Key Points
Question
Does first-line contact aspiration result in an increased successful revascularization rate compared with first-line use of a stent retriever in patients with acute ischemic stroke undergoing thrombectomy?
Findings
In this multicenter randomized clinical trial, 381 patients with acute ischemic stroke and large vessel occlusion were randomized to first-line contact aspiration or stent retriever revascularization. There was no significant difference in successful revascularization rates at the end of the procedure (85.4% for contact aspiration vs 83.1% for stent retriever).
Meaning
First-line contact aspiration did not result in increased successful revascularization compared with first-line use of a stent retriever.
Abstract
Importance
The benefits of endovascular revascularization using the contact aspiration technique vs the stent retriever technique in patients with acute ischemic stroke remain uncertain because of lack of evidence from randomized trials.
Objective
To compare efficacy and adverse events using the contact aspiration technique vs the standard stent retriever technique as a first-line endovascular treatment for successful revascularization among patients with acute ischemic stroke and large vessel occlusion.
Design, Setting, and Participants
The Contact Aspiration vs Stent Retriever for Successful Revascularization (ASTER) study was a randomized, open-label, blinded end-point clinical trial conducted in 8 comprehensive stroke centers in France (October 2015-October 2016). Patients who presented with acute ischemic stroke and a large vessel occlusion in the anterior circulation within 6 hours of symptom onset were included.
Interventions
Patients were randomly assigned to first-line contact aspiration (n = 192) or first-line stent retriever (n = 189) immediately prior to mechanical thrombectomy.
Main Outcomes and Measures
The primary outcome was the proportion of patients with successful revascularization defined as a modified Thrombolysis in Cerebral Infarction score of 2b or 3 at the end of all endovascular procedures. Secondary outcomes included degree of disability assessed by overall distribution of the modified Rankin Scale (mRS) score at 90 days, change in National Institutes of Health Stroke Scale (NIHSS) score at 24 hours, all-cause mortality at 90 days, and procedure-related serious adverse events.
Results
Among 381 patients randomized (mean age, 69.9 years; 174 women [45.7%]), 363 (95.3%) completed the trial. Median time from symptom onset to arterial puncture was 227 minutes (interquartile range, 180-280 minutes). For the primary outcome, the proportion of patients with successful revascularization was 85.4% (n = 164) in the contact aspiration group vs 83.1% (n = 157) in the stent retriever group (odds ratio, 1.20 [95% CI, 0.68-2.10]; P = .53; difference, 2.4% [95% CI, −5.4% to 9.7%]). For the clinical efficacy outcomes (change in NIHSS score at 24 hours, mRS score at 90 days) and adverse events, there were no significant differences between groups.
Conclusions and Relevance
Among patients with ischemic stroke in the anterior circulation undergoing thrombectomy, first-line thrombectomy with contact aspiration compared with stent retriever did not result in an increased successful revascularization rate at the end of the procedure.
Trial Registration
clinicaltrials.gov Identifier: NCT02523261
This randomized trial compares the effects of thrombectomy with a contact aspiration vs a stent retriever technique on successful endovascular revascularization in patients with acute ischemic stroke.
Introduction
After recent reports from 6 randomized clinical trials (RCTs) demonstrated the superiority of mechanical thrombectomy over standard medical management alone, research priorities shifted toward reducing time to revascularization, optimizing imaging methods for patient selection, and evaluating new thrombectomy devices. Because stent retriever techniques were used predominantly in these trials, questions remain regarding the safety and efficacy of aspiration thrombectomy techniques as a first-line therapy. A direct aspiration first-pass technique (ADAPT), or contact aspiration, involves the first-line use of aspiration through a large-bore catheter, then adding a stent retriever if needed. In cases in which aspiration alone is not successful in removing the thrombus, the large-bore aspiration catheter provides the additional benefit of offering access for a stent retriever.
Contact aspiration has not been demonstrated to be superior or noninferior to the stent retriever technique. Nevertheless, aspiration has gained growing acceptance as it is thought to facilitate revascularization quickly and potentially at a lower cost. Controversies about the relevance of the technique have arisen in rare cases of aspiration component failure because of concerns that it might result in a delay in revascularization that could have been avoided by using the stent retriever technique as first-line endovascular therapy. Although no randomized trials have studied aspiration vs the stent retriever technique to date, some retrospective studies have reported increased successful revascularization rates when using contact aspiration as first-line endovascular treatment. Additional insights through RCTs are needed to identify which patients may benefit from this novel technique.
The Contact Aspiration vs Stent Retriever for Successful Revascularization (ASTER) trial aimed to compare the efficacy and adverse events of first-line neurothrombectomy using the contact aspiration technique vs the standard stent retriever technique.
Methods
The study protocol and the consent form were approved by the Comité de Protection des Personnes Ile de France VI (ID 2015-A00830-49). The details of the trial protocol were published previously (available in Supplement 1).
Trial Design
This trial was a randomized, multicenter, open-label, blinded end-point clinical trial. It was an investigator-initiated trial designed to assess the effect of the first-line strategy for mechanical thrombectomy (contact aspiration vs stent retriever) on revascularization rates at the end of all endovascular procedures.
Patients were recruited at 8 high-volume, comprehensive stroke centers in France, all of which regularly perform both types of techniques. The study was conducted in accordance with the Declaration of Helsinki and Good Clinical Practice. Data collection during the study was facilitated with an electronic case report form developed using Clinsight software (ENNOV).
According to French laws, oral informed consent was sought from patients if their level of consciousness was sufficient, or else from a relative. This study operated under an emergency inclusion protocol because of the nature of the condition.
Patient Population
This study enrolled adults admitted with suspected ischemic stroke secondary to occlusion of the anterior circulation within 6 hours of onset of symptoms. Patients were required to have imaging evidence of occlusion of the intracranial internal carotid artery or the M1 or M2 branches of the middle cerebral artery. Use of intravenous (IV) thrombolysis treatment was permitted. Key exclusion criteria included cerebral infarction of the posterior circulation, occlusion of the cervical carotid artery, and prestroke modified Rankin Scale (mRS) score greater than 3.
Randomization
Immediately after baseline brain imaging and prior to the endovascular procedure, patients were randomly allocated in a 1:1 fashion to undergo either contact aspiration (intervention) or stent retriever (control) thrombectomy as the first-line intervention. The randomization sequence was provided by an independent statistician (who did not take part in assessing the patients at any point in the study) using computer-generated random numbers with block sizes of 4 and stratification by center and IV tissue plasminogen activator (tPA) treatment. The block size information was not specified in the protocol to ensure that vascular neurologists and interventional neuroradiologists were not able to anticipate treatment group assignment. The randomization sequence was implemented in the electronic case report form system to ensure a centralized real-time randomization procedure. Patients were enrolled and randomized by vascular neurologists and interventional neuroradiologists.
Interventions
In line with the recommendations of the American Stroke Association and European Stroke Organization, enrolled patients received IV thrombolysis (if eligible) and were then transferred to the angiographic suite for urgent thrombectomy. Patients underwent their assigned endovascular procedure (contact aspiration or stent retriever) under general anesthesia or conscious sedation. Operators were required to perform at least 3 attempts at revascularization using the assigned endovascular technique before switching to another endovascular procedure (rescue therapy) if needed and in accordance with good practice recommendations. The decisions of whether to use a rescue therapy and which rescue therapy to use were at the discretion of the operator. Permitted rescue techniques were contact aspiration, stent retriever, combined contact aspiration and stent retriever, and angioplasty with or without stenting.
Contact aspiration was performed using a long sheath positioned in the distal cervical vasculature using an exchange technique. The technique has been previously reported. A 0.021- to 0.027-in inner lumen microcatheter was advanced up to or past the thrombus over a microwire and then a large-bore aspiration catheter was advanced as close to the proximal aspect of the thrombus as possible. The large-bore aspiration catheter was connected to a source of continuous aspiration, and thrombus aspiration was attempted.
The stent retriever technique used was in accordance with the European Conformity marked device instructions for use. A large-bore balloon guide catheter was positioned in the cervical internal carotid artery. A delivery microcatheter was navigated over a microwire into the occluded artery, and the stent retriever was deployed across the occlusion. During stent retriever removal, the proximal vessel was occluded by inflation of the balloon guide catheter. The Solitaire and Trevo stent retriever devices were most commonly used.
Outcomes
Primary Outcome
The primary outcome was the percentage of patients with successful revascularization defined as a modified Thrombolysis in Cerebral Infarction (mTICI) score of 2b or 3 at the end of angiography after all endovascular treatments.
Secondary Outcomes
The secondary technical efficacy outcomes included the percentage of patients with successful revascularization (separately defined as mTICI score of 2b/3, mTICI score of 2c/3, or mTICI score of 3) at the end of the first-line procedure, the percentage of patients with successful revascularization (separately defined as mTICI score of 2c/3 or mTICI score of 3) at the end of all procedures, and the time from arterial puncture to successful revascularization (defined as mTICI score of 2b/3).
The secondary clinical efficacy outcomes were degree of disability assessed by overall distribution of the mRS score at 90 days (shift analysis combining scores of 5 and 6), functional independence as defined by a 90-day mRS score of 2 or lower, change in National Institutes of Health Stroke Scale (NIHSS) score at 24 hours, and death due to any cause at 90 days.
Adverse events included procedure-related serious adverse events (arterial perforation, arterial dissection, embolization in a new vascular territory, subarachnoid hemorrhage, vasospasm), intracranial hemorrhage on imaging at 24 hours according to the European Cooperative Acute Stroke Study 3 classification, and symptomatic intracranial hemorrhage at 24 hours, defined as any intracranial hemorrhage, including intracerebral, subarachnoid, and intraventricular hemorrhages, visualized on follow-up imaging and associated with a 4-point or greater worsening on the NIHSS score or that resulted in death.
A cost-effectiveness analysis was prespecified as a secondary end point and is ongoing.
Blinding
For the primary outcome, 2 independent assessors at a central imaging core laboratory not involved in patient management determined the mTICI score and collateral status. In cases of disagreement between the 2 assessors, a centralized neurointerventionalist reviewed angiograms and decided on the primary end-point value. All neuroimaging readings including determination of site of arterial occlusion, clot burden score, and hemorrhagic transformation were performed at the imaging core laboratory and blinded to procedure allocation. Serious adverse events and procedure-related complications were adjudicated by 3 members of the data and safety monitoring board blinded to treatment group. The 90-day mRS score was assessed by trained research nurses unaware of the group assignments during face-to-face interviews or via telephone conversations. The NIHSS score at 24 hours was assessed by the treating physician, who was not blinded to the group assignments.
Statistical Analysis
The study was designed to have a statistical power of 90% with a 2-sided α=.05 to demonstrate the superiority of first-line contact aspiration over stent retriever in achieving the primary outcome. The sample size was calculated based on an expected rate of successful revascularization of 70% in patients treated with stent retrieversand assuming an absolute increase in successful revascularization of 15% with the contact aspiration strategy. This difference was based on published data on contact aspiration and on 2 nonrandomized studies comparing contact aspiration with stent retriever as first-line endovascular therapy. Assuming a rate of spontaneous revascularization and catheterization failures of 15%, a total of 380 patients (190 per group) was required.
Analyses were performed on all randomized patients in their assigned group according to the intention-to-treat principle. Categorical variables are reported as frequencies and percentages. Quantitative variables are reported as mean (standard deviation) or median (interquartile range [IQR]) for nonnormal distribution. Normality of distributions was assessed graphically and by using the Shapiro-Wilk test.
Rates of the primary outcome were compared between the 2 groups using a mixed logistic regression model adjusting for the randomization stratification variables by including IV thrombolysis as a fixed effect and center as a random effect. From this model, we derived an effect size measure, adjusted odds ratio (OR), and 95% confidence interval around the OR for contact aspiration relative to stent retriever. We also calculated absolute and relative risk differences from the marginal probabilities of successful revascularization, estimated by a mixed logistic regression model using the method described by Austin. For the primary outcome, missing values due to groin access failure (n = 4) were treated as failures (mTICI score of 0), and in cases of unavailable or poor-quality core laboratory images (n = 20), mTICI scores from the study site evaluation were used.
A sensitivity analysis was conducted in the per-protocol population, which was defined as all patients who received at least 3 attempts at successful revascularization with the assigned first-line endovascular treatment. An unplanned sensitivity analysis was conducted using the mTICI scores as graded by the study site for all patients. Treatment effect modification on the primary outcome was explored in prespecified subgroups: IV thrombolysis (yes vs no), location of thrombus (intracranial internal carotid artery vs M1 branch of the middle cerebral artery vs M2 branch of the middle cerebral artery) based on vascular imaging at time of admission, and clot burden score (<6 vs ≥6). An unplanned subgroup analysis was also conducted according to clot length (<8 vs ≥8 mm). Treatment effect size heterogeneity across the subgroups was tested by including the corresponding multiplicative interaction term into the mixed logistic regression model.
Further details on statistical analysis for secondary outcomes are available in the eAppendix in Supplement 2). All statistical tests were 2-sided, and P < .05 was considered statistically significant. No adjustment for multiple testing was applied and thus, all secondary objectives are considered exploratory. Data were analyzed using SAS software version 9.4 (SAS Institute Inc).
Results
Randomization and Baseline Characteristics
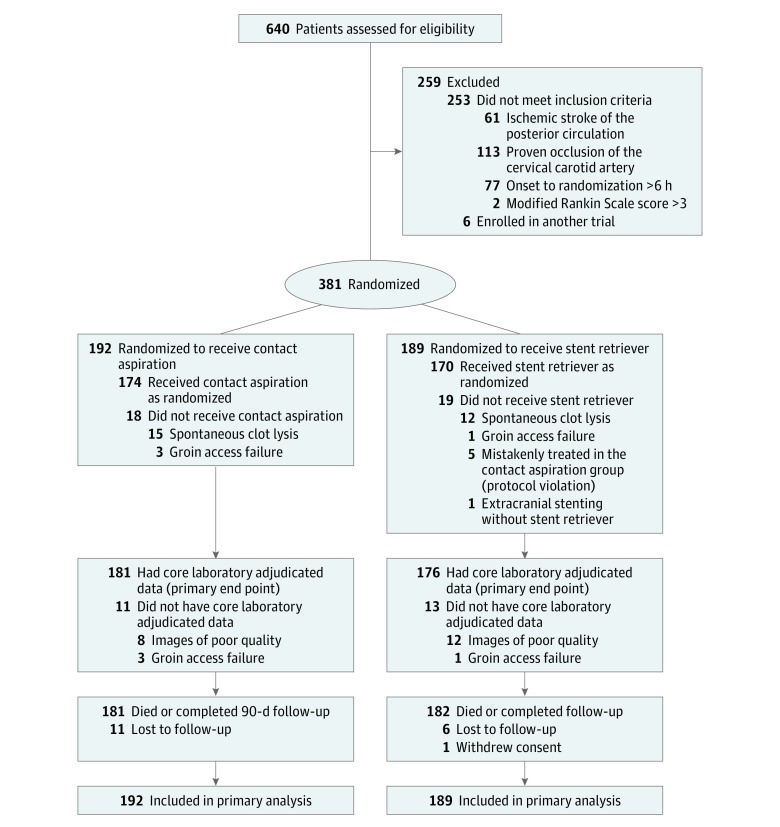
Between October 2015 and October 2016, a total of 381 patients (mean age, 69.9 [SD, 14.3] years; 207 men [54.3%]) were included in the intention-to-treat analysis (Figure 1). One hundred ninety-two patients were randomized to first-line treatment with contact aspiration and 189 to first-line treatment with a stent retriever. Details of device use are available in the eTable in Supplement 2.
Figure 1. Flow of Patients Through the ASTER Trial.
Among the 381 patients enrolled, the mean baseline NIHSS score was 16.2 (SD, 6.2) and the median time from symptom onset to arterial puncture was 227 minutes (IQR, 180-280 minutes). The 2 groups were well balanced regarding most of the baseline characteristics, except for age, admission systolic blood pressure, prestroke mRS score, and site of occlusion (Table 1).
Table 1. Baseline Characteristics of Patients.
| Characteristics | First-Line Contact Aspiration (n = 192) |
First-Line Stent Retriever (n = 189) |
|---|---|---|
| Baseline demographics and medical history | ||
| Age, mean (SD), y | 71.7 (13.8) | 68.1 (14.6) |
| Men, No./total (%) | 103/192 (53.7) | 104/189 (55.0) |
| Medical history, No./total (%) | ||
| Hypertension | 118/186 (63.4) | 111/187 (59.4) |
| Diabetes | 36/185 (19.5) | 40/188 (21.3) |
| Hypercholesterolemia | 65/184 (35.3) | 66/187 (35.3) |
| Current smoking | 31/158 (19.6) | 31/163 (19.0) |
| Coronary artery disease | 30/183 (16.4) | 33/186 (17.7) |
| Previous stroke or transient ischemic attack | 36/186 (19.4) | 29/188 (15.4) |
| Previous antithrombotic medications | 91/185 (49.2) | 91/187 (48.7) |
| Antiplatelets | 58/185 (31.4) | 60/187 (32.1) |
| Anticoagulants | 37/185 (20.0) | 35/187 (18.7) |
| Current stroke event | ||
| Systolic blood pressure, mean (SD), mm Hga | 150 (24) | 145 (26) |
| National Institutes of Health Stroke Scale (NIHSS) score, mean (SD)b | 16.3 (5.9) | 16.1 (6.5) |
| Prestroke modified Rankin Scale score, No./total (%)c | ||
| 0 | 158/190 (83.2) | 159/189 (84.1) |
| 1 | 17/190 (8.9) | 16/189 (8.5) |
| 2 | 5/190 (2.6) | 11/189 (5.8) |
| 3 | 8/190 (4.2) | 3/189 (1.6) |
| >3 | 2/190 (1.0) | 0 |
| ASPECTS, median (interquartile range)d | 7 (6-9) | 7 (5-9) |
| Site of occlusion, No./total (%)e | ||
| Middle cerebral artery branch M1 | 100/174 (57.5) | 104/176 (59.1) |
| Middle cerebral artery branch M2 | 48/174 (27.6) | 31/176 (17.6) |
| Intracranial internal carotid artery | 22/174 (12.6) | 33/176 (18.7) |
| Tandem lesionf | 4/174 (2.3) | 8/176 (4.6) |
| Clot burden score, median (interquartile range)g | 7 (5-8) | 6 (3-8) |
| Clot length, median (interquartile range), mmh | 13.0 (9.0-19.0) | 11.5 (8.0-18.0) |
| Arterial occlusion lesion score, No./total (%)i | ||
| 0 | 153/177 (86.4) | 160/175 (91.4) |
| 1 | 1/177 (0.6) | 2/175 (1.1) |
| 2 | 13/177 (7.3) | 8/175 (4.6) |
| 3 | 10/177 (5.7) | 5/175 (2.9) |
| Favorable collaterals, No./total (%)j | 37/146 (25.3) | 37/138 (26.8) |
| Suspected stroke cause, No./total (%) | ||
| Large artery atherosclerosis | 13/192 (6.8) | 17/189 (9.0) |
| Cardioembolic | 88/192 (45.8) | 75/189 (39.7) |
| Other or unknown | 91/192 (47.4) | 97/189 (51.3) |
| Directly admitted to a comprehensive stroke center, No./total (%) | 70/192 (36.5) | 68/189 (36.0) |
| Intravenous recombinant tissue plasminogen activator, No./total (%) | 126/192 (65.6) | 124/189 (65.6) |
| General anesthesia, No./total (%) | 21/191 (11.0) | 25/188 (13.3) |
| Onset to groin puncture time, median (interquartile range), mink | 217 (166-279) | 235 (186-283) |
| Onset to imaging | 109 (82-146) | 116 (85-150) |
| Imaging to randomization | 86 (43-132) | 82 (40-135) |
| Randomization to groin puncture | 11 (5-25) | 13 (5-23) |
There were 13 missing values (6 in the contact aspiration group).
The NIHSS classifies neurological deficit from 0 (no deficit) to 42 (most severe). There were 3 missing values (1 in the contact aspiration group).
Modified Rankin Scale score range: 0 (symptom free) to 6 (dead).
Alberta Stroke Program Early Computed Tomography Score (ASPECTS) measures the extension of stroke, with a score range of 0 to 10 (higher scores indicating fewer early ischemic changes). There were 5 missing values (1 in the contact aspiration group).
Assessed angiographically by an independent core laboratory (not available for spontaneous clot lysis, n = 27, or groin access failure, n = 4).
Tandem lesion involves an occlusion of the internal carotid artery at the bifurcation with an intracranial middle cerebral artery occlusion.
The clot burden score (range, 0-10; lower score indicates higher clot burden) is a semiquantitative imaging-based score that assesses the number of arterial segments exhibiting a visible clot, assessed by an independent core laboratory after excluding patients with poor-quality images, incomplete examinations, or nondetected clot (254 assessed values, 129 in the contact aspiration group).
Assessed by an independent core laboratory after excluding patients with poor-quality images, incomplete examinations, or nondetected clot (293 assessed values, 147 in the contact aspiration group).
The arterial occlusion lesion score ranges from 0 to 3 (0 indicates no revascularization of the primary occlusive lesion; 3, complete revascularization).
The collateral score ranges from 0 to 4 (0 indicates poor collateral supply; 4, good collateral supply) via an American Society of Interventional and Therapeutic Neuroradiology/Society of Interventional Radiology grading system. A favorable collateral score refers to grade 3-4.
There were 3 missing values (1 in the contact aspiration group).
Endovascular techniques were largely standardized (a balloon-guide catheter was used to allow proximal flow arrest during stent retriever removal in 92% of patients treated with the stent retriever technique).
Angiographic Efficacy Outcomes
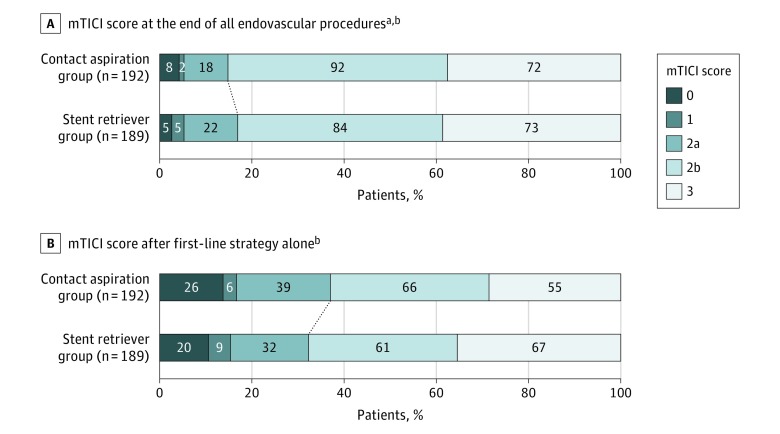
The primary outcome was assessed by the core laboratory in 357 patients (93.7%; 181 in the contact aspiration group and 176 in the stent retriever group). The primary efficacy outcome was not significantly different in the contact aspiration vs stent retriever groups (85.4% [n = 164] vs 83.1% [n = 157]; OR, 1.20; 95% CI, 0.68-2.10; P = .53) (Table 2). The corresponding risk difference was 2.4% (95% CI, −5.4% to 9.7%). The distribution of mTICI scores after all endovascular procedures is shown in Figure 2A. There were no significant between-group differences in the primary outcome in sensitivity analyses restricted to the per-protocol population or when successful revascularization was defined as mTICI score of 3 or mTICI score of 2c/3 (Table 2).
Table 2. Primary and Secondary Efficacy Outcomes.
| Outcomes | No./Total (%)a | Risk Difference, % (95% CI)b |
Odds Ratio (95% CI) |
P Value | |
|---|---|---|---|---|---|
| First-Line Contact Aspiration (n = 192) |
First-Line Stent Retriever (n = 189) |
||||
| Primary Efficacy Outcome | |||||
| Successful revascularization at the end of all procedures | |||||
| mTICI score of 2b or 3 assessed by core laboratoryc,d | |||||
| Intention-to-treat analysise | 164/192 (85.4) | 157/189 (83.1) | 2.4 (−5.4 to 9.7) | 1.20 (0.68-2.10) | .53 |
| Per-protocol analysis | 140/153 (91.5) | 140/165 (84.9) | 6.8 (−0.6 to 14.11) | 1.91 (0.93-3.91) | .08 |
| mTICI score of 2b or 3 assessed at study sited,f | 163/192 (84.9) | 163/189 (86.2) | −1.4 (−8.3 to 5.5) | 0.90 (0.50-1.59) | .71 |
| Secondary Angiographic Efficacy Outcomes | |||||
| Complete revascularization at the end of all procedures | |||||
| mTICI score of 3 assessed by core laboratoryd | 72/192 (37.5) | 73/189 (38.6) | −1.1 (−11.0 to 9.0) | 0.95 (0.62-1.45) | .82 |
| mTICI score of 2c or 3 assessed by core laboratoryd | 108/192 (56.3) | 107/189 (56.6) | 0.4 (−10.9 to 9.7) | 0.99 (0.65-1.48) | .84 |
| Successful revascularization after first-line strategy alone | |||||
| mTICI score of 2b or 3 assessed by core laboratoryd | 121/192 (63.0) | 128/189 (67.7) | −4.7 (−13.8 to 4.4) | 0.81 (0.53-1.24) | .34 |
| mTICI score of 3 assessed by core laboratoryd | 55/192 (28.7) | 67/189 (35.5) | −6.8 (−16.2 to 2.5) | 0.73 (0.54-1.13) | .16 |
| mTICI score of 2c or 3 assessed by core laboratoryd | 83/192 (43.2) | 94/189 (49.7) | −6.5 (−16.4 to 3.3) | 0.77 (0.51-1.16) | .21 |
| Use of rescue treatment | 63/192 (32.8) | 45/189 (23.8) | 9.0 (−0.9 to 18.1) | 1.57 (0.99-2.47) | .05 |
| Clinical Efficacy Outcomes | |||||
| Change in NIHSS score at 24 h, mean (95% CI)g |
−4.8 (−6.1 to −3.6)h | −5.2 (−6.5 to −3.9)h | 0.38 (−1.42 to 2.18)i | NA | .68 |
| Functional independence at 3 moj | 82/181 (45.3) | 91/182 (50.0) | −4.6 (−14.7 to 6.1) | 0.83 (0.54-1.26) | .38 |
| Modified Rankin Scale score at 3 mo, median (interquartile range) | 3.0 (1.0 to 5.0) | 2.5 (1.0 to 5.0) | NA | 0.76 (0.53-1.10)k | .15 |
Abbreviations: mTICI, modified Treatment in Cerebral Infarction; NA, not applicable; NIHSS, National Institutes of Health Stroke Scale.
Values expressed as No./total No. (%) unless otherwise indicated. Effect sizes were calculated after adjustment for randomization stratification variables (center and intravenous thrombolysis).
Expressed as a percentage and calculated from the marginal probabilities accordingly to the Austin method unless otherwise indicated.
Eleven patients in the contact aspiration group and 13 in the stent retriever group were not assessed by the core laboratory because of groin access failure or unavailable or poor-quality images.
mTICI score: 0, no perfusion or anterograde flow beyond site of occlusion; 1, penetration but not perfusion (contrast penetration exists past the initial obstruction but with minimal filling of the normal territory); 2, incomplete perfusion wherein the contrast passes the occlusion and opacifies the distal arterial bed but rate of entry or clearance from the bed is slower or incomplete compared with noninvolved territories; 2a, some perfusion with distal branch filling of <50% of territory visualized; 2b, substantial perfusion with distal branch filling of ≥50% of territory visualized; 2c, near-complete perfusion except for slow flow in a few distal cortical vessels or presence of small distal cortical emboli; and 3, complete perfusion with normal filling of all distal branches.
Prespecified as the primary efficacy analysis.
Unplanned sensitivity analysis.
There were 23 missing 24-hour NIHSS values (12 in the contact aspiration group).
Mean change (95% CI) adjusted on baseline NIHSS score.
Mean risk difference adjusted on baseline NIHSS score.
Defined as a modified Rankin Scale score ≤2.
Common odds ratio of improvement of 1 point in modified Rankin Scale score.
Figure 2. Modified Treatment in Cerebral Infarction (mTICI) Scores at the End of All Endovascular Procedures and After First-Line Strategy Alone.
Scores indicate the following: 0 (no revascularization), no perfusion or anterograde flow beyond site of occlusion; 1 (minimal revascularization), contrast passes the area of occlusion but fails to opacify the entire cerebral bed distal to the obstruction during angiographic run; 2 (partial revascularization), 2a, partial filling (<50%) of territory visualized, and 2b, partial filling (≥50%) of territory visualized; 3 (complete revascularization), complete revascularization with normal filling.
aPrimary outcome.
bAssessed by core laboratory. Missing data due to groin access failure (n = 4) were treated as failures (mTICI score of 0) and missing data due to no core laboratory reading (n = 20 for mTICI score at end of all procedures and n = 22 for mTICI score after first-line procedure) were replaced by the study site evaluation regardless of treatment groups.
After first-line strategy only, there were no significant differences between groups in revascularization rates (Figure 2B and Table 2). Rescue treatment after first-line strategy occurred in 63 patients (32.8%) in the contact aspiration group and 45 patients (23.8%) in the stent retriever group, with no significant difference between groups (OR, 1.57; 95% CI, 0.99-2.47; P = .05). Among the 119 patients (68 contact aspiration and 51 stent retriever) with failure of first-line therapy (defined as mTICI score of 0/1/2a graded at the time of procedure by operator), rescue treatment was used in 57 patients (83.8%) in the contact aspiration group and 42 patients (82.4%) in the stent retriever group (OR, 1.21; 95% CI, 0.43-3.38; P = .72).
There was no significant difference in the total number of revascularization attempts, with a median of 2 (IQR, 1-4; range, 0-11) in the contact aspiration group and 2 (IQR, 1-3; range, 0-15) in the stent retriever group (P = .84).
Among patients reaching the primary outcome, the median time from arterial puncture to revascularization was 38 minutes (IQR, 24-60 minutes) in the contact aspiration group and 45 minutes (IQR, 31-60 minutes) in the stent retriever group (P = .10).
Clinical Efficacy Outcomes
Early improvement in neurological outcomes was not significantly different between the 2 groups, with a mean change in NIHSS score at 24 hours of −4.8 points (95% CI, −6.1 to −3.6) in the contact aspiration group and −5.2 points (95% CI, −6.5 to −3.9) in the stent retriever group (mean difference, 0.38; 95% CI, −1.42 to 2.18; P = .68). Among 363 patients (95.3%) with mRS assessments at 3 months, no significant difference was found in the proportion who were functionally independent (45.3% in the contact aspiration group vs 50.0% in the stent retriever group; OR, 0.83 [95% CI, 0.54-1.26]; P = .38; risk difference, −4.6% [95% CI, −14.7% to 6.1%]) (Table 2). There was no significant shift in the mRS distribution in favor of the contact aspiration strategy, with a common OR for a 1-point improvement of 0.76 (95% CI, 0.53-1.10; P = .15) (eFigure 1 in Supplement 2; Table 2).
Adverse Events
All-cause mortality at 3 months occurred in 70 patients (19.3%). Intracranial hemorrhage at 24 hours was observed in 87 patients (46.3%) in the contact aspiration group and 85 patients (46.2%) in the stent retriever group; the types of hemorrhage are detailed in Table 3. Symptomatic intracranial hemorrhage occurred in 10 patients (5.3%) in the contact aspiration group and 12 patients (6.5%) in the stent retriever group. Procedure-related adverse events occurred in 31 patients (16.2%) in the contact aspiration group and 30 patients (15.9%) in the stent retriever group. The most frequent event was subarachnoid hemorrhage (n=26), followed by vasospasm (n = 17), embolization in a new vascular territory (n = 12), arterial perforation (n = 8), and arterial dissection (n = 7). New ischemic stroke in a different vascular territory occurred in 10 patients (5.3%) in the contact aspiration group and 16 (8.5%) in the stent retriever group.
Table 3. Adverse Events.
| Events | No./Total (%) | |
|---|---|---|
| First-Line Contact Aspiration (n = 192) |
First-Line Stent Retriever (n = 189) |
|
| All-cause mortality at 3 mo | 35/181 (19.3) | 35/182 (19.2) |
| Intracranial hemorrhage at 24 ha,b | 87/188 (46.3) | 85/188 (46.2) |
| Hemorrhagic infarction | 58/188 (30.9) | 49/188 (26.6) |
| Type 1c | 23/188 (12.2) | 24/188 (13.0) |
| Type 2d | 35/188 (18.6) | 25/188 (13.6) |
| Parenchymal hematoma | 24/188 (12.8) | 33/188 (17.4) |
| Type 1e | 17/188 (9.0) | 19/188 (10.3) |
| Type 2f | 7/188 (3.7) | 14/188 (7.6) |
| Intraventricular hemorrhage | 6/188 (3.2) | 2/184 (1.1) |
| Remote intracranial hemorrhage | 1/188 (0.5) | 1/184 (0.5) |
| Symptomatic intracranial hemorrhage at 24 h | 10/188 (5.3) | 12/188 (6.5) |
| Procedure-related adverse eventsb | 31/192 (16.2) | 30/189 (15.9) |
| Embolization in a new vascular territory | 7/192 (3.7) | 5/189 (2.7) |
| Arterial perforation | 5/192 (2.6) | 3/189 (1.6) |
| Arterial dissection | 5/192 (2.6) | 2/189 (1.1) |
| Vasospasm | 5/192 (2.6) | 12/189 (6.4) |
| Subarachnoid hemorrhage | 13/188 (6.9) | 13/188 (7.1) |
| New ischemic stroke in a different vascular territory | 10/188 (5.3) | 16/188 (8.5) |
Assessed by core laboratory.
Patients with multiple events of one type were counted once.
Isolated petechiae in infarcted tissue without mass effect.
Confluent petechiae in infarcted tissue without mass effect.
Hemorrhage in <30% of the infarcted area with mild space-occupying effect.
Hemorrhage in >30% of the infarcted area with significant space-occupying effect.
Subgroup Analyses
Prespecified exploratory subgroup analyses (IV tPA treatment, site of occlusion, clot burden score) showed no significant heterogeneity in treatment effect on the primary outcome across the studied subgroups (eFigure 2 in Supplement 2).
Unplanned Analyses
In exploratory analyses of the primary outcome that were not prespecified, there was no heterogeneity of treatment effect in a subgroup analysis by clot length and no significant between-group differences in a sensitivity analysis using mTICI scores from local study sites. A significantly shorter time from clot contact to revascularization was observed in the contact aspiration group (median, 13 minutes; IQR, 6-38 minutes) compared with the stent retriever group (median, 22 minutes; IQR, 10-38 minutes; P = .03), but this was not a prespecified outcome and should be considered exploratory.
Discussion
In this multicenter RCT, 381 patients with acute ischemic stroke and large vessel occlusion were randomized to undergo either contact aspiration or stent retriever as first-line endovascular treatment. First-line contact aspiration was not superior to first-line stent retriever in achieving successful revascularization at the end of the endovascular procedure.
To our knowledge, this is the first open-label RCT with blinded end-point evaluation to compare first-line contact aspiration vs stent retriever for mechanical thrombectomy in acute ischemic stroke. Patients were enrolled across 8 comprehensive stroke centers, with very few restrictive inclusion criteria in keeping with clinical situations. The use of an independent imaging core laboratory reduced bias in evaluation of the primary outcome, and the short period in which patient enrollment was completed reduced potential bias in a field in which technological progress and refinement evolve rapidly. The endovascular techniques were largely standardized in both groups, patients in the stent retriever group were primarily treated with validated devices, and there were few crossovers (90% of patients received the allocated treatment).
The primary outcome for this study was the difference in revascularization rates after all procedures. Revascularization rate was chosen as the primary outcome because it is a major early indicator of treatment success, has been correlated with good clinical outcome, and has been used as a primary outcome in other stroke trials comparing thrombectomy devices; eg, SWIFT and TREVO2. The primary outcome was assessed at the end of all procedures because the goal of the study was to assess the effect of first-line endovascular strategy on revascularization after the entire procedure rather than to directly compare the contact aspiration and stent retriever techniques when used alone.
Successful revascularization was specifically defined as an mTICI score of 2b or 3 in this study because this outcome has been reported to be a predictor of clinical outcome. Theoretically, contact aspiration could result in a higher rate of an mTICI score of 3 compared with stent retriever because use of a stent retriever requires that it be passed through the clot and therefore might result in a higher rate of distal emboli (as was found in an in vitro study), but there were no significant differences between groups in the secondary outcome of an mTICI score of 3 or in the frequency of embolization to a new vascular territory in this study.
Contact aspiration and stent retriever were never used simultaneously during the first-line strategy, as this was not allowed in the study protocol. However, during rescue therapy, the choice of the technique was left to the discretion of the operator, and there were 2 instances of combined use of contact aspiration plus stent retriever in the contact aspiration group and 8 instances in the stent retriever group. The effect of combining contact aspiration and stent retriever to obtain a better rate of recanalization, especially perfect recanalization, has never been studied in an RCT and is a potential area of future study.
The hypothesis of this trial was that use of first-line contact aspiration would increase the rate of successful revascularization by 15% compared with a first-line stent retriever (superiority design), so, although contact aspiration was not superior to stent retriever in achieving successful recanalization, this study was not designed to claim equivalence or noninferiority of these strategies. Furthermore, although the contact aspiration group did not achieve a 15% increase in successful revascularization, a smaller yet potentially clinically significant difference in revascularization rate cannot be fully excluded.
Regarding secondary clinical outcomes and adverse events, there were no significant differences between groups, although the trial was not powered to assess differences in these outcomes. A retrospective study comparing aspiration and stent retriever techniques reported a lower rate of symptomatic hemorrhages for contact aspiration compared with stent retriever (2.9% for contact aspiration and 5.4% for stent retriever),and retrospective studies have reported low rates of embolization in a new territory (2%) and no incidence of symptomatic intracranial hemorrhage when using contact aspiration. Embolization in a different vascular territory occurred in 3.7% of the contact aspiration group in this study, which is less than the rates of 6% and 5.7% reported in 2 recent retrospective studies. Adverse events in the retrospective analyses were site reported, while in this trial, they were adjudicated in a blinded manner.
Limitations
This study has several limitations. First, the primary end point was technical (ie, successful revascularization after all interventions), which is less relevant than a clinical outcome such as the 90-day mRS score. Second, given its superiority design to detect a 15% difference in the primary end point, this trial was not designed to establish noninferiority between contact aspiration and stent retriever as first-line endovascular strategies and not powered to detect a smaller yet potentially clinically important difference between groups. Third, the use of rescue therapy was at the discretion of the operator and is a potential source of bias, although the rates of rescue therapy were not significantly different between groups overall or among those who experienced failure after first-line thrombectomy. Fourth, participating centers were all highly experienced in performing both endovascular techniques, which may explain the high mTICI 2b/3 score rates in both study groups and may limit the ability to generalize these findings to other comprehensive stroke centers with less experience in these techniques. Fifth, although the 2 groups were well balanced for most of the baseline characteristics, the degree of randomness was limited by using the stratified permuted randomization with fixed blocks of 4 in light of the sample size and number of strata. Sixth, although exploratory subgroup analyses showed no heterogeneity in treatment effect across the studied subgroups for the primary outcome, these results should be interpreted with caution given that the study was not designed to have adequate power for subgroup analyses.
Conclusions
Among patients with ischemic stroke in the anterior circulation undergoing thrombectomy, first-line thrombectomy with contact aspiration vs stent retriever did not result in a higher successful revascularization rate at the end of the procedure.
Trial Protocol
eAppendix. Supplemental Methods
eTable. Details of the Revascularization Devices Used in the ASTER Trial
eFigure 1. Distribution of Modified Rankin Scale Scores at 3 Months
eFigure 2. Treatment Effect Size (Aspiration vs. Stent Retriever) on Primary Outcomes According to Key Subgroups
References
- 1.European Stroke Organisation; European Society for Minimally Invasive Neurological Therapy; European Society of Neuroradiology Consensus statement on mechanical thrombectomy in acute ischemic stroke. 2014. http://2014.strokeupdate.org/sites/default/files/Consensus_thrombectomy_ESO_Karolinska_ESMINT_ESNR_final.pdf. Accessed July 13, 2016.
- 2.Goyal M, Menon BK, van Zwam WH, et al. ; HERMES Collaborators . Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from 5 randomised trials. Lancet. 2016;387(10029):1723-1731. [DOI] [PubMed] [Google Scholar]
- 3.Powers WJ, Derdeyn CP, Biller J, et al. ; American Heart Association Stroke Council . 2015 American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015;46(10):3020-3035. [DOI] [PubMed] [Google Scholar]
- 4.Blanc R, Fahed R, Redjem H, Bartolini B, Pistocchi S, Piotin M. Single center experience with the ADAPT technique for acute ischemic stroke [abstract P-031]. J Neurointerv Surg. 2014;6(suppl 1):A37. [Google Scholar]
- 5.Kabbasch C, Möhlenbruch M, Stampfl S, Mpotsaris A, Behme D, Liebig T. First-line lesional aspiration in acute stroke thrombectomy using a novel intermediate catheter: initial experiences with the SOFIA. Interv Neuroradiol. 2016;22(3):333-339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kowoll A, Weber A, Mpotsaris A, Behme D, Weber W. Direct aspiration first pass technique for the treatment of acute ischemic stroke: initial experience at a European stroke center. J Neurointerv Surg. 2016;8(3):230-234. [DOI] [PubMed] [Google Scholar]
- 7.Lapergue B, Blanc R, Guedin P, et al. . A direct aspiration, first pass technique (ADAPT) vs stent retrievers for acute stroke therapy: an observational comparative study. AJNR Am J Neuroradiol. 2016;(10):1860-1865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Turk AS, Frei D, Fiorella D, et al. . ADAPT FAST study: a direct aspiration first pass technique for acute stroke thrombectomy. J Neurointerv Surg. 2014;6(4):260-264. [DOI] [PubMed] [Google Scholar]
- 9.Turk AS, Turner R, Spiotta A, et al. . Comparison of endovascular treatment approaches for acute ischemic stroke: cost effectiveness, technical success, and clinical outcomes. J Neurointerv Surg. 2015;7(9):666-670. [DOI] [PubMed] [Google Scholar]
- 10.Stapleton CJ, Torok CM, Patel AB. Noninferiority of a direct aspiration first-pass technique vs stent retriever thrombectomy in emergent large-vessel intracranial occlusions. Neurosurgery. 2016;63(suppl 1):146-147. [DOI] [PubMed] [Google Scholar]
- 11.Lapergue B, Labreuche J, Blanc R, et al. ; ASTER Trial Investigators . First-line use of contact aspiration for thrombectomy vs a stent retriever for recanalization in acute cerebral infarction: the randomized ASTER study protocol [published online January 1, 2017]. Int J Stroke. doi: 10.1177/1747493017711948 [DOI] [PubMed] [Google Scholar]
- 12.World Medical Association World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191-2194. [DOI] [PubMed] [Google Scholar]
- 13.Wahlgren N, Moreira T, Michel P, et al. ; ESO-KSU; ESO; ESMINT; ESNR; EAN . Mechanical thrombectomy in acute ischemic stroke: consensus statement by ESO-Karolinska Stroke Update 2014/2015, supported by ESO, ESMINT, ESNR and EAN. Int J Stroke. 2016;11(1):134-147. [DOI] [PubMed] [Google Scholar]
- 14.Turk AS, Spiotta A, Frei D, et al. . Initial clinical experience with the ADAPT technique: a direct aspiration first pass technique for stroke thrombectomy. J Neurointerv Surg. 2014;6(3):231-237. [DOI] [PubMed] [Google Scholar]
- 15.Tomsick T, Broderick J, Carrozella J, et al. ; Interventional Management of Stroke II Investigators . Revascularization results in the Interventional Management of Stroke II trial. AJNR Am J Neuroradiol. 2008;29(3):582-587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Savitz SI, Lew R, Bluhmki E, Hacke W, Fisher M. Shift analysis versus dichotomization of the modified Rankin Scale outcome scores in the NINDS and ECASS-II trials. Stroke. 2007;38(12):3205-3212. [DOI] [PubMed] [Google Scholar]
- 17.Delgado Almandoz JE, Kayan Y, Young ML, et al. . Comparison of clinical outcomes in patients with acute ischemic strokes treated with mechanical thrombectomy using either Solumbra or ADAPT techniques. J Neurointerv Surg. 2016;8(11):1123-1128. [DOI] [PubMed] [Google Scholar]
- 18.Chevreul K, Durand-Zaleski I, Gouépo A, Fery-Lemonnier E, Hommel M, Woimant F. Cost of stroke in France. Eur J Neurol. 2013;20(7):1094-1100. [DOI] [PubMed] [Google Scholar]
- 19.Austin PC. Absolute risk reductions, relative risks, relative risk reductions, and numbers needed to treat can be obtained from a logistic regression model. J Clin Epidemiol. 2010;63(1):2-6. [DOI] [PubMed] [Google Scholar]
- 20.Dargazanli C, Consoli A, Barral M, et al. . Impact of modified TICI 3 vs modified TICI 2b reperfusion score to predict good outcome following endovascular therapy. AJNR Am J Neuroradiol. 2017;38(1):90-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Saver JL, Jahan R, Levy EI, et al. ; SWIFT Trialists . Solitaire With the Intention for Thrombectomy (SWIFT) trial: design of a randomized, controlled, multicenter study comparing the Solitaire flow restoration device and the Merci retriever in acute ischaemic stroke. Int J Stroke. 2014;9(5):658-668. [DOI] [PubMed] [Google Scholar]
- 22.Nogueira RG, Lutsep HL, Gupta R, et al. ; TREVO 2 Trialists . Trevo vs Merci retrievers for thrombectomy revascularisation of large vessel occlusions in acute ischaemic stroke (TREVO 2): a randomised trial. Lancet. 2012;380(9849):1231-1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kleine JF, Wunderlich S, Zimmer C, Kaesmacher J. Time to redefine success? TICI 3 vs TICI 2b recanalization in middle cerebral artery occlusion treated with thrombectomy. J Neurointerv Surg. 2017;9(2):117-121. [DOI] [PubMed] [Google Scholar]
- 24.Suh SH, Cloft HJ, Fugate JE, Rabinstein AA, Liebeskind DS, Kallmes DF. Clarifying differences among thrombolysis in cerebral infarction scale variants: is the artery half open or half closed? Stroke. 2013;44(4):1166-1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mokin M, Setlur Nagesh SV, Ionita CN, Levy EI, Siddiqui AH. Comparison of modern stroke thrombectomy approaches using an in vitro cerebrovascular occlusion model. AJNR Am J Neuroradiol. 2015;36(3):547-551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Blanc RRH, Ciccio G, Smajda S, et al. . Predictors of the aspiration component success of a direct aspiration first pass technique (ADAPT) for the endovascular treatment of stroke reperfusion strategy in anterior circulation acute stroke. Stroke. 2017;48(6):1588-1593. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol
eAppendix. Supplemental Methods
eTable. Details of the Revascularization Devices Used in the ASTER Trial
eFigure 1. Distribution of Modified Rankin Scale Scores at 3 Months
eFigure 2. Treatment Effect Size (Aspiration vs. Stent Retriever) on Primary Outcomes According to Key Subgroups