Abstract
Key challenges in providing lifelong antiretroviral therapy (ART) to pregnant and breastfeeding women (Option B+) in sub-Saharan Africa include achieving long-term adherence and retention in care. One intervention that may help address these challenges is mobile text messaging. We evaluated the acceptability of a text messaging intervention to support women’s ART adherence and retention in care in rural western Kenya. 40 in-depth interviews with 20 pregnant/postpartum women infected with HIV, their male partners, and 4 focus groups with 30 health care providers were conducted during September–November 2014. Data were coded and analyzed using thematic analysis. Findings revealed the following themes: (a) overall acceptability of the text messaging intervention; (b) proposed content of text messages; (c) format, timing, and language of text messages; and (d) potential challenges of the text messaging intervention. Findings were used to refine a text messaging intervention being evaluated at Kenyan study sites rolling out Option B+.
Keywords: adherence, HIV, Kenya, prevention of mother-to-child transmission, text messaging
To achieve the goal of eliminating mother-to-child transmission (eMTCT) and improving the health of mothers living with HIV, sub-Saharan African countries are adopting World Health Organization (WHO 2012; 2014) recommendations that simplify treatment protocols and lessen the resource burden associated with other eMTCT strategies. Option B+, life-long antiretroviral therapy (ART) for all pregnant and breastfeeding mothers infected with HIV, regardless of CD4+T cell count or clinical staging, was launched in 2010 and has been recognized as a promising strategy (WHO 2012; 2014).
Although Option B+ appears to have increased ART coverage for pregnant women in Malawi (49% in 2011 to 60% in 2012), the Ministry of Health reported retention rates markedly decreased from 87% at 2 months from time of initiation to 64% at 12 months during the first quarter in 2013 (Mwapasa et al., 2014; Tenthani et al., 2014; WHO, 2014). Research has revealed that Option B+ patients who started ART while pregnant or breastfeeding were more likely to fail to return after the initial clinic visit, compared to patients who initiated ART for their own health (Haas et al., 2016; Tenthani et al., 2014).
The challenge of retaining mother-infant pairs in the continuum of eMTCT HIV care is not unique to Malawi. Across sub-Saharan Africa, approximately 77.5% of patients were retained on average after a 9-month follow-up; loss to follow-up and death accounted for 56% and 40% of attrition (Rosen, Fox, & Gill, 2007).
Mobile Health (mHealth) strategies, such as text messaging, have the potential to serve as low-cost and effective interventions to support adherence and retention; text messaging interventions in HIV care have shown much promise (Kanters et al., 2017). Two key randomized controlled trials conducted in Kenya assessed the efficacy of mobile short messaging service (SMS) interventions on adherence to ART (Lester et al., 2010; Pop-Eleches et al., 2011). In both trials, mobile phone text messaging was significantly associated with greater ART adherence at 48 to 52 weeks when compared to standard of care (Horvath, Azman, Kennedy, & Rutherford, 2012; Lester et al., 2010; Pop-Eleches et al., 2011).
Rigorous mHealth research in the maternal, neonatal, and child health population has been limited in sub-Saharan Africa, particularly regarding use in prevention of mother-to-child transmission (PMTCT) programs implementing Option B+ (Philbrick, 2013). Unclear descriptions of the interventions, lack of theoretical frameworks, and lack of information on study impact in the existing literature make it difficult to interpret and replicate effects on maternal and infant health (Lee et al., 2016). However, there is modest evidence to suggest that text messaging interventions may improve antenatal care attendance (Lund et al., 2014) or increase PMTCT service retention and infant HIV testing (Odeny, Bukusi, et al., 2014). Additionally, results of meta-analyses of effects of text messaging for breastfeeding have indicated improvement in breastfeeding practices (Flax et al., 2014; Jiang et al., 2014; Lee et al., 2016; Sellen et al., 2013).
Based on the Kenya Demographic and Health Survey conducted in 2014, mobile phone ownership in rural households increased from 53% to 80% between 2008 and 2014 (Kenya National Bureau of Statistics, Ministry of Health, National AIDS Control Council, Kenya Medical Research Institute, National Council for Population and Development, & Demographic and Health Surveys, Inter City Fund International, 2015). As mobile networking coverage has continued to expand, mobile phone text messaging has provided the flexibility to individualize text messaging for better uptake and provided health care support and trust-building by promoting bi-directional communication between provider and patient (Finitsis, Pellowski, & Johnson, 2014; Philbrick, 2013). However, the acceptability and effectiveness of an adapted long-term text messaging intervention for pregnant women living with HIV in the context of Option B+ require further study (Kassaye et al., 2016). To this end, we are conducting rigorous research that aims to assess the effectiveness of a Health Belief Model (HBM)-based text messaging intervention (Odeny, Bukusi, et al., 2014; Rosenstock, 1974) on ART adherence and retention in care in pregnant mothers infected with HIV and infants exposed to HIV in rural Kenya. In the formative research presented here, we explored the feasibility and acceptability of a text messaging intervention for pregnant and postpartum women infected with HIV, their male partners, and health care providers in a rural setting.
Methods
Qualitative research methods were used to achieve the study objectives. Forty individual gender-matched, one-on-one in-depth interviews with pregnant/postpartum women infected with HIV and their male partners (n = 20), and four focus groups involving a total of 30 health care providers were conducted between September and November 2014 at four health care facilities in Kisumu, Migori, and Homabay counties (formerly Nyanza Province), Kenya. The four health care facilities were selected from 20 facilities participating in the Mother and Infant Visit Adherence and Treatment Engagement (MOTIVATE) Study, a trial of interventions to support adherence and retention in the context of Option B+ rollout (Clinicaltrials.gov NCT02491177). Potential female participants were identified by health care workers using patient registries and were contacted and screened for eligibility. After obtaining permission from interested participants, we contacted the women’s male partners and asked them to participate. The interviews were scheduled at a convenient date and time and conducted in a private location chosen by each participant.
Study Setting and Participants
HIV prevalence at the study sites has been estimated to be up to four times higher than the national average (5.9%), with rates ranging from 14.3% (Migori County) to 19.9% (Kisumu County) and 26.0% (Homabay County; Ministry of Health & National AIDS Control Council, 2016). Study participants were recruited from health facilities providing Option B+ services in four selected study communities (Minyenya Dispensary, Nyandiwa Dispensary, Lwanda Dispensary, Rabuor Health Clinic); the pregnant or postpartum participants were patients receiving care in these facilities. The sites were all supported by Family AIDS Care and Education Services (FACES), a President’s Emergency Plan for AIDS Relief/Centers for Prevention and Disease Control-funded program that was implemented as a collaboration between the Kenya Medical Research Institute and the University of California San Francisco (Kulzer et al., 2012).
Eligibility
Participants eligible for the study were: (a) pregnant or postpartum women infected with HIV, (b) male partners of pregnant or postpartum women infected with HIV who had disclosed, (c) health care workers currently working/supervising at one of the four study sites, and (4) ages 18 years or older.
Ethics Approval
Approval for the study was obtained from the University of Colorado, Denver, Institutional Review Board; the University of Alabama at Birmingham Institutional Review Board; and the Kenya Medical Research Institute Institutional Review Board. All participants provided written informed consent and were reimbursed for study-related travel.
Data Collection
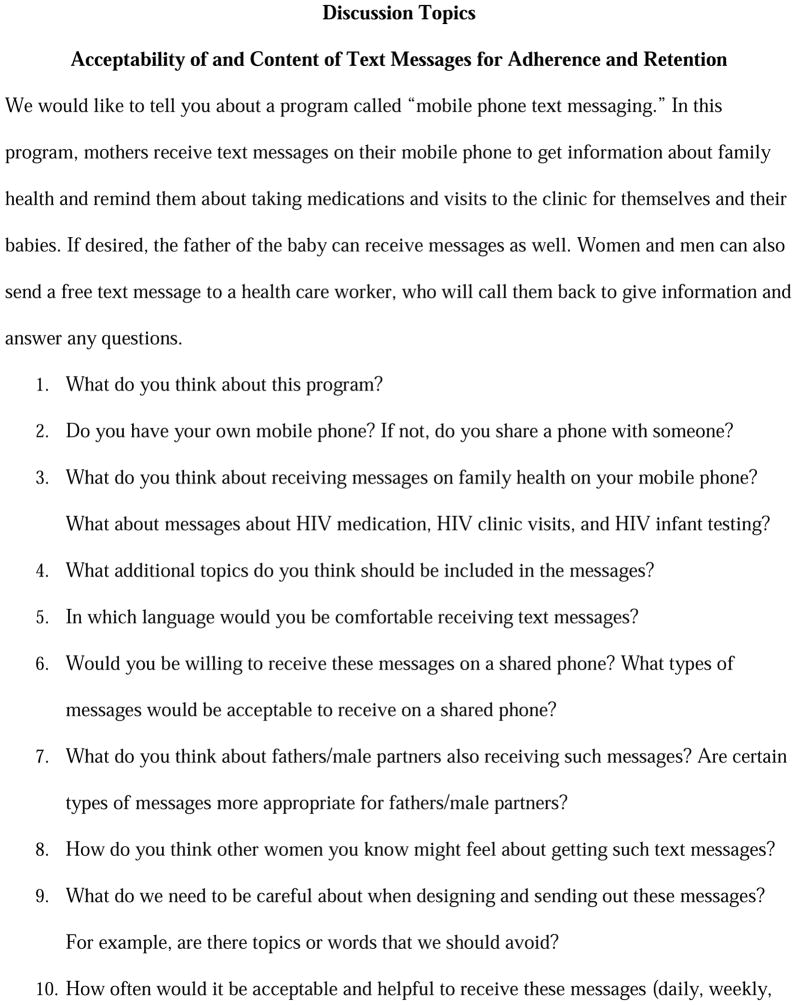
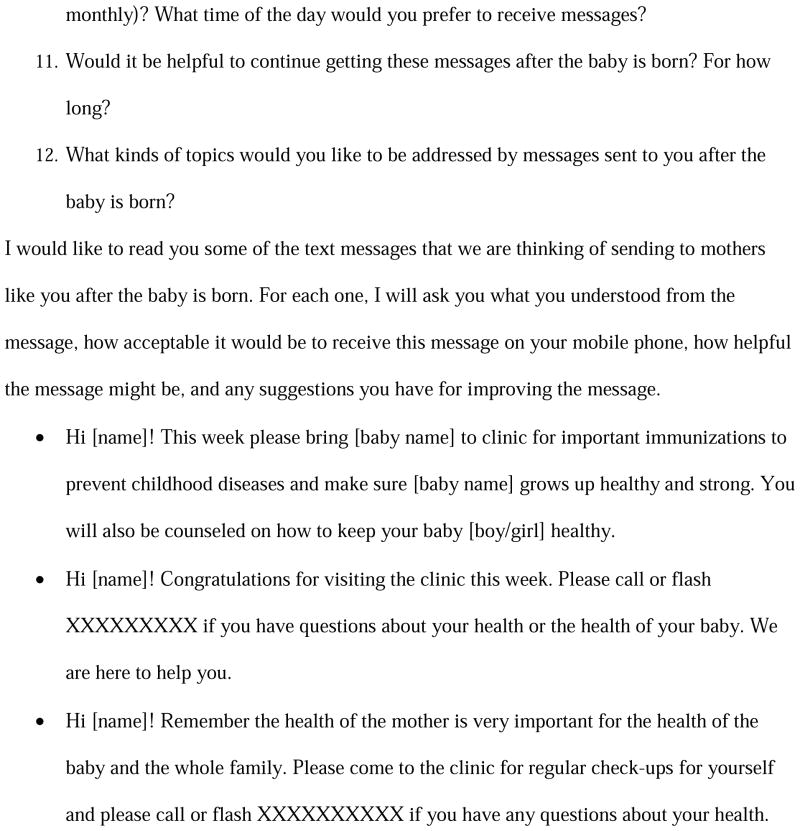
Qualitative in-depth interview and focus group discussion guides were developed based on a review of the literature and our team’s prior research that had used constructs from the HBM to develop a text messaging intervention for postpartum retention in care and infant HIV testing (Attride-Stirling, 2001; Braun & Clarke, 2006; Odeny, Newman, et al., 2014). The guides consisted of a list of open-ended questions and follow-up probes; topics included the acceptability of proposed interventions for the trial including text messaging (Figure 1). Experienced moderators fluent in English and local languages underwent additional training in qualitative interviewing, including study topics prior to initiation of the study.
Figure 1.
Interview guide for in-depth interview of women who have HIV in the antenatal clinic.
Individual in-depth interviews
To achieve our study objective of exploring perceptions of the intervention in our targeted population, we recruited a convenience sample of 20 pregnant or postpartum women infected with HIV (5 women per facility) and 20 male partners (5 men per facility). This sample size was sufficient to achieve data saturation (Creswell, 2013; Fusch & Ness, 2015; Guest, Bunce, & Johnson, 2006). Of the 20 male partners recruited for the study, half were living with HIV (concordant relationship) and half were uninfected (discordant relationship). Individual qualitative interviews were conducted in private settings in English, Dholuo, or Kiswahili language, depending on the preference of the participant. The interviews were conducted by gender-matched interviewers who identified themselves as members of an external research team, independent of the health care facility. Participant characteristics were collected on a brief structured form, including demographics, job characteristics, pregnancy, and HIV-related information.
Focus groups
Potential service provider participants were contacted in person by the research coordinator and asked to participate in a focus group located at their health care facilities. A total of 30 health care providers participated in the four focus groups. Providers included nurses, community health care workers, health educators, mentor mothers, HIV counselors, laboratory technicians, facility in-charges, program technical advisors, and administrative staff. Participants in focus groups were purposively selected for diversity in occupational characteristics, to ensure that various types of health care workers providing services to pregnant women at the site were included. Participant characteristics were collected, including demographics, and job characteristics.
Data Management and Analysis
Interviews and focus groups were digitally recorded, translated into English if applicable, and transcribed verbatim by professional transcriptionists, excluding any identifying information. All files were password-protected and stored in a secure location. Transcripts were coded independently by a team of two researchers using the Dedoose qualitative software program (SocioCultural Research Consultants, LLC). Coding and analysis followed a thematic analysis approach (Attride-Stirling, 2001; Braun & Clarke, 2006). The coding framework was based on the literature, topics from interview guides, and emerging themes from transcripts (Attride-Stirling, 2001). The consistency of coding between coders was established by initially coding the same transcripts and through weekly discussions between coders until consistency was fully established. Excerpts from broad codes were then fine-coded using an inductive approach by the same coders. As new themes emerged, the coding framework was refined and sub-themes continually identified (Attride-Stirling, 2001).
Results
Forty patients (20 pregnant/postpartum women infected with HIV and 20 male partners), ages 18 to 54 years (M = 28 ± 7.8), and 30 healthcare providers (8 male and 22 female), ages 20 to 58 years (M = 32.2 ± 7.2), participated in in-depth interviews and focus group discussions, respectively. Most of the patients had some primary level education, with the majority working in the fishing or agricultural industries. Many service providers had some form of college-level training. Among the patients, most were in monogamous marriages (85%) and had an average of 2.8 living children. Half of patients interviewed were in HIV-discordant relationships (by study design). See Table 1 for details regarding participant characteristics and demographics.
Table 1.
Socio-demographic and HIV-related Participant Characteristics
| Characteristic | Female N = 20 |
Male N = 20 |
Health care workers N = 30 |
|---|---|---|---|
| Age (years) | |||
|
| |||
| M (SD) | 24.7 (4.8) | 33.5 (8.8) | 32.2 (7.2) |
|
| |||
| Participant education, N (%) | |||
|
| |||
| Less than Primary | 11 (55.0) | 6 (30.0) | 0 (0) |
|
| |||
| Completed Primary | 5 (25.0) | 6 (30.0) | 0 (0) |
|
| |||
| Less than Secondary | 1 (5.0) | 3 (15.0) | 0 (0) |
|
| |||
| Completed Secondary | 3 (15.0) | 5 (25.0) | 10 (33.3) |
|
| |||
| Some College | 0 (0) | 0 (0) | 20 (66.7) |
|
| |||
| Marital status, N (%) | |||
|
| |||
| Monogamous marriage | 16 (80.0) | 18 (90.0) | 20 (66.7) |
|
|
|||
| Polygamous marriage | 3 (15.0) | 2 (10.0) | |
|
| |||
| Current occupation, N (%) | |||
|
| |||
| Agriculture | 3 (15.0) | 9 (45.0) | 0 (0) |
|
| |||
| Business/sales | 5 (25.0) | 2 (10.0) | 0 (0) |
|
| |||
| Skilled worker | 2 (10.0) | 9 (45.0) | 0 (0) |
|
| |||
| Housewife | 9 (45.0) | 0 (0) | 0 (0) |
|
| |||
| Length of time in current occupation (years) | |||
|
| |||
| M (SD) | Not asked | Not asked | 4.7 (5.1) |
|
| |||
| Number of living children | |||
|
| |||
| M (SD) | 2.2 (1.1) | 3.2 (1.9) | 1.8 (1.8) |
|
| |||
| Pregnancy status of self/partner, N (%) | |||
|
| |||
| Pregnant | 12 (60.0) | 12 (60.0) | Not asked |
| Postpartum | 8 (40.0) | 8 (40.0) | |
Overall, text messaging was perceived as an efficient method by which patients and health care workers could easily communicate about health matters. It was also perceived as an important tool to remind patients about adhering to clinic visits and medications. However, participants underscored the importance of overcoming logistical and cultural challenges if the text messaging intervention was to be effective. The results are described below, organized by themes and sub-themes that represented perceptions about text messaging. The development of the text messaging intervention based on these results is also described. Characteristics of the speaker are provided with each quotation including participant type and number, age, and couple HIV status.
Acceptability of Text Messaging Intervention
Overall, most participants welcomed the idea of receiving text messages that aimed to improve their lives, improve the lives of their infants and children, and encouraged healthy living.
That [mobile texting] is a good intervention and should be introduced soonest as it will help in reminding clients who may forget about the time for taking medication and also when to return for the clinic visits. I think that would be an efficient way for reminding people for taking their drugs as well as coming for their clinic appointment visits. It would be a great step and it would enhance appropriate use of the medicines. (Male Partner 02, 36 years, Discordant)
Additionally, many patients believed that text messaging was an important communication tool that health facilities could employ to encourage community members to use antenatal care services and potentially improve patient-provider relationships.
Sometimes you don’t go to the clinic. There are people who fear going to the clinic. Someone can encourage you by sending you a message. You will read the message. It will encourage you. It gives you a platform to ask a question by replying to the message. You will get the answer. (Postpartum Woman 04, 21 years, Concordant)
Further, one health care worker postulated that the text messaging intervention could help strengthen the patient-provider relationship; “It strengthens the relationship between the facility and the clients” (Mentor Mother 08, 33 years).
Health care providers conveyed similar sentiments about the positive influences the intervention could have on patients. However, they also acknowledged potential challenges with the intervention such as inadvertent disclosure and potential conflict among couples.
The text message is also a good idea but I am also seeing a limitation … I am seeing a scenario whereby the mother hasn’t disclosed, how is the SMS going to assist the mother if [it] has the detailed information that the partner is not supposed to know? And if I get the SMS and I am your partner I will ask what is so special about you in this facility that they even send you a text to bring the baby for testing and that may bring issues. (Clinical & Community Health Assistant, Female, 34 years, Focus Group Discussion [FGD])
The analysis revealed that acceptability of the text messaging intervention might hinge on male partner support, especially if mobile phones were shared. To help improve the likelihood of acceptability, participants proposed that couples be adequately informed of the intervention and consent be sought from the couple. “I raised that issue earlier and I think they should come so that you talk to both of them before sending the messages so that it shouldn’t be a challenge” (Lab Technician, Male, 33 years, FGD).
Proposed Content of Messages
In addition to exploring the acceptability and usefulness of a text messaging intervention, participants discussed suggestions for the content of the text messages. Many recommended sending text messages that promoted ART adherence, as well as other HIV-related health issues. “It will help in reminding me to take my medication that I couldn’t have taken on time; it will also help remind me of the clinic visit date and taking my child to the clinic, which is very important” (Pregnant Woman 03, 24 years, Concordant). Participants also felt that it was important that community members remain vigilant about their HIV status by getting tested regularly and being well educated on proper condom use, especially in the case of serodiscordant relationships. When asked, What other kind of information would you like to be included in the short text messages? one respondent replied, “Issues about how to protect a negative partner from getting HIV-infected” (Male Partner 02, 32 years, Discordant).
Several participants advocated for messages that promoted healthy living with HIV; they indicated that people living with HIV needed supportive messaging that encouraged positive living. “I think any advice that someone can give whereby you … get to deal with stress issues and eliminate them so let them advise as much as they can … Anything health-wise how you can live positively with HIV” (Pregnant Woman 04, 21 years, Concordant). Moreover, one participant emphasized that the intervention could be employed strategically as a motivational tool to encourage health-seeking behaviors by male partners and community members in general. “I think the partners need to be involved whether they are negative or not so that they also encourage the mothers to know their status and to continue accessing care” (Community Health Care Worker, Male, 37 years, FGD).
A few health care providers, on the other hand, believed that message content should be limited to clinic visit adherence. To remind patients to adhere to medications was considered inappropriate as it required daily text messages. They emphasized that managing medication adherence would be better handled directly by health care providers. “I feel that the issues of drugs should be handled at the facility and the phone should only handle dates and appointments” (Nurse, Male, 27 years, FGD).
Format, Timing, and Language of Messages
Participants viewed the timing of text messages not only as a way to ensure that messages were received at a convenient time that allowed for reading and responding, but also to ensure that messages came at a time that minimized the risk of inadvertent disclosure of HIV status. Most preferred that messages arrive in the early morning or late evening when they would be at home. “Because at night I am alone, during the day someone could be holding my phone or someone asks for a phone to use. I, therefore, prefer at night” (Pregnant Woman 05, 38 years, Concordant). Additionally, to minimize the potential for intervention fatigue, most participants recommended receiving texts no more than once a week.
Because sometimes my husband is far away … And when he is not around he goes with the phone so I will not get the messages if they send daily. He might also get bored with those messages [on] the phone. So, if they are sent once a week and you tell him that these are messages from such a facility…” (Postpartum woman, 02, 20 years, Discordant)
Many participants suggested that words of endearment be avoided in text messages, as such messages could bring suspicions of infidelity and possible conflict between couples. “… Some words shouldn’t be used, for example, ‘How are you sweetheart?’ This will make my partner be suspicious of the whole idea” (Pregnant Woman 01, 21 years, Concordant).
Potential Challenges of Text Messaging Intervention
A prevailing challenge voiced by many participants was the lack of access to a consistent power source for charging mobile phones. Consequently, participants could potentially spend an extensive period without being able to access their mobile phones.
Some may have phones but due to power challenges, the phone may be put on even just twice a week. Maybe the message was sent on Monday and the phone has been put on today and she was to come to the clinic on Wednesday. (Laboratory Technician, Female, 30 years, FGD)
In other circumstances, participants explained that the scarcity of electricity in many rural homes forced people to charge their mobile phones at charging kiosks in the community. Several participants feared inadvertent disclosure of their HIV status and insisted that measures be taken to keep the information shared confidential. To minimize risks of inadvertent disclosure, the participants suggested omitting “HIV” as well as patient names from text messages that promoted drug adherence or clinic appointment reminders. As this participant explained, “They can just [create] the messages without mention [of] HIV but they can just say medicine…The message can simply say ‘Have you taken your medication?’” (Pregnant Woman 01, 25 years, Discordant). However, a few participants harbored no reservations about using HIV; they believed text messages should be transparent and clearly relate the intended message. As this participant expressed, “There is no need for it to be coded. A spade should be called a spade, not a big spoon” (Pregnant Woman 01, 25 years, Concordant). The participants also emphasized that it was essential that facilities offering the text messaging service remained vigilant to ensure that messages were sent to the correct mobile phone numbers to avoid unintentional disclosure of HIV status.
Development of Text Messages
Based on findings from our formative study, as well as our prior research (Odeny, Newman, et al., 2014), we developed weekly text messages to begin during pregnancy and continue until the infant reached 1 year of age. Aspects of the HBM were used to develop the specific text messages; given the use of communication as a tool to influence behavior in this intervention, the HBM was an ideal theory to employ (Janz & Becker, 1984; Rosenstock, 1974; Rosenstock, Strecher, & Becker, 1988).
The messages were developed to incorporate key constructs of the HBM, including self-efficacy, cues to action, and perceived benefits (Table 2). Text messages based on the cues to action construct included recommendations for actions participants could perform to stay adherent to and retained in care, such as coming for regular clinic visits or making a birth plan. Another group of messages facilitated perceived self-efficacy or self-confidence to adhere to medications, attend clinic, and adopt other health promoting behaviors, by providing motivation and support for taking actions that promoted health (Odeny, Newman, et al., 2014). Other text messages emphasized the perceived benefits of adherence to care and recommendations to prevent HIV transmission, as well as safe infant care.
Table 2.
Examples of Text Messages Based on HBM Constructs
| HBM Construct | Health Content of Messages | Text message |
|---|---|---|
| Cues to Action | Birth planning | Hello_____! Have you planned where you will deliver your baby? Please call or flash if you have questions or want to discuss your options. |
| Clinic visits | Hi_____! Know that a mother’s health is important and connected to the child’s health of the whole family. Please come to the clinic for your appointments and call or flash _____ in case you have a question touching on your health. | |
| Perceived Benefits | Couple HIV testing | Testing together and knowing each other’s status allows you to plan together and make joint informed decisions about your family’s future. |
| Condom use | Condom use = peace of mind. Talk to your partner about using condoms. Please call or flash_____ for any questions or help. | |
| Self-Efficacy (positive reinforcement through motivational or supportive messages) | Medication adherence | When you take your medications regularly, you are in control. Good job with your medications. |
| Clinic visits | Hi_____! Congratulations for visiting the clinic this week. Please call or flash_____ if you have questions about your pregnancy. We are here to help you. |
Note. HBM = Health Belief Model.
Discussion
The success of an mHealth intervention, such as text messaging, not only hinges on cost-effectiveness but also on the perceived usefulness and ease of use by intended users (Smillie et al., 2014). Building on prior research in rural western Kenya (Odeny, Newman, et al., 2014), we sought to explore the acceptability and perceptions of a long-term text messaging intervention for pregnant and postpartum women living with HIV. The interviews and focus groups in the current study revealed key themes to inform refinement of the content, optimum frequency, and timing of text messages that were likely to facilitate women’s ART adherence and retention in care in the context of Option B+.
Participants consistently agreed that their health would benefit greatly from reminders to take and refill medications, as well as clinic visit reminders. Research has indicated that, during ART initiation, the most cited reasons for missed doses were incidental events such as journeys, running out of pills, and forgetfulness; for these and other reasons, participants appreciated the idea of receiving reminders (Mbuagbaw, Bonono-Momnougui, & Thabane, 2012). Additionally, participants felt that receiving motivational and educational content would provide psychosocial support, thus improving adherence. Moreover, as was also found in a study in Uganda (Ware et al., 2016), participants conveyed that recipients of text messages from the health care facility would find comfort in knowing that the health care providers cared, thus strengthening the health care provider-patient relationship and communication. Similarly, research in Kenya and Cameroon revealed that a text messaging intervention had the potential to be useful in increasing communications between patients and health care providers, enabling participants to improve medication and appointment adherence (Mbuagbaw et al., 2012; Smillie et al., 2014).
Frequency and timing of the text messages were also perceived as important elements to improve acceptability of the intervention. Most agreed that receiving text messages weekly would minimize the risk of intervention fatigue while continually engaging patients throughout the intervention period. Similarly, a recent systematic review found that participants receiving daily messages were less likely to achieve optimal adherence due to user fatigue (Mbuagbaw et al., 2012). More importantly, timing text messages such that they were received and read privately, maintaining participant confidentiality, and improving acceptability of the intervention, was a strong theme. Additionally, there was strong support for tailoring text messages to participant preferences, to ensure the intervention would be more readily accepted and adopted into daily routines. Similar preferences have been noted elsewhere in qualitative and quantitative research (Head, Noar, Iannarino, & Harrington, 2013; Lester et al., 2010; Mbuagbaw et al., 2012; Pop-Eleches et al., 2011).
Beyond technical and logistic difficulties described earlier, the prevailing challenge voiced by many participants, which could potentially undermine the acceptability and effectiveness of the intervention, was the high level of perceived HIV-related stigma. Many participants recommended avoiding the use of HIV or any terminology that would inadvertently disclose the status of the individual. Our findings suggested that inadvertent disclosure of HIV status could instigate family conflict or community shunning. This finding was similar to results from our previous research (Odeny, Newman, et al., 2014) and consistent with other studies conducted among similar participants in the same region (Turan et al., 2011; Walcott, Hatcher, Kwena, & Turan, 2013). Being sensitive to issues involving disclosure, including minimizing potential physical or emotional harm while refining and implementing the intervention was imperative (Odeny, Newman, et al., 2014).
Another important concern broached by participants during discussions was the issue of male involvement and its potential impact on the acceptability of the intervention. Other studies have indicated that uptake of and retention in antenatal care and maternal and child health services by pregnant women was greatly influenced by male partners; the inclusion of male partners could enhance male support of antenatal care clinic visits and medication adherence (Hatcher et al., 2012; Odeny, Newman, et al., 2014; Turan et al., 2011). Additionally, participants felt that male participants who received text messages would be afforded the opportunity to attain knowledge that could help them and their families achieve optimal health. The women’s interest (especially those desiring to disclose their HIV status) in male participation could be leveraged constructively to improve the use of maternal and child health services, potentially leading to improved disclosure and couple support (Hatcher et al., 2012; Odeny, Newman, et al., 2014). Findings from a study in Kenya suggested that text message reminders and tips were seen as catalysts for initiating dialogue with male partners to address partner disclosure and promote partner support for aspects of health other than PMTCT (Jennings, Ong’ech, Simiyu, Sirengo, & Kassaye, 2013).
Limitations
Because the study recruited pregnant and postpartum women visiting the clinics and their male partners, perceptions presented about the text messaging intervention could be inherently different than those of women not engaged in health services and could, thus, limit the transferability of findings. Due to the requirement of HIV status disclosure for male partner recruitment, male partners interviewed for our study may have been more supportive on the topic of HIV than men in the general population. Additionally, perceptions shared about the intervention could have been more favorably presented as participants may have been reluctant to express negative views about a potential service to be offered or social desirability bias (Nederhof, 1985). To minimize these biases, professional interviewers who were identified as being separate from the health facility staff were chosen to conduct the in-depth interviews. Additionally, the interviews were conducted in private locations to foster sharing of confidential views. Further, using a heterogeneous sampling technique, that is, recruiting pregnant and postpartum women, male partners, and health care workers, allowed for the exploration of various perspectives on issues that could impact many individuals.
Conclusion
Text messaging interventions targeting medication and visit adherence are quickly becoming integrated into health systems to improve maternal and child health outcomes across sub-Saharan Africa. Clinics and hospitals in the study area were already beginning to institute similar text messaging services for different categories of patients. For these interventions to be successful, it is necessary to understand the perceptions of the end users and stakeholders; in this case, the results of this formative study were shared with health workers from each site and community representatives through stakeholder meetings at the study sites. Accordingly, our findings, in addition to critiques provided by health workers and community representatives, were used to refine text messaging interventions for greater acceptability. The effectiveness of the intervention is being evaluated in a randomized control trial [ClinicalTrials.gov #14-0331]. Future intervention research should similarly endeavor to engage the target population early in the development phase of the intervention through formative research to address issues of feasibility and improve acceptability.
Key Considerations.
A tailored mobile text messaging intervention can be a feasible and acceptable way to support Plan B+.
Text messaging intervention can be an important communication tool to improve patient-provider relationships.
Mobile text messaging could improve medication and clinic adherence by including reminders for ART and clinic visits; it could also encourage HIV testing and positive living for overall well-being.
Confidentiality is a key consideration with mobile text messaging programs.
Messages should be generic and omit mention of HIV for greater acceptability.
Acknowledgments
We thank the Kenyan women and men who participated in the Mother and Infant Visit Adherence and Treatment Engagement (MOTIVATE) Study of interventions to support adherence and retention in the context of Option B+ rollout and shared their experiences and opinions with us. We acknowledge the support of the KEMRI-UCSF Collaborative Group, the Director of KEMRI, and especially the Family AIDS Care and Education Services (FACES) program.
The co-principal investigators of the study are Dr. Lisa Abuogi and Dr. Janet Turan. This work was supported by the National Institute of Child Health and Human Development (grant number R01HD080477, 2014; ClinicalTrials.gov #14-0331). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Child Health and Human Development or the National Institutes of Health. The funders had no role in study design, data collection, data analysis, decision to publish, or preparation of the manuscript.
Footnotes
Disclosures
The authors report no real or perceived vested interests that relate to this article that could be construed as a conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Pamela Musoke, Doctoral student, Department of Health Care Policy and Organization, School of Public Health, University of Alabama at Birmingham, Birmingham, Alabama, USA.
C. Ann Gakumo, Associate Professor, Department of Acute, Chronic and Continuing Care, School of Nursing, University of Alabama at Birmingham, Birmingham, Alabama, USA.
Lisa L. Abuogi, Pediatrician and Assistant Professor, Department of Pediatrics, University of Colorado Denver, Aurora, Colorado, USA.
Eliud Akama, Technical advisor at the Kenya Medical Research Institute (KEMRI), and KEMRI/Research Care and Training Program (RCTP), Center for Microbiology Research, Kisumu, Kenya.
Elizabeth Bukusi, Co-director of the Kenya Medical Research Institute, Nairobi, Kenya and principal research officer of the KEMRI/RCTP, Center for Microbiology Research, Kisumu, Kenya.
Anna Helova, Doctoral student, Department of Health Care Policy and Organization, School of Public Health, University of Alabama at Birmingham, Birmingham, Alabama, USA.
Wafula Z. Nalwa, Physician, Migori County Referral Hospital, Migori, Kenya.
Mariciannah Onono, Research officer, Kenya Medical Research Institute, and KEMRI/RCTP, Center for Microbiology Research, Kisumu, Kenya.
Sydney A. Spangler, Assistant Professor, Nell Hodgson Woodruff School of Nursing and Department of Global Health, Emory University, Atlanta, Georgia, USA.
Iris Wanga, Study coordinator of the parent study, Kenya Medical Research Institute, and KEMRI/RCTP, Center for Microbiology Research, Kisumu, Kenya.
Janet M. Turan, Professor, Department of Health Care Policy and Organization, School of Public Health, University of Alabama at Birmingham, Birmingham, Alabama, USA.
References
- Attride-Stirling J. Thematic networks: An analytic tool for qualitative research. Qualitative Research. 2001;1(3):385–405. [Google Scholar]
- Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology. 2006;3(2):77–101. doi: 10.1191/1478088706qp063oa. [DOI] [Google Scholar]
- Creswell JW. Research design: Qualitative, quantitative, and mixed methods approaches. Thousand Oaks, CA: Sage; 2013. [Google Scholar]
- Finitsis DJ, Pellowski JA, Johnson BT. Text message intervention designs to promote adherence to antiretroviral therapy (ART): A meta-analysis of randomized controlled trials. PloS One. 2014;9(2):e88166. doi: 10.1371/journal.pone.0088166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flax VL, Negerie M, Ibrahim AU, Leatherman S, Daza EJ, Bentley ME. Integrating group counseling, cell phone messaging, and participant-generated songs and dramas into a microcredit program increases Nigerian women’s adherence to international breastfeeding recommendations. Journal of Nutrition. 2014;144(7):1120–1124. doi: 10.3945/jn.113.190124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusch PI, Ness LR. Are we there yet? Data saturation in qualitative research. The Qualitative Report. 2015;20(9):1408. [Google Scholar]
- Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field Methods. 2006;18(1):59–82. [Google Scholar]
- Haas AD, Tenthani L, Msukwa MT, Tal K, Jahn A, Gadabu OJ, … Keiser O. Retention in care during the first 3 years of antiretroviral therapy for women in Malawi’s option B+ programme: An observational cohort study. Lancet HIV. 2016;3(4):e175–e182. doi: 10.1016/s2352-3018(16)00008-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatcher AM, Turan JM, Leslie HH, Kanya LW, Kwena Z, Johnson MO, … Cohen CR. Predictors of linkage to care following community-based HIV counseling and testing in rural Kenya. AIDS and Behavior. 2012;16(5):1295–1307. doi: 10.1007/s10461-011-0065-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Head KJ, Noar SM, Iannarino NT, Harrington NG. Efficacy of text messaging-based interventions for health promotion: A meta-analysis. Social Science and Medicine. 2013;97:41–48. doi: 10.1016/j.socscimed.2013.08.003. [DOI] [PubMed] [Google Scholar]
- Horvath T, Azman H, Kennedy GE, Rutherford GW. Mobile phone text messaging for promoting adherence to antiretroviral therapy in patients with HIV infection. Cochrane Database Systematic Review. 2012;3:Cd009756. doi: 10.1002/14651858.cd009756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janz NK, Becker MH. The Health Belief Model: A decade later. Health Education Quarterly. 1984;11(1):1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- Jennings L, Ong’ech J, Simiyu R, Sirengo M, Kassaye S. Exploring the use of mobile phone technology for the enhancement of the prevention of mother-to-child transmission of HIV program in Nyanza, Kenya: A qualitative study. BMC Public Health. 2013;13:1131. doi: 10.1186/1471-2458-13-1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang H, Li M, Wen LM, Hu Q, Yang D, He G, … Qian X. Effect of short message service on infant feeding practice: Findings from a community-based study in Shanghai, China. Journal of the American Medical Association Pediatrics. 2014;168(5):471–478. doi: 10.1001/jamapediatrics.2014.58. [DOI] [PubMed] [Google Scholar]
- Kanters S, Park JJH, Chan K, Socias ME, Ford N, Forrest JI, … Mills EJ. Interventions to improve adherence to antiretroviral therapy: A systematic review and network meta-analysis. Lancet HIV. 2017;4(1):e31–e40. doi: 10.1016/s2352-3018(16)30206-5. [DOI] [PubMed] [Google Scholar]
- Kassaye SG, Ong’ech J, Sirengo M, Kose J, Matu L, McOdida P, … Machekano R. Cluster-randomized controlled study of SMS text messages for prevention of mother-to-child transmission of HIV in rural Kenya. AIDS Research and Treatment. 2016;2016:1289328. doi: 10.1155/2016/1289328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenya National Bureau of Statistics, Ministry of Health, National AIDS Control Council, Kenya Medical Research Institute, National Council for Population and Development, & Demographic and Health Surveys, Inter City Fund International. Kenya demographic and health survey 2014. 2015 Retrieved from http://dhsprogram.com/pubs/pdf/FR308/FR308.pdf.
- Kulzer JL, Penner JA, Marima R, Oyaro P, Oyanga AO, Shade SB, … Cohen CR. Family model of HIV care and treatment: A retrospective study in Kenya. Journal of the International AIDS Society. 2012;15(1):8. doi: 10.1186/1758-2652-15-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee SH, Nurmatov UB, Nwaru BI, Mukherjee M, Grant L, Pagliari C. Effectiveness of mHealth interventions for maternal, newborn and child health in low- and middle-income countries: Systematic review and meta-analysis. Journal of Global Health. 2016;6(1):010401. doi: 10.7189/jogh.06.010401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lester RT, Ritvo P, Mills EJ, Kariri A, Karanja S, Chung MH, … Plummer FA. Effects of a mobile phone short message service on antiretroviral treatment adherence in Kenya (WelTel Kenya1): A randomised trial. Lancet. 2010;376(9755):1838–1845. doi: 10.1016/s0140-6736(10)61997-6. [DOI] [PubMed] [Google Scholar]
- Lund S, Nielsen BB, Hemed M, Boas IM, Said A, Said K, … Rasch V. Mobile phones improve antenatal care attendance in Zanzibar: A cluster randomized controlled trial. BMC Pregnancy and Childbirth. 2014;14:29. doi: 10.1186/1471-2393-14-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mbuagbaw L, Bonono-Momnougui RC, Thabane L. Considerations in using text messages to improve adherence to highly active antiretroviral therapy: A qualitative study among clients in Yaounde, Cameroon. HIV AIDS. 2012;4:45–50. doi: 10.2147/HIV.S29954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Health & National AIDS Control Council. Kenya AIDS response progress report 2016. 2016 Retrieved from http://nacc.or.ke/wp-content/uploads/2016/11/Kenya-AIDS-Progress-Report_web.pdf.
- Mwapasa V, Pro G, Chinkhumba J, Mukaka M, Kobayashi E, Stuart A, … Eliya M. Mother-infant pair clinic and SMS messaging as innovative strategies for improving access to and retention in eMTCT care and Option B+ in Malawi: A cluster randomized control trial (the PRIME study) Journal of Acquired Immune Deficiency Syndromes. 2014;67(Suppl 2):S120–S124. doi: 10.1097/qai.0000000000000327. [DOI] [PubMed] [Google Scholar]
- Nederhof AJ. Methods of coping with social desirability bias: A review. European Journal of Social Psychology. 1985;15(3):263–280. doi: 10.1002/ejsp.2420150303. [DOI] [Google Scholar]
- Odeny TA, Bukusi EA, Cohen CR, Yuhas K, Camlin CS, McClelland RS. Texting improves testing: A randomized trial of two-way SMS to increase postpartum prevention of mother-to-child transmission retention and infant HIV testing. AIDS. 2014;28(15):2307–2312. doi: 10.1097/QAD.0000000000000409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odeny TA, Newman M, Bukusi EA, McClelland RS, Cohen CR, Camlin CS. Developing content for a mHealth intervention to promote postpartum retention in prevention of mother-to-child HIV transmission programs and early infant diagnosis of HIV: A qualitative study. PloS One. 2014;9(9):e106383. doi: 10.1371/journal.pone.0106383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Philbrick WC. MHEALTH and MNCH: State of the evidence. 2013 Retrieved from http://www.mhealthknowledge.org/sites/default/files/15_un_007_evidencegapreport_digital_aaa.pdf.
- Pop-Eleches C, Thirumurthy H, Habyarimana JP, Zivin JG, Goldstein MP, de Walque D, … Bangsberg DR. Mobile phone technologies improve adherence to antiretroviral treatment in a resource-limited setting: A randomized controlled trial of text message reminders. AIDS. 2011;25(6):825–834. doi: 10.1097/QAD.0b013e32834380c1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen S, Fox MP, Gill CJ. Patient retention in antiretroviral therapy programs in sub-Saharan Africa: A systematic review. PLoS Medicine. 2007;4(10):e298. doi: 10.1371/journal.pmed.0040298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenstock IM. Historical origins of the Health Belief Model. Health Education & Behavior. 1974;2(4):328–335. doi: 10.1177/109019817400200403. [DOI] [Google Scholar]
- Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the Health Belief Model. Health Education Quarterly. 1988;15(2):175–183. doi: 10.1177/109019818801500203. [DOI] [PubMed] [Google Scholar]
- Sellen D, Mbugua S, Webb GA, Kalungu S, Sarange C, Lou W, … Kamau-Mbuthia E. A randomized controlled trial indicates benefits of cell phone based peer counseling to support exclusive breastfeeding in Kenya. Annals of Nutrition and Metabolism. 2013;63(Suppl 1):751. [Google Scholar]
- Smillie K, Van Borek N, Abaki J, Pick N, Maan EJ, Friesen K, … Murray M. A qualitative study investigating the use of a mobile phone short message service designed to improve HIV adherence and retention in care in Canada (WelTel BC1) Journal of the Association of Nurses in AIDS Care. 2014;25(6):614–625. doi: 10.1016/j.jana.2014.01.008. [DOI] [PubMed] [Google Scholar]
- Tenthani L, Haas AD, Tweya H, Jahn A, van Oosterhout JJ, Chimbwandira F, … Phiri S. Retention in care under universal antiretroviral therapy for HIV-infected pregnant and breastfeeding women (‘Option B+’) in Malawi. AIDS. 2014;28(4):589–598. doi: 10.1097/QAD.0000000000000143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turan JM, Bukusi EA, Onono M, Holzemer WL, Miller S, Cohen CR. HIV/AIDS stigma and refusal of HIV testing among pregnant women in rural Kenya: Results from the MAMAS Study. AIDS and Behavior. 2011;15(6):1111–1120. doi: 10.1007/s10461-010-9798-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walcott MM, Hatcher AM, Kwena Z, Turan JM. Facilitating HIV status disclosure for pregnant women and partners in rural Kenya: A qualitative study. BMC Public Health. 2013;13:1115. doi: 10.1186/1471-2458-13-1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware NC, Pisarski EE, Tam M, Wyatt MA, Atukunda E, Musiimenta A, … Haberer JE. The meanings in the messages: How SMS reminders and real-time adherence monitoring improve antiretroviral therapy adherence in rural Uganda. AIDS. 2016;30(8):1287–1294. doi: 10.1097/QAD.0000000000001035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Use of antiretroviral drugs for treating pregnant women and preventing HIV infection in infants. 2012 Retrieved from http://www.who.int/hiv/pub/mtct/programmatic_update2012/en/ [PubMed]
- World Health Organization. Implementation of Option B+ for prevention of mother-to-child transmission of HIV: The Malawi experience. 2014 Retrieved from http://www.who.int/iris/handle/10665/112849.