Abstract
Objectives
To determine the effect of root canal irrigants on the hydrophobicity and adherence of Staphylococcus epidermidis (S. epidermidis) to root canal dentin in vitro.
Materials and Methods
Root dentin blocks (n = 60) were randomly divided into 4 groups based on the irrigation regimen: group 1, saline; group 2, 5.25% sodium hypochlorite (NaOCl); group 3, 5.25% NaOCl followed by 17% ethylenediaminetetraacetic acid (EDTA); group 4, same as group 3 followed by 2% chlorhexidine (CHX). The hydrophobicity of S. epidermidis to root dentin was calculated by cell surface hydrophobicity while the adherence was observed by fluorescence microscopy, and bacteria were quantified using ImageJ software (National Institutes of Health). Statistical analysis of the data was done using Kruskal-Wallis test and Mann-Whitney U test (p = 0.05).
Results
The hydrophobicity and adherence of S. epidermidis to dentin were significantly increased after irrigating with group 3 (NaOCl-EDTA) (p < 0.05), whereas in group 4 (NaOCl-EDTA-CHX) both hydrophobicity and adherence were significantly reduced (p < 0.05).
Conclusions
The adherence of S. epidermidis to dentin was influenced differently by root canal irrigants. Final irrigation with CHX reduces the bacterial adherence and may impact biofilm formation.
Keywords: Adherence, Chlorhexidine, Ethylenediaminetetraacetic acid, Hydrophobicity, Sodium hypochlorite, Staphylococcus epidermidis
INTRODUCTION
Microbial adhesion to a substrate is the first step in biofilm formation [1]. Infections of the root canal system and periradicular tissues are biofilm-mediated, and microbial persistence appears to play an important role in outcome of endodontic treatment [2,3]. Teeth with periradicular periodontitis have been shown to demonstrate the presence of biofilms within the root canal system [4]. For microbial biofilms to persist within the radicular space, its adhesion mechanisms are important and this is influenced by physico-chemical properties of the bacteria as well as the dentin substrate [5]. Interactions between bacteria and the substrate can be specific or non-specific. Non-specific interactions are reversible and include the first stage of bacterial adhesion. Specific interactions result in synthesis of a variety of structural components that help in binding the bacterial cells to the substrate [6,7]. Measures of non-specific interaction which helps in determining the adhesiveness of bacteria to the substrate are cell surface hydrophobicity and cell surface charge of the bacteria [8].
The objective of root canal irrigation is to disrupt the architecture of root canal biofilms, and convert biofilm bacteria to planktonic suspensions so that they can be killed by the antibacterial agents used. The most common irrigation regimen involves the use of a proteolytic agent such as sodium hypochlorite (NaOCl) which is a broad-spectrum antiseptic and also helps in dissolving vital as well as necrotic tissue [9], followed by a decalcifying agent such as ethylenediaminetetraacetic acid (EDTA) which removes the accumulated hard tissue debris [10]. NaOCl results in collagen breakdown, and the subsequent use of a chelating agent such as EDTA removes the encapsulating mineral content to expose naked collagen [9]. Another antiseptic that is used either during instrumentation [11] or as a final rinse [12] is chlorhexidine (CHX). CHX is a bisbiguanide that shows substantivity [13].
Undoubtedly, physico-chemical properties of the dentin substrate are altered during root canal instrumentation and irrigation. This has been demonstrated from the perspective of adhesion of root filling materials [14] as well as bacteria [15]. Using Enterococcus faecalis (E. faecalis) as a test microbe, Kishen et al. [15] demonstrated the influence of irrigant treatment on adhesion of E. faecalis to dentin. Murad et al. [16] showed that Staphylococcus epidermidis (S. epidermidis) was the common prevalent species among persistent endodontic infections [16]. The aim of this study was to evaluate the effect of 2 root canal irrigating regimens (NaOCl-EDTA, NaOCl-EDTA-CHX) on the hydrophobicity and adherence of S. epidermidis to root canal dentin. Saline and NaOCl served as controls. The null hypotheses were 1) there will be no significant difference between the experimental groups in the hydrophobicity and adherence of S. epidermidis, and 2) the irrigation regimens do not differ significantly from the controls in altering the hydrophobicity and adherence of the bacteria.
MATERIALS AND METHODS
Dentin blocks (n = 60) measuring 3 × 3 mm were obtained from freshly extracted human mandibular premolars based on a protocol approved by the International Medical University Joint Committee on Research and Ethics (IMU 321/2015). The dentin blocks were flattened using a polishing machine, washed with deionized water and autoclaved. The dentin blocks were immersed in centrifuge tubes containing irrigating solution. The specimens were randomly divided into 4 groups based on the irrigation regimen (n = 15): group 1, saline; group 2, 5.25% NaOCl for 30 minutes; group 3, 5.25% NaOCl (30 minutes) followed by 17% EDTA (1 minute); group 4, same as group 3 followed by 2% CHX for 30 minutes. The saline was used between different irrigating solutions. The volume of all the irrigants was standardized to 10 mL.
S. epidermidis culture and inoculum preparations
S. epidermidis was grown in Trypticase Soy Agar (TSA) medium. A single colony of isolated bacteria from 24–48 hours culture was selected and inoculated in Trypticase Soy Broth (TSB). This was allowed to grow overnight (14 hours) at 37°C. Bacterial cells were then harvested from this and dispersed in phosphate buffered saline (PBS) at concentrations of up to 108 cells/mL (0.5 McFarland standards).
All the dentin blocks were inoculated with 1 mL of bacterial suspension in a 24 well plate (Eppendorf, Hamburg, Germany) and incubated at 37°C for 30 minutes in an orbital rotary incubator. The bacterial suspension was discarded and sterile PBS was used to remove the loosely bound bacteria on the dentin blocks. Following this, the blocks were sonicated (Labsonic P, Braun Biotech International, Goettingen, Germany) in PBS at 37 kHz for 5 minutes, to dislodge the biofilm. This process effectively dislodged loosely bound bacteria and the biofilm.
Analysis of cell surface hydrophobicity
The collected bacterial suspension was used to evaluate the hydrophobicity of the bacteria based on a previously published method [17]. Briefly, the adhesion of bacteria to the hydrocarbon, i.e., xylene, was used to determine the relative cellular surface hydrophobicity (n = 40). Optical density (OD) of the bacterial cell suspension was adjusted to 1 OD (initial) at 520 nm by using PBS as a matched control blank in a spectrophotometer. Xylene was then added to the bacterial suspension in the tubes, and equilibration was done by maintaining the suspension at 37°C for 10 minutes. The contents in the tubes were mixed by vortexing for 30 seconds and then incubated at 37°C for 30 minutes. After incubation, 2 layers were observed and the absorbance intensity of the lower aqueous layer was determined at 520 nm OD (final) [18]. The percentage of hydrophobicity was calculated by the following formula:
| Cell surface hydrophobicity = (1 − OD final/OD initial) × 100 |
Analysis of bacterial adherence
Following sonication of the dentin blocks (n = 20) as mentioned earlier, the blocks were stained with acridine orange (AO) and observed under a fluorescent microscope (Eclipse Ti-U, Nikon, Tokyo, Japan) [17]. AO (50 mg) was dissolved in 10 mL of distilled water to obtain a 0.5% staining solution (AO stock) and stored in a refrigerator. One mL of AO stock solution was then added with 0.5 mL of glacial acetic acid, and made up to 50 mL using distilled water to obtain the working solution. The pH of the working solution was maintained at 3.0, and AO concentration was 0.01%. The dentin blocks were stained with the AO solution for 15 minutes and counterstained with 0.1% crystal violet (Sigma, St. Louis, MO, USA) solution for 3–5 minutes and viewed under high power lens in a fluorescent microscope. Crystal violet counterstain helps avoid background fluorescence. Three random areas were chosen from the 5 different dentin blocks by an independent observer who was blinded to the experimental groups. The bacterial count was measured by using the image captured by the ImageJ software (National Institutes of Health, Bethesda, MD, USA).
The collected data were analyzed (IBM SPSS statistics software, version 23.0, IBM Corp., Armonk, NY, USA) using Kruskal-Wallis test followed by Mann-Whitney U test with the alpha error set at p = 0.05.
RESULTS
Group 4 (NaOCl-EDTA-CHX) showed the least hydrophobicity (11.4% ± 1.77%), while group 3 (NaOCl-EDTA) showed the highest hydrophobicity percentage values (89.8% ± 7.1%) (Table 1). Analysis of the hydrophobicity (percentage) of S. epidermidis to root dentin after irrigation with different protocols revealed that there was a significant difference between the experimental groups (groups 3 and 4) in hydrophobicity values (p < 0.01). There was no statistically significant difference between saline (group 1) and NaOCl-EDTA (group 3).
Table 1. Mean value of percentage hydrophobicity of S. epidermidis to dentin treated with various irrigating regimens.
| Group | Irrigating regimen | Percentage hydrophobicity |
|---|---|---|
| 1 | Saline | 83.8 ± 6.9a |
| 2 | NaOCl | 70.7 ± 5.5b |
| 3 | NaOCl-EDTA | 89.8 ± 7.2a |
| 4 | NaOCl-EDTA-CHX | 11.4 ± 1.8c |
The values are shown as mean ± standard deviation. Groups with same superscript alphabets had no significant difference between them.
NaOCl, sodium hypochlorite; EDTA, ethylenediaminetetraacetic acid; CHX, chlorhexidine.
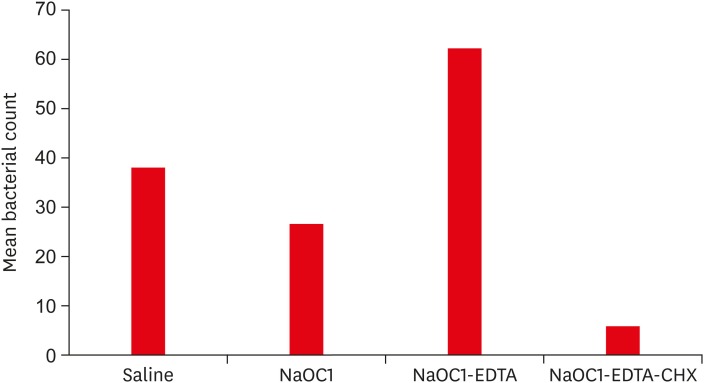
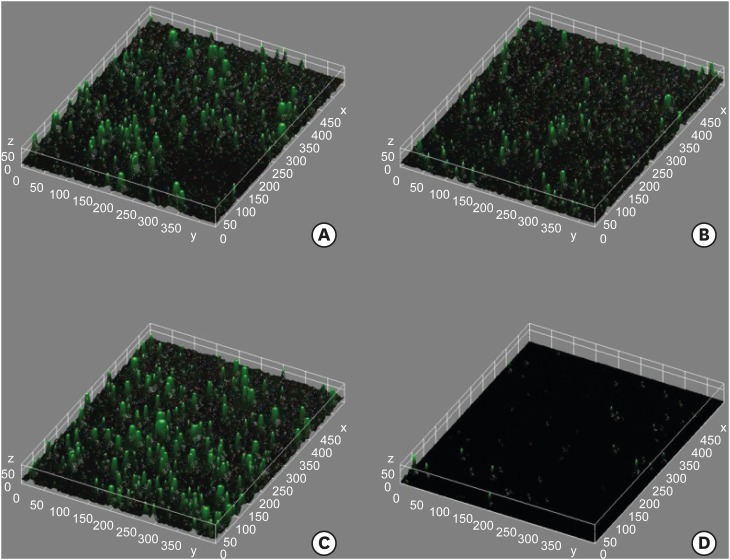
The mean adherence values after irrigating regimens is represented in Figure 1. The fluorescence microscopic images showing adherence of S. epidermidis to root dentin blocks treated with different irrigating regimens have been presented in Figure 2. The irrigating regimens differed significantly in the adherence of S. epidermidis to dentin (p < 0.01). Group 4 (NaOCl-EDTA-CHX) showed significantly lesser adherence values compared to groups 1, 2, and 3. Group 3 (NaOCl-EDTA) showed the highest values for adherence of bacteria (p < 0.05).
Figure 1.
Mean value of adherence of S. epidermidis to dentin treated with various irrigating regimens.
NaOCl, sodium hypochlorite; EDTA, ethylenediaminetetraacetic acid; CHX, chlorhexidine.
Figure 2.
Fluorescence microscopic images showing adherence of S. epidermidis to dentin treated with (A) Saline, (B) NaOCl, (C) NaOCl-EDTA, and (D) NaOCl-EDTA-CHX.
NaOCl, sodium hypochlorite; EDTA, ethylenediaminetetraacetic acid; CHX, chlorhexidine.
DISCUSSION
While several bacteria remain to be cultivated and identified from the root canal system [19], it has been widely reported that E. faecalis is important bacteria in root canal treatment failure [20]. Interestingly, E. faecalis is not a frequently isolated organism in primary endodontic infections. This may result in a speculation that the E. faecalis cells that persist after root canal treatment may demonstrate increased adhesion to the dentin that undergoes physico-chemical alterations after chemomechanical preparation. However, it has been shown that the forces of adhesion of E. faecalis to NaOCl treated or untreated root canal dentin are not significantly different [15]. Root canal biofilms are composed of more than one species of microorganism. While it is speculated that the dynamics of interaction between different microbial species plays an important role in the pathogenesis of pulpal and periradicular diseases, it may also play a vital role in failure of root canal treatment [21]. Hence, the adhesion of other common persisting bacteria needs to be evaluated. This study evaluated the adherence of S. epidermidis which has been shown to be commonly isolated bacteria in persistent infections [16].
The endodontic literature is consistent in reporting that NaOCl is able to disrupt microbial biofilms [12,22]. The results of our study showed that while NaOCl was able to reduce the bacterial adherence to dentin, it was less efficient than the NaOCl-EDTA-CHX protocol in reducing the adherence of bacteria. These results are interesting as Rosen et al. [23] recently reported that NaOCl may contribute to persistence of E. faecalis by inducing a viable but non-culturable state of biofilm cells. Consequently, it may be speculated that using NaOCl alone may be insufficient to disrupt complex multispecies biofilms. The irrigation protocol (NaOCl followed by EDTA) showed the highest percentage hydrophobicity and adherence values compared to saline group. This could be due to the demineralization of dentin by EDTA resulting in exposure of collagen and reduction in the surface free energy of root dentin [24]. EDTA brings about a demineralization gradient, and removes Ca+ and Mg+ and to a moderate extent PO2− and PO3− from the dentin [25]. A demineralization zone of 20 to 30 µm has been observed after exposing dentin to 15% EDTA for 5 minutes [15,26]. It has been reported that 3.8% of the originally applied EDTA volume remains within the root canal system after instrumentation and irrigation [27]. Such remaining traces of EDTA may continue to demineralize dentin and expose further dentinal collagen [15]. The results of this study are in agreement with those of Kishen et al. [15] in that a final rinse of EDTA increased the adherence of E. faecalis. However, the aforementioned study reported that there was a significantly reduced bacterial adherence between the NaOCl-EDTA treated group and untreated group. In contrast, our study did not have an untreated control, rather saline treatment was one of the controls. The present study showed that there was no significant difference in the bacterial adherence of the saline treated and NaOCl-EDTA treated groups. This may be due to the influence of the inorganic ions in saline, on the electrostatic attraction between bacteria and the dentin substrate during the initial stages of biofilm adhesion [28].
This difference could also be attributed to the bacterium that was studied. This is also interesting from the perspective of how the adherence of S. epidermidis may influence the recalcitrance of E. faecalis within root canal systems. Adhesion of S. epidermidis cells in biofilms is mediated by polysaccharide intercellular adhesin, a homoglycan composed of β-1,6-linked 2-deoxy-2-amino-D-glucopyranosyl residues [29]. It has been reported that this could be influenced by enhanced expression of atle, aap, agr, ica [30], and SdrF genes [31]. It may be speculated that the irrigating protocols have an impact on the gene expression influencing adhesion. It was beyond the scope of this work to determine if such an influence existed or if adherence of S. epidermidis influenced the persistence of other bacteria such as E. faecalis. These aspects need further analysis.
The use of collagen cross-linking agents may be useful in this regard to reduce the adherence of bacteria. Studies have shown that photodynamic therapy with collagen cross linkers such as chitosan with rose-bengal and curcumin demonstrate antibiofilm activity [32,33]. Dentin treated with cationic nanoparticulates has shown reduced adhesion of E. faecalis [34]. This maybe an advisable clinical strategy based on the different influence of irrigating protocols on the adherence of different bacteria. CHX as a final irrigant reduced the hydrophobicity and adherence of S. epidermidis to dentin. The cationic nature of CHX allows its bonding to the exposed collagen, and this in addition to the substantivity may have contributed to the decreased adherence of bacteria. Such a finding is in accordance with that of Kishen et al. [15]. The positively charged molecules released from CHX bind to the bacteria causing membrane damage leading to cell lysis [35]. Yang et al. [36] showed that when CHX was used as intracanal medicament, it reduces the adherence capability of bacteria. The present study did not use a rinse of distilled water after the use of final irrigating agents. It is not known if using such a water rinse may help remove traces of chemical agents and negatively influence bacterial adhesion, which further needs to be investigated. Future studies should evaluate how adhesion of some bacteria may influence the persistence of other microbes in the biofilm communities.
CONCLUSIONS
The use of CHX as a final irrigant reduces the adherence of S. epidermidis to root canal dentin, while the use of EDTA as a final rinse increased the adherence.
Footnotes
Funding: This work was supported by the International Medical University Grant (IMU 321/2015).
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
- Conceptualization: Nagendrababu V, Davamani F.
- Data curation: Nagendrababu V, Sheriff Sultan O, Neelakantan P, Davamani F.
- Formal analysis: Nagendrababu V, Sheriff Sultan O, Chitra E, Davamani F.
- Funding acquisition: Nagendrababu V, Davamani F.
- Investigation: Sheriff Sultan O, Kannathasan S, Patel AS, Chitra E, Davamani F.
- Methodology: Nagendrababu V, Kannathasan S, Patel AS, Davamani F.
- Project administration: Nagendrababu V, Davamani F.
- Resources: Nagendrababu V, Davamani F.
- Software: Sheriff Sultan O, Chitra E, Davamani F.
- Supervision: Nagendrababu V, Davamani F.
- Validation: Nagendrababu V, Neelakantan P.
- Visualization: Sheriff Sultan O, Chitra E, Davamani F.
- Writing - original draft: Nagendrababu V, Neelakantan P, Davamani F.
- Writing - review & editing: Nagendrababu V, Sheriff Sultan O, Chitra E, Neelakantan P, Davamani F.
References
- 1.Donlan RM, Costerton JW. Biofilms: survival mechanisms of clinically relevant microorganisms. Clin Microbiol Rev. 2002;15:167–193. doi: 10.1128/CMR.15.2.167-193.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fabricius L, Dahlén G, Sundqvist G, Happonen RP, Möller AJ. Influence of residual bacteria on periapical tissue healing after chemomechanical treatment and root filling of experimentally infected monkey teeth. Eur J Oral Sci. 2006;114:278–285. doi: 10.1111/j.1600-0722.2006.00380.x. [DOI] [PubMed] [Google Scholar]
- 3.Sjögren U, Figdor D, Persson S, Sundqvist G. Influence of infection at the time of root filling on the outcome of endodontic treatment of teeth with apical periodontitis. Int Endod J. 1997;30:297–306. doi: 10.1046/j.1365-2591.1997.00092.x. [DOI] [PubMed] [Google Scholar]
- 4.Ricucci D, Siqueira JF., Jr Biofilms and apical periodontitis: study of prevalence and association with clinical and histopathologic findings. J Endod. 2010;36:1277–1288. doi: 10.1016/j.joen.2010.04.007. [DOI] [PubMed] [Google Scholar]
- 5.Stewart PS, Costerton JW. Antibiotic resistance of bacteria in biofilms. Lancet. 2001;358:135–138. doi: 10.1016/s0140-6736(01)05321-1. [DOI] [PubMed] [Google Scholar]
- 6.Bos R, van der Mei HC, Busscher HJ. Physico-chemistry of initial microbial adhesive interactions--its mechanisms and methods for study. FEMS Microbiol Rev. 1999;23:179–230. doi: 10.1111/j.1574-6976.1999.tb00396.x. [DOI] [PubMed] [Google Scholar]
- 7.Waar K, van der Mei HC, Harmsen HJ, Degener JE, Busscher HJ. Enterococcus faecalis surface proteins determine its adhesion mechanism to bile drain materials. Microbiology. 2002;148:1863–1870. doi: 10.1099/00221287-148-6-1863. [DOI] [PubMed] [Google Scholar]
- 8.Ascencio F, Johansson G, Wadström T. Cell-surface charge and cell-surface hydrophobicity of collagen-binding Aeromonas and Vibrio strains. Arch Microbiol. 1995;164:223–230. doi: 10.1007/BF02529975. [DOI] [PubMed] [Google Scholar]
- 9.Zhang K, Kim YK, Cadenaro M, Bryan TE, Sidow SJ, Loushine RJ, Ling JQ, Pashley DH, Tay FR. Effects of different exposure times and concentrations of sodium hypochlorite/ethylenediaminetetraacetic acid on the structural integrity of mineralized dentin. J Endod. 2010;36:105–109. doi: 10.1016/j.joen.2009.10.020. [DOI] [PubMed] [Google Scholar]
- 10.Wu L, Mu Y, Deng X, Zhang S, Zhou D. Comparison of the effect of four decalcifying agents combined with 60°C 3% sodium hypochlorite on smear layer removal. J Endod. 2012;38:381–384. doi: 10.1016/j.joen.2011.11.013. [DOI] [PubMed] [Google Scholar]
- 11.Siqueira JF, Jr, Paiva SS, Rôças IN. Reduction in the cultivable bacterial populations in infected root canals by a chlorhexidine-based antimicrobial protocol. J Endod. 2007;33:541–547. doi: 10.1016/j.joen.2007.01.008. [DOI] [PubMed] [Google Scholar]
- 12.Zehnder M. Root canal irrigants. J Endod. 2006;32:389–398. doi: 10.1016/j.joen.2005.09.014. [DOI] [PubMed] [Google Scholar]
- 13.Böttcher DE, Sehnem NT, Montagner F, Fatturi Parolo CC, Grecca FS. Evaluation of the effect of Enterococcus faecalis biofilm on the 2% chlorhexidine substantivity: an in vitro study. J Endod. 2015;41:1364–1370. doi: 10.1016/j.joen.2015.04.016. [DOI] [PubMed] [Google Scholar]
- 14.Neelakantan P, Varughese AA, Sharma S, Subbarao CV, Zehnder M, De-Deus G. Continuous chelation irrigation improves the adhesion of epoxy resin-based root canal sealer to root dentine. Int Endod J. 2012;45:1097–1102. doi: 10.1111/j.1365-2591.2012.02073.x. [DOI] [PubMed] [Google Scholar]
- 15.Kishen A, Sum CP, Mathew S, Lim CT. Influence of irrigation regimens on the adherence of Enterococcus faecalis to root canal dentin. J Endod. 2008;34:850–854. doi: 10.1016/j.joen.2008.04.006. [DOI] [PubMed] [Google Scholar]
- 16.Murad CF, Sassone LM, Faveri M, Hirata R, Jr, Figueiredo L, Feres M. Microbial diversity in persistent root canal infections investigated by checkerboard DNA-DNA hybridization. J Endod. 2014;40:899–906. doi: 10.1016/j.joen.2014.02.010. [DOI] [PubMed] [Google Scholar]
- 17.Rosenberg M, Gutnick D, Rosenberg E. Adherence of bacteria to hydrocarbons: a simple method for measuring cell-surface hydrophobicity. FEMS Microbiol Lett. 1980;9:29–33. [Google Scholar]
- 18.George S, Kishen A. Effect of tissue fluids on hydrophobicity and adherence of Enterococcus faecalis to dentin. J Endod. 2007;33:1421–1425. doi: 10.1016/j.joen.2007.07.035. [DOI] [PubMed] [Google Scholar]
- 19.Siqueira JF, Jr, Rôças IN. As-yet-uncultivated oral bacteria: breadth and association with oral and extra-oral diseases. J Oral Microbiol. 2013;5:21077. doi: 10.3402/jom.v5i0.21077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Love RM. Enterococcus faecalis--a mechanism for its role in endodontic failure. Int Endod J. 2001;34:399–405. doi: 10.1046/j.1365-2591.2001.00437.x. [DOI] [PubMed] [Google Scholar]
- 21.Zehnder M, Belibasakis GN. On the dynamics of root canal infections-what we understand and what we don't. Virulence. 2015;6:216–222. doi: 10.4161/21505594.2014.984567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ordinola-Zapata R, Bramante CM, Aprecio RM, Handysides R, Jaramillo DE. Biofilm removal by 6% sodium hypochlorite activated by different irrigation techniques. Int Endod J. 2014;47:659–666. doi: 10.1111/iej.12202. [DOI] [PubMed] [Google Scholar]
- 23.Rosen E, Tsesis I, Elbahary S, Storzi N, Kolodkin-Gal I. Eradication of Enterococcus faecalis biofilms on human dentin. Front Microbiol. 2016;7:2055. doi: 10.3389/fmicb.2016.02055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dogan Buzoglu H, Calt S, Gümüsderelioglu M. Evaluation of the surface free energy on root canal dentine walls treated with chelating agents and NaOCl. Int Endod J. 2007;40:18–24. doi: 10.1111/j.1365-2591.2006.01169.x. [DOI] [PubMed] [Google Scholar]
- 25.Kolosowski KP, Sodhi RN, Kishen A, Basrani BR. Qualitative time-of-flight secondary ion mass spectrometry analysis of root dentin irrigated with sodium hypochlorite, EDTA, or Chlorhexidine. J Endod. 2015;41:1672–1677. doi: 10.1016/j.joen.2015.06.010. [DOI] [PubMed] [Google Scholar]
- 26.Marshall GW, Jr, Balooch M, Kinney JH, Marshall SJ. Atomic force microscopy of conditioning agents on dentin. J Biomed Mater Res. 1995;29:1381–1387. doi: 10.1002/jbm.820291109. [DOI] [PubMed] [Google Scholar]
- 27.Zurbriggen T, del Rio CE, Brady JM. Postdebridement retention of endodontic reagents: a quantitative measurement with radioactive isotope. J Endod. 1975;1:298–299. doi: 10.1016/S0099-2399(75)80137-3. [DOI] [PubMed] [Google Scholar]
- 28.Garrett TR, Bhakoo M, Zhang Z. Bacterial adhesion and biofilms on surfaces. Prog Nat Sci. 2008;18:1049–1056. [Google Scholar]
- 29.Mack D, Fischer W, Krokotsch A, Leopold K, Hartmann R, Egge H, Laufs R. The intercellular adhesin involved in biofilm accumulation of Staphylococcus epidermidis is a linear β-1,6-linked glucosaminoglycan: purification and structural analysis. J Bacteriol. 1996;178:175–183. doi: 10.1128/jb.178.1.175-183.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Patel JD, Colton E, Ebert M, Anderson JM. Gene expression during S. epidermidis biofilm formation on biomaterials. J Biomed Mater Res A. 2012;100:2863–2869. doi: 10.1002/jbm.a.34221. [DOI] [PubMed] [Google Scholar]
- 31.Trivedi S, Uhlemann AC, Herman-Bausier P, Sullivan SB, Sowash MG, Flores EY, Khan SD, Dufrêne YF, Lowy FD. The surface protein SdrF mediates Staphylococcus epidermidis adherence to keratin. J Infect Dis. 2017;215:1846–1854. doi: 10.1093/infdis/jix213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shrestha A, Hamblin MR, Kishen A. Photoactivated rose bengal functionalized chitosan nanoparticles produce antibacterial/biofilm activity and stabilize dentin-collagen. Nanomedicine (Lond) 2014;10:491–501. doi: 10.1016/j.nano.2013.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Devaraj S, Jagannathan N, Neelakantan P. Antibiofilm efficacy of photoactivated curcumin, triple and double antibiotic paste, 2% chlorhexidine and calcium hydroxide against Enterococcus fecalis in vitro . Sci Rep. 2016;6:24797. doi: 10.1038/srep24797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kishen A, Shi Z, Shrestha A, Neoh KG. An investigation on the antibacterial and antibiofilm efficacy of cationic nanoparticulates for root canal disinfection. J Endod. 2008;34:1515–1520. doi: 10.1016/j.joen.2008.08.035. [DOI] [PubMed] [Google Scholar]
- 35.Mohammadi Z, Abbott PV. The properties and applications of chlorhexidine in endodontics. Int Endod J. 2009;42:288–302. doi: 10.1111/j.1365-2591.2008.01540.x. [DOI] [PubMed] [Google Scholar]
- 36.Yang SE, Cha JH, Kim ES, Kum KY, Lee CY, Jung IY. Effect of smear layer and chlorhexidine treatment on the adhesion of Enterococcus faecalis to bovine dentin. J Endod. 2006;32:663–667. doi: 10.1016/j.joen.2005.12.002. [DOI] [PubMed] [Google Scholar]