Abstract
This study presents a novel application of the cognitive processing model of alcohol craving (CPMA) from the addictions field to the role of food craving in the well-established restrained eating–overeating relationship associated with binge eating disorder (BED). A community sample (N = 1058, ages 18-66) completed an online survey assessing four core domains: restrained eating, trait food craving, uncontrolled eating, and emotional eating. In accordance with the CPMA, food craving emerged as a significant indirect effect of the association between restrained eating and both uncontrolled and emotional eating. Gender did not significantly moderate any direct or indirect associations, suggesting that gender may not change the pattern of association between restrained eating and different facets of overeating. Results suggest that treatments targeting binge eating behaviors may benefit from 1) explicitly addressing the activation of food craving rather than concentrating on reducing restrained eating and 2) recognizing that food craving may be an important gender-neutral target with the potential to reduce binge and overeating behaviors. Future research should extend these preliminary findings by examining the application of the CPMA to eating behaviors while jointly investigating antecedents and contextual factors.
Keywords: binge eating disorder, food craving, overeating, restrained eating, obesity
Introduction
Worldwide obesity prevalence has more than doubled since 1980, with over 600 million individuals meeting obese weight status in 2014 (World Health Organization, 2016). Obesity status is associated with binge eating disorder (BED; Spitzer et al., 1992), with 87% of individuals diagnosed with BED meeting criteria for obese weight status (Villarejo et al., 2012), suggesting overlapping risk factors for these conditions. Binge eating, a core diagnostic criteria of BED (American Psychiatric Association, 2013), is associated with both uncontrolled (Spitzer et al., 1992) and emotional eating (Masheb & Grilo, 2006), and all three overeating behaviors are risk factors for obesity (Desai, Miller, Staples, & Bravender, 2008; Ganley, 1989; Rohrer, Vickers-Douglas, & Stroebel, 2009). Despite the high comorbidity and overlap in associated behaviors, treatment efforts targeting both obesity and binge eating behaviors are largely unsuccessful (Reas & Grilo, 2014; Wadden et al., 2013), underscoring the need to investigate novel processes associated with overeating behaviors (e.g., uncontrolled and emotional eating).
Restrained eating and food craving have emerged as important risk factors for overeating behaviors (Lowe, 2002; Neumark-Sztainer, Wall, Haines, Story, & Eisenberg, 2007); however, theoretical models incorporating both processes to explain overeating behaviors are limited. Drawing from the alcohol use literature, the cognitive processing model of craving (CPMC; Tiffany, 1990; Tiffany & Conklin, 2000) provides a framework through which the relationships between restrained eating, food craving, and problematic overeating behaviors can be understood and posits food craving as a potential target for intervention that is relevant to both obesity and BED.
Restrained eating, defined as an intentional restriction of food intake (Lowe, 2002), is consistently linked with overeating behaviors. Although this relationship seems counterintuitive, many highly influential theories variously conceptualize the well-established relationship (disinhibition hypothesis: Herman & Polivy, 1975; boundary model: Herman & Polivy, 1980; goal conflict model: Stroebe, Mensink, Aarts, Schut, & Kruglanski, 2008). Collectively, these models explain the tendency of individuals restraining their food intake to overeat in response to negative cognitions or emotions, by breaking self-imposed dietary boundaries, or due to violation of internal goals. While these theoretical models have accrued evidence supporting the role of both internal and external cues, this prior work is limited by its discounting of the experience of food craving in the restrained–overeating behavior relationship.
Food craving has been defined as an intensely strong desire for a specific food, or specific type of food (Gendall, Joyce, & Sullivan, 1997) and a psychological or physiological motivational state that prompts the consumption or ingestion of a desired substance (Meule & Kübler, 2012). Showing strong associations with both overeating/binge eating behaviors (Havermans, 2013; Moreno, Warren, Rodríguez, Fernández, & Cepeda-Benito, 2009; Rogers & Smit, 2000) and restrained eating (Burton, Smit, & Lightowler, 2007; Cepeda-Benito, Fernandez, & Moreno, 2003), food craving is substantially higher in individuals who engage in binge eating compared to those who do not (e.g., Moreno et al., 2009; Ng & Davis, 2013). Further, dieters report stronger and less resistible cravings than non-dieters (Massey & Hill, 2012). Thus, food craving may act as potent risk factor for overeating behaviors and serve as a common trigger for the development of binge eating behavior (American Psychiatric Association, 2015; Neumark-Sztainer et al., 2007) and obesity status (Drewnowski, Kurth, Holden-Wiltse, & Saari, 1992). More importantly, its associations with both restrained eating and overeating suggests a potential mechanistic relationship that may help clarify the restrained eating–overeating relationship.
Addiction models are increasingly applied to understand the neural mechanisms, behaviors, and cognitions involved in maladaptive eating (Cartwright & Stritzke, 2008; Cartwright et al., 2007; Hoebel, 1999) and may provide a framework through which the paradoxical relationship between restrained eating and overeating can be understood. The cognitive processing model of alcohol craving (CPMA; Tiffany, 1990; Tiffany & Conklin, 2000) may be particularly appropriate for understanding the role of food craving in this relationship. According to this model, when individuals attempt abstinence, alcohol craving occurs in parallel with either 1) the presentation of an obstacle to consumption (e.g., an individual’s favorite bar is closed), or 2) attempts to inhibit the execution of alcohol consumption (e.g., someone recently sober trying to remain sober). In theory, for individuals experiencing alcohol use disorder, the activation of craving helps to explain the relationship between attempts at alcohol abstinence and continued excessive use. Applying the CPMA to eating behaviors would suggest that the association between restrained eating and overeating behaviors may be accounted for by food craving.
Two facets of overeating are of particular interest due to their similarities with the addiction literature: uncontrolled eating and emotional eating. Uncontrolled eating is characterized by a loss of control during food intake (Karlsson, Persson, Sjöström, & Sullivan, 2000), and is similar to the concept of loss of control drinking which has been characterized as an underlying explanation for overconsumption of alcohol (Heather, Tebbutt, Mattick, & Zamir, 1993; Jellinek, 1960; Lyvers, 2000). Indeed, data suggest that treatment-seeking individuals with overeating behaviors who are subsequently diagnosed with BED report uncontrolled eating episodes as particularly impairing (Spitzer et al., 1992). Similarly, uncontrolled eating is strongly associated with obese status (Rohrer et al., 2009). In contrast, emotional eating represents the tendency to overeat during the experience of dysphoric mood states (Karlsson et al., 2000). Originally derived from theories of obesity (Bruch, 1973; Kaplan & Kaplan, 1957), emotional eating occurs in an effort to reduce emotional distress (Karlsson et al., 2000), and is similar to theories and supporting evidence that individuals use alcohol to cope with negative affect (e.g., Baker, Piper, McCarthy, Majeskie, & Fiore, 2004; Cooper, Frone, Russell, & Mudar, 1995; Sher, 2007). Emotional eating research indicates that individuals diagnosed with BED report an association between anxiety-related emotional eating and more frequent binge eating episodes (Masheb & Grilo, 2006). Building upon alcohol literature, the current study independently considers the applicability of the CPMA to uncontrolled and emotional eating.
Current Study
The current study sought to test an application of a theoretical framework that incorporated restrained eating, overeating, and craving to better understand the potential mechanisms underlying the well-established association between restrained eating and overeating. Based on previous literature, it was hypothesized that: (1) greater restrained eating and food craving would be associated with increased overeating (i.e., both uncontrolled and emotional eating) and (2) consistent with the CPMA, food craving would emerge as an indirect effect of the relationships between restrained eating and each facet of overeating.
Further, potential gender differences in these relationships were examined. Research suggests mean level differences in the constructs of interest across genders, with women consistently reporting greater degrees of restrained eating (Burton et al., 2007), higher levels of food craving (Opwis, Schmidt, Martin, & Salewski, 2017), a greater number of uncontrolled eating episodes (Striegel-Moore et al., 2009) and more emotional eating (Konttinen, Männistö, Sarlio-Lähteenkorva, Silventoinen, & Haukkala, 2010; Larsen, van Strien, Eisinga, & Engels, 2006) compared to men. Early work also suggests that craving for specific types of foods also may differ by gender (Pelchat, 1997). Thus, this study explored gender as a potential moderator of all direct and indirect associations for both uncontrolled and emotional eating to test whether these established gender differences also represent differences in mechanistic processes.
Method
Participants and Procedures
The study received approval from the University of South Florida’s Institutional Review Board. Participants were sampled via Amazon’s Mechanical Turk (MTurk), and completed a series of questionnaires online lasting approximately 45-minutes to earn $0.50. MTurk represents the dominant crowdsourcing market used by academic researchers (Buhrmester, Kwang, & Gosling, 2011; Mason & Suri, 2012). MTurk allows for rapid data collection, is inexpensive, and represents attentive (Hauser & Schwarz, 2016) and diverse populations (Gosling & Mason, 2015; Mason & Suri, 2012; Weinberg, Freese, & McElhattan, 2014). Inclusion criteria included being between the ages of 18 and 65 years, living in the United States, and being native English speakers.
Data quality was evaluated in multiple ways. First, MTurk has policies and built-in reputation systems to reinforce participants who provide quality data (Mason & Suri, 2012). Second, three attention checks were inserted throughout the questionnaire (e.g., “I have been to every country in the world”; Meade & Craig, 2012) to ensure quality data and guard against the increasing threat of form-completion bots (Prince, Litovsky, & Friedman-Wheller, 2012). Data suggest that missing two or more attention checks is associated with less reliable data (Aust, Diedenhofen, Ullrich, & Musch, 2013). Third, visual inspections for careless responding (e.g., same value across surveys) were conducted.
Of the original 1250 individuals who consented to participate, 193 individuals were excluded from analyses for either failing two or more attention checks (n = 129), showing excessive missing data (n = 63), or missing data on variables of interest (n =1), leaving a total of 1057 individuals for analysis. This sample was 59.70% women (n = 632) and ranged in age from 18 to 66 (M = 37.15, SD = 11.82). Participants’ mean body mass index (BMI) was 27.20 (SD = 6.70), which is in the overweight range. Ninety-three percent (92.9%) identified as non-Hispanic, Spanish or Latino (6.8% Hispanic, Spanish, or Latino, 0.2% unknown). Of those who identified as Non-Hispanic, Spanish or Latino, 83.3% identified as White, 6.3% as Black, 6.7% as Asian, 0.8% as American Indian or Alaskan Native, 0.2% as Native Hawaiian or Pacific Islander, and 2.6% as other/multiracial. Of those who identified as Hispanic, Spanish or Latino, 58.3% identified as White, 6.9% as Black, 2.7% as Asian, 1.4% as American Indian or Alaskan Native, and 26.4% as other/multiracial.
Measures
The data were collected as a part of a larger investigation of eating, weight, and substance use attitudes and behaviors. The following are relevant to the current study.
Demographics
Demographic data including age, gender, race/ethnicity, height and weight, were collected via self-report. Body mass index (BMI) was used as an index of body weight adjusted for participant height, and calculated from by using the equation BMI = Weight (kg)/Height (m)2.
Food Craving
Trait food craving was assessed with the General Food Craving Questionnaire – Trait (G-FCQ-T; Nijs, Franken, & Muris, 2007). The 21-item scale measures a general ‘desire for food’ or ‘desire to eat’ and consists of four subscales: (1) preoccupation with food, (2) loss of control, (3) positive outcome expectancy, and (4) emotional craving. Items are summed to generate a total craving score, with higher scores indicating more trait-like characteristics of food craving, including a general urge to eat. A sample item from this scale is “I find myself preoccupied with food” with responses ranging from 1 (never or not applicable) to 6 (always). The internal consistency of this scale has been established with adult men and women (α = .94; Alberts, Thewissen, & Raes, 2012; α = .94; Nijs et al., 2007) and was similarly high in the current sample (women α = .97; men α = .96). The G-FCQ-T was presented to respondents as the third questionnaire in the larger survey.
Restrained Eating
The restrained eating subscale of the Dutch Eating Behavior Questionnaire (DEBQ; Van Strien, Frijters, Bergers, & Defares, 1986) was used to assess restrained eating and presented as the seventh questionnaire in the larger survey. The subscale consisted of 10-items rated on a five-point scale from 1 (never) to 5 (very often). Items are summed for a total score, with higher scores indicating a greater degree of food restriction. An example item is “When you have eaten too much, do you eat less than usual the following day?” The restraint scale demonstrated acceptable internal consistency in past research (α = .95; Stice & Agras, 1998; Van Strien et al., 1986), as well as in the current sample (women α = .94; men α = .94).
Uncontrolled and Emotional Eating
Eating behavior was assessed using the uncontrolled and emotional eating subscales of the revised Three Factor Eating Questionnaire (TFEQ-R18V2; Cappelleri et al., 2009), which was presented as the fifth questionnaire in the larger survey. The 9-item uncontrolled eating subscale reflects difficulty in regulation or loss of control while eating. A sample item is “Sometimes when I start eating, I just can’t seem to stop” with responses ranging from 1 (definitely true) to 4 (definitely false). The 6-item emotional eating subscale measures overeating that occurs during dysphoric mood states. A sample item is “When I feel blue, I often overeat” with responses ranging from 1 (definitely true) to 4 (definitely false). For both subscales, higher values indicate more overeating behavior. Both the uncontrolled eating and emotional eating subscales have shown high internal consistency in past research with adult men and women (α = .82; α = .89; Keskitalo et al., 2008), which was replicated in the current sample (women: uncontrolled α = .89; emotional α = .95; men: uncontrolled α = .89; emotional α = .96).
Data Analytic Strategy
Descriptive statistics were examined using independent samples t-tests and bivariate correlations (see Tables 1 and 2). Hypotheses were tested in SPSS using PROCESS Model 59 (Hayes, 2013) with 10,000 bootstrapped estimates. This model estimates a moderated indirect effect by evaluating the impact of the moderator on the indirect effect, as well as the predictive relationship to the direct effect. In both models, the independent variable was restrained eating, the intervening variable was trait food craving, and the dependent variable was either uncontrolled eating or emotional eating, with BMI and age as covariates. Gender was included as a moderator of each of the paths in the indirect effect model.
Table 1.
Correlations of Primary Variables by Gender
| Variable | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| 1. Restrained Eating (DEBQ) | – | .27** | .28** | .27** | .30** | .04 |
| 2. Uncontrolled Eating (TFEQ) | .18** | – | .79** | .80** | .29** | −.14** |
| 3. Emotional Eating (TFEQ) | .18** | .75** | – | .73** | .26** | −.10* |
| 4. Food Craving (G-FCQ-T) | .21** | .81** | .75** | – | .24** | −.16** |
| 5. BMI | .06 | .32** | .34** | .34** | – | .18** |
| 6. Age | .06 | −.08* | .03 | −.06 | .14** | – |
Note. Correlations of primary variables among men presented above the diagonal, and correlations of primary variables among women are presented below the diagonal. All significance tests were two-tailed
p < .05;
p < .01.
Table 2.
Descriptive Statistics for Primary Variables for Overall Sample and by Gender
| Overall | Men | Women | |||||||
|---|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | t | p | d | |
| Restrained Eating | 26.62 | 9.29 | 24.63 | 8.91 | 27.98 | 9.29 | −5.85 | .001 | 0.37 |
| Uncontrolled Eating | 19.14 | 5.95 | 18.48 | 5.76 | 19.56 | 6.00 | −2.92 | .004 | 0.18 |
| Emotional Eating | 12.54 | 5.26 | 11.41 | 4.98 | 13.26 | 5.31 | −5.70 | .001 | 0.36 |
| Food Craving | 54.92 | 21.70 | 51.35 | 19.82 | 57.21 | 22.45 | −4.36 | .001 | 0.28 |
| BMI | 27.20 | 6.70 | 26.71 | 5.37 | 27.52 | 7.45 | −1.91 | .057 | 0.12 |
| Age | 37.15 | 11.82 | 35.86 | 11.38 | 38.04 | 12.02 | −2.95 | .003 | 0.19 |
Note. All significance tests were two-tailed. M = mean score; SD = standard deviation; t = t-test; p = p-value; d = Cohen’s d.
Due to concerns about potential measurement contamination between two factors included in the intervening variable (i.e., G-FCQ-T loss of control and emotional craving factors) and the two dependent variables (i.e., TFEQ-R18V2 uncontrolled and emotional eating subscales), factors of concern were excluded from the intervening variable calculation for individual model estimates. Specifically, G-FCQ-T loss of control factor items were removed from the food craving variable when uncontrolled eating was the dependent variable. Similarly, G-FCQ-T emotional craving factor items were excluded from the food craving variable when emotional eating was the dependent variable.
Results
Descriptive Statistics
The zero-order correlations, means, and standard deviations of all relevant variables are presented in Tables 1 and 2, respectively. Results indicated that women were significantly older than men, t(1055) = −2.95, p = .003. Consistent with past research, women reported higher levels of restrained eating, t(1055) = −5.85, p < .001, higher levels of food craving, t(1055) = −4.36, p < .001, more uncontrolled eating, t(1055) = −2.92, p = .004, and more emotional eating episodes, t(1055) = −5.70, p < .001, compared to men.
Moderated Indirect Effect Analyses
Uncontrolled Eating
Controlling for BMI and age, food craving was examined as an indirect effect of the association between restrained eating and uncontrolled eating, with gender as a potential moderator (see Figure 1). The overall model accounted for 61% of the variance in uncontrolled eating. Higher BMI (b = .08, 95% CI [.05, .12], p < .001) and younger age (b = −.02, 95% CI [−.04, −.00], p = .03) were associated with more uncontrolled eating. Greater restrained eating was associated with higher levels of food craving (b = .27, 95% CI [.12, .42], p < .001) and higher levels of food craving were associated with more frequent uncontrolled eating (b = .30, 95% CI [.27, .32], p < .001). A significant indirect effect of food craving on the association between restrained eating and uncontrolled eating was observed for both women (b = .09, 95% CI [.05, .12]) and men (b = .08, 95% CI [.04, .12]). Gender did not moderate any of the paths within the model and the magnitude of the indirect effect estimate was not significantly different across gender groups (b = .01, 95% CI [−.05, .06]).
Figure 1.
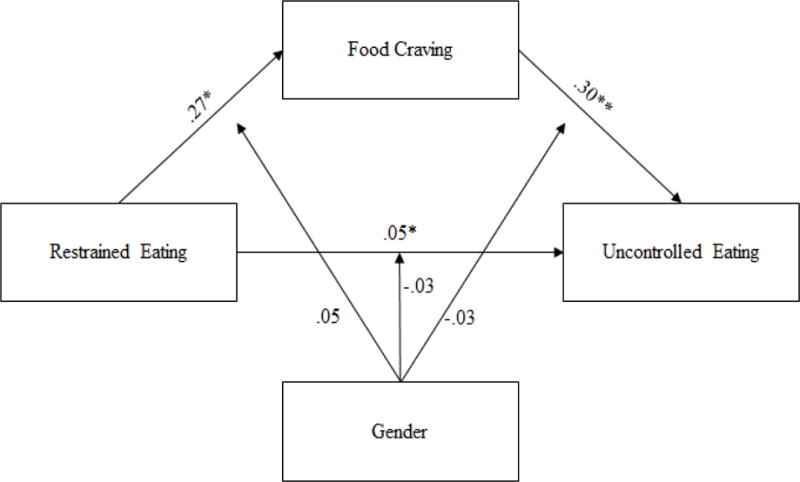
Graphic representation with unstandardized regression coefficients of moderated mediation of indirect effect model of uncontrolled eating (* p < .05; ** p < .001)
Emotional Eating
Controlling for BMI and age, food craving was examined as an indirect effect of the association between restrained eating and uncontrolled eating, with gender as a potential moderator (see Figure 2). The overall model accounted for 48% of the variance in emotional eating. Higher BMI was associated with more emotional eating (b = .10, 95% CI [.06, .14], p < .001); age was not significant (b = .01, 95% CI [−.01, .03], p = .52). Greater restrained eating was associated with greater food craving (b = .31, 95% CI [.14, .49], p < .001), and higher levels of food craving were associated with more frequent emotional eating (b = .19, 95% CI [.17, .22], p < .001). A significant indirect effect of food craving on the association between restrained eating and emotional eating was observed for both women (b = .07, 95% CI [.04, .10]) and men (b = .06, 95% CI [.03, .09]). Similar to uncontrolled eating, gender did not moderate any of the paths within the model and the magnitude of the indirect effect estimate was not significantly different across gender groups (b = .01, 95% CI [−.03, .05]).
Figure 2.
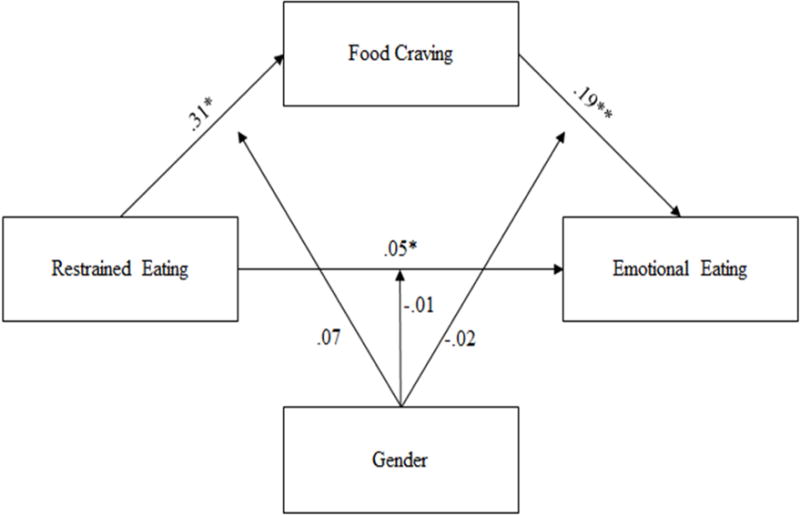
Graphic representation with unstandardized regression coefficients of moderated mediation of indirect effect model of emotional eating (* p < .05; ** p < .001).
Discussion
The current study builds upon past theories describing the restrained eating–overeating relationship and presents a novel application of a theoretical model from the addictions field. In accordance with the CPMA, food craving emerged as a significant indirect effect of the association between restrained eating and both uncontrolled and emotional eating, suggesting that attempts to restrain one’s eating may activate food cravings, thereby increasing the risk of overeating. Notably, gender was not a moderator of these associations. The present study addresses a gap in current literature by presenting a model that integrates and explicitly recognizes the role of food craving in the established association between restrained eating and overeating behaviors. Further, findings support food craving as a potential treatment target for both individuals with binge eating behaviors and obesity. Notably, these findings suggest that gender may not change the pattern of association between restrained eating and different facets of overeating.
Consistent with substance use treatment findings that targeting craving improves treatment outcomes (Helstrom et al., 2016; Monterosso et al., 2001), results of the current study suggest that explicitly targeting the activation food craving may confer treatment benefits. Rather than focusing attention on reducing restrained eating behaviors, the results of the current study indicate efforts should concentrate on reducing the activation of, and coping with the sensations associated with, food craving. Both pharmacological (Greenway et al., 2010; Greenway et al., 2009) and behavioral treatments (Alberts, Mulkens, Smeets, & Thewissen, 2010; May, Andrade, Batey, Berry, & Kavanagh, 2010) have begun to focus on food craving in individuals of obese weight status, those impaired by binge eating episodes, and those subsequently diagnosed with BED. Unfortunately, these treatment efforts show mixed results at reducing food craving activation. Similar to work in the addictions field showing the utility of mindfulness to decrease alcohol cravings (Bowen et al., 2009), mindfulness-based interventions show some promise of reducing food craving, which is associated with reduced loss of control eating following exposure to food cues (Alberts et al., 2010). The current application of the CPMA further supports empirical data from the eating disorder and obesity literatures indicating that treatments targeting restrained and overeating behaviors should allocate greater attention to the reduction of food craving, which may garner benefits to both individuals with BED and/or obesity.
Consistent with past findings, results indicate that the presentation of restrained eating (Williamson, Serdula, Anda, Levy, & Byers, 1992), food craving (Opwis et al., 2017; Weingarten & Elston, 1991), and both facets of overeating (Konttinen et al., 2010; Turner, Luszczynska, Warner, & Schwarzer, 2010) differ across levels of gender, with women showing greater levels of disordered eating behavior than men. Larsen et al. (2006) reported gender differences in emotional eating among a sample of individuals with obese or overweight status, and argued for gender-specific treatments targeting emotional eating. While the current results show corresponding mean level differences, the mechanistic processes involved in the restrained eating–overeating relationship seem to function similarly across men and women. Thus, food craving, which accounts for a significant proportion of variance in the restrained eating–emotional eating relationship, may be an important and gender-neutral treatment target. Treatments aimed at reducing emotional eating and overeating more broadly may benefit from focusing on non-gender specific processes.
Consistent with Luo and colleagues’ (2016) call to utilize community samples to capture the full range of severity of eating pathology, this study benefited from novel contributions including an application of an addictions model to common maladaptive eating behaviors in a large community sample. Despite these strengths, a number of limitations deserve consideration. The current study relied on self-report measures; however, past research indicates that subjective binge eating episodes have comparable outcomes to objective binge eating episodes when criteria are presented clearly (Kerzhnerman & Lowe, 2002). Second, while the current study represented cross-sectional data, this is the first test of a theoretical model with transdiagnostic implications that highlights potentially similar maintaining processes across substance use and eating disorders. Given the promising findings, this novel application of the CPMA to eating behaviors should be replicated using longitudinal analyses to establish temporal ordering. In addition, the current model may be limited to the understanding of emotional eating in response to negative emotions, rather than emotional eating broadly. Future research should investigate the applicability of this model to emotional eating in response to both positive and negative emotional states. Third, the current sample may not be wholly representative of broader community samples. Additionally, due to the large proportion of non-Hispanic White participants, findings may not generalize to individuals of other racial/ethnic groups. Lastly, data were collected via a crowdsourcing data collection tool. To further guard against form-completion bots, future research should consider implementation of extra precautionary measures such as inserting Completely Automatic Public Turing Tests to discriminate between human and computer responders.
Despite these limitations, this study supported the application of the CPMA to elucidate the association between restrained and overeating eating behaviors and suggests that food craving may be a gender-neutral process. The present study broadens our understanding of role of food craving on the restrained eating–overeating relationship and establishes gender similarities in the way these processes function. Future research should further explore the application of the CPMA to eating behaviors while jointly investigating antecedents and contextual factors, as well as additional cognitive, affective, and biological underpinnings related to food intake.
Acknowledgments
Funding
This work was supported in part by the National Institute of Child Health and Human Development (L40 HD078334) and the National Institute on Alcohol Abuse and Alcoholism (K23 AA021768).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Alberts H, Mulkens S, Smeets M, Thewissen R. Coping with food cravings. Investigating the potential of a mindfulness-based intervention. Appetite. 2010;55(1):160–163. doi: 10.1016/j.appet.2010.05.044. [DOI] [PubMed] [Google Scholar]
- Alberts HJ, Thewissen R, Raes L. Dealing with problematic eating behaviour. The effects of a mindfulness-based intervention on eating behaviour, food cravings, dichotomous thinking and body image concern. Appetite. 2012;58(3):847–851. doi: 10.1016/j.appet.2012.01.009. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®) 5th. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- American Psychiatric Association. Feeding and Eating Disorders: DSM-5® Selections. American Psychiatric Publishing; 2015. [Google Scholar]
- Aust F, Diedenhofen B, Ullrich S, Musch J. Seriousness checks are useful to improve data validity in online research. Behavior research methods. 2013;45(2):527–535. doi: 10.3758/s13428-012-0265-2. [DOI] [PubMed] [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, Fiore MC. Addiction motivation reformulated: an affective processing model of negative reinforcement. Psychol Rev. 2004;111(1):33–51. doi: 10.1037/0033-295x.111.1.33. [DOI] [PubMed] [Google Scholar]
- Bowen S, Chawla N, Collins SE, Witkiewitz K, Hsu S, Grow J, Marlatt A. Mindfulness-based relapse prevention for substance use disorders: a pilot efficacy trial. Subst Abus. 2009;30(4):295–305. doi: 10.1080/08897070903250084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruch H. Eating disorders; obesity, anorexia nervosa, and the person within. New York: Basic Books; 1973. [Google Scholar]
- Buhrmester M, Kwang T, Gosling SD. Amazon’s Mechanical Turk: A new source of inexpensive, yet high-quality, data? Perspectives on psychological science. 2011;6(1):3–5. doi: 10.1177/1745691610393980. [DOI] [PubMed] [Google Scholar]
- Burton P, Smit HJ, Lightowler HJ. The influence of restrained and external eating patterns on overeating. Appetite. 2007;49(1):191–197. doi: 10.1016/j.appet.2007.01.007. [DOI] [PubMed] [Google Scholar]
- Cappelleri JC, Bushmakin AG, Gerber RA, Leidy NK, Sexton CC, Lowe MR, Karlsson J. Psychometric analysis of the Three-Factor Eating Questionnaire-R21: results from a large diverse sample of obese and non-obese participants. Int J Obes (Lond) 2009;33(6):611–620. doi: 10.1038/ijo.2009.74. [DOI] [PubMed] [Google Scholar]
- Cartwright F, Stritzke WG. A multidimensional ambivalence model of chocolate craving: construct validity and associations with chocolate consumption and disordered eating. Eat Behav. 2008;9(1):1–12. doi: 10.1016/j.eatbeh.2007.01.006. [DOI] [PubMed] [Google Scholar]
- Cartwright F, Stritzke WG, Durkin K, Houghton S, Burke V, Beilin LJ. Chocolate craving among children: implications for disordered eating patterns. Appetite. 2007;48(1):87–95. doi: 10.1016/j.appet.2006.07.081. [DOI] [PubMed] [Google Scholar]
- Cepeda-Benito A, Fernandez MC, Moreno S. Relationship of gender and eating disorder symptoms to reported cravings for food: construct validation of state and trait craving questionnaires in Spanish. Appetite. 2003;40(1):47–54. doi: 10.1016/s0195-6663(02)00145-9. [DOI] [PubMed] [Google Scholar]
- Cooper ML, Frone MR, Russell M, Mudar P. Drinking to regulate positive and negative emotions: a motivational model of alcohol use. J Pers Soc Psychol. 1995;69(5):990–1005. doi: 10.1037//0022-3514.69.5.990. [DOI] [PubMed] [Google Scholar]
- Desai MN, Miller WC, Staples B, Bravender T. Risk factors associated with overweight and obesity in college students. J Am Coll Health. 2008;57(1):109–114. doi: 10.3200/jach.57.1.109-114. [DOI] [PubMed] [Google Scholar]
- Drewnowski A, Kurth C, Holden-Wiltse J, Saari J. Food preferences in human obesity: carbohydrates versus fats. Appetite. 1992;18(3):207–221. doi: 10.1016/0195-6663(92)90198-f. [DOI] [PubMed] [Google Scholar]
- Ganley RM. Emotion and eating in obesity: A review of the literature. International Journal of eating disorders. 1989;8(3):343–361. [Google Scholar]
- Gendall KA, Joyce PR, Sullivan PF. Impact of definition on prevalence of food cravings in a random sample of young women. Appetite. 1997;28(1):63–72. doi: 10.1006/appe.1996.0060. [DOI] [PubMed] [Google Scholar]
- Gosling SD, Mason W. Internet research in psychology. Annual review of psychology. 2015;66 doi: 10.1146/annurev-psych-010814-015321. [DOI] [PubMed] [Google Scholar]
- Greenway FL, Fujioka K, Plodkowski RA, Mudaliar S, Guttadauria M, Erickson J, Dunayevich E. Effect of naltrexone plus bupropion on weight loss in overweight and obese adults (COR-I): a multicentre, randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2010;376(9741):595–605. doi: 10.1016/s0140-6736(10)60888-4. [DOI] [PubMed] [Google Scholar]
- Greenway FL, Whitehouse MJ, Guttadauria M, Anderson JW, Atkinson RL, Fujioka K, Cowley MA. Rational design of a combination medication for the treatment of obesity. Obesity (Silver Spring) 2009;17(1):30–39. doi: 10.1038/oby.2008.461. [DOI] [PubMed] [Google Scholar]
- Hauser DJ, Schwarz N. Attentive Turkers: MTurk participants perform better on online attention checks than do subject pool participants. Behavior research methods. 2016;48(1):400–407. doi: 10.3758/s13428-015-0578-z. [DOI] [PubMed] [Google Scholar]
- Havermans RC. Pavlovian craving and overeating: a conditioned incentive model. Current Obesity Reports. 2013;2(2):165–170. [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Guilford Press; 2013. [Google Scholar]
- Heather N, Tebbutt JS, Mattick RP, Zamir R. Development of a scale for measuring impaired control over alcohol consumption: a preliminary report. J Stud Alcohol. 1993;54(6):700–709. doi: 10.15288/jsa.1993.54.700. [DOI] [PubMed] [Google Scholar]
- Helstrom AW, Blow FC, Slaymaker V, Kranzler HR, Leong S, Oslin D. Reductions in alcohol craving following naltrexone treatment for heavy drinking. Alcohol and alcoholism. 2016;51(5):562–566. doi: 10.1093/alcalc/agw038. [DOI] [PubMed] [Google Scholar]
- Herman C, Polivy J. Anxiety, restraint, and eating behavior. Journal of abnormal psychology. 1975;84(6):666. [PubMed] [Google Scholar]
- Herman C, Polivy J. Restrained eating. In: Stunkard AJ, editor. Obesity. Philadelphia: WB Saunders; 1980. pp. 208–225. [Google Scholar]
- Hoebel BG, Rada PV, Mark GP, Pothos EN. Neural systems for reinforcement and inhibition of behavior: Relevance to eating, addiction and depression. In: Kahneman E, Dierner E, Schwarz N, editors. ) Well-being: The foundation of hedonic psychology; New York, NY: Russel Sage Foundation; 1999. pp. 558–572. [Google Scholar]
- Jellinek EM. The disease concept of alcoholism. New Haven: Hillhouse Press; 1960. [Google Scholar]
- Kaplan HI, Kaplan HS. The psychosomatic concept of obesity. The Journal of nervous and mental disease. 1957;125(2):181–201. doi: 10.1097/00005053-195704000-00004. [DOI] [PubMed] [Google Scholar]
- Karlsson J, Persson LO, Sjöström L, Sullivan M. Psychometric properties and factor structure of the Three-Factor Eating Questionnaire (TFEQ) in obese men and women. Results from the Swedish Obese Subjects (SOS) study. International journal of obesity. 2000;24(12):1715. doi: 10.1038/sj.ijo.0801442. [DOI] [PubMed] [Google Scholar]
- Kerzhnerman I, Lowe MR. Correlates of subjective and objective binge eating in binge-purge syndromes. International Journal of eating disorders. 2002;31(2):220–228. doi: 10.1002/eat.10026. [DOI] [PubMed] [Google Scholar]
- Keskitalo K, Tuorila H, Spector TD, Cherkas LF, Knaapila A, Kaprio J, Perola M. The Three-Factor Eating Questionnaire, body mass index, and responses to sweet and salty fatty foods: a twin study of genetic and environmental associations. The American journal of clinical nutrition. 2008;88(2):263–271. doi: 10.1093/ajcn/88.2.263. [DOI] [PubMed] [Google Scholar]
- Konttinen H, Männistö S, Sarlio-Lähteenkorva S, Silventoinen K, Haukkala A. Emotional eating, depressive symptoms and self-reported food consumption. A population-based study. Appetite. 2010;54(3):473–479. doi: 10.1016/j.appet.2010.01.014. [DOI] [PubMed] [Google Scholar]
- Larsen JK, van Strien T, Eisinga R, Engels RC. Gender differences in the association between alexithymia and emotional eating in obese individuals. Journal of psychosomatic research. 2006;60(3):237–243. doi: 10.1016/j.jpsychores.2005.07.006. [DOI] [PubMed] [Google Scholar]
- Lowe MR. Dietary restraint and overeating. In: Fairburn CG, Brownell KD, editors. Eating disorders and obesity: A comprehensive handbook. New York, NY: The Guilford Press; 2002. pp. 88–92. [Google Scholar]
- Lyvers M. “Loss of control” in alcoholism and drug addiction: a neuroscientific interpretation. Experimental and clinical psychopharmacology. 2000;8(2):225. doi: 10.1037//1064-1297.8.2.225. [DOI] [PubMed] [Google Scholar]
- Masheb RM, Grilo CM. Emotional overeating and its associations with eating disorder psychopathology among overweight patients with binge eating disorder. International Journal of eating disorders. 2006;39(2):141–146. doi: 10.1002/eat.20221. [DOI] [PubMed] [Google Scholar]
- Mason W, Suri S. Conducting behavioral research on Amazon’s Mechanical Turk. Behavior research methods. 2012;44(1):1–23. doi: 10.3758/s13428-011-0124-6. [DOI] [PubMed] [Google Scholar]
- Massey A, Hill AJ. Dieting and food craving. A descriptive, quasi-prospective study. Appetite. 2012;58(3):781–785. doi: 10.1016/j.appet.2012.01.020. [DOI] [PubMed] [Google Scholar]
- May J, Andrade J, Batey H, Berry LM, Kavanagh DJ. Less food for thought. Impact of attentional instructions on intrusive thoughts about snack foods. Appetite. 2010;55(2):279–287. doi: 10.1016/j.appet.2010.06.014. [DOI] [PubMed] [Google Scholar]
- Meade AW, Craig SB. Identifying careless responses in survey data. Psychological methods. 2012;17(3):437. doi: 10.1037/a0028085. [DOI] [PubMed] [Google Scholar]
- Meule A, Kübler A. Food cravings in food addiction: The distinct role of positive reinforcement. Eat Behav. 2012;13(3):252–255. doi: 10.1016/j.eatbeh.2012.02.001. [DOI] [PubMed] [Google Scholar]
- Monterosso JR, Flannery BA, Pettinati HM, Oslin DW, Rukstalis M, O’Brien CP, Volpicelli JR. Predicting treatment response to naltrexone: the influence of craving and family history. The American Journal on Addictions. 2001;10(3):258–268. doi: 10.1080/105504901750532148. [DOI] [PubMed] [Google Scholar]
- Moreno S, Warren CS, Rodríguez S, Fernández MC, Cepeda-Benito A. Food cravings discriminate between anorexia and bulimia nervosa. Implications for “success” versus “failure” in dietary restriction. Appetite. 2009;52(3):588–594. doi: 10.1016/j.appet.2009.01.011. [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Wall M, Haines J, Story M, Eisenberg ME. Why does dieting predict weight gain in adolescents? Findings from project EAT-II: a 5-year longitudinal study. Journal of the American Dietetic Association. 2007;107(3):448–455. doi: 10.1016/j.jada.2006.12.013. [DOI] [PubMed] [Google Scholar]
- Ng L, Davis C. Cravings and food consumption in binge eating disorder. Eat Behav. 2013;14(4):472–475. doi: 10.1016/j.eatbeh.2013.08.011. [DOI] [PubMed] [Google Scholar]
- Nijs IM, Franken IH, Muris P. The modified Trait and State Food-Cravings Questionnaires: development and validation of a general index of food craving. Appetite. 2007;49(1):38–46. doi: 10.1016/j.appet.2006.11.001. [DOI] [PubMed] [Google Scholar]
- Opwis M, Schmidt J, Martin A, Salewski C. Gender differences in eating behavior and eating pathology: The mediating role of rumination. Appetite. 2017;110:103–107. doi: 10.1016/j.appet.2016.12.020. [DOI] [PubMed] [Google Scholar]
- Pelchat ML. Food cravings in young and elderly adults. Appetite. 1997;28(2):103–113. doi: 10.1006/appe.1996.0063. [DOI] [PubMed] [Google Scholar]
- Prince KR, Litovsky AR, Friedman-Wheller DG. Interne-mediated research: Beware of bots. The behavior therapist. 2012;35(85):87–88. [Google Scholar]
- Reas DL, Grilo CM. Current and emerging drug treatments for binge eating disorder. Expert opinion on emerging drugs. 2014;19(1):99–142. doi: 10.1517/14728214.2014.879291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers PJ, Smit HJ. Food craving and food “addiction”: a critical review of the evidence from a biopsychosocial perspective. Pharmacology Biochemistry and Behavior. 2000;66(1):3–14. doi: 10.1016/s0091-3057(00)00197-0. [DOI] [PubMed] [Google Scholar]
- Rohrer JE, Vickers-Douglas KS, Stroebel RJ. Uncontrolled eating and obesity in adult primary care patients. Obesity research & clinical practice. 2009;3(2):115–121. doi: 10.1016/j.orcp.2009.01.004. [DOI] [PubMed] [Google Scholar]
- Sher KL, Grekin ER. Alcohol and affect regulation. In: Gross J, editor. Handbook of Emotion Regulation. New York, NY: Guidford Press; 2007. pp. 560–580. [Google Scholar]
- Spitzer RL, Devlin M, Walsh BT, Hasin D, Wing R, Marcus M, Agras S. Binge eating disorder: a multisite field trial of the diagnostic criteria. International Journal of eating disorders. 1992;11(3):191–203. [Google Scholar]
- Stice E, Agras WS. Predicting onset and cessation of bulimic behaviors during adolescence: A longitudinal grouping analysis. Behavior therapy. 1998;29(2):257–276. [Google Scholar]
- Striegel-Moore RH, Rosselli F, Perrin N, DeBar L, Wilson GT, May A, Kraemer HC. Gender difference in the prevalence of eating disorder symptoms. International Journal of eating disorders. 2009;42(5):471–474. doi: 10.1002/eat.20625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroebe W, Mensink W, Aarts H, Schut H, Kruglanski AW. Why dieters fail: Testing the goal conflict model of eating. Journal of Experimental Social Psychology. 2008;44(1):26–36. [Google Scholar]
- Tiffany ST. A cognitive model of drug urges and drug-use behavior: role of automatic and nonautomatic processes. Psychol Rev. 1990;97(2):147–168. doi: 10.1037/0033-295x.97.2.147. [DOI] [PubMed] [Google Scholar]
- Tiffany ST, Conklin CA. A cognitive processing model of alcohol craving and compulsive alcohol use. Addiction. 2000;95(Suppl 2):S145–153. doi: 10.1080/09652140050111717. [DOI] [PubMed] [Google Scholar]
- Turner SA, Luszczynska A, Warner L, Schwarzer R. Emotional and uncontrolled eating styles and chocolate chip cookie consumption. A controlled trial of the effects of positive mood enhancement. Appetite. 2010;54(1):143–149. doi: 10.1016/j.appet.2009.09.020. [DOI] [PubMed] [Google Scholar]
- Van Strien T, Frijters JE, Bergers G, Defares PB. The Dutch Eating Behavior Questionnaire (DEBQ) for assessment of restrained, emotional, and external eating behavior. International Journal of eating disorders. 1986;5(2):295–315. [Google Scholar]
- Villarejo C, Fernandez-Aranda F, Jimenez-Murcia S, Penas-Lledo E, Granero R, Penelo E, Menchon JM. Lifetime obesity in patients with eating disorders: increasing prevalence, clinical and personality correlates. Eur Eat Disord Rev. 2012;20(3):250–254. doi: 10.1002/erv.2166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wadden TA, Volger S, Tsai AG, Sarwer DB, Berkowitz RI, Diewald LK, Vetter M. Managing obesity in primary care practice: an overview with perspective from the POWER-UP study. Int J Obes (Lond) 2013;37(Suppl 1):S3–11. doi: 10.1038/ijo.2013.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinberg JD, Freese J, McElhattan D. Comparing Data Characteristics and Results of an Online Factorial Survey between a Population-Based and a Crowdsource-Recruited Sample. Sociological Science. 2014;1:292–310. [Google Scholar]
- Weingarten HP, Elston D. Food cravings in a college population. Appetite. 1991;17(3):167–175. doi: 10.1016/0195-6663(91)90019-o. [DOI] [PubMed] [Google Scholar]
- Williamson DF, Serdula MK, Anda RF, Levy A, Byers T. Weight loss attempts in adults: goals, duration, and rate of weight loss. Am J Public Health. 1992;82(9):1251–1257. doi: 10.2105/ajph.82.9.1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Obesity and Overweight Fact Sheet. 2016 Retrieved from http://www.who.int/mediacentre/factsheets/fs311/en/


