Key Points
Question
Are genetically elevated serum calcium levels associated with an increased risk of coronary artery disease or myocardial infarction?
Findings
In this mendelian randomization study including 60 801 cases of coronary artery disease and 123 504 noncases, genetically elevated serum calcium levels were associated with increased odds of coronary artery disease and myocardial infarction (odds ratio per 0.5-mg/dL increase in genetically predicted serum calcium levels, 1.25 and 1.24, respectively).
Meaning
A genetic predisposition to higher serum calcium levels was associated with increased risk of coronary artery disease and myocardial infarction.
Abstract
Importance
Serum calcium has been associated with cardiovascular disease in observational studies and evidence from randomized clinical trials indicates that calcium supplementation, which raises serum calcium levels, may increase the risk of cardiovascular events, particularly myocardial infarction.
Objective
To evaluate the potential causal association between genetic variants related to elevated serum calcium levels and risk of coronary artery disease (CAD) and myocardial infarction using mendelian randomization.
Design, Setting, and Participants
The analyses were performed using summary statistics obtained for single-nucleotide polymorphisms (SNPs) identified from a genome-wide association meta-analysis of serum calcium levels (N = up to 61 079 individuals) and from the Coronary Artery Disease Genome-wide Replication and Meta-analysis Plus the Coronary Artery Disease Genetics (CardiogramplusC4D) consortium’s 1000 genomes-based genome-wide association meta-analysis (N = up to 184 305 individuals) that included cases (individuals with CAD and myocardial infarction) and noncases, with baseline data collected from 1948 and populations derived from across the globe. The association of each SNP with CAD and myocardial infarction was weighted by its association with serum calcium, and estimates were combined using an inverse-variance weighted meta-analysis.
Exposures
Genetic risk score based on genetic variants related to elevated serum calcium levels.
Main Outcomes and Measures
Co-primary outcomes were the odds of CAD and myocardial infarction.
Results
Among the mendelian randomized analytic sample of 184 305 individuals (60 801 CAD cases [approximately 70% with myocardial infarction] and 123 504 noncases), the 6 SNPs related to serum calcium levels and without pleiotropic associations with potential confounders were estimated to explain about 0.8% of the variation in serum calcium levels. In the inverse-variance weighted meta-analysis (combining the estimates of the 6 SNPs), the odds ratios per 0.5-mg/dL increase (about 1 SD) in genetically predicted serum calcium levels were 1.25 (95% CI, 1.08-1.45; P = .003) for CAD and 1.24 (95% CI, 1.05-1.46; P = .009) for myocardial infarction.
Conclusions and Relevance
A genetic predisposition to higher serum calcium levels was associated with increased risk of CAD and myocardial infarction. Whether the risk of CAD associated with lifelong genetic exposure to increased serum calcium levels can be translated to a risk associated with short-term to medium-term calcium supplementation is unknown.
This analysis evaluates the potential causal association between genetic variants related to elevated serum calcium levels and risk of coronary artery disease and myocardial infarction using mendelian randomization.
Introduction
Calcium has a vital role in many biological processes in the body such as nerve transmission, blood clotting, blood pressure regulation, enzyme activation, hormone regulation, and muscle contraction. Observational studies have suggested that serum calcium levels are positively associated with risk of cardiovascular disease, including myocardial infarction. Moreover, evidence from randomized clinical trials indicates that calcium supplementation, which results in an acute and sustained elevation in serum calcium, may modestly increase the risk of cardiovascular events, particularly myocardial infarction.
However, it remains unclear whether lifelong elevated serum calcium may be causally associated with coronary artery disease (CAD) risk. Nationally representative data show that one-fifth of US adults use calcium supplements, and the proportion is even higher among middle-aged and older women and individuals with disabilities, with more than half of this group being regular calcium supplement users. Because of the widespread use of calcium supplements, any association between raised serum calcium and CAD risk by a high calcium intake could have clinical and public health implications. The findings of an elevated risk of cardiovascular events with calcium supplement use have been debated in recent years without consensus being reached.
Genetic variants that have a specific influence on possible risk factors can be used to assess associations with explicit outcomes. This method, known as mendelian randomization, avoids some of the limitations of observational studies (because genetic information should be free from confounding) and is not affected by disease status, thereby avoiding reverse causation bias. Hence, genetic variants that influence serum calcium levels could serve as instrumental variables (proxies) to determine the association of lifelong elevated serum calcium with CAD risk. We conducted a mendelian randomization study to investigate the association of serum calcium with CAD and myocardial infarction.
Methods
Study Design and Data Sources
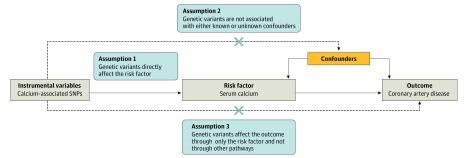
The mendelian randomization approach builds upon 3 principal assumptions (Figure 1). First, the genetic variants utilized as instrumental variables should be associated with the risk factor. Second, the genetic variants should not be associated with confounders. Third, the genetic variants should affect the risk of the outcome through the risk factor, not via other pathways.
Figure 1. Schematic Diagram of the Mendelian Randomization Assumptions Underpinning a Mendelian Randomization Analysis of the Association Between Serum Calcium Levels and Coronary Artery Disease.
SNPs indicate single-nucleotide polymorphisms. The dashed lines represent potential causal associations between variables that would represent violations of the mendelian randomization assumptions. For a formal treatment of the assumptions, see Greenland.
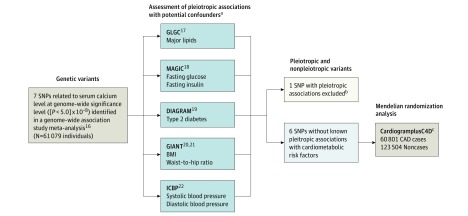
This study involved analysis of publicly available, deidentified data; specific ethical review and informed consent had been obtained in all of the original studies. This mendelian randomization study was designed to use summary statistics from large-scale genome-wide association studies (GWAS) (Figure 2). GWAS identified 7 single-nucleotide polymorphisms (SNPs) associated with serum calcium levels in a meta-analysis of 39 400 individuals of European ancestry and which were replicated in up to 21 679 additional individuals (up to 61 079 individuals). These 7 SNPs were associated with serum calcium levels at genome-wide significance level ([P < 5.0] × 10−8) in the meta-analysis of the discovery and replication cohorts. All the SNPs were in different gene regions and were distributed independently, not in linkage disequilibrium.
Figure 2. Data Sources and Analysis Plan Using Mendelian Randomization.
BMI indicates body mass index; DIAGRAM, Diabetes Genetics Replication and Meta-analysis; GIANT, Genetic Investigation of Anthropometric Traits; GLGC, Global Lipids Genetics Consortium; ICBP, International Consortium of Blood Pressure; MAGIC, Meta-Analyses of Glucose and Insulin-related traits Consortium; SNPs, single-nucleotide polymorphisms.
aFor sample sizes of each study, see Methods.
bAny SNP with pleiotropic effects (ie, associated with more than 1 risk factor) violates the Mendelian randomization assumptions. One SNP (rs780094 in the GCKR gene region) had pleiotropic associations with cardiometabolic risk factors and was excluded, leaving 6 calcium-related SNPs for inclusion in the mendelian randomization analyses.
cThe estimates for the association of each SNP with coronary artery disease were combined using the inverse-variance weighted method, with summary statistics for coronary artery disease obtained from the CardiogramplusC4D consortium.
Among the GWAS, each calcium-associated SNP was evaluated for pleiotropic associations with potential confounders, including major lipids in up to 188 577 individuals (Global Lipids Genetics Consortium); glycemic traits in up to 46 186 individuals without diabetes (Meta-Analyses of Glucose and Insulin-Related Traits Consortium); type 2 diabetes in up to 110 452 individuals (Diabetics Genetics Replication and Meta-analysis); body mass index (BMI) in up to 339 224 individuals and waist-to-hip ratio adjusted for BMI in up to 224 459 individuals (Genetic Investigation of Anthropometric Traits); and systolic and diastolic blood pressure in up to 69 395 individuals (International Consortium for Blood Pressure) (Figure 2). Of the 7 SNPs associated with serum calcium, 1 variant (rs780094 in the GCKR gene region) had pleiotropic associations at the Bonferroni-corrected significance threshold ([P < .05]/7 SNPs = .007) with lipids, glycemic traits, type 2 diabetes, and measures of adiposity (eTable in the Supplement). To avoid violations of the mendelian randomization assumptions (Figure 1), the pleiotropic SNP was omitted. Thus, 6 SNPs associated with serum calcium were used as instrumental variables in the mendelian randomization analyses.
Summary statistics for the associations of the 6 remaining calcium-associated SNPs with the prespecified primary outcomes of CAD and myocardial infarction were extracted from the Coronary Artery Disease Genome-Wide Replication and Meta-analysis plus the Coronary Artery Disease Genetics (CardiogramplusC4D) consortium’s 1000 genomes-based genome-wide association meta-analysis of 48 studies. Case status was determined using a broad definition of CAD, including myocardial infarction (approximately 70% of the total number of cases), acute coronary syndrome, chronic stable angina, or coronary artery stenosis greater than 50% (Table 1).
Table 1. Descriptive Information of the 48 Studies Included in the CardiogramplusC4D Consortium’s 1000 Genomes-Based Genome-Wide Association Meta-analysis.
| Source | Design (Years of Baseline Collection) | Country (Ancestry) | Cases | Noncases | Case Definition | |||
|---|---|---|---|---|---|---|---|---|
| No. of Individuals With CAD (% Women)a | Individuals With MI, % | Age, Mean (SD), y | No. of Individuals (% Women)a | Age, Mean (SD) | ||||
| Atherosclerotic Disease, Vascular Function, and Genetic Epidemiology Study | Cohort (2001-2003) | United States (white European) | 278 (58) | 50 | 46 (6) | 312 (59) | 45 (6) | MI, angina with ≥1 angiographic stenosis of >50%, or revascularization procedure (in men aged 18 to 45 y or women aged 18 to 55 y at the time of the event), incident stable exertional angina at an older age, and incident nonfatal MI at an older age |
| Age, Gene/Environment Susceptibility—Reykjavik Study | Cohort (2002-2006) | Iceland (white European) | 397 (NA) | 80 | NA | 2474 (58)b | 76 (5)b | MI, validated by death certificates, hospital records, and autopsy records |
| Atherosclerosis Risk in Communities Study | Cohort (1987-1989) | United States (white European) | 454 (19) | 82 | 57 (5) | 8443 (45) | 54 (6) | NA |
| Beijing Hospital Atherosclerosis Study | Case-control (NA) | China (Chinese) | 505 (15) | 100 | 57 (9) | 1021 (26) | 48 (8) | Confirmed MI |
| Cardiogenics Study | Case-control (NA) | Germany, United Kingdom (white European) | 392 (14) | 13 | 57 (9) | 410 (61) | 54 (7) | Confirmed MI and acute coronary syndrome with stenosis >50% in ≥1 major coronary artery |
| GeneBank at the Cleveland Clinic | Cohort (2001-2006) | United States (white European) | 1628 (22) | 60 | NA | 368 (45) | 64 (11)b | MI, coronary artery bypass graft, percutaneous intervention, or ≥50% stenosis in ≥1 epicardial vessel |
| China Atherosclerosis Study | Case-control (NA) | China (Chinese) | 1010 (16) | 56 | 51 (8) | 3998 (53) | 53 (8) | MI or >70% stenosis in ≥1 major epicardial vessel or >50% stenosis in the left main coronary artery |
| Corogene Study | Cohort (2006-2008) | Finland (white European) | 2083 (NA) | 90 | 66 (12) | 2048 (36)b | 57 (11) | MI and CAD (not specified) |
| Catheterization Genetics Study | Cohort (2001-2010) | United States (white European) | 1216 (31) | 48 | 58 (10) | 653 (59) | 63 (9) | ≥1 epicardial coronary vessel with ≥50% stenosis |
| Estonian Genome Center, University of Tartu | Cohort (2000-2013) | Estonia (white European) | 658 (50) | 20 | NA | 5841 (51) | NA | CAD (ICD-10 codes I20-I25), including MI (ICD-10 codes I21 and I22) |
| Family Heart Study | Cohort (1992) | United States (white European) | 334 (NA) | 9 | NA | 3446 (54)b | 51 (14)b | MI, coronary bypass, or coronary angioplasty, balloon angioplasty, atherectomy, stent, percutaneous transluminal coronary angioplasty, or percutaneous coronary intervention |
| Functional Genomic Diagnostic Tools for Coronary Artery Disease | Case-control (2007-2009) | Lebanon (Lebanese) | 1802 (25) | 16 | 61 (11) | 466 (56) | 56 (12) | MI diagnosed by ECG and high troponin levels, unstable or stable angina, heart failure, or reversible ischemia |
| Framingham Heart Study | Cohort (1948) | United States (white European) | 259 (NA) | 6 | 65 (13) | 4202 (NA) | 75 (12) | Nonfatal MI (diagnosed with documented evidence from ECG or elevated enzymes) or CHD (defined as recognized fatal or nonfatal MI, coronary insufficiency, or the first fatal CHD event |
| Genomics Research in Cardiovascular Disease | Case-control (NA) | Korea (East Asian) | 2099 ( ~ 39) | 30 | ≈ 52 (8) | 2690 ( ≈ 56) | ≈ 53 (8) | MI, stable angina, or unstable angina |
| German Myocardial Infarction Family Study | ||||||||
| I | Case-control (NA) | Germany (white European) | 634 (34) | 100 | 50 (8) | 1608 (51) | 63 (10) | Included patients who had MI at an early age |
| II | Case-control (NA) | Germany (white European) | 1207 (21) | 100 | 51 (8) | 1288 (49) | 51 (12) | Confirmed MI with an early age (<60 y) of onset and a positive family history for CAD |
| III (KORA) | Cohort (NA) | Germany (white European) | 1061 (21) | 100 | 59 (9) | 1467 (52) | 58 (10) | Nonfatal MI diagnosed by the use of the algorithm of the World Health Organization's Multinational Monitoring of Trends and Determinants in Cardiovascular Disease (MONICA) project |
| IV (KORA) | Cohort (NA) | Germany (white European) | 1089 (36) | 100 | 58 (10) | 1147 (62) | 57 (17) | MI or CAD defined as ≥50% stenosis in 1 major coronary vessel and age of onset <65 y in men and <70 y in women |
| Genetics of Diabetes and Audit Research in Tayside and Scotland | Case-control (NA) | Scotland (white European) | 877 (NA) | NA | NA | 2187 (NA) | NA | Nonfatal and fatal MI, unstable angina or coronary revascularization |
| Medical Research Council and British Heart Foundation Heart Protection Study | Nested CC (1994-2001) | United Kingdom (white European) | 2700 (24) | 65 | 59 (9) | 2758 (73) | 50 (15) | History of MI, unstable or stable angina, coronary artery bypass grafting, or angioplasty |
| Helsinki Sudden Death Study and the Tampere Coronary Study | Case-control (1981-1992) | Finland (white European) | 206 (0) | 46 | NA | 259 (0) | NA | Coronary artery stenosis ≥50, old or acute MI, or sudden cardiac death caused by plaque rupture and thrombosis |
| Biome Biobank Program at Mt Sinai | Case-control (2007) | United States (African Americans) | 361 (67) | 36 | NA | 2778 (71) | NA | NA |
| Case-control (2007) | United States (European American) | 487 (35) | 30 | NA | 1381 (62) | NA | NA | |
| Case-control (2007) | United States (Hispanic American) | 758 (55) | 37 | NA | 3337 (71) | NA | NA | |
| INTERHEART study | Case-control (NA) | Worldwide (white European) | 402 (29) | 100 | 63 (11) | 448 (33) | 64 (10) | Incident acute MI, presenting to a hospital within 24 h of symptom onset |
| Leipzig Research Center for Civilization Diseases Heart Study | Case-control (2006-2011) | Germany (white European) | 1535 (25) | 44 | 64 (11) | 772 (50) | 64 (11) | Luminal reduction of >50% in any vessel |
| London Life Sciences Prospective Population Study | Cohort (2002-NA) | United Kingdom (white European) | 2791 (19) | 44 | 59 (1) | 3757 (14) | 52 (10) | History of MI, coronary artery revascularization, or angiographically confirmed coronary artery stenosis >50% |
| Ludwigshafen Risk and Cardiovascular Health Study | Case-control (1997-2000) | Germany (white European) | 2095 (25) | 63 | NA | 503 (48) | 63 (11)a | Luminal narrowing (>50% stenosis) in ≥15 coronary segments according to a classification of the American Heart Association |
| Mayo Vascular Diseases Biorepository Study | Case-control (2009-) | United States (white European) | 745 (NA) | NA | NA | 1389 (NA) | NA | History of MI, coronary revascularization, angina with a positive stress test result, or >50% stenosis of an epicardial coronary artery on coronary angiography |
| Medstar cardiac catheterization study | Case-control (2004-2007) | United States (white European) | 875 (33) | 100 | 49 (7) | 447 (55) | 60 (9) | ≥1 coronary vessel(s) with ≥50% stenosis |
| Myocardial Infarction Genetics Consortium | Case-control (NA) | United States (white European) | 2905 (25) | 100 | NA | 2998 (27) | NA | MI diagnosed on the basis of autopsy evidence of fatal MI or a combination of chest pain, ECG evidence of MI, or elevation of ≥1 cardiac biomarkers |
| Ottawa Heart Genetic Study | ||||||||
| A2 | Case-control (NA) | Canada (white European) | 947 (25) | 64 | NA | 1008 (51) | NA | MI, coronary artery bypass graft, percutaneous intervention or a stenosis of ≥50% in ≥1 epicardial vessel |
| B2 | Case-control (NA) | Canada (white European) | 1294 (22) | 56 | NA | 1529 (50) | NA | MI, coronary artery bypass graft, percutaneous intervention or a stenosis of ≥50% in ≥1 epicardial vessel |
| C2 | Case-control (NA) | Canada (white European) | 843 (6) | 44 | NA | 318 (67) | NA | MI, coronary artery bypass graft, percutaneous intervention or a stenosis of ≥50% in ≥1 epicardial vessel |
| PennCath Study | Case-control (NA) | United States (white European) | 933 (24) | 100 | 53 (8) | 468 (52) | 62 (10) | ≥1 coronary vessels with ≥50% stenosis |
| Prospective Investigation of the Vasculature in Uppsala Seniors | Cohort (2001-NA) | Sweden (white European) | 119 (24) | 77 | 65 (7) | 830 (55) | 70 (0.2) | Fatal or nonfatal MI, stable or unstable angina, coronary revascularization, or coronary artery stenosis |
| A subset of FINRISK cohort study | Cohort (1987-2012) | Finland (white European) | 631 (31) | 40 | NA | 334 (43) | NA | MI, unstable angina, coronary revascularization, or CHD death |
| Precocious Coronary Artery Disease | Case-control (2007-2011) | Germany, Sweden, Italy, United Kingdom (white European) | 5719 (29) | 80 | 54 (8) | 6545 (63) | NA | MI, intervention for coronary revascularization, symptomatic acute coronary syndrome, or chronic stable angina with an age at diagnosis of ≤65 y |
| Pakistan Risk of Myocardial Infarction Study | Case-control (NA) | Pakistan (South Asian) | 4651 (NA) | 100 | 54 (11) | 4452 (NA) | 54 (10) | MI within 24 h of hospital presentation; typical ECG changes; and positive troponin I test result |
| Pakistan Risk of Myocardial Infarction Study II | Case-control (NA) | Pakistan (South Asian) | 4380 (NA) | 100 | NA | 3929 (NA) | NA | MI within 24 h of hospital presentation; typical ECG changes; and positive troponin I test result |
| Prospective Study of Pravastatin in the Elderly at Risk | Nested Case-control (1998-NA) | Scotland, Ireland, the Netherlands (white European) | 2034 (47) | 38 | 75 (3) | 3210 (47) | 75 (3) | MI and other unspecified CAD cases |
| Rotterdam Study | Cohort (1990-1993) | Netherlands (white European) | 506 (NA) | 83 | NA | 5335 (58) | 67 (8)b | MI and other unspecified CAD cases |
| Sikh Diabetes Study and Asian Indian Diabetic Heart Study | Case-control (NA) | India (Indian, Asian, or Punjabi) | 836 (30) | 80 | NA | 761 (49) | NA | MI, nitrate medication use (nitroglycerine), angina pain, or >50% coronary artery stenosis |
| Hellenic Study of Interactions between SNPs and Eating in Atherosclerosis Susceptibility | Case-control (2006-2009) | Greece (white European) | 426 (21) | 60 | ~ 59 (14) | 594 (56) | ~ 60 (14) | Acute MI or unstable angina corresponding to class III of the Braunwald classification |
| TwinGene | Cohort (2004-2008) | Sweden (white European) | 814 (29) | 71 | NA | 5999 (56) | 65 (8)b | Fatal or nonfatal MI, stable or unstable angina, coronary revascularization, or coronary artery stenosis |
| Uppsala Longitudinal Study of Adult Men | Cohort (NA) | Sweden (white European) | 322 (0) | 84 | NA | 857 (0) | 71 (1)b | Fatal or nonfatal MI, stable or unstable angina, coronary revascularization, or coronary artery stenosis |
| Women's Genome Health Study | Cohort (1992-1995) | United States (white European) | 1007 (100) | 38 | NA | 22 286 (100) | 55 (7)b | NA |
| Wellcome Trust Case Control Consortium | Case-control (2005-NA) | United Kingdom (white European) | 1926 (21) | 72 | 50 (8) | 2938 (51) | 50 (8) | History of MI or coronary revascularization |
Abbreviations: CAD, coronary artery disease; CHD, coronary heart disease; ECG, electrocardiogram/electrocardiography; ICD-10, International Classification of Diseases, 10th Revision; MI, myocardial infarction; NA, not available.
The number of cases and noncases in each study do not sum to the number of individuals included in the analysis because a few individuals were removed after quality control criteria were established.
Based on the whole cohort at baseline.
Statistical Analysis
SNPs were matched across the data sources by assigning them to the same effect allele. The association of each SNP with CAD and myocardial infarction was weighted by its association with serum calcium, and estimates were combined using an inverse-variance weighted meta-analysis. Complementary analyses using the weighted median and MR-Egger regression methods were performed. The odds ratios (ORs) of CAD and myocardial infarction were scaled per 0.5-mg/dL increase (about 1 SD) in serum calcium levels. For the calcium-associated SNPs, the summary statistics were based on 44 to all 48 studies included in the CardiogramplusC4D consortium. All statistical tests were 2-sided. The threshold of statistical significance for the analyses of 6 SNPs by Bonferroni correction was P < .008 ([P < .05]/6 SNPs); statistical tests for the mendelian randomization analyses of CAD and myocardial infarction were considered statistically significant at P < .025 ([P < .05]/2 outcome measures). All analyses were conducted in Stata (StataCorp), version 14.2, and R (R Foundation), version 3.2.5.
Results
The analytic sample included up to 60 801 CAD cases (approximately 70% with myocardial infarction) and 123 504 noncases from 48 cohort and case-control studies. The majority of participants were of European (77%), South Asian (13%), and East Asian (6%) ancestry (Table 1).
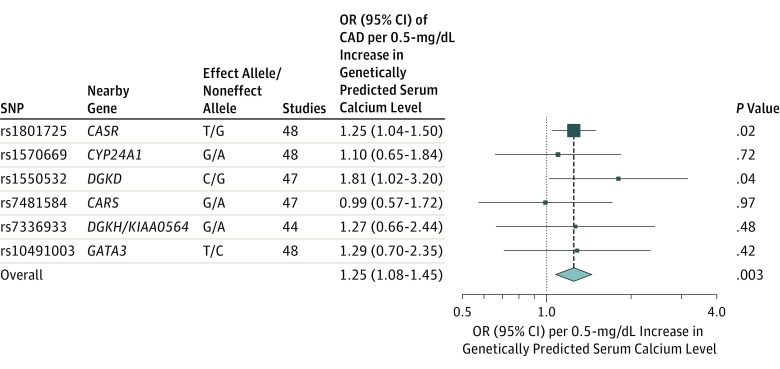
The 6 SNPs related to serum calcium levels and without pleiotropic associations with potential confounders were estimated to explain about 0.8% of the variation in serum calcium levels. None of the individual 6 SNPs was associated with CAD at Bonferroni corrected significance level (P < .008) (Table 2). In the overall inverse-variance weighted meta-analysis of the 6 SNPs, the OR of CAD per 0.5-mg/dL increase (about 1 SD) in genetically predicted serum calcium was 1.25 (95% CI, 1.08-1.45; P = .003) (Figure 3). In a sensitivity analysis excluding the SNP in the CASR gene, which provided the most weight to the overall estimate, the OR of CAD was 1.25 (95% CI, 0.97-1.62). An analysis of patients with only myocardial infarction as the outcome (about 70% of all study cases) yielded similar results (OR, 1.24 [95% CI, 1.05-1.46]; P = .009) (eFigure in the Supplement).
Table 2. Characteristics of the Calcium-Associated Genetic Variants.
| SNP | Nearby Gene | Chromosome | Effect Allelea | Effect Allele Frequencyb | Calcium Results | CAD Results | |||
|---|---|---|---|---|---|---|---|---|---|
| β (mg/dL)c | P Valuec | Variance, %d | OR (95% CI)e |
P Valuee | |||||
| rs1801725 | CASR | 3 | T | 0.14 | 0.071 | 8.9 × 10−86 | 0.49 | 1.032 (1.006-1.059) |
.02 |
| rs1570669 | CYP24A1 | 20 | G | 0.36 | 0.018 | 9.1 × 10−12 | 0.06 | 1.003 (0.985-1.022) |
.72 |
| rs1550532 | DGKD | 2 | C | 0.31 | 0.018 | 8.2 × 10−11 | 0.06 | 1.021 (1.001-1.043) |
.04 |
| rs7481584 | CARS | 11 | G | 0.69 | 0.018 | 1.2 × 10−10 | 0.06 | 1.000 (0.980-1.020) |
.97 |
| rs7336933 | DGKH/KIAA0564 | 13 | G | 0.86 | 0.022 | 9.1 × 10−10 | 0.05 | 1.011 (0.982-1.040) |
.48 |
| rs10491003 | GATA3 | 10 | T | 0.09 | 0.027 | 4.8 × 10−09 | 0.05 | 1.014 (0.981-1.047) |
.42 |
Abbreviations: CAD, coronary artery disease; OR, odds ratio; SNP, single-nucleotide polymorphism.
Calcium-raising allele.
Frequency of the calcium-raising allele, expressed as a proportion, in the CardiogramplusC4D consortium.
Summary statistics per effect allele for serum calcium levels obtained from a genome-wide association meta-analysis of about 61 000 individuals of European ancestry. As an example, for the genetic variant in CASR, serum calcium levels increase by 0.071 mg/dL per additional T allele.
Proportion of variance in serum calcium explained by each SNP. Calculated as r2 = 2 × minor allele frequency × (1 − minor allele frequency) × (β/SD), where 1 SD equals 0.5 mg/dL.
Effect size estimate (β coefficient, measured as log OR of CAD per additional calcium-raising allele, and standard error) and P value for each SNP on CAD were obtained from the CardiogramplusC4D consortium (a 1000 genomes-based genome-wide association meta-analysis of 48 studies) comprising a total of 60 801 CAD cases and 123 504 noncases.
Figure 3. Mendelian Randomization Estimates of the Association Between Genetically Predicted Serum Calcium Levels and Coronary Artery Disease.
OR indicates odds ratio; SNP, single-nucleotide polymorphisms. Data markers indicate the OR for the association of each calcium-associated SNP with coronary artery disease. Size of the data marker is inversely proportional to variance of the estimate. Error bars indicate 95% CIs.
The association between genetically predicted serum calcium levels and CAD was consistent in complementary analyses using the weighted median method (OR, 1.25 [95% CI, 1.06-1.48]) and MR-Egger regression, although with a wider CI (OR, 1.26 [95% CI, 0.96-1.63]). There was no evidence of pleiotropy (MR-Egger intercept, −0.00035; P = .96), or heterogeneity between the mendelian randomization estimates from different SNPs (I2 = 0%, P = .78 for heterogeneity).
Discussion
This mendelian randomization study showed that a genetic predisposition to higher serum calcium levels was associated with increased risk of CAD and myocardial infarction. The OR per 0.5-mg/dL increase (about 1 SD) in serum calcium levels was 1.25 for CAD and 1.24 for myocardial infarction. The risk increase is similar or weaker in magnitude to previously reported genetic associations (per 1-SD increase) with triglyceride levels (OR, 1.28), low-density lipoprotein cholesterol levels (OR, 1.68), systolic and diastolic blood pressure (OR, 1.49), and body mass index (OR, 1.40).
The finding from this study corroborates results from several observational studies showing a positive association of serum calcium levels with risk of cardiovascular disease. A meta-analysis of 8 observational studies found a hazard ratio of cardiovascular disease of 1.08 (95% CI, 1.04-1.13) per 1-SD increment of serum calcium levels and a corresponding OR of 1.22 (95% CI, 1.11-1.32) in 2 studies that reported ORs.
Data from randomized clinical trials indicate that calcium supplementation leads to hypercalcemia and increased transition of soluble calcium-related protein particles to insoluble calciprotein particles reflecting higher concentrations of activators of calcification present in serum, as well as an increased risk of myocardial infarction. Based on results from interventions, there is a peak in ionized and total serum calcium levels 4 hours after ingestion of 1000-mg supplemental calcium and the increase in total serum calcium corresponds to about 1 SD.
A similar increase in serum calcium from baseline over 6 hours is observed following the ingestion of a 500-mg calcium supplement, whereas the increase in serum calcium after a corresponding calcium dose by a dairy product intake is less pronounced. In a meta-analysis of 9 randomized clinical trials, calcium supplementation with or without vitamin D increased the risk of myocardial infarction by 24%, but the result is disputed.
Findings from observational studies further show that calcium supplement use is associated with increased risk of incident coronary artery calcification, incident myocardial infarction, and coronary heart disease mortality. Possible mechanisms whereby elevated serum calcium levels may increase the risk of CAD include effects on vascular calcification, vascular cells, blood coagulation, and altered gene expression induced by effects on arterial wall calcium-sensing receptor. The potential mechanisms underlying the association need to be more thoroughly evaluated.
Strengths of this mendelian randomization analysis include the large sample size and the use of multiple uncorrelated SNPs associated with serum calcium levels, which increases the precision of the estimate.
Limitations
This study has several limitations. First, the genetic variant in the CASR gene provided more weight, explained by the stronger relation between this SNP and serum calcium, than the other variants to the overall estimate of the genetic association between serum calcium levels and CAD. However, 4 of the other 5 variants associated with serum calcium had positive estimates for association with CAD, and 3 variants had higher ORs for association with CAD per 0.5 mg/dL increase in serum calcium compared with the genetic variant in the CASR gene. Moreover, the overall estimate was identical although with lower precision after omitting the variant in CASR. CASR encodes the calcium-sensing receptor, which plays a key role in calcium homeostasis.
Second, there was partial overlap between studies included in the GWAS meta-analysis of calcium (N = 61 069) and the CardiogramplusC4D consortium (N = 184 305). This could result in model overfitting if the SNP-calcium associations were estimated in studies that were included in the CardiogramplusC4D consortium. Of the 28 studies included in the GWAS meta-analysis of calcium, 9 were also included in CardiogramplusC4D. If all the individuals in each of these studies appeared in both meta-analyses, then there would be an overlap of 26 776 of the 61 069 individuals in the calcium GWAS meta-analysis. This could potentially lead to a small bias in mendelian randomization estimates. However, if genetic associations with serum calcium levels were estimated in noncases only (as is usual for continuous phenotypes such as serum calcium levels), then this sample overlap would not lead to bias or type 1 error inflation.
Third, the study lacked complete information on sex and age, and that a potential nonlinear association between serum calcium levels and CAD could not be evaluated.
Fourth, a replication data set with a similar large number of CAD cases was not available.
The reliability of the findings from a mendelian randomization study depends on 3 key assumptions (Figure 1), which could be violated by population stratification, canalization, pleiotropy, and linkage disequilibrium. It cannot be completely ruled out that population stratification may have had some influence on the results because the CardiogramplusC4D consortium included individuals of different ancestry with potentially different allele frequencies. However, analyses for the CardiogramplusC4D consortium were conducted separately in each study and then combined, and adjustment was made for genetic principal components, mitigating the potential effect of population stratification.
Furthermore, the vast majority of participants in CardiogramplusC4D were of European descent and the effect allele frequencies of the 6 calcium-associated SNPs were very similar in CardiogramplusC4D and the GWAS meta-analysis of calcium. The SNP in the CASR gene has been consistently associated with serum calcium in populations of different ancestry, including Europeans, Indian Asians, and Japanese. The other 5 SNPs were robustly associated with serum calcium in a GWAS meta-analysis of about 61 000 individuals.
Whether canalization, which is defined as compensatory feedback mechanisms, may have affected the results could not be directly tested. Because canalization assumes that there are other mechanisms that mitigate the genetic effect, such feedback mechanisms would bias the results toward the null and cannot explain the observed association.
Several approaches were undertaken to assess and adjust for potential confounding or pleiotropic effects. First, each SNP associated with serum calcium was assessed for associations with known cardiometabolic risk factors for CAD, and 1 SNP with pleiotropic associations was excluded. In addition, sensitivity analyses using the weighted median and MR-Egger regression approaches to explore and adjust for pleiotropy were conducted. The results were consistent in these analyses, indicating that confounding is unlikely to explain the observed association. Linkage disequilibrium with directly causal variants (violating the third assumption) was likely avoided owing to the use of multiple SNPs of which most were positively associated with CAD.
Conclusions
A genetic predisposition to higher serum calcium levels was associated with increased risk of CAD and myocardial infarction. Whether the risk of CAD associated with lifelong genetic exposure to increased serum calcium levels can be translated to a risk associated with short-term to medium-term calcium supplementation is unknown.
eTable. P Values for Associations of the Calcium-Associated Genetic Variants with Cardiometabolic Traits
eFigure. Mendelian Randomization Estimates of the Association Between Genetically Predicted Serum Calcium Levels and Myocardial Infarction
References
- 1.Reid IR, Gamble GD, Bolland MJ. Circulating calcium concentrations, vascular disease and mortality: a systematic review. J Intern Med. 2016;279(6):524-540. [DOI] [PubMed] [Google Scholar]
- 2.Rohrmann S, Garmo H, Malmström H, et al. Association between serum calcium concentration and risk of incident and fatal cardiovascular disease in the prospective AMORIS study. Atherosclerosis. 2016;251:85-93. [DOI] [PubMed] [Google Scholar]
- 3.Bristow SM, Gamble GD, Stewart A, et al. Acute and 3-month effects of microcrystalline hydroxyapatite, calcium citrate and calcium carbonate on serum calcium and markers of bone turnover: a randomised controlled trial in postmenopausal women. Br J Nutr. 2014;112(10):1611-1620. [DOI] [PubMed] [Google Scholar]
- 4.Barry EL, Mott LA, Melamed ML, et al. Calcium supplementation increases blood creatinine concentration in a randomized controlled trial. PLoS One. 2014;9(10):e108094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bolland MJ, Grey A, Avenell A, Gamble GD, Reid IR. Calcium supplements with or without vitamin D and risk of cardiovascular events: reanalysis of the Women’s Health Initiative limited access dataset and meta-analysis. BMJ. 2011;342:d2040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Van Hemelrijck M, Michaelsson K, Linseisen J, Rohrmann S. Calcium intake and serum concentration in relation to risk of cardiovascular death in NHANES III. PLoS One. 2013;8(4):e61037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mangano KM, Walsh SJ, Insogna KL, Kenny AM, Kerstetter JE. Calcium intake in the United States from dietary and supplemental sources across adult age groups: new estimates from the National Health and Nutrition Examination Survey 2003-2006. J Am Diet Assoc. 2011;111(5):687-695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.An R, Chiu CY, Andrade F. Nutrient intake and use of dietary supplements among US adults with disabilities. Disabil Health J. 2015;8(2):240-249. [DOI] [PubMed] [Google Scholar]
- 9.Dickinson A, MacKay D. Health habits and other characteristics of dietary supplement users: a review. Nutr J. 2014;13:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Reid IR, Bristow SM, Bolland MJ. Cardiovascular complications of calcium supplements. J Cell Biochem. 2015;116(4):494-501. [DOI] [PubMed] [Google Scholar]
- 11.Margolis KL, Manson JE. Calcium supplements and cardiovascular disease risk: what do clinicians and patients need to know? Ann Intern Med. 2016;165(12):884-885. [DOI] [PubMed] [Google Scholar]
- 12.Bauer DC. The calcium supplement controversy: now what? J Bone Miner Res. 2014;29(3):531-533. [DOI] [PubMed] [Google Scholar]
- 13.Burgess S, Thompson SG. Mendelian randomization: methods for using genetic variants in causal estimation. London, UK: Chapman & Hall; 2015. [Google Scholar]
- 14.Greenland S. An introduction to instrumental variables for epidemiologists. Int J Epidemiol. 2000;29(4):722-729. [DOI] [PubMed] [Google Scholar]
- 15.Burgess S, Scott RA, Timpson NJ, Davey Smith G, Thompson SG; EPIC- InterAct Consortium . Using published data in mendelian randomization: a blueprint for efficient identification of causal risk factors. Eur J Epidemiol. 2015;30(7):543-552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.O’Seaghdha CM, Wu H, Yang Q, et al. ; SUNLIGHT Consortium; GEFOS Consortium . Meta-analysis of genome-wide association studies identifies six new Loci for serum calcium concentrations. PLoS Genet. 2013;9(9):e1003796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Willer CJ, Schmidt EM, Sengupta S, et al. ; Global Lipids Genetics Consortium . Discovery and refinement of loci associated with lipid levels. Nat Genet. 2013;45(11):1274-1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dupuis J, Langenberg C, Prokopenko I, et al. New genetic loci implicated in fasting glucose homeostasis and their impact on type 2 diabetes risk. Nat Genet. 2010;42(2):105-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mahajan A, Go MJ, Zhang W, et al. Genome-wide trans-ancestry meta-analysis provides insight into the genetic architecture of type 2 diabetes susceptibility. Nat Genet. 2014;46(3):234-244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Locke AE, Kahali B, Berndt SI, et al. Genetic studies of body mass index yield new insights for obesity biology. Nature. 2015;518(7538):197-206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shungin D, Winkler TW, Croteau-Chonka DC, et al. New genetic loci link adipose and insulin biology to body fat distribution. Nature. 2015;518(7538):187-196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ehret GB, Munroe PB, Rice KM, et al. Genetic variants in novel pathways influence blood pressure and cardiovascular disease risk. Nature. 2011;478(7367):103-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nikpay M, Goel A, Won HH, et al. ; CARDIoGRAMplusC4D Consortium . A comprehensive 1000 Genomes-based genome-wide association meta-analysis of coronary artery disease. Nat Genet. 2015;47(10):1121-1130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Burgess S, Bowden J, Fall T, Ingelsson E, Thompson SG. Sensitivity analyses for robust causal inference from mendelian randomization analyses with multiple genetic variants. Epidemiology. 2017;28(1):30-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.White J, Swerdlow DI, Preiss D, et al. Association of lipid fractions with risks for coronary artery disease and diabetes. JAMA Cardiol. 2016;1(6):692-699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.van Iperen EP, Sivapalaratnam S, Holmes MV, Hovingh GK, Zwinderman AH, Asselbergs FW. Genetic analysis of emerging risk factors in coronary artery disease. Atherosclerosis. 2016;254:35-41. [DOI] [PubMed] [Google Scholar]
- 27.Hägg S, Fall T, Ploner A, et al. ; European Network for Genetic and Genomic Epidemiology Consortium . Adiposity as a cause of cardiovascular disease: a mendelian randomization study. Int J Epidemiol. 2015;44(2):578-586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bristow SM, Gamble GD, Pasch A, et al. Acute and 3-month effects of calcium carbonate on the calcification propensity of serum and regulators of vascular calcification: secondary analysis of a randomized controlled trial. Osteoporos Int. 2016;27(3):1209-1216. [DOI] [PubMed] [Google Scholar]
- 29.Bristow SM, Gamble GD, Stewart A, Kalluru R, Horne AM, Reid IR. Acute effects of calcium citrate with or without a meal, calcium-fortified juice and a dairy product meal on serum calcium and phosphate: a randomised cross-over trial. Br J Nutr. 2015;113(10):1585-1594. [DOI] [PubMed] [Google Scholar]
- 30.Anderson JJ, Kruszka B, Delaney JA, et al. Calcium intake from diet and supplements and the risk of coronary artery calcification and its progression among older adults: 10-year follow-up of the Multi-Ethnic Study of Atherosclerosis (MESA). J Am Heart Assoc. 2016;5(10):e003815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li K, Kaaks R, Linseisen J, Rohrmann S. Associations of dietary calcium intake and calcium supplementation with myocardial infarction and stroke risk and overall cardiovascular mortality in the Heidelberg cohort of the European Prospective Investigation into Cancer and Nutrition study (EPIC-Heidelberg). Heart. 2012;98(12):920-925. [DOI] [PubMed] [Google Scholar]
- 32.Xiao Q, Murphy RA, Houston DK, Harris TB, Chow WH, Park Y. Dietary and supplemental calcium intake and cardiovascular disease mortality: the National Institutes of Health-AARP diet and health study. JAMA Intern Med. 2013;173(8):639-646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Burgess S, Davies NM, Thompson SG. Bias due to participant overlap in two-sample mendelian randomization. Genet Epidemiol. 2016;40(7):597-608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kapur K, Johnson T, Beckmann ND, et al. Genome-wide meta-analysis for serum calcium identifies significantly associated SNPs near the calcium-sensing receptor (CASR) gene. PLoS Genet. 2010;6(7):e1001035. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. P Values for Associations of the Calcium-Associated Genetic Variants with Cardiometabolic Traits
eFigure. Mendelian Randomization Estimates of the Association Between Genetically Predicted Serum Calcium Levels and Myocardial Infarction