Abstract.
The authors describe a multiinstitutional collaborative project to address a gap in global health training by creating a free online platform to share a curriculum for performing procedures in resource-limited settings. This curriculum called PEARLS (Procedural Education for Adaptation to Resource-Limited Settings) consists of peer-reviewed instructional and demonstration videos describing modifications for performing common pediatric procedures in resource-limited settings. Adaptations range from the creation of a low-cost spacer for inhaled medications to a suction chamber for continued evacuation of a chest tube. By describing the collaborative process, we provide a model for educators in other fields to collate and disseminate procedural modifications adapted for their own specialty and location, ideally expanding this crowd-sourced curriculum to reach a wide audience of trainees and providers in global health.
As interest in global health (GH) continues to grow, more providers are spending time participating in clinical care in resource-limited settings both in training and as part of their postgraduate careers.1–3 Proper preparation for these experiences is essential to reduce harm to patients and optimize provider and partner collaboration.4,5 Yet while predeparture preparatory curriculum has become increasingly common in graduate medical education, it is far from universal and less commonly available to practitioners who have already completed their training.1,6 Many of the existing preparatory curricula have focused on addressing knowledge gaps within tropical medicine and creating an awareness of the challenges of working across cultures.7,8 Less has been done to formally prepare trainees for the emotional and technical obstacles of working in resource-limited settings, or equip them with practical solutions to address some of these resource limitations.9,10
In 2013, a group of educators from the Midwest Consortium (MWC) of Global Child Health Educators attempted to address some of these gaps in GH preparatory curricula by developing and evaluating a standardized simulation-based curriculum to prepare learners for the emotional challenges of GH experiences called Simulation Use for Global Away Rotations (SUGAR).10 This curriculum is open source with training videos and downloadable materials available for free at sugarprep.org11 By participating in simulation scenarios that mimic the challenges of working in resource-limited settings, providers experience many of the emotions encountered when faced with obstacles common to these settings (frustration, floundering, failure, and futility) and have the opportunity to debrief and develop adaptive characteristics prior to travel.
Although we have found SUGAR to be valuable in our preparation of residents—most notably in creating an awareness of the “knowledge” and “attitudes” necessary for work in resource-limited settings10,12,13—there still remained a gap in the preparatory curricula regarding the acquisition of “skills.” Providers practicing in resource-limited settings may find themselves in situations where a procedure is indicated but despite their competency in the procedure in their home environment, they feel unprepared to perform the procedure with the supplies available in a setting with significantly limited resources. There is a wealth of experience in the global medical community at creating adaptive low-tech modifications to procedures necessary in these settings, yet there is a lack of a structured curriculum addressing these common procedural adaptations. Although some low-tech solutions are increasingly well known, such as the creation of a bubble continuous positive airway pressure (bubble CPAP) device using a water bottle and oxygen source,14,15 we were unable to find a collective source for procedural modifications for use in resource-limited settings.
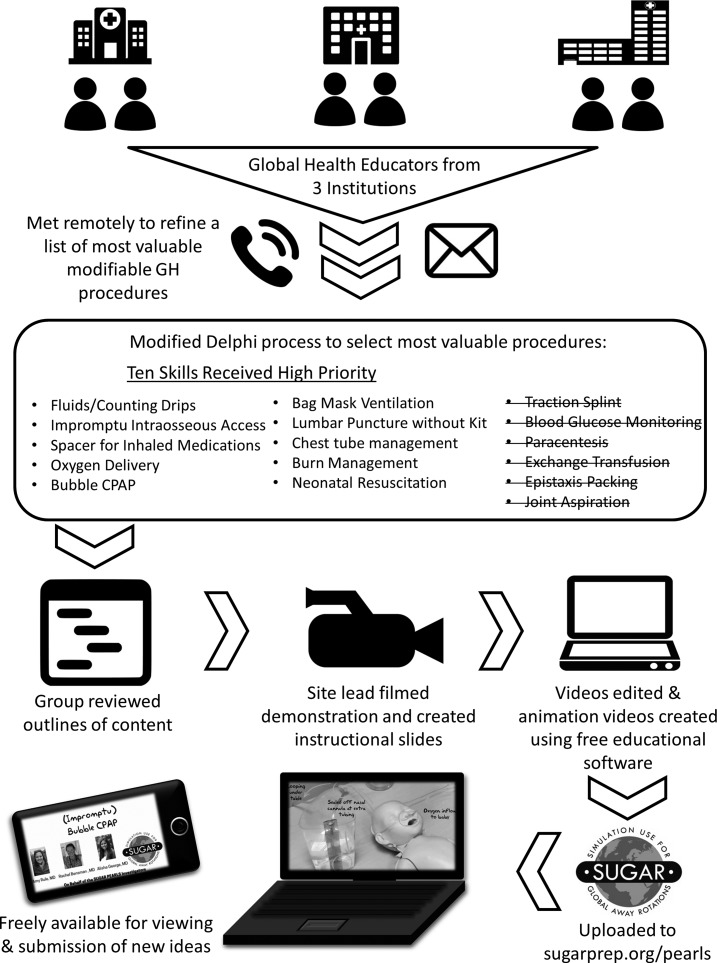
In 2015, we aimed to leverage the collective experience of the MWC that created SUGAR to create a free, dynamic online platform for vetting and disseminating video training of adaptations for common pediatric procedures. We were explicit in our mission from the outset that each video would not be intended for comprehensive procedural instruction but would instead target learners already competent with the high-resource version of the skill to give specific tips about performing the procedure without access to the supplies they may be accustomed to using. We called this curriculum Procedural Education for Adaptation to Resource-Limited Settings (PEARLS). The stepwise process of curating and refining the content, creating the videos, and vetting, is summarized in Figure 1 and described here. A workgroup with representatives from three institutions in the MWC developed a list of procedures and then ranked these based on clinical importance, frequency of expected use, ability to practice prior to travel, and ability to make a low-tech resource modification if needed. Procedures for the initial curriculum were selected by a modified Delphi process to narrow 16 suggested procedures down to 10. Procedures that were included ranged from those with a minor modification (e.g., using a nonspinal needle for a lumbar puncture) to more complex adaptations such as the creation of a water-based vacuum chamber for chest tube evacuation. Table 1 summarizes the initial 10 procedures covered in the PEARLS curriculum with a description of the modifications described for each.
Figure 1.
Process of PEARLS (Procedural Education for Adaptation to Resource-Limited Settings) curriculum development.
Table 1.
Procedures and modifications
| Procedure | Description |
|---|---|
| Bag-valve-mask ventilation | Provides an overview of bag-valve-mask ventilation and describes potential modifications if appropriate mask size or preferred oxygen source is unavailable |
| Bubble CPAP | Outlines creation of a low-cost model using nasal cannula, water container, and compressed air source16 |
| Burns and wound care | Describes basic burn care including low-cost substitutes for burn dressings and commercial antiseptic agents |
| Chest tube drainage system with bonus construction of procedural simulation model | Demonstrates creation of one-, two-, and three-chamber drainage systems in absence of commercial product. Also describes the creation of a model for teaching chest tube placement using animal ribs |
| Spacer for inhaled medications | Demonstrates creation of a spacer from a drink bottle17 |
| IO access | Shows modification of a standard 16 or 18 gauge needle with needle cover for use as an IO needle |
| IV fluid infusion | Describes how to prepare IV fluid infusions and administer correct volume and rate of fluids when an IV pump is not available |
| Lumbar puncture | Reviews lumbar puncture technique and describes modifications when no spinal needle or commercial kit is available |
| Neonatal resuscitation | Highlights the key steps of neonatal resuscitation using Helping Babies Breathe model18 |
| Oxygen delivery | Demonstrates various ways to deliver oxygen in low resource settings |
CPAP = continuous positive airway pressure; IO = intraosseous; IV = intravenous.
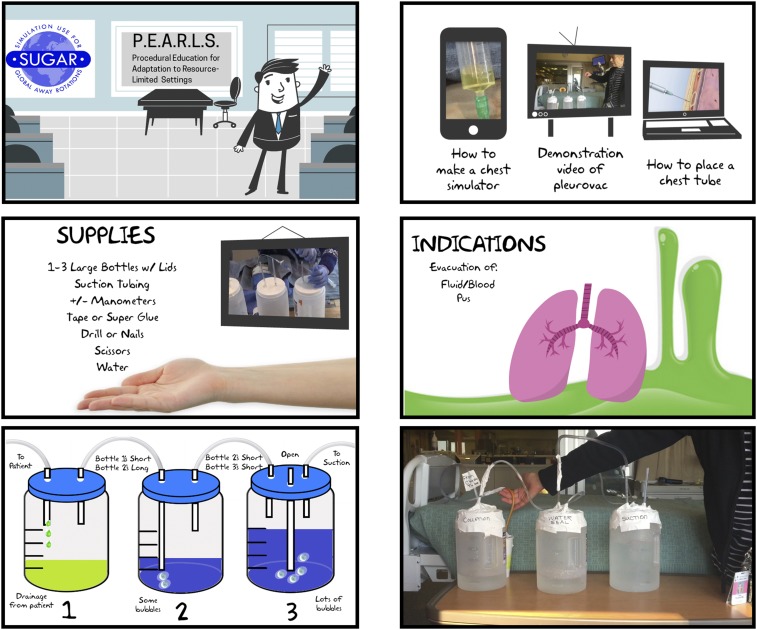
We identified content experts among the workgroup for development of each procedure’s training videos, which included both an animated instructional video with photos of supplies, diagrams of any set-up needed, and discussion of indications and complications, as well as a live-action demonstration video of the procedural modification. Each video begins with a reminder to the user addressing its limitations as an adjunctive tool to increase the user’s ability to solve problems when facing situations without the resources he or she is accustomed to having, rather than teaching specifics of the medical management. Members of the MWC reviewed all videos prior to publication online. PEARLS was launched publicly at the Association of Pediatric Program Directors Annual Spring meeting in April 2016 and is available at sugarprep.org/pearls.11 Since that time, the videos have been collectively been viewed 1853 times. Figure 2 includes representative screenshots from the PEARLS videos.
Figure 2.
Screenshots from PEARLS (Procedural Education for Adaptation to Resource-Limited Settings) Chest Tube drainage system instructional and demonstration videos. This figure appears in color at www.ajtmh.org.
A core principle of the initial SUGAR project and its subsequent offshoots has been to make GH preparatory content available for free immediately and indefinitely. This approach allows the content to get into the hands of the end users faster and opens pathways for future collaboration, real-time feedback, evaluation, and modification. Sharing the initial SUGAR curriculum in this manner led to rapid expansion with facilitators trained from more than 120 institutions in nine countries in 3 years, with several spin-off projects (including PEARLS) being led by over thirty collaborators at more than a dozen institutions.13 Our goal is to share PEARLS with providers in specialties beyond pediatrics as a prototype-to-production model to collate and disseminate procedural modifications specific to their own fields and resource-limited settings, as well as to invite future collaborators with skills to share to help expand this crowd-sourced curriculum.
Acknowledgment:
We would like to thank Dr. Ainhoa Costas-Chavarri for sharing the chest tube evacuation system model and for all health care providers working in low-resource settings for their suggestions as well.
SUGAR PEARLS Investigators: Amanda Becker, Brinda Desai, Alisha George, Scott Hagen, Andrew Kiragu, Ron Johannsen, Kathleen Miller, Amy Rule, and Sarah Webber.
REFERENCES
- 1.Butteris SM,, et al. 2015. Global health education in US pediatric residency programs. Pediatrics 136: 458–465. [DOI] [PubMed] [Google Scholar]
- 2.Greysen SR, Richards AK, Coupet S, Desai MM, Padela AI, 2013. Global health experiences of U.S. Physicians: a mixed methods survey of clinician-researchers and health policy leaders. Global Health 9: 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Drain PK, Holmes KK, Skeff KM, Hall TL, Gardner P, 2009. Global health training and international clinical rotations during residency: current status, needs, and opportunities. Acad Med 84: 320–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Crump JA,, et al. 2010. Ethics and best practice guidelines for training experiences in global health. Am J Trop Med Hyg 83: 1178–1182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Balmer DF, Marton S, Gillespie SL, Schutze GE, Gill A, 2015. Reentry to pediatric residency after global health experiences. Pediatrics 136: 680–686. [DOI] [PubMed] [Google Scholar]
- 6.Tupesis JP, Babcock C, Char D, Alagappan K, Hexom B, Kapur GB, 2012. Optimizing global health experiences in emergency medicine residency programs: a consensus statement from the Council of Emergency Medicine Residency Directors 2011 Academic Assembly global health specialty track. Int J Emerg Med 5: 43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.De Cortina SH, Arora G, Wells T, Hoffman RM, 2016. Evaluation of a structured predeparture orientation at the david geffen school of medicine’s global health education programs. Am J Trop Med Hyg 94: 563–567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schwartz K, Prentiss K, 2015. Simulation in pre-departure training for residents planning clinical work in a low-income country. West J Emerg Med 16: 1666–1672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Margolick J, Kanters D, Cameron BH, 2015. Procedural skills training for Canadian medical students participating in international electives. Can Med Educ J 6: e23–e33. [PMC free article] [PubMed] [Google Scholar]
- 10.Butteris SM, Gladding SP, Eppich W, Hagen SA, Pitt MB, 2014. Simulation Use for Global Away Rotations (SUGAR): preparing residents for emotional challenges abroad—a multicenter study. Acad Pediatr 5: 533–541. [DOI] [PubMed] [Google Scholar]
- 11.Butteris SM, Pitt MB. SUGAR Curriculum Available at: www.sugarprep.org. Accessed February 26, 2016.
- 12.Rosenman JR, Fischer PR, Arteaga GM, Hulyalkar M, Butteris SM, Pitt MB, 2016. Global health simulation during residency. Glob Pediatr Heal 3: 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pitt MB, Gladding SP, Butteris SM, 2016. Using simulation for global health preparation. Pediatrics 137: 1–4. [DOI] [PubMed] [Google Scholar]
- 14.Brown J,, et al. 2013. A high-value, low-cost bubble continuous positive airway pressure system for low-resource settings: technical assessment and initial case reports. PLoS One 8: 6–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kawaza K, Machen HE, Brown J, Mwanza Z, Iniguez S, Gest A, Smith EOB, Oden M, Richards-Kortum RR, Molyneux E, 2014. Efficacy of a low-cost bubble CPAP system in treatment of respiratory distress in a neonatal ward in Malawi. PLoS One 9: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Health Organization, 2016. Bubble CPAP. Oxygen Therapy for Children. Geneva, Switzerland: World Health Organization, 34–37. [Google Scholar]
- 17.Zar HJ, Brown G, Donson H, Brathwaite N, Mann MD, Weinberg EG, 1999. Home-made spacers for bronchodilator therapy in children with acute asthma: a randomised trial. Lancet 354: 979–982. [DOI] [PubMed] [Google Scholar]
- 18.American Academy of Pediatrics, 2011. Guide for Implementation of Helping Babies Breathe® (HBB): Strengthening Neonatal Resuscitation in Sustainable Programs of Essential Newborn Care Available at: http://www.helpingbabiesbreathe.org/docs/IG_pdfs/Impl. Accessed January 30, 2016.