Abstract
Objectives
The aim of this study is to compare the shear bond strengths of ceramic brackets bonded to zirconia surfaces using different zirconia primers and universal adhesive.
Materials and Methods
Fifty zirconia blocks (15 × 15 × 10 mm, Zpex, Tosoh Corporation) were polished with 1,000 grit sand paper and air-abraded with 50 µm Al2O3 for 10 seconds (40 psi). They were divided into 5 groups: control (CO), Metal/Zirconia primer (MZ, Ivoclar Vivadent), Z-PRIME Plus (ZP, Bisco), Zirconia Liner (ZL, Sun Medical), and Scotchbond Universal adhesive (SU, 3M ESPE). Transbond XT Primer (used for CO, MZ, ZP, and ZL) and Transbond XT Paste was used for bracket bonding (Gemini clear ceramic brackets, 3M Unitek). After 24 hours at 37°C storage, specimens underwent 2,000 thermocycles, and then, shear bond strengths were measured (1 mm/min). An adhesive remnant index (ARI) score was calculated. The data were analyzed using one-way analysis of variance and the Bonferroni test (p = 0.05).
Results
Surface treatment with primers resulted in increased shear bond strength. The SU group showed the highest shear bond strength followed by the ZP, ZL, MZ, and CO groups, in that order. The median ARI scores were as follows: CO = 0, MZ = 0, ZP = 0, ZL = 0, and SU = 3 (p < 0.05).
Conclusions
Within this experiment, zirconia primer can increase the shear bond strength of bracket bonding. The highest shear bond strength is observed in SU group, even when no primer is used.
Keywords: Ceramic bracket, Multi-mode adhesive, Orthodontic bracket, Universal adhesive, Zirconia, Zirconia primer
INTRODUCTION
Recently, the increased demand for esthetically-pleasing orthodontic treatments has led to the use of various new materials to produce more esthetic crowns or orthodontic brackets. Orthodontists frequently encounter patients who have had their teeth restored with metal, feldspathic porcelain, reinforced ceramics, and zirconia instead of natural tooth material. Because of the growing demand to maintain esthetics, the use of ceramic or resin brackets has become more popular than the use of metal brackets for orthodontic treatment.
Originally, the zirconia core was covered with feldspathic porcelain powder as a veneer to maintain esthetics; however, owing to frequent fracture of the veneer, the use of monolithic zirconia crowns has increased [1,2]. In the past, they are used only for the posterior teeth because of the unaesthetic opacity problem. However, as the esthetics of monolithic zirconia crowns improve, they are being used not only for the posterior teeth, but also for anterior teeth [3,4].
However, zirconia is resistant to hydrofluoric acid etching, making it difficult to obtain proper surface roughness using this traditional technique. Thus, various studies have reported techniques to improve the bond strength between zirconia and resin cement by mechanical, chemical, or combined methods. In mechanical surface treatments, roughening using Al2O3- or silica-coated particles leads to increased bond strength [5,6,7]. Several zirconia primers are available for chemical treatment [4,8,9,10]. Usually, these primers contain 10-methacryloyloxydecyl dihydrogen phosphate (10-MDP) as a key component. The phosphate group of the 10-MDP can react with the zirconium oxide, and this increases the bond strength. However, the separate use of a zirconia primer for increasing bonding requires time and increases the cost.
Universal or multi-mode adhesives for direct and indirect restoration with etch-and-rinse or self-etch modes were introduced recently. They usually contain 10-MDP and thus make bonding to zirconia possible without the use of zirconia primers. However, only a few studies on the bond strength between orthodontic brackets and zirconia crowns when these adhesives are used have been published [11,12,13].
There are various materials used to make orthodontic brackets, such as metal, ceramic, resin, and zirconia. Many patients now prefer transparent or white-colored brackets to metal brackets for esthetic reasons, but the bond strength between the bracket and the crown in these devices should be adequate for clinical treatment. A few studies on the shear bond strength between porcelain and metal or ceramic brackets have been published [14]. However, to our knowledge, there have been no such studies on zirconia and ceramic orthodontic brackets. The base of the ceramic bracket is different from that of the metal bracket; thus, the effect of surface treatments using zirconia primers or a universal adhesive to replace the zirconia primer for orthodontic purposes should be evaluated.
The aim of this study was to compare the shear bond strengths of orthodontic ceramic brackets bonded to zirconia surfaces using 3 different zirconia primers and a universal adhesive. The null hypothesis was that there was no difference in the bonding strength of orthodontic ceramic brackets bonded to zirconia surfaces using different primers and universal adhesive.
MATERIALS AND METHODS
Fifty yttria-stabilized zirconium oxide core (Zpex, Tosoh Corporation, Tokyo, Japan) specimens were produced (15 × 15 × 10 mm) using a copy milling machine and sintered. They were embedded in auto-polymerizing acrylic resin (Ortho-Jet, Lang Dental Manufacturing Co., Inc., Wheeling, IL, USA). Zirconia surfaces were polished with 1,000 grit silicon carbide paper, ultrasonically cleaned, and air-dried. Specimens were sandblasted with 50 µm Al2O3 particles for 10 seconds at 40 psi. The specimens were distributed into 5 groups (n = 10 in each group).
The control group (CO) was not treated with zirconia primer. Transbond XT Primer (3M Unitek, Monrovia, CA, USA) was applied on both surfaces and brackets were bonded using Transbond XT Paste (3M Unitek). Each specimen was light-cured for 15 seconds at 1,100 mW/cm2 (Mr. Light LED curing light, Dent Zar, Tarzana, CA, USA).
Three different zirconia primers were applied on the zirconia surface. Metal/Zirconia primer (MZ; Ivoclar Vivadent, Schaan, Liechtenstein), Z-PRIME Plus (ZP; Bisco, Schaumburg, IL, USA), and Zirconia Liner (ZL; Sun Medical, Shiga, Japan) were applied to the specimens of the MZ, ZP, and ZL groups, respectively according to the manufacturer's instructions. Then, Transbond XT Primer was applied on both surfaces and brackets were bonded using Transbond XT.
For the SU group, Scotchbond Universal adhesive (3M ESPE, St. Paul, MN, USA) was applied on the zirconia surface according to the manufacturer's instructions, and ceramic brackets were then bonded on the specimens in a manner similar to that used in the CO group. To minimize the difference, all procedures were done by one operator. The compositions of the 3 zirconia primers and universal adhesive are shown in Table 1.
Table 1. Composition of primers and universal adhesive.
| Trade name (abbreviation) | Composition | Manufacturer |
|---|---|---|
| Metal/Zirconia Primer (MZ) | Tertiary butyl alcohol, methyl isobutyl ketone, phosphonic acid acrylate, benzoylperoxide | Ivoclar Vivadent, Schaan, Liechtenstein |
| Z-PRIME Plus (ZP) | Carboxylic acid monomer (BPDM), HEMA, ethanol, organophosphate monomer (10-MDP) | Bisco, Schaumburg, IL, USA |
| Zirconia Liner (ZL) | MMA, 10-MDP, 4-methoxyphenol (HQME) | Sun Medical, Shiga, Japan |
| Scotchbond Universal adhesive (SU) | Organophosphate monomer (10-MDP), dimethacrylate resins (BisGMA, etc.), HEMA, Vitrebond copolymer, filler, ethanol, water, initiators, silane | 3M ESPE, St. Paul, MN, USA |
BPDM, biphenyl dimethacrylate; HEMA, hydroxyethyl methacrylate; BPDM, biphenyl dimethacrylate; 10-MDP, 10-methacryloyloxydecyl dihydrogen phosphate; MMA, methyl methacrylate; HQME, hydroquinone monomethyl ether.
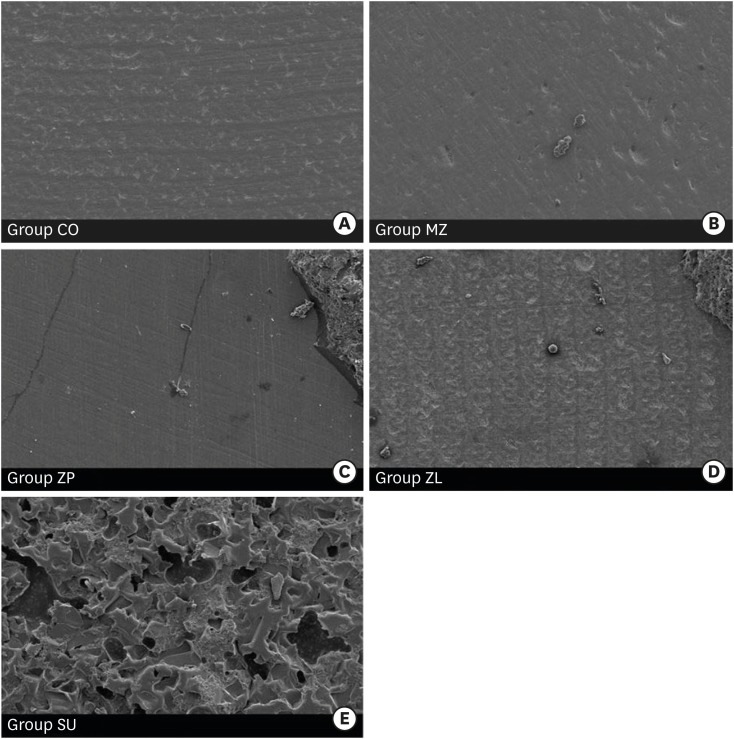
The fifty specimens were stored in a distilled water at 37°C for 24 hours and subjected to 2,000 one-minute-long thermocycles at 5°C and 55°C. The bracket bonded zirconia specimens were mounted on the testing machine zig which bonded surface was perpendicular to the base and the shear bond strength was measured by a universal testing machine (EZ test, Shimadzu Co., Kyoto, Japan), at a crosshead speed of 1 mm/min until bonding failure occurred. The fractured surface was assessed using a stereomicroscope (X30, OPMI Pico, Carl Zeiss Meditec AG, Jena, Germany); the magnified surfaces were classified according to the adhesive remnant index (ARI) score (Table 2) [15]. To obtain a representative image, scanning electron microscope (SEM) images (×100) were obtained (Figure 1). For comparison of shear bond strength, we performed the one-way analysis of variance and post hoc multiple comparisons using the Bonferroni method at α = 0.05. For comparison of the ARI index, we used Fisher's exact test (p < 0.05).
Table 2. Adhesive remnant index (ARI) scores.
| ARI score | Criteria |
|---|---|
| 0 | No adhesive left on the tooth. |
| 1 | Less than half of the adhesive left on the tooth. |
| 2 | More than half of the adhesive left on the tooth. |
| 3 | All adhesive left on the tooth, with distinct impression of the bracket mesh. |
Figure 1.
Scanning electron micrographs (×100) of zirconia surface. (A, B) adhesive failure pattern; (C, D) mixed failure pattern; (E) cohesive failure pattern within the cement. The remnants of the cement were observed on the zirconia surface.
CO, control; MZ, Metal/Zirconia primer (Ivoclar Vivadent, Schaan, Liechtenstein); ZP, Z-PRIME Plus (Bisco, Schaumburg, IL, USA); ZL, Zirconia Liner (Sun Medical, Shiga, Japan); SU, Scotchbond Universal adhesive (3M ESPE, St. Paul, MN, USA).
RESULTS
The results of shear bond strength analysis are described in Table 3. Surface treatments with primers resulted in shear bond strength higher than that obtained without primer use in the CO group. The SU group showed the highest shear bond strength, followed by the ZP, ZL, MZ, and CO groups.
Table 3. Shear bond strengths (SBSs) of ceramic brackets bonded to zirconia surface (MPa, n = 10).
| Group | SBS | Minimum | Maximum |
|---|---|---|---|
| CO | 1.07 ± 0.81d | 0.22 | 2.60 |
| MZ | 5.16 ± 0.83c | 4.08 | 6.51 |
| ZP | 10.47 ± 2.69b | 5.91 | 13.37 |
| ZL | 9.55 ± 1.75b | 7.09 | 12.32 |
| SU | 13.85 ± 1.48a | 11.20 | 16.47 |
Same superscript indicates that the bond strength was not significantly different between the materials.
CO, control; MZ, Metal/Zirconia primer (Ivoclar Vivadent, Schaan, Liechtenstein); ZP, Z-PRIME Plus (Bisco, Schaumburg, IL, USA); ZL, Zirconia Liner (Sun Medical, Shiga, Japan); SU, Scotchbond Universal adhesive (3M ESPE, St. Paul, MN, USA).
During the analysis of the debonded surfaces, most of the CO and MZ specimens showed adhesive failure patterns. However, some specimens of the ZP and ZL groups showed mixed failure (Table 4). The SU group showed mixed or cohesive failure patterns within the bonding resin and ceramic bracket. The SEM micrographs of the representative failure pattern are illustrated in Figure 1. Both the CO and MZ groups showed adhesive failure when observed using a stereomicroscope; the difference was small when SEM images were observed. In the CO group, no remnants were observed on the zirconia surface, and for the MZ group, small particles remained on the zirconia surface. Some of the specimens of the ZP and ZL groups showed mixed failure patterns and adhesive remnants were observed. For the SU group, large quantities of cement and adhesives remained on the zirconia surface.
Table 4. Adhesive remnant index (ARI) scores calculated depending on the remnants of adhesive on the zirconia surface after debonding.
| Group | ARI score | |||||
|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | Median (Q1–Q3) | Mean ± SD | |
| CO | 9 | 1 | - | - | 0 (0–0) | 0.10 ± 0.30 |
| MZ | 10 | - | - | - | 0 (0–0) | 0.00 ± 0.00 |
| ZP | 6 | 4 | - | - | 0 (0–1) | 0.40 ± 0.49 |
| ZL | 7 | 3 | - | - | 0 (0–1) | 0.30 ± 0.46 |
| SU | - | - | 4 | 6 | 3 (2–3)* | 2.60 ± 0.49 |
Q1, first quartile; Q3, third quartile; SD, standard deviation; CO, control; MZ, Metal/Zirconia primer (Ivoclar Vivadent, Schaan, Liechtenstein); ZP, Z-PRIME Plus (Bisco, Schaumburg, IL, USA); ZL, Zirconia Liner (Sun Medical, Shiga, Japan); SU, Scotchbond Universal adhesive (3M ESPE, St. Paul, MN, USA).
*Statistically significant difference (Fisher's exact test; p < 0.05).
DISCUSSION
The ideal bond strength required for orthodontic brackets is not the maximum bond strength. Instead, the bond strength should be adequate enough for enduring orthodontic treatment while being sufficiently weak to permit easy bracket removal. This is to avoid any concerns about inflicting damage to the restorations while debonding brackets that the clinician may have. In this study, 4 different surface treatments (MZ, ZP, ZL, and SU) were applied on zirconia surfaces to increase the bond strength between ceramic brackets and zirconia. Previous studies have shown that the bond strength between the orthodontic bracket and the restoration on tooth surface is acceptable if it exceeds 6–8 MPa [16,17]. The CO group showed the lowest shear bond strength, implying that only sandblasting is not an appropriate surface pretreatment method for bracket bonding on zirconia surfaces. The ZP, ZL, and SU groups showed significantly higher shear bond strengths than the CO group, but the shear bond strength of the MZ group was lower than 6 MPa, which might not be clinically acceptable for bracket bonding. These results are coincident with the ARI score. This might be due to the absence of 10-MDP.
It has been reported that combined treatment using silica-coating, silane, and MDP is reliable, and MDP-containing monomers improve the adhesion between resin cement and zirconia [4,18]. Many previous studies have reported that MDP-containing primers not only increase the bond strength by improving chemical bonding with zirconium oxide, but also maintain stable bonding after thermocycling [19,20,21]. Consistent with previous research, the ZP, ZL, and SU groups, which were treated with primer containing MDP, showed clinically acceptable shear bond strengths. ZP contains organophosphate and carboxylic acid monomers; phosphate monomers can co-polymerize with monomers of resin, and carboxylic monomer helps in substrate bonding [22,23]. It was reported that ZP application was associated with lower bond strength than the application of other MDP-containing primers, because carboxylic acid monomers may have weakened the bonding with the methacrylate group of resin cement [24]. However, according to the results of this study, there was no significant difference between the bond strength in the ZP and ZL groups.
It has been reported that universal adhesives are stable alternatives to conventional bonding techniques [25]. In this experiment, the SU group had significantly higher shear bond strength than the other groups. This adhesive had not been originally developed as a zirconia adhesive, but as observed in this study, it improved bond strength better than other primers that are specialized for zirconia. A possible explanation is that the 10-MPD in the Scotchbond could increase the bond strength, and the Vitrebond copolymer, which is a unique component of the Scotchbond, may also help in bonding to the zirconia surface. Following these results, SU could replace the zirconia primer in the separate step implemented before application of the bonding agent, and it may simplify the bonding step.
In the study of bonding failure patterns, the SU groups showed the most amount of cement remnants on the zirconia surface, and this is consistent with the results of the shear bond strength analysis. Most of the CO and MZ samples showed adhesive failure patterns, reflecting low shear bond strengths.
CONCLUSIONS
Using the zirconia primers can increase the bond strength between the ceramic bracket and zirconia restoration. The SU group showed the highest shear bond strength, even without the use of the zirconia primer, suggesting that the Scotchbond adhesive can be used to simplify the bonding step. The shear bond strengths of the ZP, ZL, and SU groups are clinically acceptable.
Footnotes
Funding: This work was supported by the National Health Insurance Corporation Ilsan Hospital (NHIMC2013CR56).
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
- Conceptualization: Lee JY, Park JW.
- Data curation: Lee JY.
- Formal analysis: Ahn JC, An SI.
- Funding acquisition: Lee JY.
- Investigation: Ahn JC, An SI.
- Methodology: Lee JY, Park JW.
- Project administration: Park JW.
- Resources: Lee JY.
- Software: Ahn JC, Lee JY.
- Supervision: Lee JY, Park JW.
- Validation: Lee JY, Park JW.
- Visualization: Ahn JC, An SI.
- Writing - original draft: Lee JY.
- Writing - review & editing: Lee JY, Park JW.
References
- 1.Aboushelib MN, de Jager N, Kleverlaan CJ, Feilzer AJ. Effect of loading method on the fracture mechanics of two layered all-ceramic restorative systems. Dent Mater. 2007;23:952–959. doi: 10.1016/j.dental.2006.06.036. [DOI] [PubMed] [Google Scholar]
- 2.Miyazaki T, Nakamura T, Matsumura H, Ban S, Kobayashi T. Current status of zirconia restoration. J Prosthodont Res. 2013;57:236–261. doi: 10.1016/j.jpor.2013.09.001. [DOI] [PubMed] [Google Scholar]
- 3.Özcan M, Bernasconi M. Adhesion to zirconia used for dental restorations: a systematic review and meta-analysis. J Adhes Dent. 2015;17:7–26. doi: 10.3290/j.jad.a33525. [DOI] [PubMed] [Google Scholar]
- 4.Atsu SS, Kilicarslan MA, Kucukesmen HC, Aka PS. Effect of zirconium-oxide ceramic surface treatments on the bond strength to adhesive resin. J Prosthet Dent. 2006;95:430–436. doi: 10.1016/j.prosdent.2006.03.016. [DOI] [PubMed] [Google Scholar]
- 5.Kato H, Matsumura H, Atsuta M. Effect of etching and sandblasting on bond strength to sintered porcelain of unfilled resin. J Oral Rehabil. 2000;27:103–110. doi: 10.1046/j.1365-2842.2000.00489.x. [DOI] [PubMed] [Google Scholar]
- 6.Wolf DM, Powers JM, O'Keefe KL. Bond strength of composite to etched and sandblasted porcelain. Am J Dent. 1993;6:155–158. [PubMed] [Google Scholar]
- 7.Baldissara P, Querzè M, Monaco C, Scotti R, Fonseca RG. Efficacy of surface treatments on the bond strength of resin cements to two brands of zirconia ceramic. J Adhes Dent. 2013;15:259–267. doi: 10.3290/j.jad.a28729. [DOI] [PubMed] [Google Scholar]
- 8.Ernst CP, Cohnen U, Stender E, Willershausen B. In vitro retentive strength of zirconium oxide ceramic crowns using different luting agents. J Prosthet Dent. 2005;93:551–558. doi: 10.1016/j.prosdent.2005.04.011. [DOI] [PubMed] [Google Scholar]
- 9.Sahafi A, Peutzfeld A, Asmussen E, Gotfredsen K. Effect of surface treatment of prefabricated posts on bonding of resin cement. Oper Dent. 2004;29:60–68. [PubMed] [Google Scholar]
- 10.de Souza G, Hennig D, Aggarwal A, Tam LE. The use of MDP-based materials for bonding to zirconia. J Prosthet Dent. 2014;112:895–902. doi: 10.1016/j.prosdent.2014.01.016. [DOI] [PubMed] [Google Scholar]
- 11.Kwak JY, Jung HK, Choi IK, Kwon TY. Orthodontic bracket bonding to glazed full-contour zirconia. Restor Dent Endod. 2016;41:106–113. doi: 10.5395/rde.2016.41.2.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee JH, Lee M, Kim KN, Hwang CJ. Resin bonding of metal brackets to glazed zirconia with a porcelain primer. Korean J Orthod. 2015;45:299–307. doi: 10.4041/kjod.2015.45.6.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee JY, Kim JS, Hwang CJ. Comparison of shear bond strength of orthodontic brackets using various zirconia primers. Korean J Orthod. 2015;45:164–170. doi: 10.4041/kjod.2015.45.4.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abu Alhaija ES, Abu AlReesh IA, AlWahadni AM. Factors affecting the shear bond strength of metal and ceramic brackets bonded to different ceramic surfaces. Eur J Orthod. 2010;32:274–280. doi: 10.1093/ejo/cjp098. [DOI] [PubMed] [Google Scholar]
- 15.Bishara SE, Olsen ME, Von Wald L. Evaluation of debonding characteristics of a new collapsible ceramic bracket. Am J Orthod Dentofacial Orthop. 1997;112:552–559. doi: 10.1016/s0889-5406(97)70083-0. [DOI] [PubMed] [Google Scholar]
- 16.Reynolds IR. A review of direct orthodontic bonding. Br J Orthod. 1975;2:171–178. [Google Scholar]
- 17.Whitlock BO, 3rd, Eick JD, Ackerman RJ, Jr, Glaros AG, Chappell RP. Shear strength of ceramic brackets bonded to porcelain. Am J Orthod Dentofacial Orthop. 1994;106:358–364. doi: 10.1016/S0889-5406(94)70056-7. [DOI] [PubMed] [Google Scholar]
- 18.Blatz MB, Sadan A, Martin J, Lang B. In vitro evaluation of shear bond strengths of resin to densely-sintered high-purity zirconium-oxide ceramic after long-term storage and thermal cycling. J Prosthet Dent. 2004;91:356–362. doi: 10.1016/j.prosdent.2004.02.001. [DOI] [PubMed] [Google Scholar]
- 19.Blatz MB, Chiche G, Holst S, Sadan A. Influence of surface treatment and simulated aging on bond strengths of luting agents to zirconia. Quintessence Int. 2007;38:745–753. [PubMed] [Google Scholar]
- 20.Kern M, Wegner SM. Bonding to zirconia ceramic: adhesion methods and their durability. Dent Mater. 1998;14:64–71. doi: 10.1016/s0109-5641(98)00011-6. [DOI] [PubMed] [Google Scholar]
- 21.Wegner SM, Kern M. Long-term resin bond strength to zirconia ceramic. J Adhes Dent. 2000;2:139–147. [PubMed] [Google Scholar]
- 22.Chen L, Suh BI, Brown D, Chen X. Bonding of primed zirconia ceramics: evidence of chemical bonding and improved bond strengths. Am J Dent. 2012;25:103–108. [PubMed] [Google Scholar]
- 23.Magne P, Paranhos MP, Burnett LH., Jr New zirconia primer improves bond strength of resin-based cements. Dent Mater. 2010;26:345–352. doi: 10.1016/j.dental.2009.12.005. [DOI] [PubMed] [Google Scholar]
- 24.Lorenzoni FC, Leme VP, Santos LA, de Oliveira PC, Martins LM, Bonfante G. Evaluation of chemical treatment on zirconia surface with two primer agents and an alkaline solution on bond strength. Oper Dent. 2012;37:625–633. doi: 10.2341/11-216-L. [DOI] [PubMed] [Google Scholar]
- 25.Amaral M, Belli R, Cesar PF, Valandro LF, Petschelt A, Lohbauer U. The potential of novel primers and universal adhesives to bond to zirconia. J Dent. 2014;42:90–98. doi: 10.1016/j.jdent.2013.11.004. [DOI] [PubMed] [Google Scholar]