Abstract
Dental erosion is frequently overlooked in clinical practice. The management of erosion-induced damage to the dentition is often delayed, such that extensive occlusal rehabilitation is required. These cases can be diagnosed by a careful clinical examination and a thorough review of the patient's medical history and/or lifestyle habits. This case report presents the diagnosis, categorization, and management of a case of gastro-esophageal reflux disease-induced palatal erosion of the maxillary teeth. The early management of such cases is of utmost importance to delay or prevent the progression of damage both to the dentition and to occlusal stability. Non-invasive adhesively bonded restorations aid in achieving this goal.
Keywords: Composite resins, Conservative treatment, Dental bonding, Dental wear, Minimally invasive dentistry, Tooth erosion
INTRODUCTION
Dental erosion is a major cause of the loss of mineralized tooth structure. Based on etiology, erosion is classified as intrinsic or extrinsic, with each type having different clinical presentations. Intrinsic erosion results from the regurgitation of stomach contents into the esophagus, oropharynx, and oral cavity, and is associated with diseases such as bulimia and gastro-esophageal reflux disorder (GERD). These regurgitated contents have a pH of less than 2, which is below the critical pH of enamel (5.5) and dentin (6.7). Intrinsic erosive lesions appear on the palatal surfaces of the maxillary teeth and the occlusal surfaces of the mandibular posterior teeth [1,2].
While dental caries lead clinicians to intervene immediately, in cases of erosion, many clinicians postpone dental treatment until the patient is older, even though literature confirms that direct clinical observation is an unreliable method for monitoring the rate of tooth wear [3]. Additionally, clinicians are reluctant to propose extensive dental rehabilitation in asymptomatic patients. This approach is problematic, as these patients will eventually need complex restorative treatment. The debate over whether it is preferable to start earlier with less invasive rehabilitation or later with a highly aggressive but eventually more resilient rehabilitation is still open. This is a crucial issue because the incidence of GERD in modern society is increasing [1].
CASE REPORT
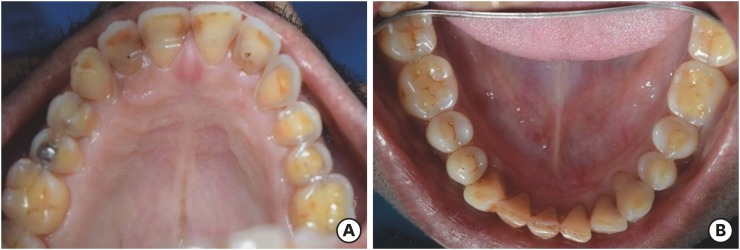
A 46-year-old male patient reported to the outpatient Department of Conservative Dentistry and Endodontics with the chief complaint of pain in the upper left back tooth for 3 weeks. The pain was due to food lodgment. The patient's medical history revealed that he had suffered from frequent episodes of vomiting and stomach upset for a period of 8 months, 1 year ago. Examination of the patient's medical file revealed that he had been diagnosed with gastro-esophageal reflux disease (GERD) and was currently under medication (Aciloc-RD 20, Cadila Pharmaceuticals, Ahmedabad, India) for the same, and had not reported episodes of vomiting for 4 months. This medication is a proton pump inhibitor with the generic name of omeprazole. An oral examination revealed a class II mesio-occlusal carious lesion on tooth #25 (World Dental Federation system). Additionally, the loss of enamel and a shiny appearance of the dentin on the palatal surfaces of the maxillary teeth (teeth #11–17 and teeth #21–27) were noted (Figure 1A). A similar appearance was seen on the occlusal surfaces of the mandibular posterior teeth (teeth #34–37 and teeth #44–47, Figure 1B).
Figure 1.
Pre-operative. (A and B) The pre-operative status of the dentition reveals erosion of the palatal surfaces of the maxillary teeth and the occlusal surfaces of the mandibular teeth.
All teeth responded normally to pulp sensibility tests (cold test and electric pulp test [EPT]). Based on the clinical findings, a diagnosis of class II dental erosion induced by GERD was made. Class II erosion was defined according to the anterior clinical erosive (ACE) classification described by Vailati and Belser [2] as representing dentin exposure on the palatal aspect (contact areas) with no damage to the incisal edges. The vertical dimension at occlusion (VDO) remained unchanged, based on the measurement of the free-way space (the vertical dimension at rest minus the VDO).
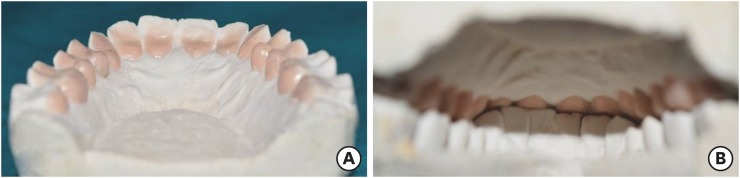
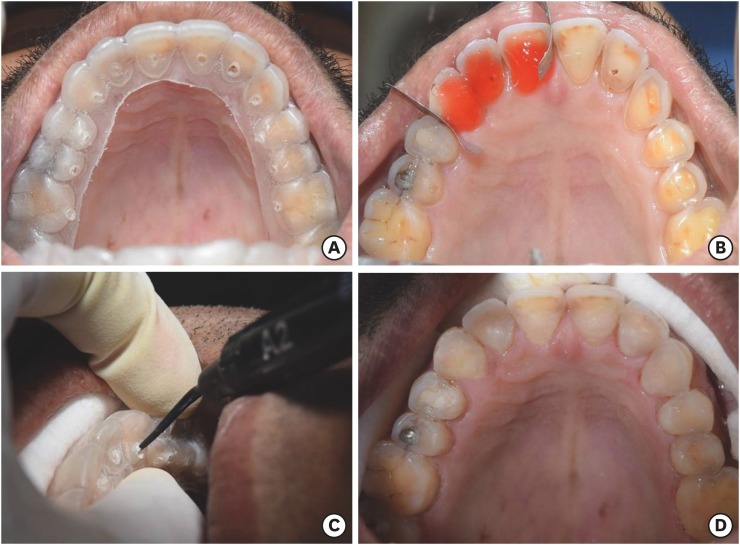
The carious lesion on tooth #25 was restored. The patient was informed of the treatment plan of palatal composite veneering for the erosion-induced damage, as per the ACE classification. Alginate impressions were taken of both arches, and study models were poured. A wax-up of the palatal surfaces was done on the mounted casts (Figure 2A and 2B). An alginate impression was taken of the wax-up, and poured. On the latter master cast, a vacuum-forming soft splint matrix (0.9 mm thick Sof-Tray Sheets, Ultradent Products, Inc., South Jordan, UT, USA) was adapted (Figure 3A). Holes were drilled on the palatal surfaces of the matrix to enable the injection of flowable composite (Figure 3B).
Figure 2.
Wax-up. (A and B) Wax-up was done to build up the cingulum and functional cusps.
Figure 3.
Fabrication of splint. (A and B) A vacuum-forming splint matrix was adapted and trimmed.
After try-in of the matrix (Figure 4A), the teeth were etched in groups (Figure 4B), and bonding agent was applied (Adper Single Bond 2, 3M ESPE, Bangalore, KA, India), air-thinned, and cured. Following placement of the matrix on the maxillary arch, flowable composite resin (G-aenial Universal Flo, GC America, Alsip, IL, USA, shade A2) was injected (Figure 4C) and light-cured. The occlusion was checked by instructing the patient to bite in maximum intercuspation (static occlusion), and guiding the patient in mandibular lateral excursions (dynamic occlusion). The high points were removed. All restorations were finished and polished (SofLex contouring and polishing discs, 3M ESPE) (Figure 4D).
Figure 4.
Restorative protocol. (A) Oral try-in of the splint matrix. (B) Acid etching of the teeth in segments. (C) After the bonding protocol, flowable composite was injected. (D) Composite restorations were finished and polished.
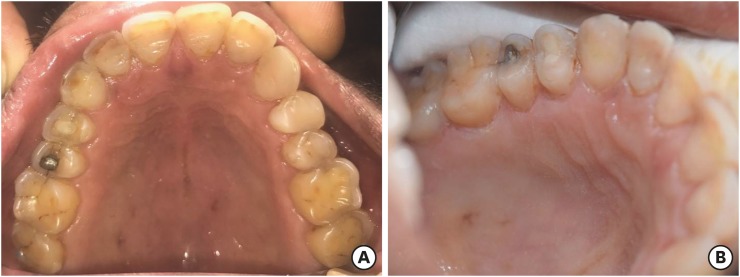
The follow-up at 13 months revealed satisfactory retention, marginal adaptation, surface texture, and anatomic form of the composite restorations (Figure 5A). All teeth responded to pulp sensibility tests (cold test and EPT). Discolored margins were evident at the gingival area (Figure 5B), and these restorations were finished and polished.
Figure 5.
Follow-up at 13 months. (A) An occlusal view reveals satisfactory restorations. (B) Discolored margins were evident.
DISCUSSION
The signs of dental erosion that may be clearly evident at an early stage include a ‘glossy’ (smooth, glazed) enamel, yellowing of the teeth from the underlying dentin, increased incisal translucency, and cupping of the occlusal surfaces. Patients may be asymptomatic. GERD is an intrinsic cause of tooth erosion, and leads to the loss of enamel and dentin. This tooth structure loss leads to instability of the occlusion as teeth passively erupt (alveolar compensation) to maintain occlusion [5]. Despite losing crown height, teeth maintain their occlusal contact, which may lead to problems for their reconstruction because there is not enough space for the restorative material [6].
Vailati and Belser [2] proposed the ACE classification of erosion based on treatment needs. This particular case was classified as ACE class II (dentin exposure on the palatal aspect, i.e., contact areas, with no damage to the incisal edges). The treatment protocol recommended by the authors is to use direct or indirect palatal composites. In the management of acid erosion, direct composite has been proposed as a reversible restorative option [7]. It has been used as a cost-effective strategy for treating erosive wear in patients suffering from GERD [8,9,10]. Initial restorative treatments should be conservative, using adhesive materials. Reconstructive restorative treatments should be adapted to the tooth, and not vice versa [11].
Teeth affected by erosion exhibit sclerotic dentin [12]. The resin bond strength to non-carious sclerotic dentin is lower than to normal dentin due to tubule occlusion by mineral salts, preventing resin tag formation [13]. Researchers have suggested that the tooth surface be roughened prior to bonding. Ogata et al. [14] demonstrated that restorations placed on diamond bur-roughened lesions showed no difference in retention when compared to non-roughened lesions after a 2-year clinical examination period. Van Dijken [15] investigated the durability of 3 simplified adhesive systems in cervical abrasion/erosion lesions with dentin involvement. The loss rates of the materials in sclerotic versus non-sclerotic lesions were not significantly different.
In this clinical case, a fifth-generation total-etch bonding system (Adper Single Bond 2) was used due to the presence of an enamel margin at the periphery of the erosive lesions despite dentin exposure. According to Briggs et al. [16], this rim of enamel (‘gingival ring’) present at the gingival margins is retained even in severely eroded teeth. This enamel rim improves the predictability of resin bonding to hard dental tissues. This gingival ring of enamel is thought to exist because of the neutralizing effect of gingival crevicular fluid, as well as the presence of plaque at the gingival margin that acts as a barrier to the diffusion of erosive acids.
Although under acidic conditions all dental restorative materials show degradation over time (surface roughness, decrease of surface hardness, substance loss, etc.), ceramic and composite materials show good durability [11]. In this case report, a nanohybrid flowable composite (G-aenial Universal Flo) was used for the direct restorations. This product is compatible with all other standard bonding agents [17]. An in vitro study demonstrated that a thin coating of flowable composite resin (150 μm thick) could provide long-term protection against erosive/abrasive tooth wear [18]. The wear and mechanical properties of nanohybrid flowable resin composites are comparable to those of universal resin composites [19].
In the current case, marginal discoloration at the gingival margins was noted at the 13-month follow-up visit. Although stains accumulate more prominently near the gingival margins of teeth, it is also true that well-polished dental restorations rarely pick up stains [5]. In retrospect, the placement of retraction cords would have further facilitated the polishing procedure at the gingival margins of the composite restorations.
Indirect composite or ceramic veneers are a valid treatment option. The patient chose direct composite veneers due to concerns about the high laboratory cost and the desire to undergo a non-invasive treatment. The indirect technique may require the removal of hard tissue undercuts [16]. Even though the use of matrix splints for constructing the direct composite veneers requires a second dental visit and a minor laboratory procedure, it is an easier alternative to free-hand composite build-up, especially when erosive lesions involve the entire arch [20,21].
Holes were drilled into the matrix splint to enable the injection of the flowable composite and the extrusion of the excess. A valid alternative modality to the current protocol might be to place composite resin on the tooth surface and to press it with a splint to allow composite resin to extrude through the hole. However, the operator may be uncertain whether sufficient pressure is generated within each tooth segment of the flexible splint to ensure effective composite flow without voids. In the current injection technique, the operator was assured of the absence of dead space between the splint and tooth due to the transparency of the splint, and also by ensuring that the syringe tip was not retracted until the excess composite had extruded from the hole.
Direct composite veneers are a cost-effective and reversible treatment modality. In this particular case, an intervention was performed before there was a loss of the vertical dimensions or dentinal hypersensitivity developed, thus preventing the need for complex occlusal rehabilitation procedures.
CONCLUSIONS
Non-carious lesions such as erosion are overlooked in clinical practice. Early recognition, diagnosis, and treatment can eliminate the need for further complex treatment procedures involving occlusal rehabilitation.
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
- Conceptualization: Sood A.
- Data curation: Deepak BS.
- Formal analysis: Niranjan NT.
- Investigation: Chockattu SJ.
- Methodology: Sood A.
- Project administration: Jayasheel A.
- Resources: Niranjan NT.
- Software: Chockattu SJ.
- Supervision: Jayasheel A.
- Validation: Goud MK.
- Writing - original draft: Chockattu SJ.
- Writing - review & editing: Deepak BS.
References
- 1.Ahmed SN, Donovan TE, Swift EJ., Jr Dental erosion: the unrecognized epidemic. J Esthet Restor Dent. 2015;27:119–121. doi: 10.1111/jerd.12169. [DOI] [PubMed] [Google Scholar]
- 2.Vailati F, Belser UC. Classification and treatment of the anterior maxillary dentition affected by dental erosion: the ACE classification. Int J Periodontics Restorative Dent. 2010;30:559–571. [PubMed] [Google Scholar]
- 3.Lussi A, Jaeggi T. Dental erosion: diagnosis, risk assessment, prevention, treatment. London: Quintessence Publishing; 2011. pp. 1–132. [Google Scholar]
- 4.Bartlett D, Ganss C, Lussi A. Basic Erosive Wear Examination (BEWE): a new scoring system for scientific and clinical needs. Clin Oral Investig. 2008;12(Supplement 1):S65–S68. doi: 10.1007/s00784-007-0181-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Newman MG, Takei HH, Carranza FA. Carranza's clinical periodontology. 9th ed. Philadelphia (PA): W.B. Saunders Co.; 2002. pp. 31–32.pp. 187–188.pp. 670 [Google Scholar]
- 6.Dahl BL, Krogstad O. The effect of a partial bite raising splint on the occlusal face height. An X-ray cephalometric study in human adults. Acta Odontol Scand. 1982;40:17–24. doi: 10.3109/00016358209019805. [DOI] [PubMed] [Google Scholar]
- 7.Milosevic A, Burnside G. The survival of direct composite restorations in the management of severe tooth wear including attrition and erosion: a prospective 8-year study. J Dent. 2016;44:13–19. doi: 10.1016/j.jdent.2015.10.015. [DOI] [PubMed] [Google Scholar]
- 8.Milosevic A. Acid erosion: an increasingly relevant dental problem. Risk factors, management and restoration. Prim Dent J. 2017;6:37–45. doi: 10.1177/205016841700600105. [DOI] [PubMed] [Google Scholar]
- 9.Metz MJ, Stapleton BM, Harris BT, Lin WS. A cost-effective treatment for severe generalized erosion and loss of vertical dimension of occlusion: laboratory-fabricated composite resin restorations. Gen Dent. 2015;63:e12–e17. [PubMed] [Google Scholar]
- 10.Sethi S. A clinical case involving severe erosion of the maxillary anterior teeth restored with direct composite resin restorations. Int J Esthet Dent. 2016;11:281–286. [PubMed] [Google Scholar]
- 11.Jaeggi T, Grüninger A, Lussi A. Restorative therapy of erosion. In: Lussi A, editor. Dental erosion: from diagnosis to therapy. Basel: Karger; 2006. Chapter 13. [Google Scholar]
- 12.Stanley HR, Pereira JC, Spiegel E, Broom C, Schultz M. The detection and prevalence of reactive and physiologic sclerotic dentin, reparative dentin and dead tracts beneath various types of dental lesions according to tooth surface and age. J Oral Pathol. 1983;12:257–289. doi: 10.1111/j.1600-0714.1983.tb00338.x. [DOI] [PubMed] [Google Scholar]
- 13.Tay FR, Pashley DH. Resin bonding to cervical sclerotic dentin: a review. J Dent. 2004;32:173–196. doi: 10.1016/j.jdent.2003.10.009. [DOI] [PubMed] [Google Scholar]
- 14.Ogata M, Harada N, Yamaguchi S, Nakajima M, Pereira PN, Tagami J. Effects of different burs on dentin bond strengths of self-etching primer bonding systems. Oper Dent. 2001;26:375–382. [PubMed] [Google Scholar]
- 15.van Dijken JW. Durability of three simplified adhesive systems in Class V non-carious cervical dentin lesions. Am J Dent. 2004;17:27–32. [PubMed] [Google Scholar]
- 16.Briggs P, Djemal S, Chana H, Kelleher M. Young adult patients with established dental erosion--what should be done? Dent Update. 1998;25:166–170. [PubMed] [Google Scholar]
- 17.GC America Inc. Product Information - G-ænial™ Universal Flo [Internet] Alsip (IL): GC America Inc.; c2011. [updated 2018 Jan 19]. [cited 2011 Jan 1]. Available from: http://www.gcamerica.com/products/operatory/G-aenialFlowable/TechniqueCard.pdf. [Google Scholar]
- 18.Zhao X, Pan J, Malmstrom HS, Ren YF. Protective effects of resin sealant and flowable composite coatings against erosive and abrasive wear of dental hard tissues. J Dent. 2016;49:68–74. doi: 10.1016/j.jdent.2016.01.013. [DOI] [PubMed] [Google Scholar]
- 19.Sumino N, Tsubota K, Takamizawa T, Shiratsuchi K, Miyazaki M, Latta MA. Comparison of the wear and flexural characteristics of flowable resin composites for posterior lesions. Acta Odontol Scand. 2013;71:820–827. doi: 10.3109/00016357.2012.734405. [DOI] [PubMed] [Google Scholar]
- 20.Mizrahi B. A technique for simple and aesthetic treatment of anterior toothwear. Dent Update. 2004;31:109–114. doi: 10.12968/denu.2004.31.2.109. [DOI] [PubMed] [Google Scholar]
- 21.Talbot TR. A technique for placing multiple composite restorations. Restorative Dent. 1985;1:83–84. [PubMed] [Google Scholar]