Abstract
This study examines the association of anchoring with patient willingness to use a monthly injectible medication for psoriasis.
Biological therapies are highly effective in treating immune-mediated diseases, such as psoriasis, but patients are often fearful of injections. The fear of injection is inherently subjective and may be easily modified.
Anchoring is the tendency for humans to make judgments relative to the first piece of information presented. Patients who have never taken an injection may subjectively compare taking an injection to not taking one. This comparison can be a frightening hurdle to starting an injectable medication. In a similar fashion, a $500 product (the anchor) marked down to $100 seems like a much better deal than if the product were simply offered at $100.
Since psychological anchors can be arbitrary, resetting the anchor may be a potential approach to help patients overcome fear of injection. We assessed whether patients offered a once-monthly injectable option would be more amenable to the injection if initially anchored to a once-daily injectable.
Methods
Participants received a study fact sheet letter detailing the study and informed consent was obtained verbally and assumed based on patient completion of the questionnaire. They were not compensated for participating. Written consent was waived by the institutional review board at the Wake Forest School of Medicine, which approved the study, because the research presented no more than minimal risk of harm to participants and involved no procedures for which consent is normally required outside of the research context. One hundred patients with a clinical diagnosis of psoriasis, aged 18 years or older, and not prescribed an injectable medication were recruited and randomized to either completing a control or intervention questionnaire. The 50 participants in the intervention group were first asked an anchoring question assessing their willingness to start a once-daily injectable medication and then subsequently queried on their willingness to start a once-monthly injection for their psoriasis (a scale of 1-10 with 1 being “not willing” and 10 being “very willing”). The 50 participants in the control group were only asked their willingness to start a once-monthly injection. Scores were treated as ordinal data and evaluated using the Mann-Whitney U test.
Results
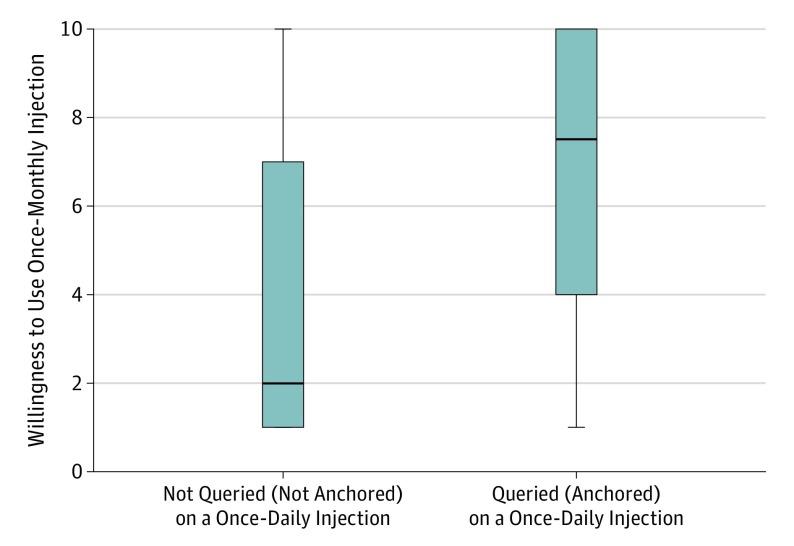
There were no significant differences between the groups’ baseline characteristics (Table). Participants anchored to a once-daily injectable biologic intervention were more willing to start a once-monthly injectable biologic (median, 7.5) than those not anchored (median, 2.0) to the once-daily injectable medication (P < .001) (Figure). Subgroup race and age analysis was not possible owing to small subgroup size.
Table. Summary of Baseline Characteristicsa.
| Variable | Groups | |
|---|---|---|
| Control (n = 50) | Anchored (n = 50) | |
| Age, mean (SD), y | 53.0 (15.9) | 51.1 (16.4) |
| Sex, No. (%) | ||
| Male | 26 (52) | 23 (46) |
| Female | 24 (48) | 27 (54) |
| White race, No. (%)b | 47 (94) | 40 (98) |
There were no significant differences between the group’s baseline characteristics.
Race was self-reported.
Figure. The Anchoring Effect Increases Patients’ Willingness to Consider Injection Treatment for Psoriasis.
Patients were asked how willing they would be, on a 1 to 10 scale, to take an injectable treatment for their psoriasis once per month. The intervention group was first asked how willing they would be to take the injection once per day. Median willingness to a once-monthly injection in the control and intervention group were 2.0 and 7.5, respectively; the distributions in the 2 groups differed significantly (Mann-Whitney U = 733; n1 = n2 = 50; 2-tailed P < .001 ). Boxes indicate 25th and 75th percentiles; the horizontal line in the box indicates group median; the error bars indicate minimum and maximum values, excluding outliers.
Discussion
The use of anchoring interventions is well studied in behavioral economics, but its applications in medicine may be in its infancy. Human perception is inherently subjective, and such perceptions are easily malleable. Our data suggest that if a patient were first counseled regarding the possibility of a daily injectable biologic medication, they would be less hesitant to the warranted monthly injection. We made the once-monthly injection seem like it was a bargain in terms of the number of injections needed. The objective number of injections did not change, but the perception of that number changed dramatically.
Such an anchoring phenomenon in pain perception is familiar in the treatment of psoriasis with biologics (etanercept). Patients prescribed prefilled syringes often report greater pain with the autoinjector. However, patients starting on the autoinjector who have never received the prefilled syringe, rarely, if ever, complain about its level of pain.
An important consideration is the ethics of manipulating patients’ subjective perceptions. There is always an anchor—as humans we are consistently making judgments relative to other values. The ethical dilemma is whether or not to make a rational choice of what the anchor should be. Choosing one that helps patients is appropriate, and potentially, powerful. Using the approach to encourage greater purchases of cosmetic services (eg, “Botox marked down this week”) might be effective, but most likely, not the best medical use of this psychological phenomenon.
As such, we expect anchoring to be a very general phenomenon that could be used to impact a wide array of patient decisions (safety or efficacy discussions). As part of a complete treatment education program, addressing appropriate anchors may be a very low-cost, useful intervention.
References
- 1.Sandoval LF, Pierce A, Feldman SR. Systemic therapies for psoriasis: an evidence-based update. Am J Clin Dermatol. 2014;15(3):165-180. [DOI] [PubMed] [Google Scholar]
- 2.Wilson TD, Houston CE, Etling KM, Brekke N. A new look at anchoring effects: basic anchoring and its antecedents. J Exp Psychol Gen. 1996;125(4):387-402. [DOI] [PubMed] [Google Scholar]
- 3.Brewer NT, Chapman GB. The fragile basic anchoring effect. J Behav Decis Mak. 2002;15(1):65-77. [Google Scholar]
- 4.Davis SA, Feldman SR. An Illustrated Dictionary of Behavioral Economics for Healthcare Professionals. CreateSpace Independent Publishing Platform; Charleston, NC: 2014. [Google Scholar]