Abstract
Background
Increasing use of nurse practitioners (NPs) and physician assistants (PAs) is a possible solution to the shortage of primary care providers (PCPs) in the US, but the quality of care they provide is not well understood.
Methods
Since the scope of practice of the three provider types is similar in the Veterans Health Administration (VA), we determined whether patients managed by primary care NPs, PAs or physicians had similar HbA1c levels at comparable times in the natural history of diabetes. Our retrospective cohort study examined Veterans with diabetes newly-diagnosed in 2008, continuous primary care 2008–2012, and >75% of primary care visits with an NP, PA or physician.
Results
The 19,238 patients were 95.3% male, 77.7% white, and had mean age 68.5 years; 14.7%, 7.1%, and 78.2% of patients were managed by NPs, PAs and physicians, respectively. Median HbA1c was comparable at diagnosis (6.6%, 6.7%, 6.7%, p>0.05) and after 4 years (all 6.5%, p>0.5). HbA1c levels at initiation of the first (7.5–7.6%) and second (8.0–8.2%) oral medication for patients of NPs and PAs compared to that of physicians was also similar after adjusting for patient characteristics (all p>0.05). NPs started insulin at a lower HbA1c (9.4%) than physicians (9.7%), which remained significant after adjustment, p<0.05.
Conclusions
At diagnosis and during 4 years of follow-up, diabetes management by NPs and PAs was comparable to management by physicians. The VA model for roles of NPs and PAs may be broadly useful to help meet the demand for PCPs in the US.
Keywords: diabetes, midlevel providers, nurse practitioner, physician assistant, primary care
Introduction
Diabetes is a major health problem in the United States. More than 29 million Americans have diabetes, with 1.4 million newly-diagnosed in 20131. In 2012, the American Diabetes Association (ADA) estimated that the total economic burden of diagnosed diabetes in the US was $176 billion in direct costs2.
After enactment of the Affordable Care Act (ACA), more Americans obtained access to health care. However, less than one third of physicians in the US currently practice in a primary care specialty3. One study estimated that the US requires an additional 46,000 primary care providers (PCPs) by 2025 in order to meet patient demands4. The shortfall in PCPs has spurred interest in the role of nurse practitioners (NPs) and physician assistants (PAs) in the primary care management of chronic diseases such as diabetes. While the cost of utilizing NPs and PAs is lower than physicians5, whether NPs, PAs and physicians deliver similar quality of care is poorly understood.
Several studies have suggested that patients managed by NPs and PAs have outcomes similar to those of physicians6–11. However, due to scope of practice laws3,12, only a few studies included direct comparisons between NPs or PAs and physicians with similar independence and patient populations. Comparisons of diabetes care in particular have mainly been limited to cross-sectional analyses of single HbA1c levels without comparisons at similar time points in the natural history of the disease9,13.
We chose the Veterans Health Administration (VHA) as a model health care system in which to compare diabetes outcomes between patients managed by primary care NPs, PAs and physicians. Of the approximately 8.3 million patients seen at the VA each year14, an estimated one in five has a diagnosis of diabetes15. The VHA is the largest integrated health care system, as well as the largest employer of NPs and PAs in the nation16,17. The majority of NPs and PAs in the VHA primary care setting are responsible for patient panels similar to those of physicians, and can prescribe non-controlled medications, place orders, and document without physician co-signatures18. In 2010, up to 29% of VHA primary care provider visits in 2010 were attended solely by NPs and PAs, with diabetes being the third most common primary care visit diagnosis for physicians and NPs, and fourth among PAs18.
Our study utilized the national VHA Corporate Data Warehouse (CDW) database to compare NP, PA and physician management of patients with diabetes who were at comparable stages of their natural history – at diagnosis in 2008, during 4 years of follow-up, and at initiation of oral medications and insulin.
METHODS
Study design
We conducted a retrospective analysis to compare HbA1c levels in patients managed by primary care NPs, PAs or physicians. All patients were newly-diagnosed with diabetes in 2008, had four years of consistent primary care follow-up, and had annual HbA1c levels documented through 2012. This study was approved by the Emory University Institutional Review Board and the Atlanta VA Research and Development Committee.
Database
The CDW includes patient, visit, and provider information from all VHA encounters. Access to the CDW is obtained through the VA Informatics and Computing Infrastructure (VINCI).
Patient selection
“Primary care” was defined by use of the VHA database “clinic stop codes” for primary care/general medicine; women’s health; geriatric primary care; shared primary care; chronic infectious disease primary care; and spinal cord injury primary care.
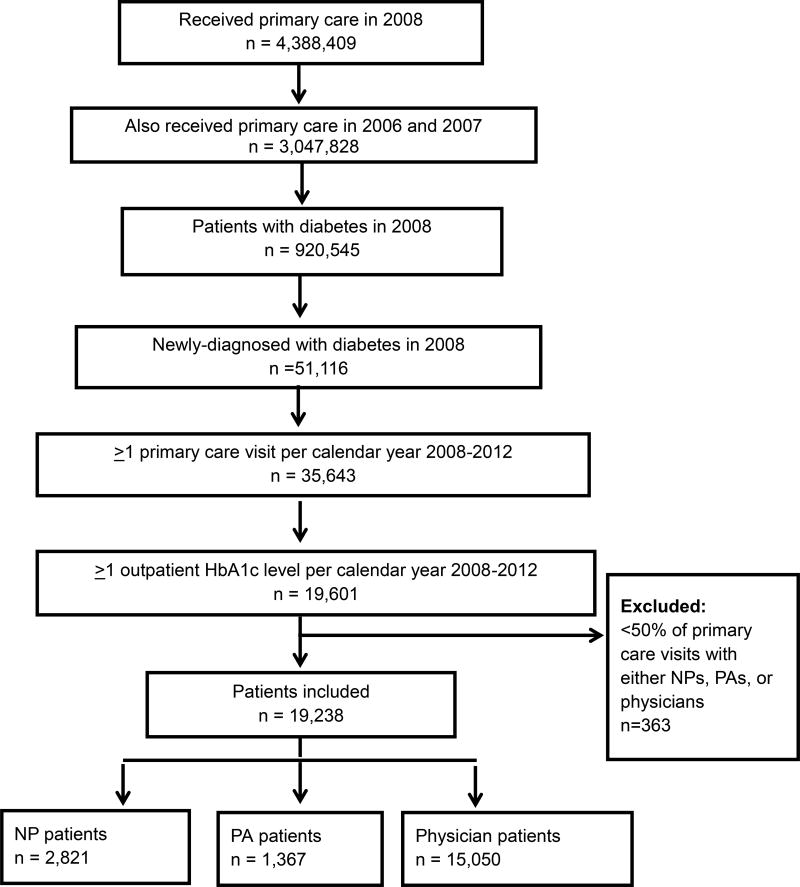
We defined a patient as having newly-diagnosed diabetes in 2008 if he/she had at least one PCP visit per calendar year (CY) from 2006–2008 and met any one of the following validated criteria19,20 in 2008 but not in 2006–2007: (i) use of ICD-9 code 250.xx at a primary care visit, (ii) any use of 250.xx twice in 2008, and/or (iii) outpatient prescription of a diabetes drug. The diagnosis date was the earliest date in 2008 that the patient met one of the three criteria above. We further required patients to have at least one PCP visit in each year from 2006–2012 and within 6 months of diagnosis to ensure that patients had an adequate amount of contact with PCPs; at least one HbA1c measurement within 12 weeks before or 6 weeks after diagnosis; and at least one HbA1c per year from 2008–2012. Patients were categorized as managed by NPs, PAs or physicians if they had more than 50% of PCP visits with one of the three provider types. A total of 19,238 patients were found to meet these criteria (Appendix Figure1).
Patient demographics / characteristics
Of the 19,238 patients selected, 17,288 (89.9%) had self-identified race data available. BMI was calculated at each visit for 16,727 patients who had height and weight information documented. A mean BMI value was calculated over time for each patient. Patients’ Charlson Comorbidity Index (CCI) scores were calculated using ICD-9 diagnosis codes as previously described21,22. We also identified whether patients had seen a diabetes specialist based upon visits to a diabetes clinic.
Medication Initiation
Initiation of oral antihyperglycemic medication or insulin was defined as the first outpatient prescription of medications with national drug codes HS502 (indicating oral agents) or HS501 (insulin agents), respectively, on or after the diagnosis date in 2008. Initiation of a second oral antihyperglycemic drug was determined as the issue date of a second HS502 drug of a different name. Inpatient prescriptions were not included.
HbA1c results
The HbA1c measurement closest to the diagnosis date and within 12 weeks before to 6 weeks after diagnosis was considered the HbA1c at diagnosis. Within each time period, values were averaged if patients had multiple tests. We also calculated a 5-year mean HbA1c of all levels reported from diagnosis in 2008 through four years of follow-up in 2012 for each patient. HbA1c at medication initiation utilized measurements within 12 weeks before to 6 weeks after prescription of the first oral antihyperglycemic medication, second oral medication, and/or insulin; approximately 98% of patients with diabetes medication prescriptions had HbA1c tested within this time frame.
Statistical Analysis
For group comparisons among different provider types, Chi-square tests were used for categorical variables; ANOVA and two-tailed t-tests to evaluate means of continuous variables; and Kruskal-Wallis and Wilcoxon tests to evaluate median values of outcomes which were not normally distributed. Statistical analysis of HbA1c outcomes is reported as both median and mean values due to right skewing of HbA1c distributions. Multivariate regression analyses were conducted for HbA1c outcomes to adjust for variations in patient characteristics. All statistical analyses were conducted using R and a p-value of <0.05 was considered statistically significant.
RESULTS
Diabetes cohort
In 2008, 19,238 veterans had two years of primary care before a new diagnosis of diabetes, continuity of primary care from 2006–2012, an HbA1c at diagnosis and at least one HbA1c per year from 2008–2012, and a majority of visits with a single provider type (Appendix Figure 1). Of these, 2,821 were managed by NPs, 1,367 by PAs, and 15,050 by physicians. Concordance between visit provider type and each patient’s designated managing provider type (i.e., for a patient managed by NPs by our criteria, the mean percent of primary care visits seen by an NP) was high at 82.3%, 78.9% and 92% for patients of NPs, PAs and physicians, respectively (Appendix Table 1). Patients managed by NPs and PAs had 14.5% and 15% of primary care visits with physicians, respectively.
Demographics
Patient characteristics are shown in Table 1. All values were clinically comparable although some were statistically different. NP patients were slightly older than physician patients (68.8 vs 68.4 years). NPs also managed a slightly lower percentage of male patients than physicians (94.3% vs. 95.5%). PAs had a higher percentage of white patients than physicians did (81.0% vs. 77.4%). NPs had patients with higher BMI compared to patients of physicians (32.6 vs. 32.2 kg/m2). The patients of NPs, PAs and physicians had similar comorbidity, with median CCI scores of 0.0 in the two years prior to diabetes diagnosis, and CCI scores over the entire study period 2006–2012 of 1.0.
Table 1.
Demographics and characteristics of patients with newly-diagnosed diabetes in 2008, by managing provider type
| NPs | PAs | Physician | P-values | ||||
|---|---|---|---|---|---|---|---|
| n=2,821 | n=1,367 | n=15,050 | ANOVA/ KW |
NP vs. Phys |
PA vs. Phys |
NP vs. PA |
|
| Age at diagnosis mean years ± SD | 68.8 ± 10.1 | 68.9 ± 10.0 | 68.4 ± 10.5 | 0.033 | 0.028 | 0.075 | 0.886 |
| Male, n (%) | 2,659 (94.3) | 1,313 (96.0) | 14,367 (95.5) | <0.001 | <0.001 | 0.170 | 0.002 |
| Race Available n (%) | 2,495 (88.4) | 1,197 (87.6) | 13,596 (90.3) | <0.001 | 0.002 | 0.001 | 0.438 |
| White (%) | 1,950 (78.2) | 969 (81.0) | 10,516 (77.3) | ||||
| Black/African American (%) | 398 (16.0) | 157 (13.1) | 2,150 (15.8) | 0.020 | 0.220 | 0.016 | 0.077 |
| Other (%) | 147 (5.9) | 71 (5.9) | 930 (6.8) | ||||
| BMI, mean kg/m2 ± SD | 32.5 ± 5.7 | 32.2 ± 5.4 | 32.2 ± 5.6 | 0.014 | 0.004 | 0.941 | 0.062 |
| CCI 06–08, median (quartiles) | 0 (0,1) | 0 (0,1) | 0 (0,1) | 0.271 | 0.115 | 0.592 | 0.592 |
| CCI 06–12, median (quartiles) | 1 (0,3) | 1 (0,3) | 1 (0,3) | 0.066 | 0.070 | 0.940 | 0.770 |
Age at diagnosis, gender, race, body mass index, and Charlson Comorbidity Index scores for patients newly-diagnosed with diabetes in 2008, continuity of primary care from 2008 through 2012, and HbA1c levels recorded at diagnosis and at least once every calendar year from 2008–2012, who were managed mainly by NPs, PAs, or physicians. Race ratios and BMI means were calculated using total number of patients with race data and BMI data available. ANOVA and t-tests were used to compare means, Chi-square to compare percentages, Kruskal Wallis and Wilcoxon to compare medians. NP = nurse practitioner, PA = physician assistant, MD = physician (MD and DO), BMI = body mass index, CCI = Charlson Comorbidity Index.
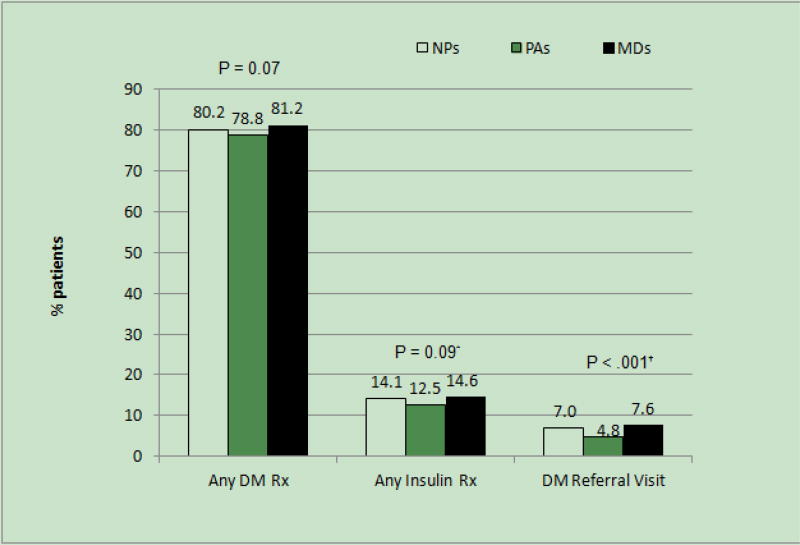
PAs had 4.8% of patients visit a diabetes specialist clinic, lower compared to the 7.0% of NP patients and 7.6% of physician patients (Figure 1). Neither NPs (80.2%) nor PAs (78.8%) had a significantly different percentage of patients prescribed any glucose-lowering medications compared to physicians (81.2%) (Figure 1). However, PAs had significantly fewer patients using insulin than physicians did (12.5% vs 14.6%).
Figure 1. Percent of patients prescribed diabetes medications, and referred to diabetes clinic, from 2008–2012 by managing provider type.
Bar graphs depicting: percent of patients who completed at least one diabetes specialist clinic visit between 2008–2012; percent of patients who were prescribed any diabetes medication and/or insulin. DM = diabetes, Rx = prescription. Group P values shown were determined by Chi-square test.
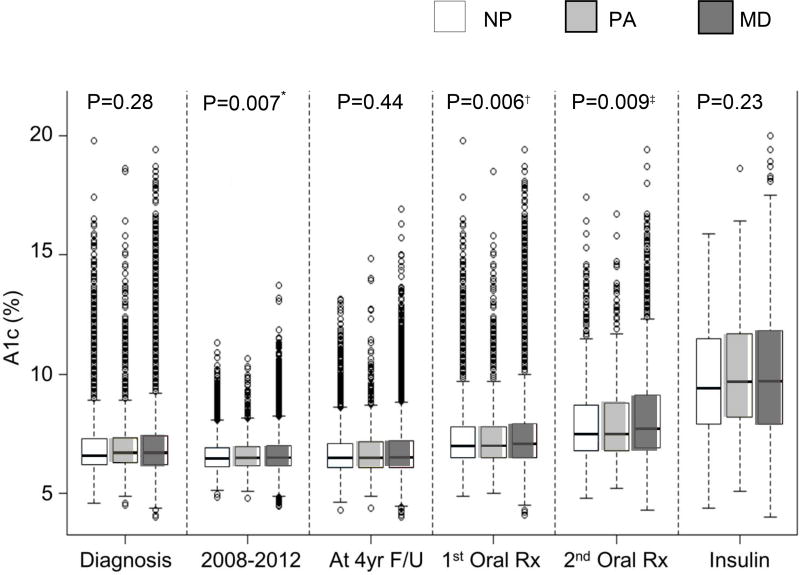
HbA1c levels during the natural history of diabetes
Patients of NPs, PAs and physicians had similar median HbA1c levels both at diagnosis (6.6%, 6.7%, and 6.7%) (Figure 2) and after four years of primary care follow-up (all 6.5%). The median of each patient’s 5-year mean HbA1c (median 5-year mean HbA1c) from diagnosis in 2008 through 2012 for NPs was 6.4%, slightly lower than the median 5-year mean HbA1c of 6.5% for patients of physicians. The median 5-year mean HbA1c level for patients of PAs was not different compared to NPs or physicians.
Figure 2. Median HbA1c levels at systematic time points in the natural history of diabetes in patients newly-diagnosed in 2008.
Box and whisker plots of median patient HbA1c levels compared between patients at various time points in the natural history of diabetes: 1) within 12 weeks before/6 weeks after diabetes diagnosis, 2) each patient’s mean HbA1c over 5 years from 2008–2012, 3) after four years of primary care follow-up in 2012, 4) at initiation of first oral antihyperglycemic medication, 5) at initiation of second oral antihyperglycemic medication, and 6) at initiation of insulin. Boxes include 25th–75th percentile, dashed lines indicate min-max range, dots represent outliers. Group P values shown were calculated using Kruskal-Wallis tests. Wilcoxon tests were used to compare HbA1c between two provider groups.
A total of 15,841 patients were prescribed glucose-lowering medications. Of these, 15,301 (96%) had at least one oral medication, 5,889 (37%) at least two oral medications, and 2,769 (17%) were prescribed insulin. Among these patients, 14,635 (96%) had an HbA1c level at initiation of the first oral drug; 5,271 at initiation of the second oral drug (89%); and 2,245 (81%) at initiation of insulin.
Median HbA1c at initiation of the first and second oral drug was significantly lower in patients of NPs (7.0% and 7.5%) compared to that of physicians (7.1% and 7.7%) (Figure 2), but NPs and physicians started patients on insulin at similar HbA1c levels (9.4% and 9.7%). There was no difference in median HbA1c levels at initiation of oral drugs or insulin between PAs and physicians.
Regression analysis showed that patient age was inversely associated with HbA1c level during the duration of the study, and during initiation of all diabetes medications. Being male and African American was independently associated with higher HbA1c throughout the duration of the study, and during initiation of all diabetes medications. After adjusting for these patient characteristics, the differences in HbA1c levels at initiation of the first and second oral medications between NPs and physicians became non-significant (Table 2). However, the difference in HbA1c levels at initiation of insulin between NPs and physicians remained significant (Table 2).
Table 2.
Multiple regression analyses of 5-year patient mean HbA1c, HbA1c at initiation of first oral medication, second oral medication, and insulin
| 5-year mean 2008–2012 |
1st oral drug | 2nd oral drug | Insulin | |||||
|---|---|---|---|---|---|---|---|---|
| coefficient | p | coefficient | p | coefficient | p | coefficient | p | |
| Provider | ||||||||
| NP (ref=MD) | −0.028 | 0.46 | −0.061 | 0.18 | −0.140 | 0.08 | −0.359 | 0.03 |
| PA (ref=MD) | 0.028 | 0.595 | 0.030 | 0.64 | −0.016 | 0.89 | 0.049 | 0.84 |
| Age (years) | −0.025 | <0.001 | −0.023 | <0.001 | −0.031 | <0.001 | −0.018 | 0.004 |
| CCI | 0.003 | 0.66 | −0.009 | 0.26 | −0.061 | <0.001 | −0.200 | <0.001 |
| BMI | 0.005 | 0.046 | −0.001 | 0.88 | −0.001 | 0.91 | −0.012 | 0.22 |
| Male | 0.278 | <0.001 | 0.258 | 0.001 | 0.332 | 0.01 | 0.663 | 0.008 |
| Race | ||||||||
| Black (ref=white) | 0.618 | <0.001 | 0.485 | <0.001 | 0.418 | <0.001 | 1.153 | <0.001 |
| Other (ref=white) | 0.115 | 0.03 | 0.176 | 0.006 | 0.146 | 0.22 | 0.184 | 0.50 |
| Diabetes clinic | ||||||||
| Yes (ref=never) | 0.723 | <0.001 | 0.736 | <0.001 | 0.519 | <0.001 | 0.357 | 0.04 |
Multiple regression analyses of each patient’s 5-year mean HbA1c, HbA1c at initiation of first oral medication, second oral medication and insulin for patients with newly-diagnosed diabetes in 2008 and managed by primary care NPs, PAs or physicians. Coefficients indicate the change in HbA1c level associated with gender, race, diabetes clinic referral, age, Charlson Comorbidity Index and BMI. CCI7 = Charlson Comorbidity Index score calculated from visit diagnoses in 2008 through 2012, DM clinic = referral to diabetes clinic.
There was no difference in the median time from diabetes diagnosis to initiation of oral drugs or insulin between any of the three provider types (Appendix Table 2).
DISCUSSION
The results of our study demonstrate that primary care NPs and PAs provide glycemic management that is comparable to that of physicians for patients who had newly-diagnosed diabetes with four years of follow-up. There was no difference in HbA1c levels at diagnosis, initiation of the first and second oral medication, or after four years of primary care follow-up between NPs, PAs or physicians, after adjusting for patient characteristics. Patients of NPs were started on insulin at slightly lower HbA1c levels than patients of physicians after multivariate regression analyses. However, despite statistical significance, these differences in HbA1c were not clinically significant, much less than the 0.5% HbA1c difference that corresponds to an increased risk of developing diabetic retinopathy, as shown in the Diabetes Control and Complications Trial23.
The minimal differences in HbA1c outcomes are unlikely to be due to differences in patient complexity. Median Charlson Comorbidity Index scores within the two years prior to diagnosis, as well as throughout 2006–2012, were not significantly different between patients of NPs and physicians. NPs and physicians also had comparable percentages of patients with diabetes specialist visits and prescriptions for insulin. However, PAs had fewer patients with diabetes specialist visits, and fewer patients using insulin compared to physicians, suggesting that patients of PAs either were managed better with oral agents, or might have been less complex in terms of diabetes management.
The HbA1c trend of our patient population overall shows good control, with median HbA1c four years after diagnosis between 6.5 and 7%. This brings to question whether process measures within the VHA regarding diabetes management could explain some of our study findings. While the highly-integrated structure of VHA primary care differs from that in other primary care settings, especially in rural regions of the US, we are not aware of any particular algorithm followed systematically through the VHA that assigns a particular demographic of patients preferentially to PAs, NPs or physicians. Although the VHA has diabetes management guidelines24, no specific algorithm is used uniformly across the health system. Although veterans tend to be older and to have more complex disease and comorbidities than the general US population, previous studies have shown that veterans tend to have better chronic disease outcomes than their non-veteran counterparts25. The cost of care is also lower in the VHA compared to non-VA settings26. Further prospective, randomized, controlled trials would be helpful to determine the extent to which our findings will apply to other practice environments.
The results of our study are consistent with prior research comparing management of diabetes between NPs and physicians. Mundinger et al conducted a randomized trial in which urgent care and emergency room patients with diabetes who lacked a regular primary care provider were assigned to NPs (n=58) or physicians (n=46) in four community-based primary care clinics in New York City9. Six months after the first primary care visit, NPs and physicians had similar percentages of patients with insufficiently-controlled diabetes, and the groups had comparable HbA1cs of 9.5% vs. 9.4%. Jackson et al found that inclusion of NPs within a primary care practice was associated with patient HbA1c levels that were 0.3% lower than in practices without NPs13. Kuo et al conducted two retrospective studies of patients with diabetes cared for solely by primary care NPs or primary care physicians. Prevalence of patient comorbidities like heart disease, hypertension, metabolic disorders were similar between the two patient groups. They found that HbA1c levels and preventable diabetes-related hospitalizations were comparable between the two provider groups27, and adjusted Medicare spending per patient between the two provider groups was similar as well11.
Processes of care have been found to be mixed when comparing management by NPs to that of physicians. Lenz et al found that NPs were more likely than physicians to document diabetes education, medication education, and urinalysis results, but not foot and cardiovascular examinations, glucose and creatinine levels, or ophthalmologist referrals28. Ohman-Strickland et al found that family medicine practices that employed NPs were more likely to measure HbA1c, lipid, and urine microalbumin levels compared to practices without NPs29, although the groups were comparable in percentage of patients with HbA1c <7.0%. Kuo et al noted no significant difference in lipid screens and foot examinations, but significantly higher rates of eye examinations and vaccinations for patients cared for by NPs than physicians11.
The strengths of our study include the incorporation of longitudinal data from medical centers across the nation, a large sample size, and a design which permitted comparison of HbA1c outcomes in patients who were at similar stages of their diabetes natural history and management. Our study also compared NPs, PAs and physicians who had similar prescribing privileges and scopes of practice. This allowed us to evaluate NPs and PAs who had levels of independence, responsibilities, and patient panels similar to those of their physician counterparts – a dimension which had been lacking in prior studies. While our operative definition of provider “ownership” as having greater than 50% of primary care visits with either NPs, PAs or physicians could allow patients to receive some of their care from one of the other two provider types, “ownership” and visit provider type concordance was greater than 75% for all groups.
Limitations to our study include its retrospective design, difference in sample size across provider groups, lack of female patients, and non-uniform testing of HbA1c. We do not know if NPs, PAs and physicians had similar allotted appointment time with patients. While most NPs and PAs in the VHA see patients without immediate, during-visit feedback from physicians on management, how frequent post-visit MD input is incorporated into diabetes management by NPs and PAs is not known. Additionally, while our evaluation was restricted to the year of diagnosis and the first four years of follow-up, management appeared to be comparable in the (delayed) initiation of insulin. It is possible that patients who received insulin at higher levels of HbA1c were diagnosed later in their natural history of disease. Finally, the findings of comparable management of diabetes in our study may not be generalizable to management of other chronic disorders and to other care settings
While glycemic control is one important aspect in the management of diabetes, this initial study did not address questions related to adverse effects of medications, or management of cardiovascular risk factors. While hypoglycemia is a common side effect of management, patient laboratory results would not necessarily be representative of the periodic episodes of mild to moderate hypoglycemia in outpatients which may or may not be reflected in the home blood glucose monitoring results, which patients bring to visits irregularly and are typically made by patient recall at visits. As a result, the true incidence of hypoglycemia is difficult to assess accurately, and was not included in this study. Further studies need to be conducted to compare diabetes care-specific process measures, blood pressure and hyperlipidemia management, and the incidence of diabetes-related complications such as microvascular end-organ damage, cardiaovascular events, and hospitalizations among patients managed by NPs, PAs or physicians. Of equal importance is assessment of patient satisfaction among patients with diabetes managed by NPs and PAs vs. MDs.
From a health quality and policy standpoint, our results demonstrate that independently-practicing NPs and PAs, within a highly integrated health care system, are able to perform as well as physicians in management of diabetes at diagnosis and during 4 years of follow-up care. These findings indicate that there could be benefits from expanding the roles of NPs and PAs in patient management both within and outside of the VA – and that the VA model for use of NPs and PAs may be broadly useful to help meet the demand for primary care providers in the US.
Highlights.
Primary care nurse practitioners, physician assistants, and physicians at the Veterans Health Administration care for diabetic patients with similar medical complexity.
Patients managed by nurse practitioners, physician assistants, and physicians had comparable HbA1c at diagnosis (6.6–6.7%), initiation of first (7.5–7.6%) and second (8.0–8.2%) oral medications, initiation of insulin (9.4–9.7%), and after 4 years of follow-up (6.5).
Acknowledgments
All authors had access to the data and a role in writing the manuscript
Funding Sources
Drs. Rhee, Phillips, Olson, and Tomolo are supported in part by the VA. This work is not intended to reflect the official opinion of the VA or the US government.
This work was supported in part by FDA award RO1FD003527 (L.S.P), VA awards HSR&D IIR 07-138 (L.S.P, S.L.J.), and I01-CX001025 and I01-01BX003340 (L.S.P.), NIH awards R21DK099716 (L.S.P., Q.L., and S.L.J.), DK066204 (L.S.P.), U01 DK091958 (L.S.P. and M.K.R.), U01 DK098246 (L.S.P. and D.E.O.), R21 NS091630 (Q.L.), and a Cystic Fibrosis Foundation award PHILLI12A0 (L.S.P). The sponsors had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
The authors declare that there is potential duality of interest associated with this manuscript. With regard to potential conflicts of interest, within the past five years, Dr. Phillips has served on Scientific Advisory Boards for Boehringer Ingelheim, Profil and Janssen, and has or had research support from Merck, Amylin, Eli Lilly, Novo Nordisk, Sanofi, PhaseBio, Roche, Abbvie, Glaxo SmithKline, Janssen, Vascular Pharmaceuticals, Glaxo SmithKline, Astra Zeneca, and the Cystic Fibrosis Foundation. In the past, he was a speaker for Novartis and Merck, but not for the last five years. Darin E Olson has research support from Novo Nordisk and Amylin, and Qi Long receives support from NIH, PCORI, NSF, AHA, and the Cystic Fibrosis Foundation and served as a consultant for Eisai. Sandra Jackson received support from Amylin. These activities involve diabetes, but have nothing to do with this manuscript. After the study reported here was completed, Dr. Phillips founded a company, Diasyst Inc., which aims to develop and commercialize diabetes management programs.
Appendix
Appendix Figure 1. Consort diagram.
51,116 veterans had two years of primary care before a new diagnosis of diabetes (diabetes diagnosis was defined by (i) use of ICD-9 code 250.xx at a primary care visit, (ii) any use of 250.xx twice in 2008, and/or (iii) outpatient prescription of a diabetes drug). Of these, 35,643 had continuity of primary care from 2006–2012 defined as at least one primary care attending visit per calendar year, and 19,601 also had an HbA1c at diagnosis and at least one A1c per year from 2008–2012. Less than 2% of patients (n=363) lacked a majority of visits with one particular provider type. Because such a small percentage of patients had “mixed” provider type care, we included only the 19,238 patients who were managed either by NPs, PAs, or physicians. Of these, 2,821 were managed by NPs, 1,367 managed by PAs, and 15,050 managed by physicians. NP = nurse practitioner, PA = physician assistant, MD = physician (MD and DO).
Appendix Table 1.
Managing provider and visit provider concordance for patients of NPs, PAs or physicians
| Patient managing provider type | NP | PA | Physician |
|---|---|---|---|
| Total primary care visits per patient, mean | 19.6 | 19.7 | 19.4 |
| Primary care visits with NPs, mean (%) | 16.0 (82.3) | 1.2 (6.1) | 1.1 (5.3) |
| Primary care visits with PAs, mean (%) | 0.6 (3.1) | 15.4 (78.9) | 0.6 (2.8) |
| Primary care visits with Physicians, mean (%) | 3.0 (14.5) | 3.1 (15.0) | 17.7 (92) |
Among patients designated as being managed by nurse practitioners (NPs), physician assistants (PAs) or physicians by our criteria, mean number and percent of total primary care visits (per patient) from 2006–2012 that were staffed by NPs, PAs or physicians.
Appendix Table 2.
Median time in days from diagnosis to medication initiation in patients with newly-diagnosed diabetes managed by NPs, PAs or physicians
| Days from diagnosis to medication prescription, median, (25th, 75th percentiles) |
NPs | PAs | Physicians | p value, group |
|---|---|---|---|---|
| 1st oral Rx | 0 (0, 8) | 0 (0, 29) | 0 (0, 28) | 0.429 |
| 2nd oral Rx | 556 (154, 1008) | 640 (209,1102) | 560 (173, 1030) | 0.134 |
| insulin Rx | 628 (4, 1177) | 559 (1.25, 1117) | 537 (1, 1123) | 0.481 |
Time in days from diagnosis to initiation of diabetes medications in patients with newly-diagnosed diabetes who were managed by NPs, PAs or physicians. Median time to medication initiation was compared with Kruskal Wallis and Wilcoxon test
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributions
YY and LP researched the data, QL performed the statistical analyses, YY drafted the manuscript, and LP, AT, SJ, DO, MR, and all of the other authors contributed to the discussion and reviewed/edited the manuscript.
The authors gratefully acknowledge the contributions of Christine Jasien, Atlanta VAMC who assisted the authors with obtaining VINCI data. We also acknowledge Qing He, Emory School of Public Health, for assistance with data analysis. Both of their contributions was without compensation.
Lawrence Phillips (Atlanta VA Medical Center and Emory University School of Medicine) had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentations
This work was presented in part at the American Diabetes Association meeting in June, 2014.
Disclosures
Other authors have no potential conflicts of interest to declare.
References
- 1.Centers for Disease Control and Prevention. National Diabetes Statistics Report: Estimates of diabetes and its burden in the United States. Atlanta, GA: 2014. 2014. [Google Scholar]
- 2.American Diabetes Association. Economic costs of diabetes in the U.S. in 2012. Diabetes care. 2013;36:1033–46. doi: 10.2337/dc12-2625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Iglehart JK. Expanding the role of advanced nurse practitioners--risks and rewards. The New England journal of medicine. 2013;368:1935–41. doi: 10.1056/NEJMhpr1301084. [DOI] [PubMed] [Google Scholar]
- 4.Petterson SM, Liaw WR, Phillips RL, Jr, Rabin DL, Meyers DS, Bazemore AW. Projecting US primary care physician workforce needs: 2010–2025. Annals of family medicine. 2012;10:503–9. doi: 10.1370/afm.1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Physician Compensation and Production Survey 2012 Report Based on 2011 Data. Englewood, CO: Medical Group Management Association; 2012. [Google Scholar]
- 6.Spitzer WO, Sackett DL, Sibley JC, et al. 1965–1990: 25th anniversary of nurse practitioners. A classic manuscript reprinted in celebration of 25 years of progress. The Burlington randomized trial of the nurse practitioner. 1971–2. Journal of the American Academy of Nurse Practitioners. 1990;2:93–9. doi: 10.1111/j.1745-7599.1990.tb00786.x. [DOI] [PubMed] [Google Scholar]
- 7.Brown SA, Grimes DE. A meta-analysis of nurse practitioners and nurse midwives in primary care. Nursing research. 1995;44:332–9. [PubMed] [Google Scholar]
- 8.Horrocks S, Anderson E, Salisbury C. Systematic review of whether nurse practitioners working in primary care can provide equivalent care to doctors. BMJ. 2002;324:819–23. doi: 10.1136/bmj.324.7341.819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mundinger MO, Kane RL, Lenz ER, et al. Primary care outcomes in patients treated by nurse practitioners or physicians: a randomized trial. JAMA : the journal of the American Medical Association. 2000;283:59–68. doi: 10.1001/jama.283.1.59. [DOI] [PubMed] [Google Scholar]
- 10.Kamps AW, Brand PL, Kimpen JL, et al. Outpatient management of childhood asthma by paediatrician or asthma nurse: randomised controlled study with one year follow up. Thorax. 2003;58:968–73. doi: 10.1136/thorax.58.11.968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kuo YF, Goodwin JS, Chen NW, Lwin KK, Baillargeon J, Raji MA. Diabetes Mellitus Care Provided by Nurse Practitioners vs Primary Care Physicians. J Am Geriatr Soc. 2015;63:1980–8. doi: 10.1111/jgs.13662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Professional Issues: PA Scope of Practice. Alexandria, VA: American Academy of Physician Assistants; 2011. Oct, [Google Scholar]
- 13.Jackson GL, Lee SY, Edelman D, Weinberger M, Yano EM. Employment of mid-level providers in primary care and control of diabetes. Primary care diabetes. 2011;5:25–31. doi: 10.1016/j.pcd.2010.09.005. [DOI] [PubMed] [Google Scholar]
- 14. [Accessed December 10, 2013];About VHA. 2011 at http://www.va.gov/health/aboutVHA.asp#datasource.
- 15.Miller DR, Safford MM, Pogach LM. Who has diabetes? Best estimates of diabetes prevalence in the Department of Veterans Affairs based on computerized patient data. Diabetes care. 2004;27(Suppl 2):B10–21. doi: 10.2337/diacare.27.suppl_2.b10. [DOI] [PubMed] [Google Scholar]
- 16.Woodmansee DJ, Hooker RS. Physician assistants working in the Department of Veterans Affairs. JAAPA : official journal of the American Academy of Physician Assistants. 2010;23:41–4. doi: 10.1097/01720610-201011000-00008. [DOI] [PubMed] [Google Scholar]
- 17.Fletcher CE, Copeland LA, Lowery JC, Reeves PJ. Nurse practitioners as primary care providers within the VA. Military medicine. 2011;176:791–7. doi: 10.7205/milmed-d-10-00329. [DOI] [PubMed] [Google Scholar]
- 18.Morgan PA, Abbott DH, McNeil RB, Fisher DA. Characteristics of primary care office visits to nurse practitioners, physician assistants and physicians in United States Veterans Health Administration facilities, 2005 to 2010: a retrospective cross-sectional analysis. Human resources for health. 2012;10:42. doi: 10.1186/1478-4491-10-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Miller DR, Pogach L. Longitudinal approaches to evaluate health care quality and outcomes: the Veterans Health Administration diabetes epidemiology cohorts. Journal of diabetes science and technology. 2008;2:24–32. doi: 10.1177/193229680800200105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Twombly JG, Long Q, Zhu M, et al. Validity of the primary care diagnosis of diabetes in veterans in the southeastern United States. Diabetes research and clinical practice. 2011;91:395–400. doi: 10.1016/j.diabres.2010.11.001. [DOI] [PubMed] [Google Scholar]
- 21.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Journal of chronic diseases. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 22.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Medical care. 2005;43:1130–9. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 23.The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. The Diabetes Control and Complications Trial Research Group. The New England journal of medicine. 1993;329:977–86. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 24.Department of Veterans Affairs. VA/DoD Clinical practie guideline for the management of type 2 diabetes mellitus in primary care. 2017 Apr; ed2017. [Google Scholar]
- 25.Asch SM, McGlynn EA, Hogan MM, et al. Comparison of quality of care for patients in the Veterans Health Administration and patients in a national sample. Annals of Internal Medicine. 2004;141:938–45. doi: 10.7326/0003-4819-141-12-200412210-00010. [DOI] [PubMed] [Google Scholar]
- 26.Nugent GN, Hendricks A, Nugent L, Render ML. Value for taxpayers' dollars: what VA care would cost at medicare prices. Medical care research and review : MCRR. 2004;61:495–508. doi: 10.1177/1077558704269795. [DOI] [PubMed] [Google Scholar]
- 27.Kuo YF, Chen NW, Baillargeon J, Raji MA, Goodwin JS. Potentially Preventable Hospitalizations in Medicare Patients With Diabetes: A Comparison of Primary Care Provided by Nurse Practitioners Versus Physicians. Medical care. 2015;53:776–83. doi: 10.1097/MLR.0000000000000406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lenz ER, Mundinger MO, Hopkins SC, Lin SX Smolowitz JLCINDEJ-A, Pmid. Diabetes care processes and outcomes in patients treated by nurse practitioners or physicians. The Diabetes educator. 2002;28:590–8. doi: 10.1177/014572170202800413. [DOI] [PubMed] [Google Scholar]
- 29.Ohman-Strickland PA, Orzano AJ, Hudson SV, et al. Quality of diabetes care in family medicine practices: influence of nurse-practitioners and physician's assistants. Annals of family medicine. 2008;6:14–22. doi: 10.1370/afm.758. [DOI] [PMC free article] [PubMed] [Google Scholar]