Key Points
Question
Can low-dose naltrexone be used to successfully treat Hailey-Hailey disease?
Findings
In this case series of 3 patients with severe Hailey-Hailey disease recalcitrant to multiple therapies, treatment with low-dose naltrexone at 3 mg and, in 2 of the patients, titrated to 4.5 mg nightly, was attempted and resulted in clinical resolution within 2 months. Lesions flared when stopping low-dose naltrexone and cleared within a few days on rechallenge.
Meaning
The success of these cases of Hailey-Hailey disease treated with low-dose naltrexone along with the medication’s low adverse effect profile suggest low-dose naltrexone as a novel therapy for Hailey-Hailey disease.
Abstract
Importance
Hailey-Hailey disease is a severe genetic blistering disease of intertriginous skin locations that can lead to poor quality of life and increased morbidities. Multiple therapies are available with inconsistent outcomes and potentially severe adverse effects.
Objective
To determine whether low-dose naltrexone is an effective treatment for Hailey-Hailey disease.
Design, Setting, and Participants
This study was a case series performed at a dermatology outpatient clinic of 3 patients with severe Hailey-Hailey disease recalcitrant to at least 4 therapies.
Interventions
Low-dose naltrexone, 3 mg nightly, titrated to 4.5 mg nightly in 2 patients.
Main Outcomes and Measures
Reduction in size of lesions as well as subjective improvement of symptoms.
Results
All 3 patients noted significant healing of erosions and plaques starting from the peripheral aspect within 1 to 2 weeks of treatment, and clinical resolution of lesions within 2 months. Discontinuation of low-dose naltrexone resulted in flaring of symptoms, which cleared within 2 to 3 days on rechallenge with low-dose naltrexone.
Conclusions and Relevance
We present herein 3 cases of patients with severe Hailey-Hailey disease treated with low-dose naltrexone who achieved clinical resolution of symptoms. The success of these cases suggests low-dose naltrexone as a novel therapy for Hailey-Hailey disease. The possible mechanism may involve low-dose naltrexone influencing opioid or toll-like receptor signaling to improve calcium mobilization and improve keratinocyte differentiation and wound healing. Future studies are needed to clarify the mechanism and to define the role of low-dose naltrexone for treatment of Hailey-Hailey disease.
This case series investigates whether low-dose naltrexone is an effective treatment for recalcitrant Hailey-Hailey disease.
Introduction
Hailey-Hailey disease (HHD) is a severe genetic blistering disease of intertriginous skin. Patients can experience poor quality of life with chronic painful erosions, especially during periods of increased heat or stress, resulting in secondary infections and scarring. A myriad of treatments have been attempted, including various topical antibiotics, systemic and intralesional corticosteroids, botulinum toxin type A, laser therapies, and systemic immunosuppression, with inconsistent outcomes and potentially severe adverse effects.1 Low-dose naltrexone has been widely touted in social media platforms, including multiple YouTube videos, as an anecdotal treatment for patients with HHD with surprisingly no published evidence until this year with 1 recent theoretical article.2
Herein, we present 3 patients with HHD with severe disease recalcitrant to at least 4 therapies, including a recently published regimen of magnesium3 and vitamins K and D3, who were treated with low-dose naltrexone, resulting in complete clinical resolution of symptoms.
Report of Cases
Patient 1, a man in his 50s, presented with a 15-year history of recurrent vesicles and severe erosions of the axillae previously confirmed as HHD by biopsy. Results from indirect immunofluorescence and enzyme-linked immunosorbent assay (ELISA) were negative. Various treatments had failed, including topical, intralesional, and intramuscular steroids, and oral and topical antibiotics. His sores persisted with triggers including minor trauma, sweat, heat, and excessive sugar in his diet. Low-dose naltrexone was initiated at 3 mg nightly, and other medications were discontinued. Low-dose naltrexone capsules were compounded by a local pharmacy. Erosions began to heal from the peripheral aspect after 1 to 2 weeks of treatment. After a 6-week trial, hyperpigmented patches in bilateral axillae and 2 small plaques in the left axilla remained. The dosage of the low-dose naltrexone was then increased to 4.5 mg nightly, with complete clearing of erosions within several days despite the patient’s poor adherence to a low-carbohydrate diet. Three months later, he discontinued the low-dose naltrexone and within 2 to 3 days developed two 2-cm adjoining crusted erosions within the right axilla. After restarting the low-dose naltrexone at 4.5 mg, the erosions cleared within 1 week. The patient remained clear for 7 more months and then ran out of medication for 2 weeks. He began to develop small new erosions in both axillae, which healed after restarting his low-dose naltrexone.
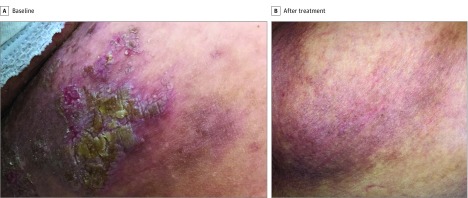
Patient 2, a woman in her 60s, presented with a family history significant for HHD and a personal 27-year history of vesicles and erosions initially involving bilateral axillae and then the arms and groin and below the breasts, with constant symptoms throughout the past 6 years regardless of season. She had attempted topical, intralesional, and systemic steroids with temporary subjective improvement of symptoms and reduced size of lesions, and oral and topical antibiotics with only limited improvement. Treatment with oral magnesium3 and vitamins K and D3 resulted in some improvement. The baseline physical examination revealed eroded plaques over the right anterior side of the neck, left axilla, beneath the left breast, and in the groin bilaterally (Figure, A). Results from indirect immunofluorescence and ELISA were negative. She began treatment with low-dose naltrexone, 3 mg nightly, and discontinued other treatments. Erosions began to heal from the peripheral aspect within 1 to 2 weeks. One month after initiating treatment her lesions had significantly improved, although recent stress was associated with a mild flare in the left side of the groin. The dosage of low-dose naltrexone was increased to 4.5 mg nightly. Her skin continued to improve, and she restarted her vitamins owing to continued pain. At the 2-month follow-up, her lesions had nearly healed, with only a 1-cm plaque remaining in the left side of the groin and residual hyperpigmentation, and at 4 months her lesions completely resolved (Figure, B). The patient was able to wear pants for the first time in 6 years. Discontinuing low-dose naltrexone resulted in a flare within 4 days, which resolved within a week of restarting therapy.
Figure. Clinical Images of Resolution of Hailey-Hailey Lesions Following Treatment With Low-Dose Naltrexone, Patient 2.
A, Left side of the groin at baseline. B, Complete resolution of lesions 4 months after initiating treatment with low-dose naltrexone.
Patient 3, a woman in her 60s, presented with a clinically significant family history of HHD and a 40-year history of pruritic and painful vesicles initially over the neck and axillae, which spread to the chest, genitals, and groin, previously confirmed as HHD by biopsy. Direct immunofluorescence was negative for autoimmune blistering diseases. She had attempted topical and systemic corticosteroids, hydroxychloroquine, acitretin, and dapsone, with only partial, temporary improvement in the symptoms and size of the lesions; development of anemia limited her use of dapsone. A baseline physical examination revealed multiple large eroded plaques beneath the right breast and in the groin bilaterally extending onto the thighs. Treatment with low-dose naltrexone, 3 mg nightly, was initiated while other medications were discontinued, and lesions began to heal from the peripheral aspect within 2 to 3 days. Pruritus initially increased for 1 week, followed by improvement of both pruritus and pain. She noted 1 episode of intense dreams, a known adverse effect of low-dose naltrexone, which subsequently resolved. One month after initiating treatment, a 1-cm eroded plaque remained in the right medial aspect of the groin, with violaceous hyperpigmentation remaining where other plaques had healed within the groin and on the right breast. Two months later her skin was completely clear. She discontinued the low-dose naltrexone, and 2 new erosions appeared in the left side of the groin within 12 days. Her erosions healed within 1 week of restarting low-dose naltrexone.
Discussion
Hailey-Hailey disease is a genetic blistering disease caused by a mutation of the ATP2 C1 gene on chromosome 3 encoding a calcium transporter protein in the Golgi apparatus.4 Defective calcium transport results in abnormal adhesion of keratinocytes and subsequent acantholysis, likely triggered by shear stress of the epidermis. Opioid receptors are expressed in keratinocytes and modulate many processes, including wound healing.5 It is possible that naltrexone, which predominantly inhibits μ-opioid receptors, may modulate these receptors in the basal layer of the epidermis, resulting in increased cellular adhesion and healing of the skin. Naltrexone is also a known toll-like receptor 4 antagonist, and downstream signaling pathways have been implicated in calcium homeostasis in keratinocytes.6 Increased availability of calcium would allow for proper differentiation of keratinocytes and wound healing. It is possible that the magnesium within patient 2’s vitamin regimen had a synergistic effect with the low-dose naltrexone to increase calcium mobilization, improving response of her severe disease.3
Low-dose naltrexone has been used in multiple diseases, including several randomized placebo-controlled trials in Crohn disease, and its safety has been established.7 Patients may experience minor adverse effects, including headache, gastrointestinal tract symptoms, and vivid dreams.7 To screen for unexpected adverse effects, findings from a complete blood cell count and metabolic panel were checked at baseline and at the 1-month follow-up in all 3 patients, with no changes noted. Low-dose naltrexone is compounded because there is no commercial formulation of naltrexone at low dosage.8 As an off-label medication, there are no long-term safety data. Naltrexone acts as an opioid antagonist and may precipitate withdrawal in patients dependent on opioids.8
The rapid and significant improvement of symptoms in these patients along with the medication’s low adverse effect profile and reasonable cost suggest low-dose naltrexone as a novel treatment for HHD. Larger studies are needed to verify these preliminary findings and to further explore the mechanism in HHD, as well as the potential efficacy of low-dose naltrexone in other defective calcium transport diseases, such as Darier disease.
Conclusions
These 3 cases demonstrate the effectiveness of low-dose naltrexone in treatment of HHD with initial healing of lesions within 2 weeks of starting treatment, and complete resolution of severe disease within 2 months. Additional research is needed to evaluate the mechanism of low-dose naltrexone in HHD, as well as its potential use in treating other inflammatory and calcium transport diseases.
References
- 1.Arora H, Bray FN, Cervantes J, Falto Aizpurua LA. Management of familial benign chronic pemphigus. Clin Cosmet Investig Dermatol. 2016;9:281-290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Izquierdo D, Renvoise B, LaPoint K, Gouw AM, Lin JCH, Babar I. Could low-dose naltrexone be an effective treatment for Hailey-Hailey disease? Mol Med Lett. 2016;1(1):5-9. [Google Scholar]
- 3.Borghi A, Rimessi A, Minghetti S, Corazza M, Pinton P, Virgili A. Efficacy of magnesium chloride in the treatment of Hailey-Hailey disease: from serendipity to evidence of its effect on intracellular Ca(2+) homeostasis. Int J Dermatol. 2015;54(5):543-548. [DOI] [PubMed] [Google Scholar]
- 4.Hu Z, Bonifas JM, Beech J, et al. Mutations in ATP2C1, encoding a calcium pump, cause Hailey-Hailey disease. Nat Genet. 2000;24(1):61-65. [DOI] [PubMed] [Google Scholar]
- 5.Bigliardi PL, Neumann C, Teo YL, Pant A, Bigliardi-Qi M. Activation of the δ-opioid receptor promotes cutaneous wound healing by affecting keratinocyte intercellular adhesion and migration. Br J Pharmacol. 2015;172(2):501-514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Song PI, Park YM, Abraham T, et al. Human keratinocytes express functional CD14 and toll-like receptor 4. J Invest Dermatol. 2002;119(2):424-432. [DOI] [PubMed] [Google Scholar]
- 7.Segal D, Macdonald JK, Chande N. Low dose naltrexone for induction of remission in Crohn’s disease. Cochrane Database Syst Rev. 2014;(2):CD010410. [DOI] [PubMed] [Google Scholar]
- 8.Younger J, Parkitny L, McLain D. The use of low-dose naltrexone (LDN) as a novel anti-inflammatory treatment for chronic pain. Clin Rheumatol. 2014;33(4):451-459. [DOI] [PMC free article] [PubMed] [Google Scholar]