Abstract
Measure Accurately, Act Rapidly, and Partner With Patients (MAP) is an evidence‐based protocol implemented to improve hypertension control in a clinic for underserved patients (49.9% Medicaid and 50.2% black). Patients with hypertension seen during the year before intervention and with at least one visit during the 6‐month intervention (N = 714) were included. If initial attended blood pressure (BP; standard aneroid manometer) was ≥140/≥90 mm Hg, unattended automated office BP was measured in triplicate and averaged (Measure Accurately) using an Omron HEM‐907XL. When automated office BP was ≥140/≥90 mm Hg, Act Rapidly included intensification of antihypertensive medications, assessed by therapeutic inertia. Partner With Patients included BP self‐monitoring, reducing pill burden, and minimizing medication costs, which was assessed by systolic BP change per therapeutic intensification. Between baseline and the last study visit, BP control to <140/<90 mm Hg increased from 61.2% to 89.9% (P < .0001). MAP rapidly and significantly improved hypertension control in medically underserved patients, largely as a result of measuring BP accurately and partnering with patients.
Keywords: blood pressure, health equity, hypertension
1. INTRODUCTION
Approximately 34% of US adults, or nearly 86 million people, have hypertension. Hypertension was a factor in 410 624 US deaths in 2014.1 Approximately 45.6% of adults with hypertension have uncontrolled blood pressure (BP) of ≥140 mm Hg systolic BP (SBP) and/or ≥90 mm Hg diastolic BP (DBP).1, 2 Consequently, an estimated 39 million adults in the United States have uncontrolled hypertension and remain at risk for preventable cardiovascular disease.1 Dr Thomas Frieden, former Director of the Centers for Disease Control, concluded that better BP control could save more lives than any other single treatment intervention.3
Hypertension control is dependent on three crucial and interrelated variables. First, clinical measurement of BP must be accurate and reflect usual daytime values in order to properly diagnose hypertension and assess control. Unfortunately, BP measurements in clinical settings often include multiple methodologic errors,4 which limit accuracy. Even when measured accurately, clinic BP is higher than usual daytime values in about 20% of patients, reflecting an office or white‐coat effect.4
When hypertension is diagnosed and uncontrolled, adequate treatment is the next critical step. Unfortunately, limited confidence in office BP accuracy and concern that office BP may not represent usual daytime values contribute to therapeutic inertia.5 Therapeutic inertia reflects the failure to initiate or intensify pharmacotherapy when office BP is uncontrolled and can occur in as many as nine of 10 visits in adults with uncontrolled hypertension.6 Therapeutic inertia contributes to uncontrolled hypertension and may have a greater impact than patient nonadherence with prescribed therapy.6, 7
Suboptimal adherence with recommended lifestyle changes and antihypertensive medications prescribed to control BP represents the third key barrier to hypertension control. While no single intervention optimizes adherence,8 a multifactorial approach that includes engaging patients in shared decision‐making,9 patient‐centered care,10 reducing out‐of‐pocket costs,11 lowering the pill burden with single‐pill combinaitons,12, 13 consolidating refills,14 and using reminders15 can improve adherence.
Minority and uninsured adults often have poorer hypertension control than white and insured adults.16, 17 Medically underserved adults can experience limited access to health care and difficulties in obtaining and adhering to medications.17, 18 Our medically underserved patient population and limited clinical resources provided an important test of the Measure Accurately, Act Rapidly, Partner With Patients, Families, and Communities (MAP) framework19 in our 6‐month clinical effectiveness pilot study.
2. METHODS
2.1. Study design and regulatory considerations
Our MAP intervention used a quasi‐experimental, prestudy vs poststudy design. The protocol was reviewed by the institutional review board for Greenville Health System. MAP was exempt from written informed consent as the protocol utilized evidence‐based processes for managing hypertension. Approval was obtained to use data without protected health information for publication.
The American Medical Association (AMA) partnered with John Hopkins Medicine to develop the MAP framework: Measure Accurately, Act Rapidly, Partner With Patients, Families, and Communities.19 Each phase of MAP, designed to address a major barrier to better BP control, included extensive educational materials, audio podcasts, clinical checklists, and teleconferences. MAP was streamlined by the Care Coordination Institute and AMA to fit the needs of busy primary care practice sites including those with limited resources that serve diverse patient populations.
2.2. Setting
The study was conducted at a single site, the Center for Family Medicine, which serves as a principal location for training residents in Family Medicine in the Greenville Health System.
2.3. Study population: inclusion and exclusion criteria
The study population included eligible patients aged 18 to 85 years with a diagnosis of hypertension. Eligible patients had to have had at least one visit during the MAP intervention (February 1, 2016, through July 31, 2016) with a recorded BP and a documented office visit with a recorded BP in the 12 months before February 1, 2016. Descriptive data are also provided for adults with hypertension who were not seen during the MAP intervention but had one documented office visit with a recorded BP during the 6 months (August 1, 2015, through January 31, 2016) before the MAP intervention. Adults with hypertension who were exempt from the National Quality Foundation controlling high blood pressure measure (NQF‐18), eg, those with end‐stage renal disease and pregnant women, were excluded from the analysis.20
2.4. Clinical measurements
Hypertension control, the primary outcome variable, was defined as BP <140/<90 mm Hg. BP during the baseline period did not include unattended automated office BP (AOBP) and was performed according to usual practice at that time. During the intervention, BP control was defined by an initial attended BP <140/<90 mm Hg or by automated AOBP <140/<90 mm Hg, as described below, when initial attended BP was elevated. Height was measured using a vertical stadiometer with units standardized to the 0.01 meter. Since height is not measured on most visits, the most recent value was used including values before baseline. Weight was measured on a Scale‐Tronix model 5002 standing scale (Welch Allyn) and standardized to the nearest 0.1 kg. Body mass index was calculated as weight (kg)/height2 (m2).
2.5. Accurate BP measurement
2.5.1. Initial attended BP measurement
Personnel were trained to measure BP using an evidence‐based protocol. The first BP was obtained after the patient was seated for 5 minutes in a semiprivate area. During the 5‐minute waiting period, the presenting complaint, medical history, review of current medications, and other required items, eg, depression or falls risk screening, were obtained. BP was then measured quietly with the patient properly positioned and the measurement arm supported at heart level using a standard aneroid sphygmomanometer and an appropriately sized arm cuff. The single BP value was entered into the patient's electronic medical record. Values <140/<90 mm Hg were accepted as the BP value for that visit. Values of SBP ≥140 mm Hg and/or DBP ≥90 mm Hg led to a protocol recommendation for unattended AOBP.
2.5.2. Unattended AOBP
Patients with an elevated initial BP value were taken to a private examination room.21 The AOBP protocol was briefly described, the patient was properly positioned, and an appropriate‐sized cuff was applied to the upper arm supported at heart level. The staff member then promptly obtained one BP reading to ensure the Omron HEM‐907XL was working properly, activated a series of three additional readings at 1‐minute intervals without additional rest prior to the first unattended AOBP, and left the room. After the unattended AOBP was completed, the staff member returned and entered the mean of the three unattended AOBP values into the electronic health record with the comment “confirm” to distinguish the unattended AOBP from the attended intake BP.
2.6. Defining key process variables
Measure Accurately was assessed in adults with hypertension as: Act Rapidly was defined for adults with uncontrolled hypertension by the therapeutic inertia index: Partner With Patients was defined as the mean of the SBP change for each initiation or intensification of antihypertensive medication in adults with uncontrolled hypertension.
2.7. Monthly feedback reports for physicians and staff
Each staff and resident physician received a monthly “score card” that included BP control for their panel of adults with hypertension, the percentages with an elevated initial BP value that had confirmatory AOBP, their therapeutic inertia score, and the change of SBP with each therapeutic intensification. Patient‐level data for each metric were available to physicians.
2.8. Statistical analysis
Descriptive statistics were used to summarize demographic and clinical characteristics of the patients with hypertension at baseline and at first and last visits during the intervention. Data are reported as sample number, percentage, and standard error of the mean (SEM). The primary outcome variable was the change in BP control rate from baseline among adults with hypertension. Changes in the SBP between the baseline visit and both the first visit and the last visit during the intervention were secondary outcome variables. Additional outcome variables included the following three process variables: (1) percentages of adults with an elevated initial reading who had confirmatory measurement during the intervention period (Measure Accurately); (2) change in therapeutic inertia between the baseline and intervention period (Act Rapidly); and (3) difference in the change of SBP with each therapeutic intensification between the baseline and intervention period in eligible patients with uncontrolled hypertension (Partnering With Patients).
Two‐tailed t tests were performed to assess differences in demographic and clinical characteristics between patients with a baseline visit and at least one intervention visit and patients with only a baseline visit. Dependent group t tests were used to assess the outcome variables, and the process measures related to Measure Accurately, Act Rapidly, and Partner With Patients as defined above. Wilcoxon two‐sample tests were used to compare the distributions of SBP and DBP at baseline vs the last visit during the intervention. All analyses were performed in SAS version 9.4 (SAS Institute).
3. RESULTS
There were 908 patients with a baseline visit, with 714 (78.6%) who did and 194 (21.4%) who did not have another visit during the intervention period (Figure 1). The baseline control rate among the 908 patients was 62.6%. In the 714 patients with baseline and intervention visits, BP was controlled to <140/<90 mm Hg in 437 (61.2%) and uncontrolled in 277 (38.8%) patients. By the last visit during the intervention period, BP control had risen to 89.9%, a 28.7 percentage point increase. Of the patients with visits during the intervention period, 29.3% had one visit, 21.4% had two visits, and 49.3% had three or more visits, ie, more than two thirds (70.7%) had at least two visits.
Figure 1.
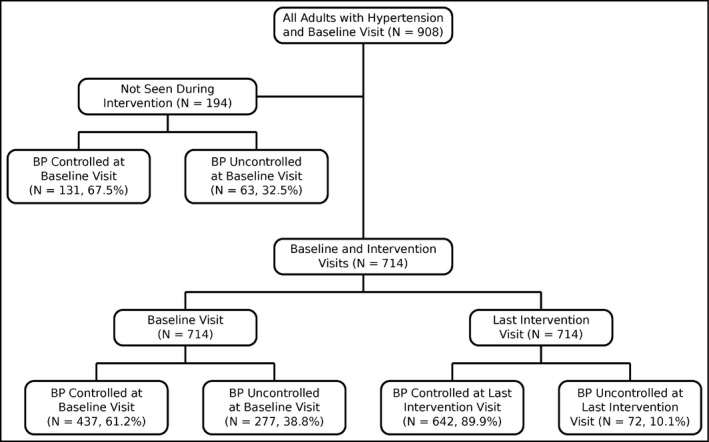
Flow diagram depicting the number of patients with hypertension and blood pressure (BP) control among those with only a baseline visit (n = 194) or both baseline and intervention visits (n = 714)
Table 1 presents comparisons of selected demographic and clinical characteristics, at baseline, between the 714 patients who also had a visit during the intervention period and the 194 who had only a baseline visit. Patients seen during the intervention were not significantly different from those with only a baseline visit by age category, sex, health insurance status, and mean SBP or DBP (all P > .05). Compared with patients seen during the intervention period, those seen only during the baseline visit were less likely to be black (37.1% vs 53.8%; P < .0001), to have a lower body mass index (34.2 vs 32.6 kg/m2; P < .05), or to have diabetes mellitus (29.9% vs 42.4%; P = .0015).
Table 1.
Comparison of characteristics of adults with hypertension at baseline, by intervention status, and BP control status
| All adults with hypertension | Adults with hypertension seen during intervention perioda | Adults with hypertension not seen during intervention periodb | P valuec | |||||
|---|---|---|---|---|---|---|---|---|
| Initial BP | <140/90 mm Hg | ≥140/90 mm Hg | <140/90 mm Hg | ≥140/90 mm Hg | ||||
| BP status | All patients | Controlled | Uncontrolled | All patients | Controlled | Uncontrolled | ||
| Patients, No. | 908 | 714 | 437 | 277 | 194 | 131 | 63 | |
| Age, y | 54.1 | 54.4 | 53.8 | 55.2 | 53 | 51.8 | 55.5 | .2087 |
| Age 18–35 y, No. (%) | 95 (10.5) | 72 (10.1) | 42 (9.6) | 30 (10.8) | 23 (11.9) | 19 (14.5) | 4 (6.3) | .4752 |
| Age 36–64 y, No. (%) | 616 (67.8) | 482 (67.5) | 307 (70.3) | 175 (63.2) | 134 (69.1) | 90 (68.7) | 44 (69.8) | .6794 |
| Age ≥ 65 y, No. (%) | 197 (21.7) | 160 (22.4) | 88 (20.1) | 72 (26.0) | 37 (19.1) | 22 (16.8) | 15 (23.8) | .3179 |
| Men, No. (%) | 320 (35.2) | 243 (34.0) | 147 (33.6) | 96 (34.7) | 77 (39.7) | 52 (39.7) | 25 (39.7) | .1439 |
| Race | ||||||||
| White, No. (%) | 421 (46.4) | 310 (43.4) | 202 (46.2) | 108 (39.0) | 111 (57.2) | 77 (58.8) | 34 (54.0) | .0006 |
| Black, No. (%) | 456 (50.2) | 384 (53.8) | 221 (50.6) | 163 (58.8) | 72 (37.1) | 47 (35.9) | 25 (39.7) | <.0001 |
| BMI, kg/m2 | 33.8 | 34.2 | 34.1 | 34.3 | 32.6 | 32.1 | 33.7 | .0329 |
| Diabetes mellitus, No. (%) | 361 (39.8) | 303 (42.4) | 190 (43.5) | 113 (40.8) | 58 (29.9) | 36 (27.5) | 22 (34.9) | .0015 |
| Insurance | ||||||||
| Medicaid, No. (%) | 453 (49.9) | 359 (50.3) | 231 (52.9) | 128 (46.2) | 94 (48.5) | 66 (50.4) | 28 (44.4) | .6523 |
| Medicare, No. (%) | 211 (23.2) | 176 (24.6) | 104 (23.8) | 72 (26.0) | 35 (18.0) | 25 (19.1) | 10 (15.9) | .0534 |
| Private or other, No. (%) | 220 (24.2) | 165 (23.1) | 97 (22.2) | 68 (24.5) | 55 (28.4) | 31 (23.7) | 24 (38.1) | .1311 |
| Uninsured, No. (%) | 24 (2.6) | 14 (2.0) | 5 (1.1) | 9 (3.2) | 10 (5.2) | 9 (6.9) | 1 (1.6) | .0576 |
| SBP/DBP, mm Hg | ||||||||
| <140/<90, No. (%) | 568 (62.6) | 437 (61.2) | 437 (100) | 131 (67.5) | 131 (100) | .1069 | ||
| 140–159/90–99, No. (%) | 310 (34.1) | 253 (35.4) | 253 (91.3) | 57 (29.4) | 57 (90.5) | .1151 | ||
| ≥160/≥100, No. (%) | 30 (3.3) | 24 (3.4) | 24 (8.7) | 6 (3.1) | 6 (9.5) | .8530 | ||
Abbreviations: BMI, body mass index; BP, blood pressure DBP, diastolic blood pressure; SBP, systolic blood pressure.
Hispanic data and counts from categories may not add up to the total because of missing data.
aPatients with baseline visit and at least one follow‐up visit during the intervention period, February 2016 to July 2016.
bPatients with no visit during the intervention with a baseline visit between August 2015 to January 2016.
c t test to compare characteristics between patients in the intervention and those with no visit during the intervention period.
The difference between the BP from the first intervention visit and baseline visit among adults with controlled vs uncontrolled hypertension served as an indirect measure for the change of BP resulting from improved measurement technique. By this measure, SBP rose 2.5 mm Hg (P < .01) for the 301 patients with BP controlled at baseline and fell 12.7 mm Hg (P < .001) for those 109 patients who did not have BP control at baseline (data not shown). Measure Accurately was also assessed by the difference between an elevated initial BP at any visit during the intervention period (203) and the unattended AOBP. For those with an elevated initial BP, their unattended AOBP was 2.5 mm Hg lower (P < .05).
The distributions of SBP and DBP shifted between the baseline and last intervention visit to lower values (P < .0001) among the target group of 277 adults with uncontrolled BP at the last baseline visit (Figure 2). The percentage of adults with uncontrolled SBP in the stage 1 range of 140 to 159 mm Hg declined from 71.5% at baseline to 13.4% by the last intervention visit. The percentage of patients with stage 1 DBP of 90 to 99 mm Hg declined from 44.4% at the first to 8.0% at the last intervention visit. Percentages of patients with stage 2 SBP of ≥160 mm Hg declined from 14.4% at baseline to 4.7% at the last visit during the intervention period.
Figure 2.
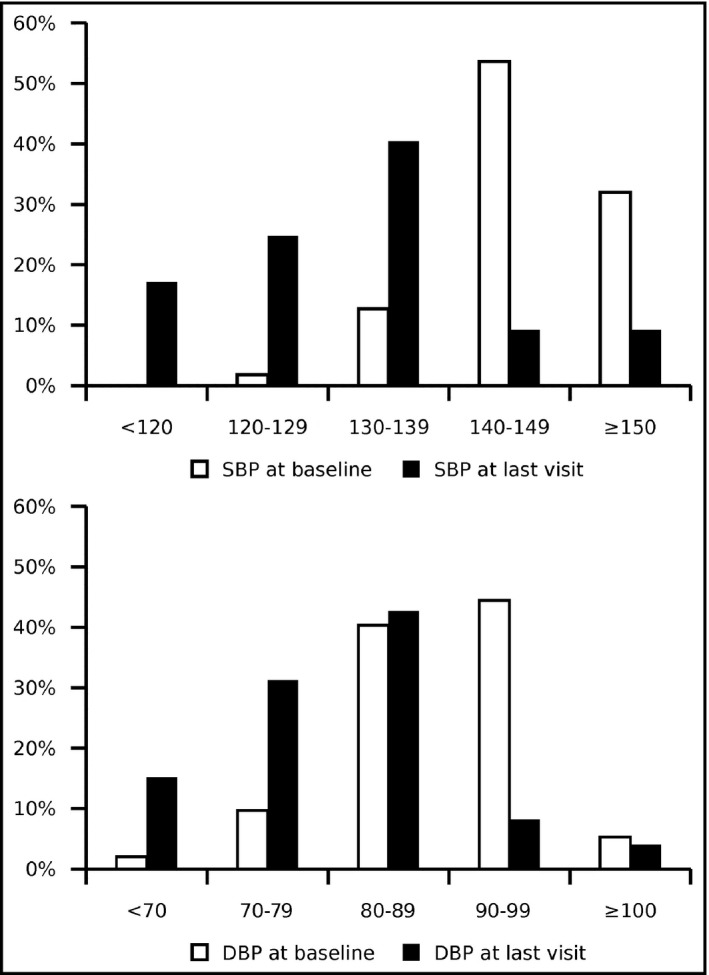
Distributions of systolic blood pressure (SBP) and diastolic blood pressure (DBP) for patients with uncontrolled hypertension at baseline and at the last visit during the intervention period (n = 277)
Patient demographic and clinical characteristics at the last intervention visit, which included unattended AOBP for patients with an elevated attended BP, are presented in Table 2. At their last intervention visit, 628 patients with hypertension had controlled BP and 86 had uncontrolled BP based on their initial clinic BP value. Of the 86 adults with initially elevated clinic BP at the last visit, 59 (68.6%) had confirmatory AOBP, which showed that 14 had controlled BP and 45 had uncontrolled BP confirmed. For patients with a confirmatory AOBP, their initial attended BP was 149/89 mm Hg vs 126/78 mm Hg with AOBP.
Table 2.
| Initial BP at last visit | <140/90 mm Hg | ≥140/90 mm Hg | ≥140/90 mm Hg | ≥140/90 mm Hg |
|---|---|---|---|---|
| Last visit—initial BP | Last visit—confirmatory BPb | |||
| Confirmatory AOBP | NA | NA | <140/90 mm Hg | ≥140/90 mm Hg |
| BP status | Controlled | Uncontrolled | Controlled | Uncontrolled |
| No. | 628 | 86b | 14b | 45b |
| Age, mean, y | 54.4 | 54.2 | 47.1 | 55.5 |
| Age 18–35 y, No. (%) | 61 (9.7) | 11 (12.8) | 5 (35.7) | 5 (11.1) |
| Age 36–64 y, No. (%) | 426 (67.8) | 56 (65.1) | 8 (57.1) | 28 (62.2) |
| Age ≥65 y, No. (%) | 141 (22.5) | 19 (22.1) | 1 (7.1) | 12 (26.7) |
| Men, No. (%) | 200 (31.8) | 43 (50.0) | 6 (42.9) | 22 (48.9) |
| Race, No. (%) | ||||
| White | 282 (44.9) | 28 (32.6) | 2 (14.3) | 13 (28.9) |
| Black | 327 (52.1) | 57 (66.3) | 12 (85.7) | 31 (68.9) |
| BMI, kg/m2 | 34.1 (0.4) | 34.6 (1.2) | 41.2 (3.4) | 33.5 (1.5) |
| Diabetes mellitus, No. (%) | 270 (43.0) | 33 (38.4) | 4 (28.6) | 19 (42.2) |
| Insurance, No. (%) | ||||
| Medicaid | 326 (51.9) | 33 (38.4) | 7 (50.0) | 18 (40.0) |
| Medicare | 155 (24.7) | 21 (24.4) | 1 (7.1) | 11 (24.4) |
| Private or other | 136 (21.7) | 29 (33.7) | 6 (42.9) | 14 (31.1) |
| Uninsured | 11 (1.8) | 3 (3.5) | 0 (0) | 2 (4.4) |
| SBP, mean, mm Hg, | ||||
| Initial SBP, mm Hg | 125 (0.4) | 149 (1.2) | ||
| Confirmatory AOBP, SBP, mm Hg | 126 (2.1) | 151 (2.0) | ||
| DBP, mean, mm Hg | ||||
| Initial DBP, mm Hg | 76 (0.3) | 89 (1.2) | ||
| Confirmatory AOBP DBP, mm Hg | 78 (2.9) | 91 (1.8) | ||
| ≥160/≥100 mm Hg, No. (%) | NA | 17 (19.8) | NA | 7 (15.6) |
| SBP change from baseline, mean, mm Hg | −7.2 (0.6)*** | 8.4 (1.9)*** | −8.3 (3.8)* | 9.4 (2.9)** |
| DBP change from baseline, mean, mm Hg | −4.5 (0.4)*** | 4.2 (1.4)** | −4.9 (2.9) | 6.0 (1.9)** |
Data are presented as mean and standard error or number (percentage).
Abbreviations: BMI, body mass index; DBP, diastolic blood pressure; NA, not available; SBP, systolic blood pressure.
Hispanic ethnicity data were unavailable. Data and counts from categories may not add up to the total because of missing data.
aAll patients had baseline and at least one follow‐up visit during the intervention period, February 2016 to July 2016.
bConfirmatory automated office blood pressure (AOBP) data were available in 59 and missing in 27 of the 86 patients with uncontrolled initial blood pressure (BP) at the last intervention visit.
*P < .05, **P < .01, ***P < .001.
At the baseline visit, BP was controlled in 65.2% of white and 57.6% of black adults with hypertension. At the last intervention visit accounting for the AOBP measurement, BP was controlled in 96.6% of white and 88.2% of black patients. The change in BP control from baseline to intervention was similar in white and black adults (+31.4% vs +29.6%, P = not significant). Among Medicaid patients, BP control increased from 65.5% to 92.6%. Regardless of their control status at baseline, based on the initial BP measurement at the last visit during the intervention, those with BP control experienced a 7.2‐mm Hg decrease in SBP from baseline (P < .001), while those with an elevated BP had a 8.4‐mm Hg increase in SBP from baseline (P < .001).
Table 3 compares characteristics between the baseline and the last visit for the 277 adults seen during the intervention who had an elevated baseline BP. On average, their BP declined from 147/88 mm Hg at baseline to 131/79 mm Hg by the last intervention (P < .0001/<.0001). The percentages of patients prescribed various antihypertensive medication classes did not change between the baseline and last intervention visits (all P > .05). Therapeutic inertia declined slightly from baseline during the intervention, but the difference was not statistically significant (43.5% vs 37.5%; all P = not significant). The decline in SBP for each therapeutic intensification, a proxy for Partnering With Patients, increased from baseline to the intervention period (−8.3 mm Hg vs −21.6 mm Hg, P = .0004).
Table 3.
Comparison of characteristics of adults with hypertension with uncontrolled baseline BP between baseline and the last visit during the intervention period (N = 277)
| Baseline: last visit before February 2016 | Intervention: latest visit between February 2016 and July 2016 | P value | |
|---|---|---|---|
| Initial BP | |||
| SBP, mm Hg | 147 (0.65) | 131 (0.81) | <.0001 |
| DBP, mm Hg | 88 (0.52) | 79 (0.60) | <.0001 |
| AOBP | |||
| SBP, mm Hg | NA | 147 (2.61) | NA |
| DBP, mm Hg | NA | 91 (1.96) | NA |
| Patients prescribed BP medications, No. (%) | 235 (84.8) | 241 (87.0) | .2213 |
| α1‐Receptor blocker, % | 12.6 | 14.1 | .2489 |
| ACEI or ARB, % | 59.9 | 60.6 | .7636 |
| β‐Blocker, % | 30.7 | 28.9 | .3182 |
| Dihydropyridine CCB, % | 37.2 | 41.9 | .0578 |
| Nondihydropyridine CCB, % | 3.6 | 4 | .3182 |
| Diuretic, % | 71.5 | 72.2 | .7582 |
| Thiazide‐type, % | 69 | 68.6 | .8843 |
| Loop, % | 9.7 | 9 | .5281 |
| Potassium‐sparing, % | 3.6 | 3.2 | .5646 |
| Aldosterone antagonist, % | 4 | 4.3 | .7395 |
| Therapeutic inertia,%* | 43.5 | 37.6 | .5429 |
| ΔSBP/RxΔ, mm Hg | −8.3 (2.0) | −21.6 (2.1) | .0004 |
Data are presented as mean and standard error or number (percentage). Automated office blood pressure (AOBP) is the mean of three readings with the patient alone in an examination room).
Abbreviations: ACEI, angiotensin‐converting enzyme inhibitor; ARB, angiotensin receptor blocker; CCB, calcium channel blocker; DBP, diastolic blood pressure; ΔSBP; RxΔ, change in systolic blood pressure after the most recent visit with intensification of antihypertensive medications for uncontrolled hypertension; NA, not available; SBP, systolic blood pressure.
*Percentage of visits with uncontrolled blood pressure (BP) with no change in antihypertensive medications.
4. DISCUSSION
Our MAP pilot study demonstrated a clinically and statistically significant improvement in BP control in a predominantly underserved population. BP control improved from 61.2% to 89.9% (P < .0001) in 714 adults with hypertension in only 6 months. The large short‐term rise in hypertension control equals or exceeds mean changes with team‐based care, perhaps the most effective intervention, during the past 10 to 15 years.22, 23 BP control attained in this underserved population also approximates control in a large managed care organization with a long‐standing hypertension control program.24
While MAP facilitated team‐based care, it did not include additional personnel, eg, nurse clinicians or pharmacists, nutritionists, or community health workers, typically included in team‐based interventions.22, 23 No incremental resources were provided in our streamlined MAP intervention except for automated BP monitors and approximately 2 hours of practice facilitation weekly during the first 3 months, then 2 hours every other week during the last 3 months. The practice facilitator focused on appropriate use of AOBP monitoring (Measure Accurately) when the initial value was high and patient engagement with an emphasis on monthly office visits or other contact in patients with uncontrolled hypertension. In fact, the Measure Accurately and Partner With Patients components explained most of the BP reduction during our MAP pilot study. Therapeutic inertia was already relatively low at <50% during baseline and did not significantly decline during the intervention. Therapeutic inertia in the current study was much lower than in earlier studies, which concluded that this variable was a greater barrier to hypertension control than patient adherence.7 The fall in SBP with each therapeutic intensification, a proxy for adherence, increased (Table 3). When patients with uncontrolled hypertension were selected, the subsequent decline in BP and improvement in control is partially explained by regression to the mean. Regression to the mean is an unlikely explanation for the large rise in hypertension control seen in this clinic population, as this level of change is rarely seen.
The patient population in our MAP pilot study qualified as “medically underserved” based on demographic characteristics and health insurance status. Our clinic serves a large proportion of black adults who are less likely to have controlled hypertension than whites, although the absolute difference was small. Lower hypertension control rates are documented in black and Hispanic than white adults in the United States, especially when assessed in the context of other variables that impact BP control.16, 25 Of importance, MAP raised BP control similarly in black and white patients (+31.4% vs +29.6%, P = not significant).
It is important to assess our current MAP results in the context of other quality improvement projects in hypertension. Team‐based care is consistent among the most effective interventions for controlling BP.22, 23 In team‐based care, healthcare professionals, eg, advanced nurse practitioners, pharmacists, nutritionists, and community health workers, practicing at the top of their licenses, partner with the patient and primary physician. Team members have complementary roles to implement and coordinate evidence‐based care, to train and equip patients in self‐management, and to ensure follow‐up.
A meta‐analysis of team‐based care interventions from 1980 to 2003 reported a median absolute improvement of 21.8% in SBP and 17.0% improvement in DBP control.22, 23 Studies of team‐based care and BP control from 2003 to 2012 showed median absolute improvement of 12 percentage points. The diminishing impact of team‐based care likely reflects higher baseline control rates, especially since 1999 to 2002. Systematic reviews indicated that team‐based interventions were more effective than other interventions, eg, medical education, practice data audit and feedback reporting, patient BP self‐monitoring, and reminder systems in electronic health records.22, 23
A hypertension quality improvement program was conducted among 14 clinics in Baltimore, Maryland, serving a disproportionately low‐income, black population.26 The factorial study design included26 enhancing physician communication skills to better understand and engage their patients and improving patient communication skills related to engagement, activation, and empowerment. Yet, after 12 months, the interventions did not lower BP or improve control significantly compared with no‐intervention controls. A larger sample size may have led to positive results as SBP in patients with uncontrolled hypertension declined a mean of 13.2 mm Hg with the combined intervention, 16.8 mm Hg with the patient intervention, and 10.6 mm Hg with the physician intervention compared with only 2.0 mm Hg without intervention. The 16‐mm Hg mean reduction of SBP among adults with uncontrolled hypertension in our pilot study is similar in magnitude to the reduction seen among the intervention groups in the Baltimore study.26
A pooled analysis was reported on three cluster randomized trials of health systems–level interventions to improve hypertension control.27 While the three interventions were not identical, all were designed to improve patient adherence and reduce therapeutic inertia to attain goal BP. The investigators found that initial improvements of hypertension control in blacks were not sustained over the 12‐month study. They suggested that future studies should include a run‐in period since improvements in hypertension control should be expected at intervention and control sites. Moreover, studies should be powered on small differences in effect size between intervention and control clinics. In our pilot study, the intervention lasted for 6 months. Based on this and other reports, it will be important to assess the sustained effects of our MAP intervention over a year or more.
5. STUDY LIMITATIONS
Several limitations of our study should be noted, including the single study site that precludes a randomized control group and the limited duration of the intervention. Hypertension control during the baseline period reflected usual office BP measurements rather than protocol‐based BP measurements during the intervention. While not all patients seen during the baseline period had a follow‐up visit during the intervention, the majority of eligible patients (78.6%) were included, lessening the risk of biased sampling. However, patients with both baseline and intervention visits included in the analysis were more likely to be black and to have diabetes mellitus than patients with only a baseline visit who were excluded. There was no significant change in therapeutic inertia from the baseline period to the intervention period, although baseline therapeutic inertia was already relatively low at <50%. Prior evidence suggests that these lower levels of “clinical inaction” may be appropriate.28
6. CONCLUSIONS
The preventable toll of hypertension‐related cardiovascular and renal diseases is large, especially in medically underserved patients, and the benefits of better hypertension control are well documented. Our pilot study shows that MAP is an effective framework for rapidly improving hypertension control in a resource‐limited clinic that serves medically underserved adults. To examine the potential for widespread dissemination, it is important to assess both short‐ and long‐term effects of MAP in a range of clinics that care for diverse populations.
CONFLICTS OF INTEREST
Brent M. Egan has received income as a consultant from AstraZeneca, Inside Edge, Medtronic, and Valencia; research support from Boehringer; and royalties from UpToDate. R. Bruce Hanlin, Irfan M. Asif, Gregory Wozniak, Jianing Yang, Michael Rakotz, Susan E. Sutherland, and Rob Davis have no conflicts of interest to disclose.
ACKNOWLEDGMENTS
Care Coordination Institute: The authors thank Lindsey Bayne for facilitating update and implementation of the MAP intervention, Luisa Chmielecki for logistical support, and Shaun Wagner and Dave Ramsey with database management and quality indicator reports for physicians and staff implementing MAP. Department of Family Medicine: The authors thank Sheri Johnston for tirelessly implementing MAP into the clinic routine. American Medical Association: The authors thank Laken Barkowski for facilitating the update and implementation of the MAP intervention.
Hanlin RB, Asif IM, Wozniak G, et al. Measure Accurately, Act Rapidly, and Partner With Patients (MAP) improves hypertension control in medically underserved patients: Care Coordination Institute and American Medical Association Hypertension Control Project Pilot Study results. J Clin Hypertens. 2018;20:79–87. 10.1111/jch.13141
Funding information
The work in this article was funded in part by grants to the Care Coordination Institute from the American Medical Association and from the Centers for Disease Control through the South Carolina Department of Health and Environmental Control.
The findings and conclusions in this report are those of the authors (Gregory Wozniak, Jianing Yang, Michael Rakotz) and do not necessarily represent the views of the American Medical Association.
REFERENCES
- 1. Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart disease and stroke statistics––2017 update: a report from the American Heart Association. Circulation. 2017;135:e146‐e603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Merai R, Siegel C, Rakotz M, et al. CDC grand rounds: a public health approach to detect and control hypertension. MMWR Morb Mortal Wkly Rep. 2016;65:1261‐1264. [DOI] [PubMed] [Google Scholar]
- 3. Freiden TR. The future of public health. N Engl J Med. 2015;373:1748‐1754. [DOI] [PubMed] [Google Scholar]
- 4. Pickering TG, Hall JE, Appel LJ, et al. Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation. 2005;111:697‐716. [DOI] [PubMed] [Google Scholar]
- 5. Holland N, Segraves D, Nnadi VO, Belletti DA, Wogen J, Arcona S. Identifying barriers to hypertension care: implications for quality improvement initiatives. Dis Manage. 2008;11:71‐77. [DOI] [PubMed] [Google Scholar]
- 6. Okonofua EC, Simpson K, Jesri A, Rehman S, Durkalski V, Egan BM. Therapeutic inertia is an impediment to achieving the healthy people 2010 blood pressure control goals. Hypertension. 2006;47:1‐7. [DOI] [PubMed] [Google Scholar]
- 7. Daugherty SL, Powers JD, Magid DJ, et al. The association between medication adherence and treatment intensification with blood pressure control in resistant hypertension. Hypertension. 2012;60:303‐309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Zullig LL, Peterson ED, Bosworth HB. Ingredients of successful interventions to improve medication adherence. JAMA. 2013;310:2611‐2612. [DOI] [PubMed] [Google Scholar]
- 9. Fowler FJ Jr, Gerstein BS, Barry MJ. How patient centered are medical decision? Results of a national survey. JAMA Intern Med. 2013;173:1215‐1221. [DOI] [PubMed] [Google Scholar]
- 10. Roumie CL, Greevy R, Wallston KA, et al. Patient centered primary care is associated with patient hypertension medication adherence. J Behav Med. 2011;34:244‐253. [DOI] [PubMed] [Google Scholar]
- 11. Eaddy MT, Cook CL, O'Day K, Burch SP, Cantrell CR. How patient cost‐sharing trends affect adherence and outcomes: a literature review. Pharm Ther. 2012;37:45‐55. [PMC free article] [PubMed] [Google Scholar]
- 12. Lauffenburger JC, Landon JE, Fischer MA. Effect of combination therapy on adherence among U.S. patients initiating therapy for hypertension: a cohort study. J Gen Intern Med. 2017;32:619‐625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Xie L, Frech‐Tamas F, Marrett E, Baser O. A medication adherence and persistence comparison of hypertensive patients treated with single‐, double‐ and triple‐pill combination therapy. Curr Med Res Opin. 2014;30:2415‐2422. [DOI] [PubMed] [Google Scholar]
- 14. Choudhry NK, Fischer MA, Avorn J. The implications of therapeutic complexity on adherence to cardiovascular medications. Arch Intern Med. 2011;171:814‐822. [DOI] [PubMed] [Google Scholar]
- 15. Thakkar J, Kurup R, Laba TL, et al. Mobile telephone text messaging for medication adherence in chronic disease. JAMA Intern Med. 2016;176:340‐349. [DOI] [PubMed] [Google Scholar]
- 16. Yoon SS, Fryar CD, Carroll MD. Hypertension prevalence and control among adults: United States, 2011–2014. NCHS Data Brief, #220, November 2015. https://www.cdc.gov/nchs/data/databriefs/db220.pdf. [PubMed]
- 17. Egan BM, Li J, Small J, Nietert PJ, Sinopoli A. The growing gap in hypertension control between insured and uninsured adults: NHANES 1988–2010. Hypertension. 2014;64:997‐1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lewis LM, Ogedegbe C, Ogedegbe G. Enhancing adherence of antihypertensive regimens in hypertensive African‐Americans: current and future prospects. Expert Rev Cardiov Ther. 2012;10:1375‐1380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. STEPS Forward: Improving blood pressure control. AMA in partnership with Johns Hopkins. https://www.stepsforward.org/modules/hypertension-blood-pressure-control#section-conclusion.
- 20. Measure #236 (NQF 0018): Controlling high blood pressure. https://www.auanet.org/common/pdf/practices-resources/quality/pqrs-toolkit/2016/Measured-Specs/measure_236.pdf.
- 21. Myers MG. Eliminating the human factor in office blood pressure measurement. J Clin Hypertens (Greenwich). 2014;16:83‐86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Walsh J, McDonald KM, Shojania KG, et al. Quality improvement strategies for hypertension management: a systematic review. Med Care. 2006;44:646‐657. [DOI] [PubMed] [Google Scholar]
- 23. Proia KK, Thota AB, Njie GJ, et al. Team‐based care and improved blood pressure control: a community guide systematic review. Am J Prev Med. 2014;47:86‐99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Jaffe MC, Lee GA, Young JD, et al. Improved blood pressure control associated with a large‐scale hypertension program. JAMA. 2013;310:699‐705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Egan BM, Li J, Hutchison FN, Ferdinand KC. Hypertension in the United States 1999–2012: progress toward healthy people 2020 goals. Circulation. 2014;30:1692‐1699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Cooper LA, Roter DL, Carson KA, et al. A randomized trial to improve patients‐centered care and hypertension control in underserved primary care patients. J Gen Intern Med. 2011;26:1297‐1304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Pavlik VN, Chan W, Hyman DJ, et al. Designing and evaluating health systems level hypertension control interventions for African‐Americans: lessons from a pooled analysis of three cluster randomized trials. Curr Hypertens Rep. 2015;11:123‐131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Crowley MJ, Smith VA, Olsen MK, et al. Treatment intensification in a hypertension telemanagement trial. Clinical inertia or good clinical judgment? Hypertension. 2011;58:552‐558. [DOI] [PubMed] [Google Scholar]


