Key Points
Question
Have hospital readmission reductions associated with the Affordable Care Act had the unintended consequence of increasing mortality after hospitalization?
Findings
In this cohort study of more than 5 million Medicare fee-for-service hospitalizations for heart failure, acute myocardial infarction, and pneumonia from 2008 to 2014, reductions in hospital 30-day readmission rates were weakly but significantly correlated with reductions in 30-day mortality rates after hospital discharge (correlation coefficients, 0.066, 0.067, and 0.108, respectively).
Meaning
These findings do not support increasing postdischarge mortality related to reducing hospital readmissions.
This cohort study examines whether reductions in hospital readmission rates following hospitalizations for heart failure, acute myocardial infarction, and pneumonia are associated with mortality rates after hospital discharge among Medicare fee-for-service beneficiaries.
Abstract
Importance
The Affordable Care Act has led to US national reductions in hospital 30-day readmission rates for heart failure (HF), acute myocardial infarction (AMI), and pneumonia. Whether readmission reductions have had the unintended consequence of increasing mortality after hospitalization is unknown.
Objective
To examine the correlation of paired trends in hospital 30-day readmission rates and hospital 30-day mortality rates after discharge.
Design, Setting, and Participants
Retrospective study of Medicare fee-for-service beneficiaries aged 65 years or older hospitalized with HF, AMI, or pneumonia from January 1, 2008, through December 31, 2014.
Exposure
Thirty-day risk-adjusted readmission rate (RARR).
Main Outcomes and Measures
Thirty-day RARRs and 30-day risk-adjusted mortality rates (RAMRs) after discharge were calculated for each condition in each month at each hospital in 2008 through 2014. Monthly trends in each hospital’s 30-day RARRs and 30-day RAMRs after discharge were examined for each condition. The weighted Pearson correlation coefficient was calculated for hospitals’ paired monthly trends in 30-day RARRs and 30-day RAMRs after discharge for each condition.
Results
In 2008 through 2014, 2 962 554 hospitalizations for HF, 1 229 939 for AMI, and 2 544 530 for pneumonia were identified at 5016, 4772, and 5057 hospitals, respectively. In January 2008, mean hospital 30-day RARRs and 30-day RAMRs after discharge were 24.6% and 8.4% for HF, 19.3% and 7.6% for AMI, and 18.3% and 8.5% for pneumonia. Hospital 30-day RARRs declined in the aggregate across hospitals from 2008 through 2014; monthly changes in RARRs were −0.053% (95% CI, −0.055% to −0.051%) for HF, −0.044% (95% CI, −0.047% to −0.041%) for AMI, and −0.033% (95% CI, −0.035% to −0.031%) for pneumonia. In contrast, monthly aggregate changes across hospitals in hospital 30-day RAMRs after discharge varied by condition: HF, 0.008% (95% CI, 0.007% to 0.010%); AMI, −0.003% (95% CI, −0.005% to −0.001%); and pneumonia, 0.001% (95% CI, −0.001% to 0.003%). However, correlation coefficients in hospitals’ paired monthly changes in 30-day RARRs and 30-day RAMRs after discharge were weakly positive: HF, 0.066 (95% CI, 0.036 to 0.096); AMI, 0.067 (95% CI, 0.027 to 0.106); and pneumonia, 0.108 (95% CI, 0.079 to 0.137). Findings were similar in secondary analyses, including with alternate definitions of hospital mortality.
Conclusions and Relevance
Among Medicare fee-for-service beneficiaries hospitalized for heart failure, acute myocardial infarction, or pneumonia, reductions in hospital 30-day readmission rates were weakly but significantly correlated with reductions in hospital 30-day mortality rates after discharge. These findings do not support increasing postdischarge mortality related to reducing hospital readmissions.
Introduction
Significant reductions have occurred in 30-day readmission rates for US Medicare beneficiaries since passage of the Affordable Care Act (ACA). The ACA established the Hospital Readmissions Reduction Program (HRRP), which required the Centers for Medicare & Medicaid Services (CMS) to reduce payments to hospitals with higher-than-expected readmission rates for targeted conditions, including heart failure (HF), acute myocardial infarction (AMI), and pneumonia. Although financial penalties began in 2012, hospitals were provided their readmission performance relative to others from 2009 onward. Within this context, 30-day readmission rates for these 3 conditions collectively declined from 21.5% to 17.8% between 2007 and 2015.
Whether hospitals’ increased focus on lowering readmissions produced unintended consequences, particularly increased mortality after hospitalization, is unknown. Researchers and advocacy groups have raised concerns that hospitals, wary of financial penalties, might deter the readmission of patients requiring inpatient care, thereby increasing mortality after discharge. However, strategies designed to lower readmissions through improved hospital, transitional, and postacute care may have instead reduced both readmission and mortality rates following hospitalization. Research to date examining the relationship of hospital readmission and mortality rates has used cross-sectional data, with inconsistent results ranging from very small inverse relationships to no meaningful association. No studies have examined data longitudinally, which may provide further insights into paired readmission and mortality trends for individual hospitals. This information is vital to understanding whether one of the most consequential payment changes affecting hospitals in recent years caused unintended harm to patients.
This study examined whether changes in hospital 30-day readmission rates were associated with changes in 30-day mortality rates after discharge for Medicare fee-for-service (FFS) beneficiaries hospitalized with HF, AMI, or pneumonia in 2008 through 2014. This study secondarily examined whether changes in hospital 30-day readmission rates were also associated with changes in 90-day mortality rates after discharge and 90-day mortality rates after the admission date.
Methods
Institutional review board approval, including waiver of the requirement of participant informed consent, was provided by the Yale University Human Investigation Committee.
Overview
To examine whether recent national reductions in hospital 30-day readmission rates resulted in higher 30-day mortality rates after discharge, 30-day risk-adjusted readmission rates and 30-day risk-adjusted mortality rates after discharge were calculated for each condition (HF, AMI, and pneumonia) in each month at each hospital during the study period. Monthly trends in each hospital’s 30-day risk-adjusted readmission rates and 30-day risk-adjusted mortality rates after discharge were then examined for each condition. Correlation coefficients were calculated for hospitals’ paired monthly trends in 30-day risk-adjusted readmission rates and 30-day risk-adjusted mortality rates after discharge. Outcomes were recalculated in multiple secondary analyses, including with mortality alternatively defined as 90-day risk-adjusted mortality rates after discharge and 90-day risk-adjusted mortality rates after the admission date to account for late effects of readmission reduction, predischarge practices designed to lower readmissions, and in-hospital mortality.
Study Cohorts
This study primarily examined patients hospitalized with HF, AMI, or pneumonia who survived hospitalization and were at risk for readmission and death following discharge. Medicare Standard Analytic and Denominator files were used to identify all hospitalizations at short-term acute care hospitals from January 1, 2008, through December 31, 2014, with a principal discharge diagnosis of HF, AMI, or pneumonia. Cohorts were defined with International Classification of Diseases, Ninth Revision, Clinical Modification codes identical to those used in the CMS publicly reported readmission and mortality measures (eTable 1 in the Supplement). Hospitalizations among patients aged 65 years or older were included. Hospitalizations of patients who died during the index hospital stay were excluded because these patients could not be exposed to postdischarge practices designed to lower readmissions. Hospitalizations of patients with less than 30-day postdischarge enrollment in Medicare FFS in the absence of death, discharge against medical advice, or less than 1 year of enrollment in Medicare FFS prior to hospitalization were also excluded. Transfers (contiguous hospitalizations) were linked into a single episode of care. Previous Medicare claims were used to identify the presence of comorbidities for risk adjustment.
Calculation of Readmission and Mortality Rates
For each hospital, 30-day risk-adjusted readmission rates and 30-day risk-adjusted mortality rates after discharge were calculated for each condition and each month during the study period. To do so, patient-level logistic regression models for 30-day readmission and 30-day mortality after discharge were separately fit. As with the publicly reported readmission and mortality measures, adjustment was made for patient age, sex, and comorbidities predictive of readmission and mortality. Adjustment was also made for season as has been done previously and for hospital length of stay because changes over time in length of stay can shift the proportion of early mortality events that occur after hospitalization. Models were fit with all 7 years of data (2008-2014) separately for HF, AMI, and pneumonia. Coefficients for predictor variables from these patient-level regression models were used to calculate expected outcome rates, 30-day risk-adjusted readmission rates, and 30-day risk-adjusted mortality rates after discharge for each hospital in each month using indirect standardization, defined as the observed outcome rate divided by the expected outcome rate (O/E) multiplied by the total crude outcome rate. The total crude outcome rate for each condition was based on the 7-year study period.
Readmissions could occur for any unplanned reason to any short-term acute care hospital (all-cause readmission). As with the federal readmission measures, the CMS Planned Readmission algorithm version 3.0 was used to exclude planned readmissions for procedures or diagnoses that are typically scheduled, such as maintenance chemotherapy or organ transplantation. Death could occur for any reason (all-cause mortality).
Transfers were attributed to discharging hospitals when calculating 30-day and 90-day mortality rates after discharge to create identical hospital cohorts for readmission and mortality analyses. In contrast, transfers were attributed to the initial hospital caring for patients when calculating 90-day mortality rates after the admission date. This latter approach is consistent with the methods used by CMS in its publicly reported mortality measures, all of which calculate mortality from the date of admission.
Outcomes
The primary outcomes were hospital 30-day risk-adjusted readmission rates and hospital 30-day risk-adjusted mortality rates after discharge for each study condition (HF, AMI, and pneumonia) in each month at each hospital during the study period. Secondary mortality outcomes were hospital 90-day risk-adjusted mortality rates after discharge and 90-day risk-adjusted mortality rates after the admission date.
Statistical Analysis
Differences in the characteristics of patients hospitalized with HF, AMI, or pneumonia over different study years were described using analysis of variance for continuous variables and χ2 test for categorical variables.
For each hospital, weighted linear regression and repeated monthly measures of its 30-day risk-adjusted readmission rates and 30-day risk-adjusted mortality rates after discharge were used to separately calculate monthly trends in its 30-day risk-adjusted readmission rates and 30-day risk-adjusted mortality rates after discharge for HF, AMI, and pneumonia. Weighting was based on the hospital monthly volume for each condition. For the primary analysis, trend calculations were limited to hospitals with at least 36 available monthly 30-day risk-adjusted readmission rates and 30-day risk-adjusted mortality rates after discharge in 2008 through 2014. In the model, only the time variable in months from January 1, 2008, was included, and the slope of the time variable was used to denote each hospital’s monthly percentage change in its 30-day risk-adjusted readmission rate or 30-day risk-adjusted mortality rate after discharge.
Weighted Pearson correlation coefficients of hospitals’ paired monthly trends in 30-day risk-adjusted readmission rates and 30-day risk-adjusted mortality rates after discharge were then calculated for each condition in 2008 through 2014. Weighting was based on hospital volume for each condition. In additional secondary analyses, weighted Pearson correlation coefficients of hospitals’ paired monthly trends in 30-day risk-adjusted readmission rates and 30-day risk-adjusted mortality rates after discharge were calculated for each condition from April 1, 2010, through September 30, 2012. For these analyses, data were used from hospitals with at least 12 available monthly 30-day risk-adjusted readmission rates and 30-day risk-adjusted mortality rates after discharge from April 2010 through September 2012, the period with the greatest reduction in readmissions following passage of the ACA.
In addition, weighted Pearson correlation coefficients of hospitals’ paired monthly trends in 30-day risk-adjusted readmission rates and 30-day risk-adjusted mortality rates after discharge were calculated for each condition in 2008 through 2014 across hospital tertiles with low, average, and high 30-day readmission rates from January 1, 2008, through March 31, 2010, because hospitals with higher readmission rates prior to passage of the ACA had greater readmission reductions afterward. If hospital readmission rate reductions were indeed associated with increasing mortality rates after discharge, this study hypothesized that these signals would be most apparent during periods and among hospitals with the largest readmission rate declines. Weighted Pearson correlation coefficients of hospitals’ paired monthly trends in 30-day risk-adjusted readmission rates and both 90-day risk-adjusted mortality rates after discharge and 90-day risk-adjusted mortality rates after the admission date were calculated for each condition in 2008 through 2014 to account for late effects of readmission reduction and in-hospital mortality, respectively. As in the primary analysis, trend calculations were limited to hospitals with at least 36 available monthly 30-day risk-adjusted readmission rates and 90-day risk-adjusted mortality rates in 2008 through 2014. Analyses involving 90-day risk-adjusted mortality rates after discharge used the same study cohorts as the primary analysis. In contrast, analyses involving 90-day risk-adjusted mortality rates after the admission date also included hospitalizations of patients who died during the index hospital stay.
All significance levels were 2-sided, with P < .05 indicating statistical significance. Analyses were conducted using SAS version 9.3 statistical software (SAS Institute Inc).
Results
In 2008 through 2014, 2 962 554 hospitalizations for HF, 1 229 939 for AMI, and 2 544 530 for pneumonia were identified. Flow diagrams describing study population selection for cohorts with HF, AMI, and pneumonia are presented in eFigure 1 in the Supplement. Among patients hospitalized for HF, AMI, or pneumonia, the respective mean (SD) ages were 80.8 (8.2), 78.8 (8.3), and 80.2 (8.3) years; 45.8%, 51.6%, and 46.3% were male; and the mean (SD) lengths of stay were 5.2 (4.5), 5.6 (5.3), and 5.5 (4.4) days. Following hospitalization for HF, AMI, or pneumonia, the respective crude patient-level 30-day readmission rates were 22.7%, 17.9%, and 17.3% and the respective crude patient-level mortality rates after discharge were 8.6%, 7.5%, and 8.4%. In the Table, the number of hospitalizations, mean age, proportion male, mean length of stay, proportion of admissions by season, crude patient-level 30-day readmission rate, and crude patient-level 30-day mortality rate after discharge are shown by year for patients hospitalized for HF, AMI, and pneumonia. Data on the presence of comorbidities among study cohorts is presented by year in eTable 2 in the Supplement.
Table. Characteristics and Outcomes of Medicare Fee-for-Service Beneficiaries Discharged After Hospitalization for Heart Failure, Acute Myocardial Infarction, or Pneumonia, 2008 Through 2014.
| Characteristics by Outcome | Year | Overall | ||||||
|---|---|---|---|---|---|---|---|---|
| 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | ||
| Heart Failure | ||||||||
| Hospitalizations, No. | 449 135 | 450 536 | 441 674 | 425 890 | 410 057 | 400 040 | 385 222 | 2 962 554 |
| Patient age, mean (SD), y | 80.6 (8.0) | 80.7 (8.1) | 80.8 (8.1) | 80.9 (8.2) | 80.9 (8.3) | 80.8 (8.4) | 80.9 (8.4) | 80.8 (8.2) |
| Men, % | 45.2 | 45.3 | 45.6 | 45.7 | 46.3 | 47.1 | 45.7 | 45.8 |
| Length of stay, mean (SD), d | 5.3 (4.5) | 5.2 (4.4) | 5.1 (4.4) | 5.1 (4.4) | 5.1 (4.5) | 5.2 (4.6) | 5.2 (4.5) | 5.2 (4.5) |
| Hospitalizations in quarter, % | ||||||||
| Quarter 1, January-March | 28.0 | 27.4 | 28.1 | 28.3 | 28.0 | 27.9 | 27.1 | 27.8 |
| Quarter 2, April-June | 25.0 | 25.3 | 24.9 | 25.3 | 24.5 | 25.3 | 25.2 | 25.1 |
| Quarter 3, July-September | 22.0 | 22.4 | 22.3 | 22.2 | 22.2 | 22.4 | 22.4 | 22.3 |
| Quarter 4, October-December | 25.0 | 25.0 | 24.7 | 24.2 | 25.3 | 24.5 | 25.4 | 24.9 |
| 30-d Rate, % | ||||||||
| Readmission | 23.5 | 23.5 | 23.4 | 23.0 | 22.5 | 21.6 | 21.4 | 22.7 |
| Mortality after discharge | 7.9 | 8.1 | 8.4 | 8.7 | 8.8 | 9.1 | 9.2 | 8.6 |
| Acute Myocardial Infarction | ||||||||
| Hospitalizations, No. | 189 074 | 178 495 | 176 275 | 174 314 | 176 637 | 171 526 | 163 618 | 1 229 939 |
| Patient age, mean (SD), y | 79.1 (8.1) | 79.0 (8.2) | 78.9 (8.2) | 78.8 (8.3) | 78.7 (8.3) | 78.5 (8.4) | 78.4 (8.4) | 78.8 (8.3) |
| Men, % | 50.1 | 50.7 | 51.0 | 51.7 | 52.1 | 53.3 | 52.6 | 51.6 |
| Length of stay, mean (SD), d | 6.1 (5.7) | 5.9 (5.4) | 5.7 (5.3) | 5.5 (5.1) | 5.4 (5.1) | 5.3 (5.1) | 5.2 (4.9) | 5.6 (5.3) |
| Hospitalizations in quarter, % | ||||||||
| Quarter 1, January-March | 27.4 | 26.2 | 26.2 | 26.4 | 25.7 | 27.0 | 25.7 | 26.4 |
| Quarter 2, April-June | 24.6 | 24.9 | 24.6 | 24.9 | 24.3 | 24.6 | 24.9 | 24.7 |
| Quarter 3, July-September | 22.9 | 23.4 | 23.8 | 23.7 | 23.9 | 23.4 | 23.8 | 23.6 |
| Quarter 4, October-December | 25.0 | 25.5 | 25.4 | 25.1 | 26.0 | 24.9 | 25.6 | 25.4 |
| 30-d Rate, % | ||||||||
| Readmission | 19.0 | 18.8 | 18.6 | 18.3 | 17.5 | 16.5 | 16.0 | 17.9 |
| Mortality after discharge | 7.8 | 7.7 | 7.5 | 7.7 | 7.3 | 7.2 | 7.0 | 7.5 |
| Pneumonia | ||||||||
| Hospitalizations, No. | 405 375 | 373 137 | 369 456 | 380 337 | 360 164 | 351 498 | 304 563 | 2 544 530 |
| Patient age, mean (SD), y | 80.3 (8.1) | 80.1 (8.2) | 80.2 (8.2) | 80.3 (8.3) | 80.2 (8.3) | 80.3 (8.4) | 80.2 (8.5) | 80.2 (8.3) |
| Men, % | 45.9 | 46.3 | 46.6 | 46.3 | 46.7 | 46.6 | 45.3 | 46.3 |
| Length of stay, mean (SD), d | 5.7 (4.7) | 5.6 (4.5) | 5.5 (4.3) | 5.4 (4.3) | 5.3 (4.2) | 5.4 (4.2) | 5.2 (4.0) | 5.5 (4.4) |
| Hospitalizations in quarter, % | ||||||||
| Quarter 1, January-March | 35.0 | 29.6 | 30.0 | 31.2 | 30.9 | 34.5 | 29.8 | 31.6 |
| Quarter 2, April-June | 24.1 | 25.5 | 25.0 | 25.9 | 23.9 | 24.5 | 25.3 | 24.9 |
| Quarter 3, July-September | 17.9 | 19.6 | 20.1 | 19.4 | 19.4 | 19.1 | 19.6 | 19.3 |
| Quarter 4, October-December | 23.0 | 25.3 | 24.9 | 23.6 | 25.8 | 21.9 | 25.4 | 24.2 |
| 30-d Rate, % | ||||||||
| Readmission | 17.6 | 17.9 | 17.9 | 17.6 | 17.2 | 16.5 | 16.5 | 17.3 |
| Mortality after discharge | 8.1 | 8.3 | 8.5 | 8.5 | 8.5 | 8.5 | 8.6 | 8.4 |
In 2008 through 2014, 5016 hospitals caring for Medicare FFS beneficiaries hospitalized for HF, 4772 caring for Medicare FFS beneficiaries hospitalized for AMI, and 5057 caring for Medicare FFS beneficiaries hospitalized for pneumonia were identified. Median monthly volumes of hospitalizations for HF, AMI, and pneumonia among these hospitals were 6 (interquartile range [IQR], 2-12), 4 (IQR, 1-8), and 5 (IQR, 2-10), respectively. Of the 4221, 2469, and 4483 hospitals caring for patients with HF, AMI, or pneumonia, respectively, and contributing 36 or more months of data during the study period, median monthly volumes of hospitalizations for HF, AMI, and pneumonia were 6 (IQR, 2-13), 4 (IQR, 2-9), and 5 (IQR, 3-10), respectively.
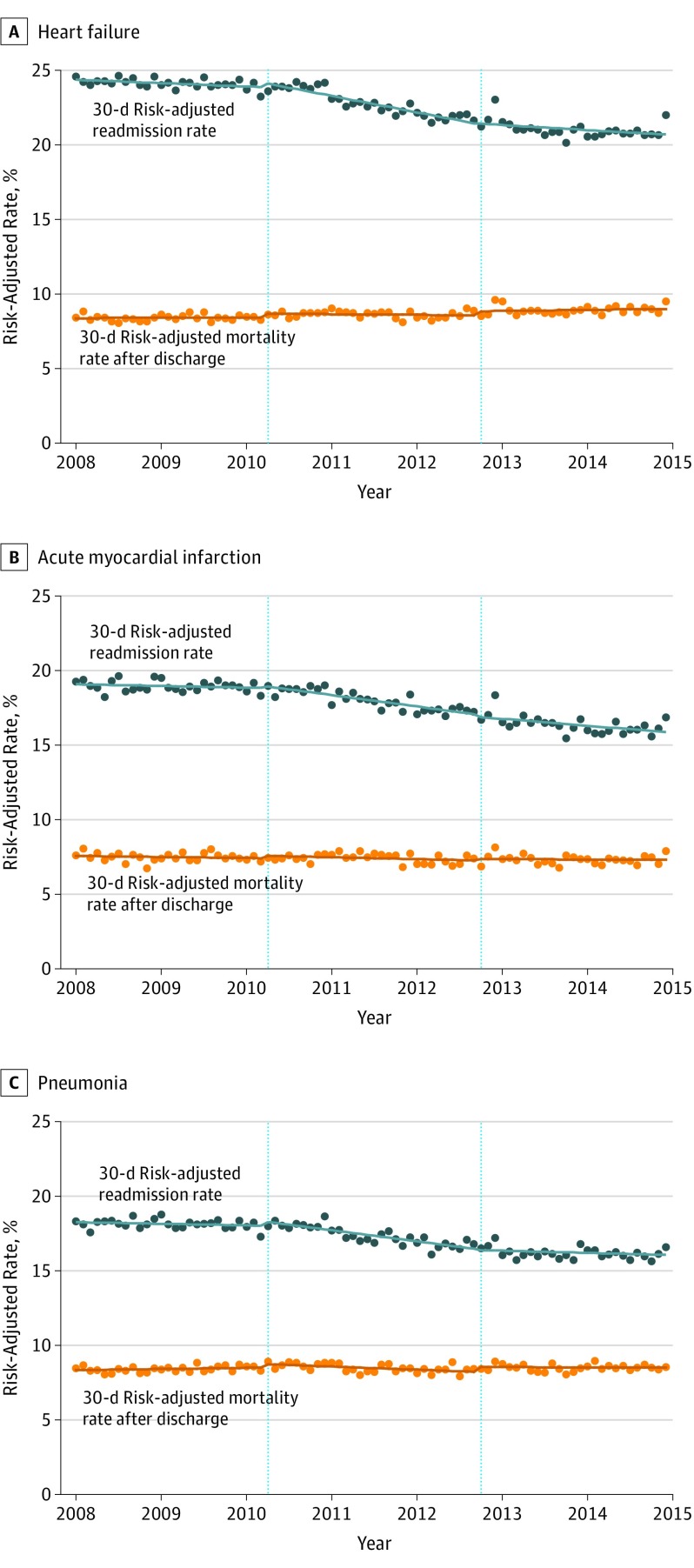
Aggregate trends in hospital 30-day risk-adjusted readmission rates and 30-day risk-adjusted mortality rates after discharge in 2008 through 2014 are presented in Figure 1. Data on hospital number and hospitalization volume by month for calculating these trends are presented in eTable 3 in the Supplement. In January 2008, mean hospital 30-day risk-adjusted readmission rates and 30-day risk-adjusted mortality rates after discharge were 24.6% and 8.4% after hospitalization for HF, 19.3% and 7.6% after hospitalization for AMI, and 18.3% and 8.5% after hospitalization for pneumonia, respectively.
Figure 1. Trends in Hospital 30-Day Risk-Adjusted Readmission Rates and Hospital 30-Day Risk-Adjusted Mortality Rates After Discharge for Heart Failure, Acute Myocardial Infarction, and Pneumonia, 2008 Through 2014.
Linear trends in mean monthly 30-day risk-adjusted readmission rates and 30-day risk-adjusted mortality rates after discharge from hospitalization for heart failure (A), acute myocardial infarction (B), and pneumonia (C) are shown for 3 periods: January 2008 through March 2010, April 2010 through September 2012, and October 2012 through December 2014. The vertical dotted lines denote April 1, 2010, and October 1, 2012, to be proximate to dates of passage of the Affordable Care Act and implementation of the Hospital Readmissions Reduction Program, respectively. Trend lines were fitted based on predictions of truncated time series models for the 3 periods above. Risk adjustment was made for patient age, sex, comorbidities, season, and hospital length of stay.
Across hospitals, 30-day risk-adjusted readmission rates declined for all 3 conditions from 2008 through 2014; monthly aggregate trends in risk-adjusted readmission rates were −0.053% (95% CI, −0.055% to −0.051%) after hospitalization for HF, −0.044% (95% CI, −0.047% to −0.041%) after hospitalization for AMI, and −0.033% (95% CI, −0.035% to −0.031%) after hospitalization for pneumonia. In contrast, monthly aggregate trends across hospitals in 30-day risk-adjusted mortality rates after discharge varied by admitting condition: HF, 0.008% (95% CI, 0.007% to 0.010%); AMI, −0.003% (95% CI, −0.005% to −0.001%); and pneumonia, 0.001% (95% CI, −0.001% to 0.003%).
Monthly reductions in risk-adjusted readmission rates across hospitals were greatest between April 2010 and September 2012 and were −0.073% (95% CI, −0.087% to −0.058%) after hospitalization for HF, −0.054% (95% CI, −0.074% to −0.034%) after hospitalization for AMI, and −0.053% (95% CI, −0.067% to −0.039%) after hospitalization for pneumonia. Monthly aggregate trends across hospitals in 30-day risk-adjusted mortality rates after discharge between April 2010 and September 2012 again varied by admitting condition: HF, −0.005% (95% CI, −0.016% to 0.005%); AMI, −0.005% (95% CI, −0.021% to 0.012%); and pneumonia, −0.024% (95% CI, −0.035% to −0.013%).
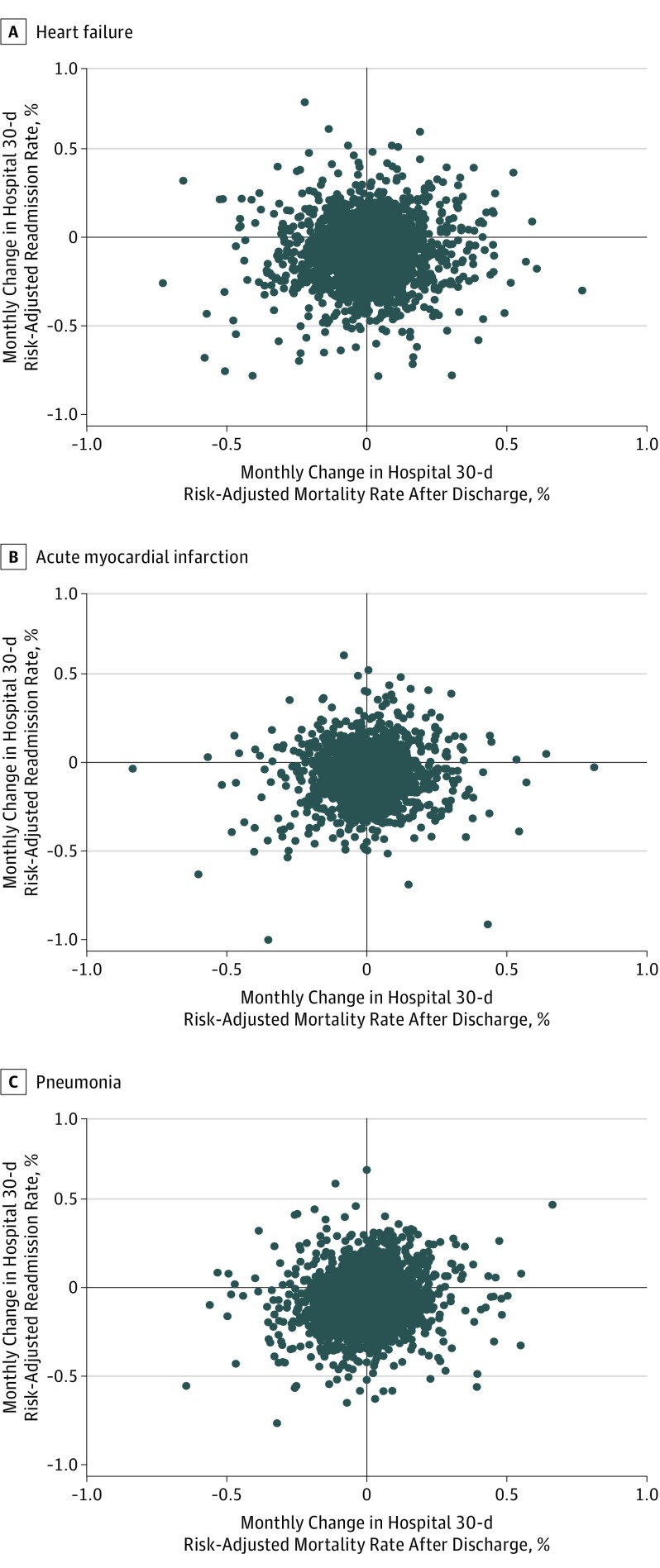
Paired trends in hospital 30-day risk-adjusted readmission rates and 30-day risk-adjusted mortality rates after discharge identified concomitant reductions in readmission and mortality rates within hospitals. Data on hospital number and hospitalization volume by month for calculating their correlations are presented in eTable 4 in the Supplement. In the primary analysis, correlation coefficients of paired monthly trends in hospital 30-day risk-adjusted readmission rates with trends in hospital 30-day risk-adjusted mortality rates after discharge for HF, AMI, and pneumonia in 2008 through 2014 were 0.066 (95% CI, 0.036 to 0.096), 0.067 (95% CI, 0.027 to 0.106), and 0.108 (95% CI, 0.079 to 0.137), respectively (Figure 2). Similarly, correlation coefficients of paired trends in hospital 30-day risk-adjusted readmission rates and 30-day risk-adjusted mortality rates after discharge for HF, AMI, and pneumonia from April 2010 through September 2012 were 0.067 (95% CI, 0.037 to 0.097), 0.080 (95% CI, 0.041 to 0.119), and 0.084 (95% CI, 0.055 to 0.113), respectively (eFigure 2 and eTable 5 in the Supplement).
Figure 2. Correlation of Paired Monthly Trends in Hospital 30-Day Risk-Adjusted Readmission Rates and Hospital 30-Day Risk-Adjusted Mortality Rates After Discharge for Heart Failure, Acute Myocardial Infarction, and Pneumonia, 2008 Through 2014.
Correlations of paired monthly trends in hospital 30-day risk-adjusted readmission rates and hospital 30-day risk-adjusted mortality rates after discharge from hospitalization for heart failure (4221 hospitals) (A), acute myocardial infarction (2469 hospitals) (B), and pneumonia (4483 hospitals) (C) from 2008 through 2014 are shown. Risk adjustment was made for patient age, sex, comorbidities, season, and hospital length of stay.
When subgroups of hospitals in different tertiles of readmission performance from January 2008 through March 2010 were examined, correlations of paired trends in hospital 30-day risk-adjusted readmission rates and 30-day risk-adjusted mortality rates after discharge were either positive or nonsignificant. Correlation coefficients for hospital tertiles with low, average, and high 30-day risk-adjusted readmission rates were 0.048 (95% CI, −0.007 to 0.103), 0.105 (95% CI, 0.056 to 0.155), and 0.038 (95% CI, −0.014 to 0.090), respectively, after hospitalization for HF; 0.057 (95% CI, −0.024 to 0.138), 0.095 (95% CI, 0.038 to 0.151), and 0.069 (95% CI, −0.003 to 0.140), respectively, after hospitalization for AMI; and 0.029 (95% CI, −0.023 to 0.081), 0.147 (95% CI, 0.099 to 0.195), and 0.071 (95% CI, 0.020 to 0.121), respectively, after hospitalization for pneumonia.
Paired trends in hospital 30-day risk-adjusted readmission rates and both 90-day risk-adjusted mortality rates after discharge and 90-day risk-adjusted mortality rates after the admission date also identified concomitant reductions in readmission and mortality rates within hospitals. Correlation coefficients of paired monthly trends in hospital 30-day risk-adjusted readmission rates with trends in hospital 90-day risk-adjusted mortality rates after discharge for HF, AMI, and pneumonia in 2008 through 2014 were 0.156 (95% CI, 0.126 to 0.185), 0.156 (95% CI, 0.118 to 0.195), and 0.186 (95% CI, 0.158 to 0.215), respectively (eFigure 3 in the Supplement). Similarly, correlation coefficients of paired trends in hospital 30-day risk-adjusted readmission rates and 90-day risk-adjusted mortality rates after the admission date for HF, AMI, and pneumonia in 2008 through 2014 were 0.163 (95% CI, 0.133 to 0.193), 0.082 (95% CI, 0.042 to 0.122), and 0.165 (95% CI, 0.135 to 0.193), respectively (eFigure 4 and eTable 6 in the Supplement).
Discussion
Among Medicare FFS beneficiaries hospitalized for HF, AMI, or pneumonia, reductions in hospital 30-day readmission rates were weakly but significantly correlated with reductions in hospital 30-day mortality rates after discharge. This finding was based on multiple longitudinal and complementary analyses of paired trends in hospital readmission and mortality rates and differs from previous work using cross-sectional data. While concerns about unintended consequences of incentivizing readmission reduction have been frequently raised, study findings strongly suggest that mortality has not increased.
Results extend previous work showing no harm and possible additional benefits from the HRRP. Researchers have expressed concern that the HRRP’s initial focus on reducing readmissions for HF, AMI, and pneumonia may worsen care for patients hospitalized for nontargeted conditions. However, studies have instead shown that readmission reductions for targeted conditions have been accompanied by lower readmission rates across the range of conditions resulting in hospitalization, albeit to a smaller degree. Researchers and policy makers have also expressed concern that penalizing hospitals caring for patients with low socioeconomic status could worsen disparities for this vulnerable group of patients. However, recent national declines in readmission rates have been greater at hospitals caring for patients with low socioeconomic status and have therefore reduced disparities in readmission across hospitals. In this context, this study has shown that hospitals with greater readmission reductions have had greater improvements in mortality. Hospitals nationally have made significant efforts to lower readmissions through improved transitional and postacute care. As these efforts have largely focused on better preparing patients and families for hospital discharge, integrating care across settings, and improving the timeliness of follow-up, they may have produced salutary effects on other outcomes besides readmission.
In contrast with declining mortality rates of previous years, hospital 30-day mortality rates after discharge changed minimally during the study period, with slight reductions for AMI and slight increases for HF. Although the reasons for changing mortality trends are not well understood, it may be that patients hospitalized with HF, AMI, and pneumonia have become more medically complex over time in ways that are not captured by risk adjustment. In support of this hypothesis, this study and others have shown reduced hospitalization rates for these conditions in recent years with concomitant increases in both comorbid conditions and illness severity among patients who are ultimately hospitalized. These changes may reflect larger trends among hospitalized older adults, as reduced admission rates, greater medical complexity, and leveling of mortality have been apparent across multiple admitting conditions not targeted by the HRRP.
Increasing postdischarge mortality rates for HF, in particular, have not been counterbalanced by mortality reductions during hospitalization; this study found that hospital 90-day risk-adjusted mortality rates after the admission date for HF also increased from 2008 through 2014 (eFigure 5 and eTable 7 in the Supplement). It is notable that readmission reductions occurred in this context and unlikely that these reductions contributed to increased deaths. Mortality rates declined to a greater extent when readmission reduction was greatest, and they began slowing prior to passage of the ACA. The results of this analysis are relatively robust to unmeasured changes over time in patient complexity, as comparative trends in readmission and mortality outcomes within hospitals were calculated with identical patient cohorts.
This analysis has a number of strengths. The study population included all hospitals continuously caring for Medicare FFS beneficiaries hospitalized for HF, AMI, or pneumonia from 2008 through 2014 and should therefore provide generalizable findings. The study years were specifically chosen to include effects of the ACA’s passage and HRRP implementation on both hospital readmission and mortality rates. The study also used multiple complementary analyses of longitudinal data and found consistent results across different periods of study, tertiles of hospital readmission performance, and definitions of hospital mortality. The approach of studying paired changes in readmission and mortality rates within individual hospitals permitted unique insights that would not have been possible from the exclusive study of aggregate trends across hospitals. For example, hospitals with larger readmission reductions for HF were more likely to have reductions in mortality rates after discharge despite the fact that aggregate trends showed decreasing hospital readmission rates and increasing postdischarge mortality rates for this condition.
This study has several limitations. It is observational in design and therefore cannot determine causality between hospitals’ efforts to lower readmissions and mortality outcomes after discharge. Nevertheless, the finding of a weak positive correlation in most cases between changes in hospital readmission and mortality rates makes it extremely unlikely that readmission reductions worsened mortality after hospitalization, as has been hypothesized. Findings also suggest that preventing deaths in patients with severe illness does not necessarily contribute to high 30-day readmission rates, as hospitals with declining mortality rates, regardless of definition, were more likely to experience concomitant reductions in readmission. Given that the study included only 3 conditions, findings may not apply to readmission reductions for conditions not targeted by the ACA. It is uncertain whether study findings would be different for younger patients who may be less vulnerable than Medicare beneficiaries to mortality after hospital discharge.
Conclusions
Among Medicare fee-for-service beneficiaries hospitalized for heart failure, acute myocardial infarction, or pneumonia, reductions in hospital 30-day readmission rates were weakly but significantly correlated with reductions in hospital 30-day mortality rates after discharge. These findings do not support increasing postdischarge mortality related to reducing hospital readmissions.
eTable 1. ICD-9-CM Codes Used to Define Heart Failure, Acute Myocardial Infarction, and Pneumonia Cohorts
eTable 2. Comorbidities Among Medicare FFS Beneficiaries Discharged After Hospitalization for Heart Failure, Acute Myocardial Infarction, or Pneumonia, 2008-2014
eTable 3. Hospital Number and Hospitalization Volume by Month for Calculating Trends in Hospital 30-Day Risk-Adjusted Readmission Rates and Hospital 30-Day Risk-Adjusted Mortality Rates After Discharge, 2008-2014
eTable 4. Hospital Number and Hospitalization Volume by Month for Calculating the Correlation of Paired Monthly Trends in Hospital 30-Day Risk-Adjusted Readmission Rates With Hospital 30-Day and 90-Day Risk-Adjusted Mortality Rates After Discharge, 2008-2014
eTable 5. Hospital Number and Hospitalization Volume by Month for Calculating the Correlation of Paired Monthly Trends in Hospital 30-Day Risk-Adjusted Readmission Rates and Hospital 30-Day Risk-Adjusted Mortality Rates After Discharge, April 2010–September 2012
eTable 6. Hospital Number and Hospitalization Volume by Month for Calculating the Correlation of Paired Monthly Trends in Hospital 30-Day Risk-Adjusted Readmission Rates and Hospital 90-Day Risk-Adjusted Mortality Rates After the Admission Date, 2008-2014
eTable 7. Hospital Number and Hospitalization Volume by Month for Calculating Trends in Hospital 30-Day Risk-Adjusted Readmission Rates and Hospital 90-Day Risk-Adjusted Mortality Rates After the Admission Date for Heart Failure, 2008-2014
eFigure 1. Flow Diagrams Describing Study Population Selection in Heart Failure, Acute Myocardial Infarction, and Pneumonia Cohorts
eFigure 2. Correlation of Paired Trends in Hospital 30-Day Risk-Adjusted Readmission Rates and Hospital 30-Day Risk-Adjusted Mortality Rates After Discharge, April 2010–September 2012
eFigure 3. Correlation of Paired Trends in Hospital 30-Day Risk-Adjusted Readmission Rates and Hospital 90-Day Risk-Adjusted Mortality Rates After Discharge, 2008-2014
eFigure 4. Correlation of Paired Trends in Hospital 30-Day Risk-Adjusted Readmission Rates and Hospital 90-Day Risk-Adjusted Mortality Rates After the Admission Date, 2008-2014
eFigure 5. Trends in Hospital 30-Day Risk-Adjusted Readmission Rates and Hospital 90-Day Risk-Adjusted Mortality Rates After the Admission Date for Heart Failure, 2008-2014
References
- 1.Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, Epstein AM. Readmissions, observation, and the Hospital Readmissions Reduction Program. N Engl J Med. 2016;374(16):1543-1551. [DOI] [PubMed] [Google Scholar]
- 2.Naylor MD, Kurtzman ET, Grabowski DC, Harrington C, McClellan M, Reinhard SC. Unintended consequences of steps to cut readmissions and reform payment may threaten care of vulnerable older adults. Health Aff (Millwood). 2012;31(7):1623-1632. [DOI] [PubMed] [Google Scholar]
- 3.Himmelstein D, Woolhandler S Quality improvement: ‘become good at cheating and you never need to become good at anything else.’ Health Affairs Blog August 27, 2015. http://healthaffairs.org/blog/2015/08/27/quality-improvement-become-good-at-cheating-and-you-never-need-to-become-good-at-anything-else/. Accessed November 12, 2016.
- 4.Carlson J. Faulty gauge? Readmissions are down, but observational-status patients are up—and that could skew Medicare numbers. Modern Healthcare June 8, 2013. http://www.modernhealthcare.com/article/20130608/magazine/306089991. Accessed November 12, 2016.
- 5.McIlvennan CK, Eapen ZJ, Allen LA. Hospital Readmissions Reduction Program. Circulation. 2015;131(20):1796-1803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gorodeski EZ, Starling RC, Blackstone EH. Are all readmissions bad readmissions? N Engl J Med. 2010;363(3):297-298. [DOI] [PubMed] [Google Scholar]
- 7.Werner RM, Bradlow ET. Public reporting on hospital process improvements is linked to better patient outcomes. Health Aff (Millwood). 2010;29(7):1319-1324. [DOI] [PubMed] [Google Scholar]
- 8.Naylor M, Brooten D, Jones R, Lavizzo-Mourey R, Mezey M, Pauly M. Comprehensive discharge planning for the hospitalized elderly: a randomized clinical trial. Ann Intern Med. 1994;120(12):999-1006. [DOI] [PubMed] [Google Scholar]
- 9.Coleman EA, Parry C, Chalmers S, Min SJ. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006;166(17):1822-1828. [DOI] [PubMed] [Google Scholar]
- 10.Brewster AL, Cherlin EJ, Ndumele CD, et al. . What works in readmissions reduction: how hospitals improve performance. Med Care. 2016;54(6):600-607. [DOI] [PubMed] [Google Scholar]
- 11.Hernandez AF, Greiner MA, Fonarow GC, et al. . Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA. 2010;303(17):1716-1722. [DOI] [PubMed] [Google Scholar]
- 12.Ouslander JG, Bonner A, Herndon L, Shutes J. The Interventions to Reduce Acute Care Transfers (INTERACT) quality improvement program: an overview for medical directors and primary care clinicians in long term care. J Am Med Dir Assoc. 2014;15(3):162-170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brotman DJ, Hoyer EH, Leung C, Lepley D, Deutschendorf A. Associations between hospital-wide readmission rates and mortality measures at the hospital level: are hospital-wide readmissions a measure of quality? J Hosp Med. 2016;11(9):650-651. [DOI] [PubMed] [Google Scholar]
- 14.Krumholz HM, Lin Z, Keenan PS, et al. . Relationship between hospital readmission and mortality rates for patients hospitalized with acute myocardial infarction, heart failure, or pneumonia. JAMA. 2013;309(6):587-593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Joynt KE, Figueroa JE, Oray J, Jha AK. Opinions on the Hospital Readmission Reduction Program: results of a national survey of hospital leaders. Am J Manag Care. 2016;22(8):e287-e294. [PMC free article] [PubMed] [Google Scholar]
- 16.Keenan PS, Normand SL, Lin Z, et al. . An administrative claims measure suitable for profiling hospital performance on the basis of 30-day all-cause readmission rates among patients with heart failure. Circ Cardiovasc Qual Outcomes. 2008;1(1):29-37. [DOI] [PubMed] [Google Scholar]
- 17.Krumholz HM, Lin Z, Drye EE, et al. . An administrative claims measure suitable for profiling hospital performance based on 30-day all-cause readmission rates among patients with acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2011;4(2):243-252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lindenauer PK, Normand SL, Drye EE, et al. . Development, validation, and results of a measure of 30-day readmission following hospitalization for pneumonia. J Hosp Med. 2011;6(3):142-150. [DOI] [PubMed] [Google Scholar]
- 19.Krumholz HM, Wang Y, Mattera JA, et al. . An administrative claims model suitable for profiling hospital performance based on 30-day mortality rates among patients with an acute myocardial infarction. Circulation. 2006;113(13):1683-1692. [DOI] [PubMed] [Google Scholar]
- 20.Krumholz HM, Wang Y, Mattera JA, et al. . An administrative claims model suitable for profiling hospital performance based on 30-day mortality rates among patients with heart failure. Circulation. 2006;113(13):1693-1701. [DOI] [PubMed] [Google Scholar]
- 21.American Hospital Association Average length of stay in community hospitals, 1994-2014. http://www.aha.org/research/reports/tw/chartbook/2016/chart3-5.pdf. Accessed February 12, 2017.
- 22.Drye EE, Normand SL, Wang Y, et al. . Comparison of hospital risk-standardized mortality rates calculated by using in-hospital and 30-day models: an observational study with implications for hospital profiling. Ann Intern Med. 2012;156(1, pt 1):19-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Horwitz LI, Grady JN, Cohen DB, et al. . Development and validation of an algorithm to identify planned readmissions from claims data. J Hosp Med. 2015;10(10):670-677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Desai NR, Ross JS, Kwon JY, et al. . Association between hospital penalty status under the Hospital Readmission Reduction Program and readmission rates for target and nontarget conditions. JAMA. 2016;316(24):2647-2656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bhalla R, Kalkut G. Could Medicare readmission policy exacerbate health care system inequity? Ann Intern Med. 2010;152(2):114-117. [DOI] [PubMed] [Google Scholar]
- 26.Joynt KE, Jha AK. Characteristics of hospitals receiving penalties under the Hospital Readmissions Reduction Program. JAMA. 2013;309(4):342-343. [DOI] [PubMed] [Google Scholar]
- 27.Joynt KE, Jha AK. A path forward on Medicare readmissions. N Engl J Med. 2013;368(13):1175-1177. [DOI] [PubMed] [Google Scholar]
- 28.Gu Q, Koenig L, Faerberg J, Steinberg CR, Vaz C, Wheatley MP. The Medicare Hospital Readmissions Reduction Program: potential unintended consequences for hospitals serving vulnerable populations. Health Serv Res. 2014;49(3):818-837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carey K, Lin MY. Hospital Readmissions Reduction Program: safety-net hospitals show improvement, modifications to penalty formula still needed. Health Aff (Millwood). 2016;35(10):1918-1923. [DOI] [PubMed] [Google Scholar]
- 30.Kociol RD, Peterson ED, Hammill BG, et al. . National survey of hospital strategies to reduce heart failure readmissions: findings from the Get With the Guidelines-Heart Failure registry. Circ Heart Fail. 2012;5(6):680-687. [DOI] [PubMed] [Google Scholar]
- 31.Bradley EH, Curry L, Horwitz LI, et al. . Hospital strategies associated with 30-day readmission rates for patients with heart failure. Circ Cardiovasc Qual Outcomes. 2013;6(4):444-450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bradley EH, Sipsma H, Horwitz LI, et al. . Hospital strategy uptake and reductions in unplanned readmission rates for patients with heart failure: a prospective study. J Gen Intern Med. 2015;30(5):605-611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Joynt KE, Orav EJ, Zheng J, Jha AK. Public reporting of mortality rates for hospitalized Medicare patients and trends in mortality for reported conditions. Ann Intern Med. 2016;165(3):153-160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chen J, Normand SL, Wang Y, Krumholz HM. National and regional trends in heart failure hospitalization and mortality rates for Medicare beneficiaries, 1998-2008. JAMA. 2011;306(15):1669-1678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chen J, Dharmarajan K, Wang Y, Krumholz HM. National trends in heart failure hospital stay rates, 2001 to 2009. J Am Coll Cardiol. 2013;61(10):1078-1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010;362(23):2155-2165. [DOI] [PubMed] [Google Scholar]
- 37.Sacks NC, Ash AS, Ghosh K, et al. . Recent national trends in acute myocardial infarction hospitalizations in Medicare: shrinking declines and growing disparities. Epidemiology. 2015;26(4):e46-e47. [DOI] [PubMed] [Google Scholar]
- 38.Nallamothu BK, Normand SL, Wang Y, et al. . Relation between door-to-balloon times and mortality after primary percutaneous coronary intervention over time: a retrospective study. Lancet. 2015;385(9973):1114-1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Krumholz HM, Nuti SV, Downing NS, Normand SL, Wang Y. Mortality, hospitalizations, and expenditures for the Medicare population aged 65 years or older, 1999-2013. JAMA. 2015;314(4):355-365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Figueroa JF, Tsugawa Y, Zheng J, Orav EJ, Jha AK. Association between the Value-Based Purchasing pay for performance program and patient mortality in US hospitals: observational study. BMJ. 2016;353:i2214. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. ICD-9-CM Codes Used to Define Heart Failure, Acute Myocardial Infarction, and Pneumonia Cohorts
eTable 2. Comorbidities Among Medicare FFS Beneficiaries Discharged After Hospitalization for Heart Failure, Acute Myocardial Infarction, or Pneumonia, 2008-2014
eTable 3. Hospital Number and Hospitalization Volume by Month for Calculating Trends in Hospital 30-Day Risk-Adjusted Readmission Rates and Hospital 30-Day Risk-Adjusted Mortality Rates After Discharge, 2008-2014
eTable 4. Hospital Number and Hospitalization Volume by Month for Calculating the Correlation of Paired Monthly Trends in Hospital 30-Day Risk-Adjusted Readmission Rates With Hospital 30-Day and 90-Day Risk-Adjusted Mortality Rates After Discharge, 2008-2014
eTable 5. Hospital Number and Hospitalization Volume by Month for Calculating the Correlation of Paired Monthly Trends in Hospital 30-Day Risk-Adjusted Readmission Rates and Hospital 30-Day Risk-Adjusted Mortality Rates After Discharge, April 2010–September 2012
eTable 6. Hospital Number and Hospitalization Volume by Month for Calculating the Correlation of Paired Monthly Trends in Hospital 30-Day Risk-Adjusted Readmission Rates and Hospital 90-Day Risk-Adjusted Mortality Rates After the Admission Date, 2008-2014
eTable 7. Hospital Number and Hospitalization Volume by Month for Calculating Trends in Hospital 30-Day Risk-Adjusted Readmission Rates and Hospital 90-Day Risk-Adjusted Mortality Rates After the Admission Date for Heart Failure, 2008-2014
eFigure 1. Flow Diagrams Describing Study Population Selection in Heart Failure, Acute Myocardial Infarction, and Pneumonia Cohorts
eFigure 2. Correlation of Paired Trends in Hospital 30-Day Risk-Adjusted Readmission Rates and Hospital 30-Day Risk-Adjusted Mortality Rates After Discharge, April 2010–September 2012
eFigure 3. Correlation of Paired Trends in Hospital 30-Day Risk-Adjusted Readmission Rates and Hospital 90-Day Risk-Adjusted Mortality Rates After Discharge, 2008-2014
eFigure 4. Correlation of Paired Trends in Hospital 30-Day Risk-Adjusted Readmission Rates and Hospital 90-Day Risk-Adjusted Mortality Rates After the Admission Date, 2008-2014
eFigure 5. Trends in Hospital 30-Day Risk-Adjusted Readmission Rates and Hospital 90-Day Risk-Adjusted Mortality Rates After the Admission Date for Heart Failure, 2008-2014