Abstract
Background
The estimated incidence of osteoporotic pelvic fractures among persons over age 60 in Germany is 224 per 100 000 persons per year, and rising. A number of surgical treatment options are available, but clinical long-term data are lacking.
Methods
This review is based on pertinent publications and guidelines retrieved by a selective literature search, and on the authors’ clinical experience.
Results
Patients often report one or more relatively trivial traumatic incidents leading up to the fracture. They complain of pain in the hip, groin, or lower lumbar region, or of low back pain and sciatica. A new classification scheme entitled Fragility Fractures of the Pelvis (FFP) takes the morphology of the fracture into account and can be used as an aid to therapeutic decision-making (evidence level IV). The goal of treatment is early mobilization with adequate pain relief. Isolated anterior pelvic ring fractures (FFP I) and nondisplaced posterior pelvic ring fractures (FFP II) are usually stable and can be treated conservatively. Type III and IV injuries are unstable and should generally be treated surgically.
Conclusion
Retrospective analyses have shown that osteoporotic pelvic fractures are associated with decreased mobility and independence and with a one-year mortality ranging from 9.5% to 27%. Prospective therapeutic trials are urgently needed.
Because of increasing life expectancy and an aging population, osteoporosis-associated fragility fractures (also known as insufficiency fractures) of the pelvic ring have become a more common, clinically important problem. The World Health Organization (WHO) defines a fragility fracture as one caused by a trauma that would be insufficient to injure bone if the bone substance were normal. Fragility fractures occur when the bone is no longer adequately resistant to compressive or torsional forces (1, 2).
In particular, fragility fractures of the pelvic ring in the elderly cause immobility and markedly impair quality of life. They pose challenges in diagnostic evaluation, classification, and treatment. Particularly with respect to appropriate treatment, there is still a lack of randomized controlled trials to provide an evidential basis for therapeutic strategies. As a result, inadequate diagnostic evaluation and improper treatment are still common, both in and out of the hospital, and many patients suffer longer than necessary while being shuttled from one group of specialists to another. The AO classification of pelvic ring fractures that has been in use to date is problematic, because such fractures in elderly persons are very different from fractures in younger persons. (AO = Arbeitsgemeinschaft für Osteosynthesefragen/Association for the Study of Internal Fixation [ASIF] or AO Foundation). In this article, we will discuss recent innovations in diagnosis, classification, and treatment and their underlying scientific basis.
Methods
Definition.
The World Health Organization (WHO) defines a fragility fracture as one caused by a trauma that would be insufficient to injure bone if the bone substance were normal.
On the basis of our clinical and scientific experience, we carried out a selective literature search in PubMed (search terms: “fragility fracture pelvis,” “pelvic fracture elderly,” “osteoporotic pelvic fracture,” “insufficiency fracture”) and obtained further information from the WHO guideline and other scientific publications not listed in PubMed, as well as from the internal guidelines of the Center for Orthopedics and Trauma Surgery of the University Hospital Giessen and Marburg GmbH, Location Marburg, Germany.
Learning goals
This article should enable the reader to
carry out a structured diagnostic evaluation of pelvic ring fractures in elderly patients and classify them according to the FFP (Fragility Fractures of the Pelvis) classification, and
know the treatment options for each type of fracture according to the FFP classification.
Etiology and epidemiology
Osteoporosis-associated pelvic ring fractures in the elderly differ markedly from pelvic ring fractures in younger patients who have normal bone consistency. In younger patients, pelvic ring injuries are often due to high-energy trauma and are associated with ligamentous injuries, fractures and dislocations, and neurovascular injuries. In contrast, pelvic injuries in the elderly are generally due to relatively trivial trauma, and the bone breaks because of its poor quality. In some patients, a history of trauma is entirely lacking. These pelvic ring fractures after low-energy trauma do not, as a rule, cause hemodynamic instability, nor are they associated with intrapelvic organ injuries or injuries of the surrounding soft tissues (2).
Loss of bone density and bone mass due to osteoporosis is the usual predisposing factor for pelvic fractures in elderly patients (3). Insufficiency fractures can also arise in patients with vitamin D deficiency, long-term corticosteroid use, prolonged immobilization, or rheumatoid arthritis, and in patients who have received radiotherapy to the pelvis (2, 4, 5).
Etiology.
Osteoporosis-associated pelvic ring fractures in the elderly differ markedly from pelvic ring fractures in younger patients who have normal bone consistency.
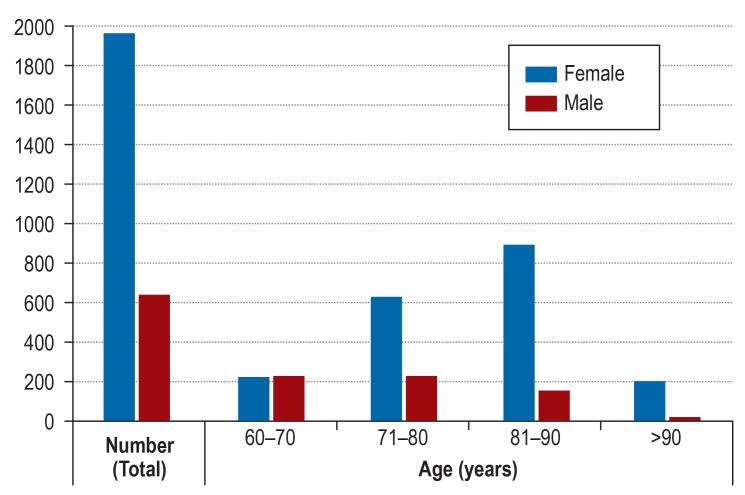
Burge et al. reported in 2007 that pelvic ring fractures in the elderly accounted for 7% of all osteoporosis-associated fractures (6). No valid data are currently available for this type of fracture (in contrast to osteoporosis-associated fractures in other locations). Andrich et al. reported an incidence of 22.4 osteoporosis-associated fractures per 10 000 persons over age 60 per year in Germany (7), while a retrospective analysis revealed that the incidence of pelvic ring fractures among persons aged 80 or above in Finland rose over the period 1970–1997 from 73 to 364 per 100 000 persons per year. Likewise, Sullivan et al. found that the number of pelvic ring fractures among elderly persons in the USA rose by 24% (from 26 500 to 33 000) over the period 1993–2010 (8). This enormous rise is due to longer life expectancies and the aging of the population, though it is partly also due to improved diagnostic evaluation (9). This can be seen, for example, in data collected for the German Pelvic Registry in the years up to 2017: over a 22-year period, the number of type A fractures in the AO classification fell, but the number of type B fractures rose significantly, most likely because of the wider availability of computed tomography as an aid to diagnosis (9). Studies to date have shown a significant correlation with female sex and advancing age. According to a study by Fuchs et al., the peak incidence of osteoporotic pelvic fractures is in the ninth decade of life (10). In a recently published analysis of data from the German Pelvic Registry, 75% of the patients aged 60 or older were women (9). This accords with the higher incidence of osteoporosis in women (11, 12) (figure 1). Similarly, in a retrospective analysis of 93 fragility fractures of the pelvis, Maier et al. found that 75% of the patients were women, and that the fractures were significantly associated with low bone density, as measured by double x-ray energy absorptiometry (DEXA), and with vitamin D deficiency (13). Overall, more than 60% of pelvic ring fractures in the elderly are associated with osteoporosis (9, 14).
Figure 1.
The sex and age distribution of pelvic ring fractures in the elderly, according to an analysis of curent data from the pelvis registry of the German Society for Trauma Surgery (Deutsche Gesellschaft für Unfallchirurgie, DGU) by Rollmann et al. 2017 (9)
Causes of fractures.
Loss of bone density and bone mass due to osteoporosis, vitamin D deficiency, long-term corticosteroid use, prolonged immobilization, rheumatoid arthritis, and radiotherapy to the pelvis.
Specific fracture morphology, and classification systems
Fragility fractures of the pelvic ring in elderly persons differ markedly from those in younger persons. In addition to osteoporosis, which was discussed above, increasing ossification and rigidity of the ligamentous structures leads to a loss of pelvic elasticity and thereby to a different pattern of stress and load transmission in the pelvic ring (15). A fall on the side often causes a compression fracture of the lateral mass of the sacrum and an associated horizontally running fracture of the superior ramus of the pubic bone (2, 16). The different fracture morphology in old age is well explained by a specific and uniform pattern of bone degeneration in the posterior portion of the pelvic ring (15, 17). The sacrum, in particular, is at increased risk of fracture because of pathological biomechanical changes of the pelvis that arise in old age (18). Fracture morphology can change over time as well: the initial finding is usually a compression fracture, as mentioned, but mobilization with full loading and repeated falls can lead to more complex fracture patterns, ranging all the way to complete collapse of the pelvic ring (2, 19).
Pelvic ring fractures are initially classified as type A, B, or C in the AO classification. Type A fractures are stable, type B fractures are rotationally unstable, and type C fractures are both rotationally and vertically unstable (9). This classification, however, does not apply to the morphologies of pelvic ring fractures in old age, and it may not correctly reflect the true severity of such injuries because fragility fractures are unlike pelvic ring fractures in younger patients. In particular, the bilateral sacral insufficiency fractures often seen in older persons are rare in young adults, except as a consequence of high-energy trauma (AO type C3).
Rommens and Hofmann have developed a new classification system, based on a detailed radiological analysis of their own patients, which gives due consideration to sacral insufficiency fractures (16). The degree of instability plays a decisive role; this criterion is a major determinant of the decision whether or not to operate (2). Moreover, the scheme includes different subtypes depending on the site of posterior pelvic ring instability.
Osteoporosis.
Overall, more than 60% of pelvic ring fractures in the elderly are associated with osteoporosis.
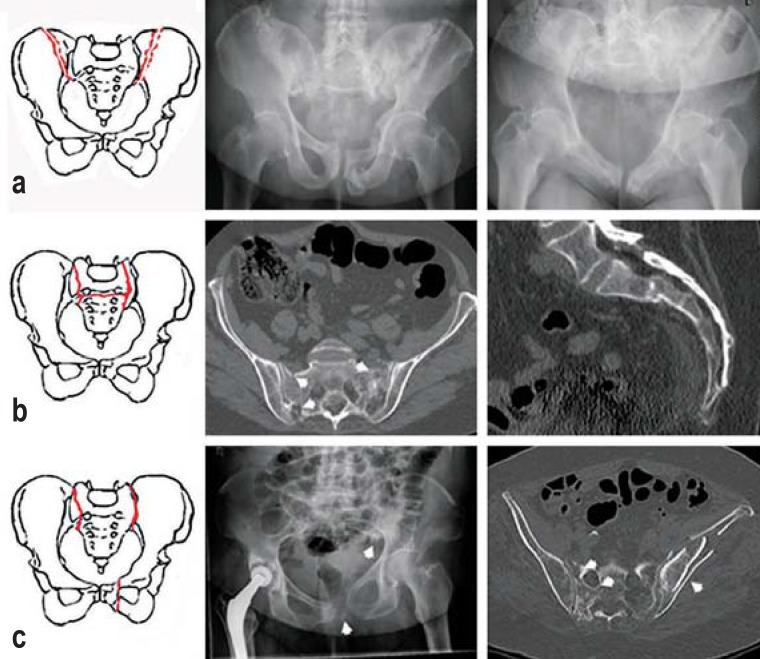
The FFP classification comprises four types of fracture (Figures 2– 5).
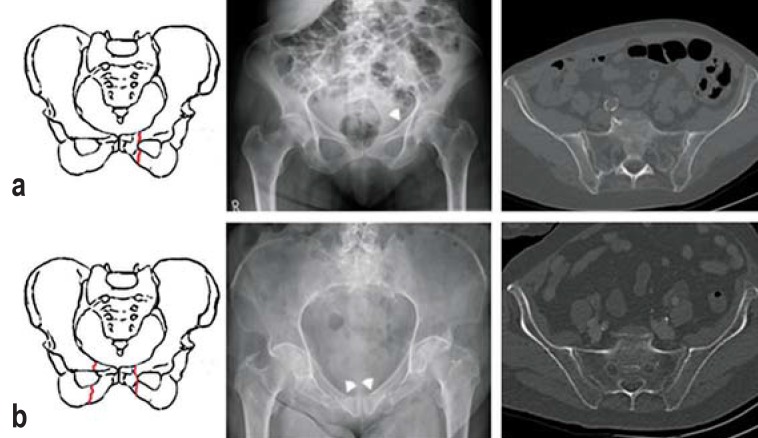
Figure 2.
An FFP type I fracture is an isolated fracture of the anterior pelvic ring in the Fragility Fractures of the Pelvis classification, according to Rommens and Hofmann (2, 16). The four different types of fracture are shown in this figure and in Figures 3–5. The letters a, b, and c correspond to the subtypes described in the text
FFP type I: These are isolated anterior pelvic ring fractures without involvement of the posterior structures. Type Ia fractures are unilateral, type Ib fractures are bilateral (figure 2).
AO classification.
Pelvic ring fractures are initially classified as type A, B, or C in the AO scheme. Type A fractures are stable, type B fractures are rotationally unstable, and type C fractures are both rotationally and vertically unstable.
FFP type II: These are nondisplaced fractures of the posterior pelvic ring. Type IIa is characterized by an isolated dorsal lesion, while type IIb is a compression fracture of the anterior portion of the lateral mass of the sacrum associated with instability of the anterior pelvic ring. Type IIc is a nondisplaced complete sacral, sacroiliac, or iliac fracture with accompanying instability of the anterior pelvic ring (figure 3).
Figure 3.
An FFP type II fracture is a nondisplaced fracture of the posterior pelvic ring
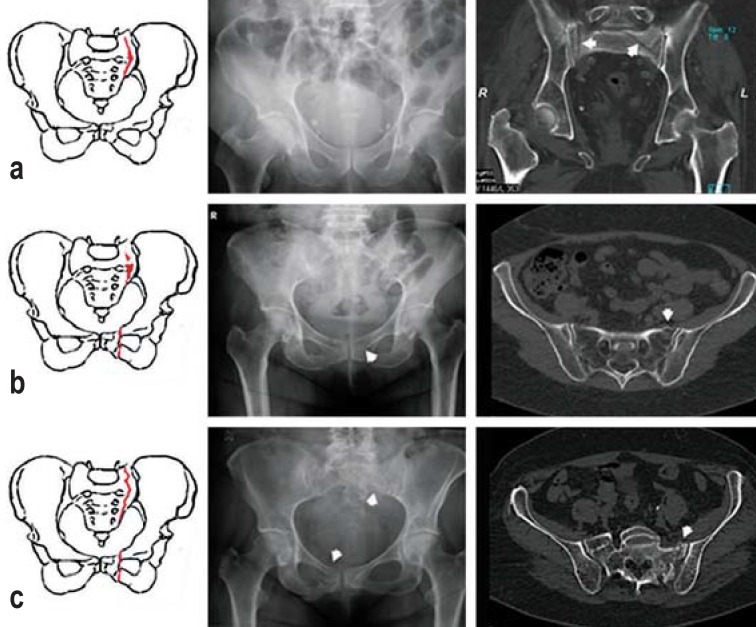
FFP type III: These are displaced unilateral fractures of the posterior pelvic ring with simultaneous instability of the anterior pelvic ring. Type IIIa consists of a displaced fracture of the ilium, while type IIb is characterized by a displaced unilateral iliosacral rupture, and type IIIc by a displaced unilateral fracture of the sacrum (figure 4).
Figure 4.
An FFP type III fracture is a displaced unilateral posterior pelvic ring fracture
FFP type IV: These are bilateral displaced posterior pelvic ring injuries. Type IVa consists of a bilateral ilium fracture or bilateral iliosacral rupture; type IVb consists of a spinopelvic burst fracture with associated bilateral vertical lesions of the lateral mass of the sacrum and a simultaneous horizontal component connecting the two vertical lesions (U or H fracture of the sacrum). Type IVc is a combination of multiple displaced instabilities of the posterior pelvic ring (figure 5).
Figure 5.
An FFP type IV fracture is a displaced bilateral posterior pelvic ring fracture
Diagnostic evaluation
Most patients relate having experienced one or more relatively trivial traumatic events; in some cases, the history is unclear or the patient cannot recall any antecedent trauma. The patients present with severe pain in the hip, the groin, or the lower lumbar region, or else with low back pain and sciatica. The physical examination should include palpation of the anterior and posterior portions of the pelvic ring as well as mechanical testing of the stability of the pelvic ring, with gentle compression of the iliac fossae and gentle “hinging outward” through controlled pressure on the iliac crests. If a pelvic ring fracture is suspected, an anteroposterior plain film of the pelvis should be obtained, supplemented (depending on the patient’s symptoms) by inlet and outlet views and/or an axial image of the hip. Multiple studies have shown that computed tomography (CT) is needed to ensure reliable diagnosis, because conventional X-ray imaging is inadequate to display nondisplaced compression fractures of the sacrum (10, 16, 20).
History.
The patients present with severe pain in the hip, the groin, or the lower lumbar region, or else with low back pain and sciatica.
Diagnostic evaluation.
Multiple studies have shown that computed tomography (CT) is needed to ensure reliable diagnosis, because conventional X-ray imaging is inadequate to display nondisplaced compression fractures of the sacrum.
As many as 80% of all injuries initially classified as isolated anterior pelvic ring fractures on the basis of conventional X-ray images are found on CT to comprise a dorsal lesion as well (20, 21). Failure to appreciate the severity of the injury can lead to inappropriate treatment and, in turn, to delayed healing and higher morbidity.
Magnetic resonance imaging (MRI) is useful for the evaluation of persistent pain in the area of the posterior pelvic ring or the lower lumbar region in the absence of positive findings on CT. It enables the early and efficient diagnosis of otherwise occult sacral insufficiency fractures. In a study by Cosker et al., 95% of patients initially thought to have an isolated anterior pelvic ring fracture were found on MRI to have a lesion of the posterior pelvic ring as well (22). MRI is thus the most sensitive diagnostic technique.
Dual-energy computed tomography (DECT) is an alternative to MRI that reveals bone marrow edema with higher sensitivity than conventional CT (23).
Whenever a pelvic fragility fracture is suspected, a comprehensive and timely diagnostic evaluation should be performed.
Treatment
Rapid mobilization and adequate pain relief are the main objectives of treatment. Hemodynamic instability is rare; it can be diagnosed on an urgently obtained contrast CT of the pelvis and, if present, should be treated with subsequent angiography and selective embolization (24). The possibility of an associated hemorrhage should always be considered in patients who are being treated with anticoagulant drugs. Hemodynamic monitoring for at least 24 hours is recommended in such cases so that protracted, relevant bleeding can be identified early and then rapidly treated with angiography and embolization (25, 26).
Bone densitometry (DEXA) should also be performed in timely fashion, and osteoporosis, if present, should be medically treated. Maier et al. report that 75% of their admitted patients had previously received a diagnosis of osteoporosis, but only 39% were under treatment for it on admission. DEXA bone densitometry yielded a T-score below –2.5 in all 69 of the patients who underwent it (13). A new treatment for osteoporosis with parathyroid hormone (teriparatide) deserves to be mentioned in this connection: Peichl et al. showed in 2011 that this treatment significantly shortens the time to healing of osteoporosis-associated pelvic ring fractures (27).
Goal of treatment.
Rapid mobilization and adequate pain relief are the main objectives of treatment, along with optimizing the patient’s condition in the shortest possible time.
Therapeutic decision-making.
Thus, the individual fracture situation must be precisely analyzed in each case.
In general, decisions about treatment should be made by a multidisciplinary team including surgeons, geriatricians, pain therapists, and physiotherapists. The goal of decision-making should be to optimize the patient’s condition as soon as possible, i.e., to relieve pain adequately and restore full mobility with the least invasive modality of effective treatment (2). Full weight-bearing, adapted to the patient’s pain, should be the aim of physical therapy.
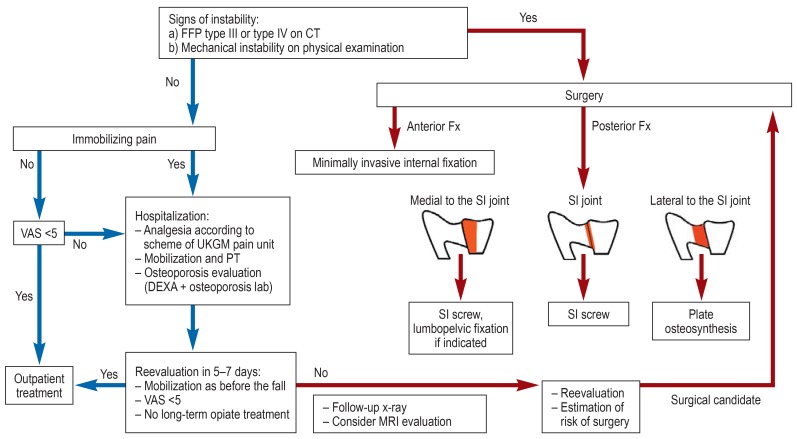
The current treatment algorithm for pelvic fractures in our institution (the Center for Orthopedics and Trauma Surgery of the University Hospital Giessen and Marburg GmbH, Location Marburg, Germany) is shown in Figure 6.
Figure 6.
Treatment algorithm in the authors’ institution (Center for Orthopedics and Trauma Surgery, University Hospital Giessen and Marburg GmbH [Universitätsklinikum Giessen und Marburg GmbH (UKGM)], Marburg, Germany) for the treatment of fragility fractures of the pelvic ring in the elderly. CT, computed tomography; DEXA, double x-rax energy absorptiometry; FFP, Fragility Fractures of the Pelvis; Fx,fracture; PT, physiotherapy; MRI, magnetic resonance imaging; SI, sacroiliac; VAS, Visual Analog Scale
Therapeutic decision-making is based on the instability criteria of the FFP classification. Thus, the individual fracture situation must be precisely analyzed in each case. In what follows, we will give a detailed presentation of the available treatment options for each type of fracture in the FFP classification.
The FFP classification, which was published in 2013, establishes a conceptual framework for these injuries, but has not been validated by any clinical studies to date. Nor have there yet been any randomized controlled trials of the treatment options discussed below, and the recommendations given here are largely based on retrospective data.
FFP type I fractures
Isolated anterior pelvic ring fractures can be considered stable and can therefore be treated conservatively. Patients with severe pain despite analgesic medication may need to be admitted to the hospital for mobilization with full weight-bearing under the supervision of a physiotherapist. The comorbidities of these elderly patients may make it difficult to apply standard protocols for the treatment of pain. Nonsteroidal anti-inflammatory drugs should be used with caution in view of their side effects and interactions (28, 29). Opioids are frequently indicated as an additional therapeutic option. Cognitively impaired patients should be thoroughly examined and assessed so that appropriate pain-relieving treatment can be given (30). There are special instruments for the detection of pain in demented patients, including, for example, the BESD score (German: Beurteilung des Schmerzes bei Demenz, i.e., pain assessment in dementia), which takes account of the patient’s respiratory pattern, negative vocalizations, body posture, facial expression, and response to consolation (31).
FFP type I fractures.
Isolated anterior pelvic ring fractures can be considered stable and can therefore be treated conservatively.
FFP type II fractures.
An FFP type II fracture is a nondisplaced fracture of the posterior pelvic ring. These injuries can be treated conservatively as well, but they render the patient immobile for a longer period of time.
Radiological follow-up is recommended to rule out secondary dislocation or secondary fractures, and whenever the pain is so severe as to preclude timely mobilization. In such cases, the FFP classification may need to be changed, depending on the findings.
FFP type II fractures
An FFP type II fracture is a nondisplaced fracture of the posterior pelvic ring. Isolated posterior pelvic ring injuries (FFP type IIa) are rare. The mechanism of injury usually leads to an anterior pelvic ring fracture as well, combined with a compression fracture of the lateral mass of the sacrum (FFP type IIb), or else to a nondisplaced, complete fracture of the sacrum or ilium or to an iliosacral injury (FFP type IIc). These injuries can be treated conservatively as well, but they render the patient immobile for a longer period of time. If conservative treatment does not lead to adequate pain relief and mobilization, surgery should be discussed with the patient. Percutaneous techniques are preferred whenever possible. In addition to stabilization of the posterior pelvic ring, stabilization of the anterior pelvic ring should be considered as well (2).
FFP type III and type IV fractures
Type III and IV injuries are characterized by marked unilateral or bilateral instability of the posterior pelvic ring. As type III injuries rarely heal spontaneously, we recommend that they be treated surgically. Here, too, percutaneous techniques are preferred to open repositioning, as long as there is no major degree of dislocation.
Type IV injuries should also be treated surgically. Both sides should be surgically stabilized so that there will be no risk of intrusion of the lumbosacral fragment (2).
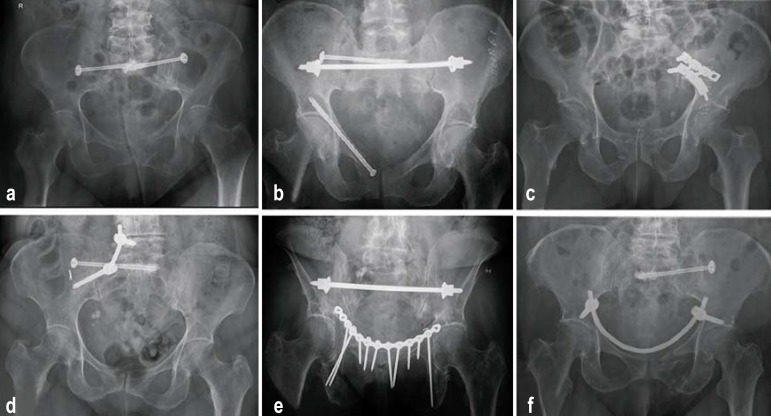
The various surgical techniques that are available for stabilization of the anterior and posterior pelvic ring are listed in the eTable. We will only discuss the more commonly used ones in what follows (figure 7).
eTable. Surgical techniques for stabilization of the posterior and anterior pelvic ring.
| Surgical technique | Indication | Advantages |
Disadvantages and potential complications |
| Anterior pelvic ring | |||
| External fixation | Ventral instability (e.g., FFP type II), also bilateral |
Minimally invasive, can be removed without general anesthesia | Pin infections, loose pins, discomfort on sitting, possible lesion of lat. fem. cutaneous n. (meralgia paresthetica) |
| Subcutaneous internal fixation | Ventral instability (e.g., FFP type II), also bilateral |
Minimally invasive | Prominent implants, possible lesion of lat. fem. cutaneous n., pressure injury of femoral n. |
| Submuscular internal fixation | Ventral instability (e.g., FFP type II), also bilateral |
Minimally invasive, no bothersome implant, good stability |
Possible vascular injury or pressure injury of femoral n. |
| Retrograde transpubic screw | Ventral instability (e.g., FFP type II) | Percutaneous, adequate stability | Only for pubic ramus fractures; high precision required |
| Plate osteosynthesis | Ventral instability (e.g., FFP type II) | Highest stability, vessels can be surgically exposed and protected |
Open technique, long procedure, loosening of implant |
| Posterior pelvic ring | |||
| Sacroplasty | Isolated incomplete compression fracture of the lateral mass of the sacrum (e.g., FFP IIa) |
Percutaneous, relieves pain | Possible cement leak |
| Percutaneous sacroiliac screw osteosynthesis |
Incomplete, complete, or displaced fracture of the lateral mass of the sacrum |
Percutaneous, compression of the fracture cleft |
Poor purchase in the sacral spongiosa |
| Percutaneous sacroiliac screw osteosynthesis with cement augmentation |
Incomplete, complete, or displaced fracture of the lateral mass of the sacrum |
Percutaneous, compression of the fracture cleft, holds strongly |
Possible cement leak |
| Transiliac internal fixation | Bilateral dorsal instability (e.g., FFP IV) |
Minimally invasive, bridging osteosynthesis |
No compression, bothersome implants |
| Transsacral bar osteosynthesis | Bilateral dorsal instability (e.g., FFP IV) |
Minimally invasive, compression, high stability |
Requires large trans-sacral corridor, not possible with sacral dysmorphism |
| Plate osteosynthesis | Frature lateral to the sacroiliac joint (e.g., FFP type IIIa) |
Mildly invasive, bridging osteosynthesis |
No compression |
| Iliolumbar fixation, combined with a sacroiliac screw if indicated (triangular stabilization) |
Displacement and vertical instability (FFP types III and IV) |
Mildly invasive, can be performed bilaterally |
Loss of mobility of the iliosacral segment, bothersome implants |
FFP, fragility fractures of the pelvis
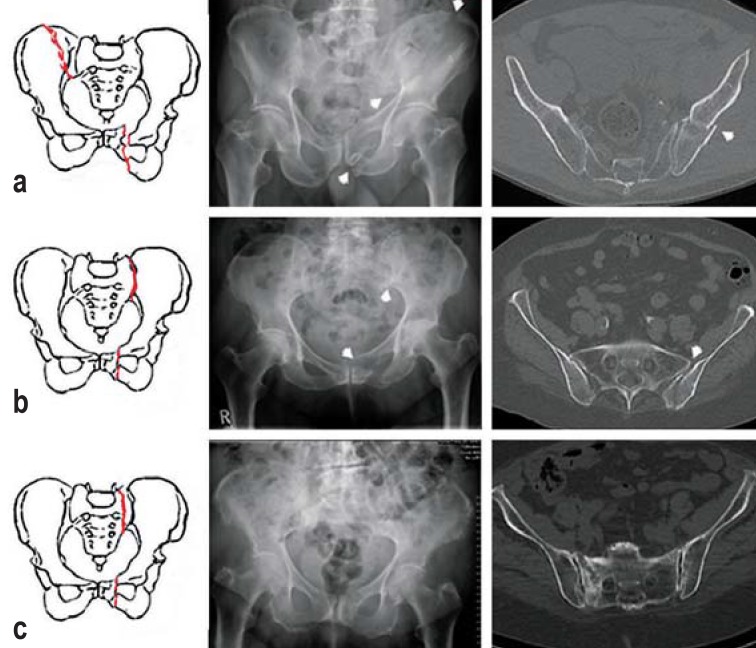
Figure 7.
The surgical methods mentioned in the text for stabilization of the anterior and posterior pelvic ring are shown here.
a) Cemented sacroiliac screw osteosynthesis for a bilateral fracture of the lateral mass of the sacrum. b) Sacroiliac screw osteosynthesis, transsacral bar osteosynthesis, and a retrograde transpubic screw in the pubic bone inserted percutaneously. c) Ventral plate osteosynthesis for a fracture lateral to the sacroiliac joint. d) Unilateral lumbopelvic fixation combined with a cemented sacroiliac screw (triangular fixation). e) Ventral plate osteosynthesis of the anterior pelvic ring and transsacral bar osteosynthesis. f) Internal fixation with a screw-and-rod system to stabilize the anterior pelvic ring
Surgical techniques for stabilization of the posterior pelvic ring
Most posterior fractures of the sacrum (complete or displaced fractures of the lateral mass of the sacrum) can be treated by percutaneous trans-sacroiliac screw osteosynthesis. This technique is already widely accepted for the stabilization of posterior pelvic ring fractures due to high-energy trauma. One or two 7–8 mm cannulated screws with a full or partial thread are inserted in the vertebral body of S1; additionally, a second screw can be placed in S2. In case of bilateral dorsal instability, both sides can be treated in the same procedure with two sacroiliac screws. Alternatively, transsacral bar osteosynthesis can be used.
Sacroplasty is an alternative option for isolated and incomplete compression fractures of the lateral mass (FFP type IIa). In this technique, which is analogous to vertebroplasty, cement is introduced into the area of the fracture. Fragility fractures only rarely arise in the ilium lateral to the sacroiliac joint (FFP type IIIa). In case of instability and dislocation, these are treated surgically by plate osteosynthesis.
In case of marked dislocation and vertical instability, as in FFP type III or IV fractures, unilateral or bilateral lumbopelvic fixation may be needed. If there is multiplanar instability, sacroiliac screw osteosynthesis can be performed as well in order to achieve both horizontal and vertical stability. This technique, known as triangular stabilization, seems to be the biomechanically most stable type of fixation (32).
Surgical techniques for stabilization of the anterior pelvic ring
Surgical techniques for stabilization of the anterior pelvic ring.
In case of ventral instability (as in FFP type IIb) and immobilizing pain, stabilization can be achieved with external or internal fixation.
In case of ventral instability (as in FFP type IIb) and immobilizing pain, stabilization can be achieved with an external fixator: minimally invasive Schanz screws are inserted into the supra-acetabular area bilaterally. The anterior pelvic ring can also be stabilized in analogous fashion with internal fixation techniques. These may be either purely subcutaneous or deep (submuscular). A further option is the insertion of a retrograde transpubic screw.
Complications and prognosis
Despite the steeply increasing incidence of fragility fractures of the pelvic ring, the literature to date contains only retrospective analyses. The reported average duration of hospital stay ranges from 9.3 to 45 days (3, 14). The 1-year mortality ranges from 9.5% to 27% (3, 13, 33); these figures are similar to those reported for proximal femur fractures. Hill et al. even reported a 5-year mortality of 54.4% (34).
Complications and prognosis.
The reported average duration of hospital stay ranges from 9.3 to 45 days. The 1-year mortality ranges from 9.5% to 27%; these figures are similar to those reported for proximal femur fractures.
The successful conservative treatment of FFP type I and II fractures generally relieves pain within 2 weeks and restores mobility within 6 weeks. Surgery for FFP type II, III, and IV fractures relieves pain rapidly as well. Fracture healing takes from 6 weeks to 3 months, and full ambulation is usually restored in 3 months (24).
Caveat.
Physicians should be aware of the risk of secondary dislocation and of a change of fracture type during the course of treatment.
In our experience, correct and rigorously applied conservative treatment with early mobilization only rarely leads to complications, yet Maier et al., in a cohort of 93 conservatively treated patients, reported a 58% complication rate (composed, in turn, of urinary tract infections [61%], pneumonia [29%], depression [5%], and thromboembolic events [3%]). Over the long term (mean follow-up interval, 34 months), the number of patients needing help in everyday life nearly doubled: 77% of the patients were independent before the fracture, but 66% were dependent on help afterward (13). Breuil et al. reported diminished independence in nearly 50% of patients after a mean follow-up time of 29 months (11). In the case series of Taillandier et al., only 22 of the 56 patients who were followed up regained their original functional status (35).
Physicians should be aware of the risk of secondary dislocation and of a change of fracture type during the course of treatment. Initially conservative treatment may need to be converted to surgical treatment if pain and immobility persist. Rarely, pseudarthroses arise during conservative treatment that may require secondary surgical stabilization.
Surgical complications.
The complications of surgical treatment range from the usual complications of any type of surgery (postoperative bleeding, infection, neural injury, deep vein thrombosis) to pulmonary embolism and multiple organ system failure.
The complications of surgical treatment range from the usual complications of any type of surgery (postoperative bleeding, infection, neural injury, deep vein thrombosis) to pulmonary embolism and multiple organ system failure. Serious complications are rarer when minimally invasive techniques are used (36, 37). No data are yet available that would permit a comparison of the complication rates and outcomes of different osteosynthetic techniques for fragility fractures of the pelvis. In a retrospective study, Hopf et al. showed that percutaneous sacroiliac screw osteosynthesis significantly lessens pain (VAS 6.8 on admission and 1.8 on discharge; VAS = Visual Analog Scale). All 30 of the patients treated in this study first underwent conservative treatment for 6 days and experienced no more than a slight decrease of pain (VAS 6.0), which was the reason for performance of a percutaneous sacroiliac screw osteosynthesis. Twenty-two of them regained their original level of mobility, and 16 of these 22 had little or no impairment in everyday life after a mean follow-up interval of 31 months (38). The main complications of sacroiliac screw osteosynthesis are malpositioned screws (3–17%) and nerve injury (0–8%) (37). Screws can become loose in osteoporotic bone, and cement augmentation is therefore recommended (39). Cement should be applied carefully, however, so that cement leaks can be avoided (2). Further clinical studies will be needed to determine whether additional cement augmentation should become part of the standard treatment for sacral insufficiency fractures (2). As for the treatment of anterior pelvic ring injuries, the available data mainly concern the complications of external fixation, which include pin-site infections (2.5%–50%), loose screws (0–19%), and loss of reposition (0–33%) (40). These complications have led to controversy about the utility of external fixation (2). Subcutaneous systems become infected much less commonly (3%) but need to be evaluated in further clinical studies (40).
The increased mortality, diminished mobility, and loss of social independence that have been described in association with prolonged conservative treatment imply that timely diagnostic evaluation is important, in both the inpatient and the outpatient settings, so that fractures can be identified and their degree of stability can be properly assessed. Pain should be evaluated regularly, and minimally invasive surgical treatment should be considered in a timely fashion to achieve pain relief and restoration of mobility. The treatment of these patients in interdisciplinary centers for geriatric trauma surgery, the use of structured processes for diagnosis and treatment, and the prospective trials that are now urgently needed should all help improve the clinical outcomes of elderly patients with fragility fractures of the pelvic ring.
Conclusion.
Pain should be evaluated regularly, and minimally invasive surgical treatment should be considered in a timely fashion to achieve pain relief and restoration of mobility.
Further Information on CME.
This article has been certified by the North Rhine Academy for Postgraduate and Continuing Medical Education (CME). Deutsches Ärzteblatt provides certified CME in accordance with the requirements of the Medical Associations of the German federal states (Länder). CME points of the Medical Associations can be acquired only through the Internet by the use of the German version of the CME questionnaire: see cme.aerzteblatt.de. Participants can manage their CME points with their 15-digit “uniform CME number” (einheitliche Fortbildungsnummer, EFN), which must be entered in the appropriate field on the cme.aerzteblatt.de website under ”“meine Daten” (“my data”), or upon registration. The EFN appears on each participant’s CME certificate. This CME unit can be accessed until 29 April 2018, and earlier ones until the dates indicated:
“Current Approaches to Epistaxis Treatment in Primary and Secondary Care” (issue 1–2/2018) until 2 April 2018
“Community-Acquired Pneumonia in Adults”
(issue 49/2017) until 4 March 2018
“Shoulder Impingement Syndrome” (issue 45/2018) until 4 February 2018
Participation via Internet (cme.aerzteblatt.de). This CME unit is accessible until 29 April 2018. Only one answer is possible per question. Please select the most appropriate answer.
Question 1
According to the treatment algorithm of the Center for Orthopedics and Trauma Surgery in Marburg, which of the following is indicated for an unstable pelvic fracture involving the ilium lateral to the sacroiliac joint?
Continuation of conservative treatment
External fixation
Percutaneous, cement-augmented sacroiliac screw fixation
A lumboplevic brace
Plate osteosynthesis
Question 2
What is the most common cause of complex pelvic fractures in young patients with normal bone structure?
A simple fall
High-speed trauma
A pathological fracture
A fall with suicidal intent
A fall due to syncope
Question 3
Which of the following testing modalities is most sensitive for fragility fractures?
Double x-ray energy absorptiometry (DEXA)
Computed tomography
Conventional pelvic x-ray
Ultrasonography
Magnetic resonance imaging
Question 4
With what systemic disease are fragility fractures most commonly associated?
Plasmacytoma
Osteopetrosis
Ankylosing spondylitis
Perthes’ disease
Osteoporosis
Question 5
How is a dislocated unilateral posterior pelvic ring fracture with simultaneous instability of the anterior pelvic ring classified in the scheme of Rommens and Hofmann?
Fragility Fractures of the Pelvis (FFP) type I
Fragility Fractures of the Pelvis (FFP) type II
Fragility Fractures of the Pelvis (FFP) type III
Fragility Fractures of the Pelvis (FFP) type IV
Fragility Fractures of the Pelvis (FFP) type V
Question 6
How is an isolated bilateral anterior pelvic ring fracture not involving the posterior pelvic ring classified in the scheme of Rommens and Hofmann?
Fragility Fractures of the Pelvis (FFP) type Ia
Fragility Fractures of the Pelvis (FFP) type Ib
Fragility Fractures of the Pelvis (FFP) type IIc
Fragility Fractures of the Pelvis (FFP) type IVa
Fragility Fractures of the Pelvis (FFP) type IIa
Question 7
You diagnose a fragility fracture, type IIb, in an otherwise well 90-year-old woman. Which of the following should be a component of early treatment?
Immediate emergency stabilization (pelvic loop)
Bed rest for 6 weeks
Full mobilization, adapted to pain
Minimally invasive external fixation
Percutaneous screw osteosynthesis
Question 8
What does the term “sacroplasty” signify?
Reconstruction of the sacrum
Percutaneous screw osteosynthesis of the sacrum
A cement augmentation technique
A complex osteosynthetic technique
A structural defect of the sacrum
Question 9
What is the most common cause of pelvic fragility fractures?
A fall from a great height
An automobile accident
A bicycle accident
A simple fall, e.g., after tripping
A fall with suicidal intent
Question 10
What is the recommended physiotherapeutic approach after percutaneous screw osteosynthesis of the sacroiliac joint?
No weight-bearing for 6 weeks
Restricted bed rest
Full mobilization, adapted to pain
Walking on crutches to keep weight off the joint
Limitation of hip flexion to 90°
► Participation is only possible via the Internet: cme.aerzteblatt.de
Acknowledgments
Translated from the original German by Ethan Taub, M.D.
Acknowledgement
We thank Dr. M. Rollmann (Universitätsklinikum des Saarlandes) for her support in the creation of Figure 1.
Footnotes
Conflict of interest statement
The authors state that no conflict of interest exists.
References
- 1.WHO. Guidelines for preclinical evaluation and clinical trials in osteoporosis; 1998. http://apps.who.int/iris/bitstream/10665/42088/1/9241545224_eng.pdf (last accessed on 3 Januaray 2018) [Google Scholar]
- 2.Rommens PM, Wagner D, Hofmann A. Fragility fractures of the pelvis. J Bone Jt Surg Rev. 2017;5:1–13. doi: 10.2106/JBJS.RVW.16.00057. [DOI] [PubMed] [Google Scholar]
- 3.Krappinger D, Kammerlander C, Hak DJ, Blauth M. Low-energy osteoporotic pelvic fractures. Arch Orthop Trauma Surg. 2010;130:1167–1175. doi: 10.1007/s00402-010-1108-1. [DOI] [PubMed] [Google Scholar]
- 4.McCabe MP, Smyth MP, Richardson DR. Current concept review: Vitamin D and stress fractures. Foot Ankle Int. 2012;33:526–533. doi: 10.3113/FAI.2012.0526. [DOI] [PubMed] [Google Scholar]
- 5.Uezono H, Tsujino K, Moriki K, et al. Pelvic insufficiency fracture after definitive radiotherapy for uterine cervical cancer: retrospective analysis of risk factors. J Radiat Res. 2013;54:1102–1109. doi: 10.1093/jrr/rrt055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22:465–475. doi: 10.1359/jbmr.061113. [DOI] [PubMed] [Google Scholar]
- 7.Andrich S, Haastert B, Neuhaus E, et al. Epidemiology of pelvic fractures in Germany: considerably high incidence rates among older people. PLoS One. 2015;10 doi: 10.1371/journal.pone.0139078. e0139078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sullivan MP, Baldwin KD, Donegan DJ, Mehta S, Ahn J. Geriatric fractures about the hip: divergent patterns in the proximal femur, acetabulum, and pelvis. Orthopedics. 2014;37:151–157. doi: 10.3928/01477447-20140225-50. [DOI] [PubMed] [Google Scholar]
- 9.Rollmann MF, Herath SC, Kirchhoff F, et al. Pelvic ring fractures in the elderly now and then-a pelvic registry study. Arch Gerontol Geriatr. 2017;71:83–88. doi: 10.1016/j.archger.2017.03.007. [DOI] [PubMed] [Google Scholar]
- 10.Fuchs T, Rottbeck U, Hofbauer V, Raschke M, Stange R. [Pelvic ring fractures in the elderly Underestimated osteoporotic fracture] Unfallchirurg. 2011;114:663–670. doi: 10.1007/s00113-011-2020-z. [DOI] [PubMed] [Google Scholar]
- 11.Breuil V, Roux CH, Testa J, et al. Outcome of osteoporotic pelvic fractures: an underestimated severity. Survey of 60 cases. Jt Bone Spine. 2008;75:585–588. doi: 10.1016/j.jbspin.2008.01.024. [DOI] [PubMed] [Google Scholar]
- 12.Melton LJ, Chrischilles EA, Cooper C, Lane AW, Riggs BL. How many women have osteoporosis? J Bone Miner Res. 2005;20:886–892. doi: 10.1359/jbmr.2005.20.5.886. [DOI] [PubMed] [Google Scholar]
- 13.Maier GS, Kolbow K, Lazovic D, et al. Risk factors for pelvic insufficiency fractures and outcome after conservative therapy. Arch Gerontol Geriatr. 2016;67:80–85. doi: 10.1016/j.archger.2016.06.020. [DOI] [PubMed] [Google Scholar]
- 14.Soles GLS, Ferguson TA. Fragility fractures of the pelvis. Curr Rev Musculoskelet Med. 2012;5:222–228. doi: 10.1007/s12178-012-9128-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Josten C, Höch A. [Fractures of the sacrum: operative/conservative Pro: Why insufficiency fractures of the sacrum should be treated operatively] Die Wirbelsäule. 2017;1:31–40. [Google Scholar]
- 16.Rommens PM, Hofmann A. Comprehensive classification of fragility fractures of the pelvic ring: recommendations for surgical treatment. Injury. 2013;44:1733–1744. doi: 10.1016/j.injury.2013.06.023. [DOI] [PubMed] [Google Scholar]
- 17.Wagner D, Kamer L, Sawaguchi T, Richards RG, Noser H, Rommens PM. Sacral bone mass distribution assessed by averaged three-dimensional CT Models: implications for pathogenesis and treatment of fragility fractures of the sacrum. J Bone Joint Surg Am. 2016;98:584–590. doi: 10.2106/JBJS.15.00726. [DOI] [PubMed] [Google Scholar]
- 18.Linstrom NJ, Heiserman JE, Kortman KE, et al. Anatomical and biomechanical analyses of the unique and consistent locations of sacral insufficiency fractures. Spine. 2009;34:309–315. doi: 10.1097/BRS.0b013e318191ea01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wagner D, Ossendorf C, Gruszka D, Hofmann A, Rommens PM. Fragility fractures of the sacrum: how to identify and when to treat surgically? Eur J Trauma Emerg Surg. 2015;41:349–362. doi: 10.1007/s00068-015-0530-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Böhme J, Höch A, Boldt A, Josten C. [Influence of routine CT examination on fracture classification and therapy for pelvic ring fractures in patients aged over 65 years old] Z Orthop Unfall. 2012;150:477–483. doi: 10.1055/s-0032-1315270. [DOI] [PubMed] [Google Scholar]
- 21.Tosounidis G, Wirbel R, Culemann U, Pohlemann T. [Misinterpretation of anterior pelvic ring fractures in the elderly] Unfallchirurg. 2006;109:678–680. doi: 10.1007/s00113-006-1098-1. [DOI] [PubMed] [Google Scholar]
- 22.Cosker TDA, Ghandour A, Gupta SK, Tayton KJJ. Pelvic ramus fractures in the elderly: 50 patients studied with MRI. Acta Orthop. 2005;76:513–516. doi: 10.1080/17453670510044634. [DOI] [PubMed] [Google Scholar]
- 23.Hackenbroch C, Riesner HJ, Lang P, et al. Dual energy CT—a novel technique for diagnostic testing of fragility fractures of the pelvis. Z Orthop Unfall. 2017;155:27–34. doi: 10.1055/s-0042-110208. [DOI] [PubMed] [Google Scholar]
- 24.Rommens PM, Wagner D, Hofmann A. [Osteoporotic fractures of the pelvic ring] Z Orthop Unfall. 2012;150:e107–e118. doi: 10.1055/s-0032-1314948. [DOI] [PubMed] [Google Scholar]
- 25.Dietz SO, Hofmann A, Rommens PM. Haemorrhage in fragility fractures of the pelvis. Eur J Trauma Emerg Surg. 2015;41:363–367. doi: 10.1007/s00068-014-0452-1. [DOI] [PubMed] [Google Scholar]
- 26.Rommens PM, Hofmann A, Hessmann MH. Management of acute hemorrhage in pelvic trauma: an overview. Eur J Trauma Emerg Surg. 2010;36:91–99. doi: 10.1007/s00068-010-1061-x. [DOI] [PubMed] [Google Scholar]
- 27.Peichl P, La H, Maier R, Holzer G. Parathyroid hormone 1-84 accelerates fracture-healing in pubic bones of elderly osteoporotic women. J Bone Joint Surg Am. 2011;93:1583–1587. doi: 10.2106/JBJS.J.01379. [DOI] [PubMed] [Google Scholar]
- 28.Buffum MD, Hutt E, Chang VT, Michael H, Snow AL. Cognitive impairment and pain management: review of issues and challenges. J Rehabil Res Dev. 2007;44:315–330. doi: 10.1682/jrrd.2006.06.0064. [DOI] [PubMed] [Google Scholar]
- 29.Roche JJ, Wenn RT, Sahota O, Moran CG. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ. 2005;331 doi: 10.1136/bmj.38643.663843.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Feldt KS, Ryden MB, Miles S. Treatment of pain in cognitively impaired compared with cognitively intact older patients with hip-fracture. J Am Geriatr Soc. 1998;46:1079–1085. doi: 10.1111/j.1532-5415.1998.tb06644.x. [DOI] [PubMed] [Google Scholar]
- 31.Harden V, Hurley AV, Volicer L. Development and psychometric evaluation of the Pain Assessment in Advanced Dementia (PAINAD) scale. J Am Med Dir Assoc. 2003;4:9–15. doi: 10.1097/01.JAM.0000043422.31640.F7. [DOI] [PubMed] [Google Scholar]
- 32.Schildhauer TA, Ledoux WR, Chapman JR, Henley MB, Tencer AF, Routt MLC. Triangular osteosynthesis and iliosacral screw fixation for unstable sacral fractures: a cadaveric and biomechanical evaluation under cyclic loads. J Orthop Trauma. 2003;17:22–31. doi: 10.1097/00005131-200301000-00004. [DOI] [PubMed] [Google Scholar]
- 33.Andrich S, Haastert B, Neuhaus E, et al. Excess mortality after pelvic fractures among older people. J Bone Miner Res. 2017;32:1789–1801. doi: 10.1002/jbmr.3116. [DOI] [PubMed] [Google Scholar]
- 34.Hill RM, Robinson CM, Keating JF. Fractures of the pubic rami Epidemiology and five-year survival. J Bone Jt Surg Br. 2001;83:1141–1144. doi: 10.1302/0301-620x.83b8.11709. [DOI] [PubMed] [Google Scholar]
- 35.Taillandier J, Langue F, Alemanni M, Taillandier-Heriche E. Mortality and functional outcomes of pelvic insufficiency fractures in older patients. Jt Bone Spine. 2003;70:287–289. doi: 10.1016/s1297-319x(03)00015-0. [DOI] [PubMed] [Google Scholar]
- 36.Mehling I, Hessmann MH, Rommens PM. Stabilization of fatigue fractures of the dorsal pelvis with a trans-sacral bar Operative technique and outcome. Injury. 2012;43:446–451. doi: 10.1016/j.injury.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 37.Osterhoff G, Ossendorf C, Wanner GA, Simmen HP, Werner CML. Percutaneous iliosacral screw fixation in S1 and S2 for posterior pelvic ring injuries: technique and perioperative complications. Arch Orthop Trauma Surg. 2011;131:809–813. doi: 10.1007/s00402-010-1230-0. [DOI] [PubMed] [Google Scholar]
- 38.Hopf JC, Krieglstein CF, Müller LP, Koslowsky TC. Percutaneous iliosacral screw fixation after osteoporotic posterior ring fractures of the pelvis reduces pain significantly in elderly patients. Injury. 2015;46:1631–1636. doi: 10.1016/j.injury.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 39.Wähnert D, Raschke MJ, Fuchs T. Cement augmentation of the navigated iliosacral screw in the treatment of insufficiency fractures of the sacrum A new method using modified implants. Int Orthop. 2013;37:1147–1150. doi: 10.1007/s00264-013-1875-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vaidya R, Kubiak EN, Bergin PF, et al. Complications of anterior subcutaneous internal fixation for unstable pelvis fractures: a multicenter study trauma. Clin Orthop Relat Res. 2012;470:2124–2131. doi: 10.1007/s11999-011-2233-z. [DOI] [PMC free article] [PubMed] [Google Scholar]