & Theielman, 2014).
Limitations
The findings from our data may be limited by selection bias. The vast majority of the participants (n = 13) were recruited from infectious disease clinics, meaning they were at least minimally engaged in care. Women living with HIV who are engaged in care may have social determinants of health that differ from those that are not actively engaged in care (Caiola et al., 2017). Additionally, visual methods such as photo elicitation pose methodological and ethical challenges requiring researchers to employ a high degree of reflexivity and ethical practices informed by detailed knowledge of the research context and population (Gubrium, Hill, & Flicker, 2014). To our knowledge, there were no breaches in privacy, no breaches in confidentiality, and no unplanned disclosures of a participant’s HIV status to another person during the study. However, confidentiality and privacy issues specific to mothers, children, and people in their support networks did create ethical challenges in using photo elicitation as a data collection method (e.g., several participants took photographs of identifiable persons, so those printed photographs were shredded and the digital photographs deleted). We found two things particularly helpful to aid our attempts to minimize these limitations and practice reflexivity. The first was acquiring critical information needed to strategically handle the ethical and methodological challenges unique to visual methods. Such information was available through an on-going dialogue with members of the research ethics committee and the guidelines and scholarly literature available in the disciplines of anthropology, sociology, documentary studies, and, more recently, public health (Cox, et al., 2014; Gubrium et al., 2014; Harper, 2002; Wang, 1999). The second was to trial the visual methods with an initial group of five participants to receive, learn from, and incorporate feedback; anticipate pitfalls; and adapt the research protocol for the specific population and setting (Cox, et al., 2014).
Conclusions
Visual methods, such as photo elicitation, offer an innovative way to involve populations in research and explore social determinants of health while providing participants with some control in the research process and acknowledging their authority on the subject (Cox et al., 2014; Guillemin & Drew, 2010). Health experiences of Black mothers living with HIV have been driven by a complex configuration of social inequalities, structural barriers, and individual strengths and vulnerabilities. Therefore, we believe our study may help other community-based researchers who want to understand facilitators and barriers to health from the perspectives of community members. Although our project was specific to Black mothers living with HIV in the southeastern region of the United States, the methods can be tailored to identify specific social determinants within different groups, a strategy that is essential to addressing the dynamic and contextual nature of the HIV epidemic.
Key Considerations.
The health experiences of Black mothers living with HIV are driven by a complex configuration of social inequalities, structural barriers, and individual strengths and vulnerabilities.
Community-based participatory research methods, including visual methods, help providers understand the facilitators and barriers for health from the perspective of community members.
Policies and research that support strength-based approaches to care will improve interventions that enhance linkage to and retention in HIV care.
Strategies aimed at funding community-based transportation and housing programs are foundations of HIV prevention and treatment.
Acknowledgments
The authors wish to sincerely thank the women who so openly shared their stories as mothers living with HIV. The authors also wish to acknowledge and thank the other members of the first author’s dissertation committee - Ursula A. Kelly, PhD, APRN, ANP-BC, PMHNP-BC; Michael V. Relf, PhD, RN, ACNS-BC, AACRN, CNE, FAAN; and Anh N. Tran, PhD, MPH, for their contributions to the development of this research project. This work was supported by the Jonas Center for Nursing Excellence and NIH/NINR: National Research Service Award 1F31NR014628-01, PI: Courtney Caiola. Ultimately, the work was completed while the first author was supported by NIH/NINR T32NR007091, PI: Sheila Santacroce.
Footnotes
Disclosures
The authors report no real or perceived vested interests that relate to this article that could be construed as a conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Courtney Caiola, Assistant Professor, University of North Carolina at Greensboro, Greensboro, North Carolina, USA.
Julie Barroso, Professor and Chair, Department of Nursing, Medical University of South Carolina, Charleston, South Carolina, USA.
Sharron L. Docherty, Associate Professor, Duke University School of Nursing, Durham, North Carolina, USA.
References
- Abbott LS, Williams CL. Influences of social determinants of health on African Americans living with HIV in the rural southeast: A qualitative meta-synthesis. Journal of the Association of Nurses in AIDS Care. 2015;26(4):340–356. doi: 10.1016/j.jana.2015.03.004. [DOI] [PubMed] [Google Scholar]
- Adimora AA, Auerbach JD. Structural interventions for HIV prevention in the United States. Journal of Acquired Immune Deficiency Syndrome. 2010;55(Suppl 2):S132–S135. doi: 10.1097/QAI.0b013e3181fbcb38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Public Health Association. Public health and equity principles for transportation. 2015 doi: 10.2190/NS.20.3.l. Retrieved from http://www.apha.org/topics-and-issues/transportation/public-health-and-equity-principles-for-transportation. [DOI] [PubMed]
- Bailey ZD, Krieger N, Agenor M, Graves J, Linos M, Bassett MT. Structural racism and health inequities in the USA: Evidence and interventions. Lancet. 2017;389(10077):1453–1463. doi: 10.1016/S0140-6736(17)30569-X. [DOI] [PubMed] [Google Scholar]
- Berkely-Patton J, Bowe-Thompson C, Bradley-Ewing A, Hawes S, Moore E, Williams E, … Goggin K. Taking it to the pews: A CBPR-guided HIV awareness and screening project with Black churches. AIDS Education and Prevention. 2010;22(3):218–237. doi: 10.1521/aeap.2010.22.3.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruton CM, Floyd MF. Disparities in built and natural features of urban parks: Comparison by neighborhood level race/ethnicity and income. Journal of Urban Health: Bulletin of the New Your Academy of Medicine. 2014;91(5):894–907. doi: 10.1007/s11524-014-9893-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchanan D, Kee R, Sadowski LS, Garcia D. The health impact of supportive housing for HIV-positive homeless patients: A randomized controlled trial. American Journal of Public Health. 2009;99:S675–S680. doi: 10.2105/AJPH.2008.137810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bugos E, Frasso R, FitzGerald E, True G, Adachi-Mejia AM, Cannuscio C. Practical guidance and ethical considerations for studies using photo-elicitation interviews. Preventing Chronic Disease. 2014;11(140216):1–9. doi: 10.5888/pcd11.140216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caiola C, Docherty SL, Relf M, Barroso J. Using an intersectional approach to study the impact of social determinants of health for African American mothers living with HIV. Advances in Nursing Science. 2014;37(4):287–298. doi: 10.1097/ANS.0000000000000046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caiola C, Barroso J, Docherty SL. Capturing the social location of African American mothers living with HIV: An inquiry into how social determinants of health are framed. Nursing Research. 2017;66(3):209–221. doi: 10.1097/NNR.0000000000000213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Heightened national response to the HIV/AIDS crisis among African Americans. 2007 Retrieved from http://stacks.cdc.gov/view/cdc/6817/
- Centers for Disease Control and Prevention. Division of Nutrition, Physical Activity, and Obesity (DNPAO) state program highlights urban design and transportation policies and practices. 2011 Retrieved from https://www.cdc.gov/obesity/downloads/UrbanDesignPolicies.pdf.
- Centers for Disease Control and Prevention. HIV among African Americans. 2017a Retrieved from https://www.cdc.gov/hiv/group/racialethnic/africanamericans/index.html.
- Centers for Disease Control and Prevention. HIV among women. 2017b Retrieved from https://www.cdc.gov/hiv/pdf/group/gender/women/cdc-hiv-women.pdf.
- Chatters LM, Taylor RJ, Bullard KM, Jackson JS. Race and ethnic differences in religious involvement: African Americans, Caribbean Blacks and non-Hispanic Whites. Ethnic and Racial Studies. 2009;32(7):1143–1163. doi: 10.1080/01419870802334531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Civic Impulse. S. 795 - 112th Congress: National Black Clergy for the Elimination of HIV/AIDS Act of 2011. 2017 Retrieved from https://www.govtrack.us/congress/bills/112/s795.
- Cohen DA, McKenzie TL, Sehgal A, Williamson S, Golinelli D, Lurie N. Contribution of public parks to physical activity. American Journal of Public Health. 2007;97(3):509–514. doi: 10.2105/AJPH.2005.072447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Janicki-Deverts D. Can we improve our physical health by altering our social networks? Perspectives on Psychological Science. 2009;4(4):375–378. doi: 10.1111/j.1745-6924.2009.01141.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coombes E, Jones AP, Hillsdon M. The relationship of physical activity and overweight to objectively measured green space accessiblity and use. Social Science & Medicine. 2010;70:816–822. doi: 10.1016/j.socscimed.2009.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox S, Drew S, Guillemin M, Howell C, Warr D, Waycott J. Guidelines for ethical visual research methods. Melbourne, Australia: University of Melbourne; 2014. [Google Scholar]
- Creagan ET, Bauer BA, Thomley BS, Borg JM. Animal-assisted therapy at Mayo Clinic: The time is now. Complementary Therapies in Clinical Practice. 2015;21:101–104. doi: 10.1016/j.ctcp.2015.03.002. [DOI] [PubMed] [Google Scholar]
- Commission on the Social Determinants of Health. Closing the gap in a generation: Health equity through action on the social determinants of health. Final Report of the Commission on Social Determinants of Health. Geneva, Switzerland: World Health Organization; 2008. [Google Scholar]
- Delavega E, Lennon-Dearing R. Differences in housing, health and wellbeing among HIV-positive women living in poverty. Social Work in Public Health. 2015;30(3):294–311. doi: 10.1080/19371918.2014.1001934. [DOI] [PubMed] [Google Scholar]
- DiNenno EA, Oster AM, Sionean C, Denning P, Lansky A. Piloting a system for behavioral surveillance among heterosexuals at increased risk of HIV in the United States. The Open AIDS Journal. 2012;6:169–176. doi: 10.2174/1874613601206010169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards LV. Perceived social support and HIV/AIDS medication adherence among African American women. Qualitative Health Research. 2006;16(5):679–691. doi: 10.1177/1049732305281597. [DOI] [PubMed] [Google Scholar]
- Griffith DM, Campbell B, Allen JO, Robinson KJ, Stewart SK. YOUR Blessed Health: An HIV-prevention program bridging faith and public health communities. Public Health Reports. 2010;125(Suppl 1):4–11. doi: 10.1177/00333549101250S102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guillemin M, Drew S. Questions of process in participant-generated visual methodologies. Visual Studies. 2010;25(2):175–188. doi: 10.1080/1472586X.2010.502676. [DOI] [Google Scholar]
- Gubrium AC, Hill AL, Flicker S. A situated practice of ethics for participatory visual and digital methods in public health research and practice: A focus on digital storytelling. American Journal of Public Health. 2014;104:1606–1614. doi: 10.2105/AJPH.2013.301310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankivsky O. Women’s health, men’s health, and gender and health: Implications of intersectionality. Social Science and Medicine. 2012;74(11):1712–1720. doi: 10.1016/j.socscimed.2011.11.029. [DOI] [PubMed] [Google Scholar]
- Harper D. Talking about pictures: A case for photo elicitation. Visual Studies. 2002;17(1):13–26. doi: 10.1080/14725860220137345. [DOI] [Google Scholar]
- Institute of Medicine and National Research Council. Local government actions to prevent childhood obesity. Washington, DC: The National Academies Press; 2009. [PubMed] [Google Scholar]
- Jirapaet V. Effects of an empowerment program on coping, quality of life, and the maternal role adaptation of Thai HIV-infected mothers. Journal of the Association of Nurses in AIDS Care. 2000;11(4):34–45. doi: 10.1016/s1055-3290(06)60394-4. [DOI] [PubMed] [Google Scholar]
- Joint United Nations Programme on HIV and AIDS. Countdown to zero: Global plan towards the elimination of new HIV infections among children by 2015 and keeping their mothers alive. 2011 Retrieved from http://www.unaids.org/sites/default/files/en/media/unaids/contentassets/documents/unaidspublication/2011/20110609_JC2137_Global-Plan-Elimination-HIV-Children_en.pdf.
- Kruger K, Stern SL, Anstead G, Finley EP. Perceptions of companion dog benefits on wellbeing of US military veterans with HIV/AIDS. Southern Medical Journal. 2014;107(3):188–193. doi: 10.1097/SMJ.0000000000000078. [DOI] [PubMed] [Google Scholar]
- Lee M, Rotheram-Borus MJ. Challenges associated with increased survival among parents living with HIV. American Journal of Public Health. 2001;91:1303–1309. doi: 10.2105/ajph.91.8.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maller C, Townsend M, Pryor A, Brown P, St Leger L. Healthy nature healthy people: ‘Contact with nature’ as an upstream health promotion intervention for populations. Health Promotion Interntational. 2005;21(1):45–54. doi: 10.1093/heapro/dai032. [DOI] [PubMed] [Google Scholar]
- Meditz AL, MaWhinney S, Allshouse A, Feser W, Markowitz M, Little S, … Connick E. Sex, race, and geographic region influence clinical outcomes following primary HIV-1 infection. Journal of Infectious Diseases. 2011;203(4):442–451. doi: 10.1093/infdis/jiq085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mignone J, Migliardi P, Harvey C, Davis J, Madariaga-Vignudo L, Pindera C. HIV as chronic illness: Caregiving and social networks in a vulnerable population. Journal of the Association of Nurses in AIDS Care. 2015;26(3):235–245. doi: 10.1016/j.jana.2014.09.002. [DOI] [PubMed] [Google Scholar]
- National AIDS Housing Coalition. Housing is the foundation of HIV prevention and treatment: Results of the National Housing and HIV/AIDS Reasearch Summit. 2005 Retrieved from http://nationalaidshousing.org/PDF/Housing%20&%20HIV-AIDS%20Policy%20Paper%2005.pdf.
- National Prevention Council. National Prevention Strategy. Washington, DC: U.S. Department of Health and Human Services, Office of the Surgeon General; 2011. [Google Scholar]
- Okeke NL, Ostermann J, Theielman NM. Enhancing linkage and retention in HIV care: A review of interventions for highly resources and resource-poor settings. Current HIV/AIDS Reports. 2014;11:376–392. doi: 10.1007/s11904-014-0233-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Packard J. ‘I’m gonna show you what it’s really like out here’: The power and limitation of participatory visual methods. Visual Studies. 2008;23(1):63–77. doi: 10.1080/14725860801908544. [DOI] [Google Scholar]
- Rhodes SD, Hergenrather KC, Wilkin AM, Jolly C. Visions and voices: Indigent persons living with HIV in the Southern United States use Photovoice to create knowledge, develop partnerships and take action. Health Promotion Practice. 2008;9(2):159–169. doi: 10.1177/1524839906293829. [DOI] [PubMed] [Google Scholar]
- Robinson R, Moodie-Mills A. HIV/AIDS inequality: Structural barriers to prevention, treatment, and care in communities of color. 2012 Retrieved from https://cdn.americanprogress.org/wp-content/uploads/issues/2012/07/pdf/hiv_community_of_color.pdf.
- Saldana J. The coding manual for qualitative researchers. 2. Thousand Oaks, CA: Sage; 2013. [Google Scholar]
- Sandelowski M. Qualitative analysis: What it is and how to begin. Research in Nursing and Health. 1995;18:371–375. doi: 10.1002/nur.4770180411. [DOI] [PubMed] [Google Scholar]
- Sandelowski M. What’s in the name? Qualitative description revisited. Research in Nursing & Health. 2010;33:77–84. doi: 10.1002/nur.20362. [DOI] [PubMed] [Google Scholar]
- Siegal JM, Angulo FJ, Detels R, Wesch J, Mullen A. AIDS diagnosis and depression in the Multicenter AIDS Cohort Study: The ameliorating impact of pet ownership. AIDS Care. 1999;11(2):157–170. doi: 10.1080/09540129948054. [DOI] [PubMed] [Google Scholar]
- Syed ST, Berber BS, Sharp LK. Traveling toward disease: Transportation barriers to health care access. Journal of Community Health. 2013;38:976–993. doi: 10.1080/713612410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teti M, French B, Bonney L, Lightfoot M. “I created something new with something that had died”: Photo-narratives of positive transformation among women with HIV. AIDS Behavior. 2015;19(7):1275–87. doi: 10.1007/s10461-015-1000-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teti M, Murray C, Johnson L, Binson D. Photovoice as a community-based participatory research method among women living with HIV/AIDS: Ethical opportunities and challenges. Journal of Empirical Research on Human Research Ethics. 2012;7(4):34–43. doi: 10.1525/jer.2012.7.4.34. [DOI] [PubMed] [Google Scholar]
- Teti M, Pichon L, Kabel A, Farnan R, Binson D. Taking pictures to take control: Photovoice as a tool to facilitate empowerment among poor and racial/ethnic minority women with HIV. Journal of the Association of Nurses in AIDS Care. 2013;24(6):539–553. doi: 10.1016/j.jana.2013.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thygeson NM. Implementing adaptive health practice: A complexity-based philosophy of health care. In: Sturmberg JP, Martin CM, editors. Handbook of systems and complexity in health. New York, New York: Springer Science + Business Media; 2013. [Google Scholar]
- U.S. Census Bureau. Income, expenditures, poverty, and wealth: Statistical abstract of the United States: 2012. 2012 Retrieved from https://www.census.gov/library/publications/2011/compendia/statab/131ed/income-expenditures-poverty-wealth.html.
- Wang C. Photovoice: A participatory action research strategy applied to women’s health. Journal of Women’s Health. 1999;8(2):185–192. doi: 10.1089/jwh.1999.8.185. [DOI] [PubMed] [Google Scholar]
- Wang C, Burris MA. Photovoice: Concept, methodology, and use for participatory needs assessment. Health Education & Behavior. 1997;24(3):369–387. doi: 10.1177/109019819702400309. [DOI] [PubMed] [Google Scholar]
- Zartler U, Richter R. My family through the lens. Photo interviews with children and sensitive aspects of family life. Children & Society. 2014;28:42–54. doi: 10.1111/j.1099-0860.2012.00447.x. [DOI] [Google Scholar]



