Abstract
Background
Temporalis muscle hypertrophy is a rare entity of masticatory muscle hypertrophy. All types of masticatory muscle hypertrophies have been documented of which temporalis muscle hypertrophy is one. Temporalis muscle hypertrophy is most commonly bilateral and usually associated with other types of masticatory muscles hypertrophy such as masseter or pterygoid hypertrophy. However, isolated unilateral temporalis muscle hypertrophy is extremely rare and only 9 cases have been reported to date in English literature since 1990 with only two patients less than 18 years. There is no exact etiology identified and the diagnosis is made by muscle biopsy combined with imaging study to exclude other possibilities. Age at presentation is ranges from 15 to 65 years with involvement of both sexes. We report the youngest child who is a seven year old girl with right side isolated unilateral temporalis muscle hypertrophy.
Case presentation
In this patient, we discuss the youngest child with isolated unilateral temporalis muscle hypertrophy and literature review to date. The patient is a seven year old female presenting with painless swelling of the right temporalis muscle. There had no features of inflammation, trauma, neoplasm or history of parafunctions such as bruxism. The child was not complaining significantly headache or visual disturbances as well. She had undergone radiological assessment with ultrasound scan and contrast MRI. The diagnosis was confirmed by muscle biopsy which shows normal muscle architecture. She was managed conservatively with regular follow up.
Conclusion
Isolated unilateral temporalis muscle hypertrophy is extremely rare in children. However this case raises the importance of considering alternative diagnoses despite the condition being rare in the pediatric population.
Electronic supplementary material
The online version of this article (10.1186/s12887-018-1061-7) contains supplementary material, which is available to authorized users.
Keywords: Isolated unilateral temporalis muscle hypertrophy, IUTMH in pediatrics, Sri Lanka
Background
Masticatory muscle hypertrophy is a rare clinical entity involving isolated or combined hypertrophy of all groups of masticatory muscles, most commonly presenting bilaterally [1–3]. Since 1880, when the first case of masticatory muscle hypertrophy was reported, there have been several other cases reported in English literature to date. In these cases, masseter and temporalis muscles were most commonly mainly involved. Temporalis muscle hypertrophy presents most commonly as isolated bilateral hypertrophy or in association with bilateral masseter hypertrophy, however, unilateral temporalis muscle hypertrophy is rare. The exact etiology has not been identified but theoretically, parafunctional movements like bruxism have been considered [4–8]. Hypertrophy of the muscle can manifest as either painful or painless enlargement with or without headaches. This condition has been reported only in nine patients in English literature (Table 1). The age was ranging from 15 years to 65 years where included five females and four males. The youngest being a 15 year old adolescent girl, reported in 1998 [6] indicating that this condition is more confined to the adult population. In this study, we report the youngest reported case in a seven year old girl with a review of the current literature of note, this is the only pediatric patient presenting less than 10 years of age according to the best of our knowledge.
Table 1.
Literature review of nine reported cases of IUTMH [17]
| Authors & year | Patient Demographics | Race | Presentation | Site | Onset in Months | Treatment | |
|---|---|---|---|---|---|---|---|
| Years | Sex | ||||||
| Wilson & Brown et al. 1990 [9] | 43 | F | Caucasian | Painless swelling | Rt | 11 | Supportive |
| Serrat et al. 1998 [6] | 15 | F | NR | Swelling, temporalis muscle contraction, limitation of mouth opening | Lt | 12 | Symptomatic |
| Isaac et al. 2000 [16] | 35 | M | Caucasian | Painless swelling | Lt | 8 | BtA |
| Lowry & Helling et al. 2003 [15] | 45 | M | African American | Swelling, recurrent headaches | Lt | 12 | Symptomatic |
| Prantl et al. 2005 [18] | 48 | F | NR | Painless swelling | Rt | 12 | Surgery |
| Prantl et al. 2005 [18] | 57 | Fa | NR | Swelling, temporalis muscle contraction, headache | Rt | NR | BtA |
| Rokadiya & Malden et al. 2006 [19] | 33 | F | Caucasian | Painful swelling, headache | Lt | 3 | Amitriptyline,splint |
| Vordenbäumen et al. 2009 [7] | 22 | F | Caucasian | Painful swelling, recurrent headaches | Rt | 6 | Acetaminophen |
| Bonnie et al. 2013 [17] | 17 | M | Caucasian | Painful swelling, recurrent headaches | Rt | 6 | BtA |
| Katsetos et al. 2014 [13] | 65 | M | NR | Painful swelling | Lt | 8 | BtA |
| Present study | 7 | F | Caucasian | Painless swelling | Rt | 2 | Symptomatic |
This table summarizes the all-previous cases of IUTMH reported in English literature up to date
Rt right, Lt Left, M Male, F Female, BtA Botulinum toxin type A administration
NR Not reported
aSame patient reported in 2005 presented 9 years later with a relapse
Case presentation
A seven year old girl presented with a lump in the right lateral forehead of two weeks duration. The mother of the patient noticed the lump while combing the child’s hair. There was no reported fever, pain, redness or tenderness over the lump indicating an inflammatory process. The patient denied any history of trauma or contact with chemicals, especially cosmetics reducing suspicion of a cutaneous hypersensitivity reaction. There was no reported visual impairment, diplopia, blurred vision, visual field defect, or opthalmoplegia to suggest ocular involvement. She strongly denied parafunction of the facial muscles like brukshism. Past medical history was non-contributory the patient reported intermittent headaches that were relieved with simple analgesics. The headache history was not compatible with migraine type or tension type headaches. The lump had not previously detected by her parents or medical practitioners. The most recent available photograph that was taken at 3 years of age revealed no evidence of hypertrophy of the right temporalis region. Physical and neurological examinations were unremarkable. The child was of average build (height 128 cm, 90th centile, weight 25 Kg, 75th centile) and healthy appearing without dysmorphism. There was marked enlargement of the right temporalis muscle, preserving the shape of the muscle, without evidence of inflammation. There was no evidence of hypertrophy of the other facial muscles on the same side or opposite side. There was no visual impairment or visual field defect. The cranial nerve examination was intact upon exam; the left side temporalis muscle was not hypertrophied. Hematological and biochemical tests were unremarkable. A complete blood count revealed a white blood cell count 9.4 × 1000 cells/mm3 (μL) (normal 4–12 × 1000 cells/mm3(μL) with 35% neutrophils and 48% lymphocytes, hemoglobin 13.2 g/dl (normal 11.5–14.5 g/dl),platelets 230 × 103/mm3(μL) (normal 150–400 × 103/mm3(μL), C-reactive protein 3 mg/L (normal 5 - 10 mg/L), clotting profile revealed Bleeding Time (BT) 2.5 min (normal 2–8 min), INR 1.06 (normal 0.8–1.2), activated Partial Thromboplastin Time (aPTT) 28.4 Seconds (normal 21.0–34.0 s). Liver function tests were within normal limits, including Alanine Aminotransferase (ALT) 20 U/L (normal 3–45 U/L) and Aspartate Aminotransferase (AST) 18 U/L (normal 15–50 U/L). Ultrasound Scan revealed uniformly enlarged right temporalis muscle. Cranial Magnetic Resonance Imaging (cMRI) revealed that the entire right temporalis muscle was hypertrophied compared to the left (right 9 mm vs. left 5.7 mm), preserving normal muscle morphology and normal signal intensity without abnormal contrast enhancement. No intracranial abnormalities or involvement of the bones were detected (Figs. 1 and 2). The diagnosis was confirmed by an incision biopsy, which demonstrated unremarkable skeletal muscle with preserved architecture. Available treatment modalities were discussed with the parents, and since the child was asymptomatic no immediate interventions were planned. She will be followed up regularly in the clinic (Additional file 1: Time line of events).
Fig. 1.
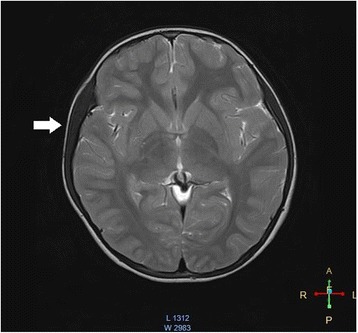
Isolated right temporalis muscle hypertrophy on an axial MRI image. T2W image of the cMRI study demonstrating enlarged right temporalis muscle on an axial section without abnormal contrast enhancement. White arrow head indicate enlarged right temporalis muscle
Fig. 2.
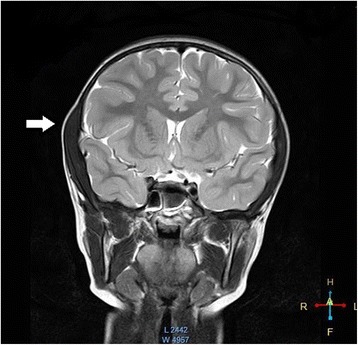
Isolated right temporalis muscle hypertrophy on a coronal MRI image. T2W image of the cMRI study demonstrating enlarged right temporalis muscle on a coronal section without abnormal contrast enhancement. White arrow head indicate enlarged right temporalis muscle
Discussion and conclusion
Masticatory muscle hypertrophy is a rare clinical entity involving isolated or combined hypertrophy of all groups of masticatory muscles. Majority are bilateral with rare cases presenting as unilateral [1–3]. Isolated unilateral temporalis muscle hypertrophy is an extremely rare condition. The first case was reported by Wilson and Brown in 1990 [9]. For the last two decades, there have been only nine cases reported in English literature (Table 1). Based on the variability of age of presentation, there does not appear to be an age predilection for the disease [10]. Masseter and temporalis muscles can be involved and they may present together or in the setting of isolated, bilateral hypertrophy [2–4, 11]. The exact etiology has not been identified for masticatory muscle hypertrophy. Theoretical explanation is secondary to parafunctional jaw movements [3]. However, the other causes such as inflammation, trauma, neoplasm, myopathy, muscular dystrophy need to be excluded [2, 12]. Out of the documented cases the youngest patient with IUTMH was a 15 year old female reported in 1998 [6]. Present study is seven year old girl with IUTMH, is the youngest child reported to date according to the best of our knowledge.
Isolated unilateral temporalis muscle hypertrophy is peculiar because there is no identifiable etiology, age category or side predominance [13, 14]. The potential etiological factors for IUTMH include local factors such as bruxism, dental malocclusion, bony prominences leading to trauma and reactive hypertrophy ascribed to psychogenic factors [13, 14]. The definitive diagnosis is confirmed via histological examination of the affected muscle [14]. However, In some cases a muscle biopsy was not performed due to various reasons and patients were treated symptomatically [7]. Regarding treatment there are several treatment modalities available for IUTMH. Some patients have not undergone any active intervention and were treated symptomatically [6, 15], while others had Botulinum toxin A (BtA) injections [16, 17], surgical interventions, [18] or depending on the severity of the symptoms treatment with analgesics [7, 19]. Even though the cost associated with BtA injection is higher there are several advantages over surgical therapy. The injections are simple and less invasive, no surgical complications like trismus, fibrosis, BtA will temporally paralyze the muscle leading to atrophy, and symptomatic improvement of associated headache [13, 16–18, 20]. In this case, our patient is under regular follow up with symptomatic treatments, including analgesics and regular visual assessments. The parents were informed about the available treatment modalities and chose symptomatic treatment over other definitive treatment modalities due to the benign nature of the condition and the lack of major cosmetic concerns.
Conclusions
IUTMH is an extremely rare condition in pediatrics and requires a high degree of suspicion as well as the exclusion of other more common etiologies of temporal swelling. This case illustrates the youngest patient with IUTMH. Initial diagnostic work up includes radiologic imaging and blood work, with the definitive diagnosis through a muscle biopsy. Based on this study and available literature, children may not need aggressive treatment, but rather require follow-up for development of further symptoms.
Additional file
Timeline of events. This data represents the time line of events carried out since diagnosis. It gives the dates and events in a chronological manner to date. (PDF 189 kb)
Acknowledgements
We are thankful to Ms. Chelsey Coles and Ms. Lauren Powell for their useful comments on manuscript.
Funding
This study had no funding source
Availability of data and materials
The dataset supporting the conclusions of this article is included within the article.
Abbreviations
- ALT
Alanine Aminotransferase
- aPTT
Activated Partial Thromboplastin Time
- AST
Aspartate Aminotransferase
- BtA
Botulinum toxin A
- cMRI
Cranial Magnetic Resonance Imaging
- CT
Clotting Time
- INR
International Normolized Ratio
- IUTMH
Isolated Unilateral Temporalis Muscle Hypertrophy
Authors’ contributions
JCR was involved in the management of patient, designing and conducting the study, data collection and writing the initial manuscript; SCW was involved in the management, designing the study, supervising data collection, and critically reviewing and revising the manuscript; GR performed and reported the radiological imaging and critically reviewed and revised the manuscript; All authors approved the final manuscript as submitted.
Authors’ information
JCR (MBBS, DCH) is a trainee MD pediatrics affiliated with the Teaching Hospital Kandy Sri Lanka. CW (MBBS,DCH,MD,FCCP) is a consultant pediatrician at the Teaching Hospital Kandy Sri Lanka. GR (MBBS, MD) is a consultant radiologist at the Teaching Hospital Kandy Sri Lanka.
Ethics approval and consent to participate
Not applicable
Consent for publication
Written informed consent was obtained from the parents of the patient for publication of this Case report and any accompanying images. A copy of the written consent is available for review by the Editor-In-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
Electronic supplementary material
The online version of this article (10.1186/s12887-018-1061-7) contains supplementary material, which is available to authorized users.
Contributor Information
Jagath C. Ranasinghe, Email: c.ranasinghe0323@gmail.com
Chandani Wickramasinghe, Email: chandaniwick@gmail.com.
Ganganath Rodrigo, Email: grodrigo237@gmail.com.
References
- 1.Legg JW. Enlargement of the temporal and masseter muscles on both sides. Trans Pathol Soc L. 1880;31:361–366. [Google Scholar]
- 2.Kessel LJ. Benign bilateral masseteric hypertrophy with temporal muscle involvement. Oral Surgery, Oral Med. Oral Pathol. [Internet]. 1970 [cited 2016 Feb 5];30:450–3. Available from: https://www.sciencedirect.com/science/article/pii/0030422070901568 [DOI] [PubMed]
- 3.Kalish GH. Hypertrophy of the Masseter or Temporalis Muscles or Both. Arch. Pediatr. Adolesc. Med. [Internet]. American Medical Association; 1971 [cited 2016 Feb 4];121:346. Available from: https://jamanetwork.com/journals/jamapediatrics/article-abstract/503983?redirect=true [DOI] [PubMed]
- 4.Da Silva K, Mandel L. Bilateral temporalis muscle hypertrophy: a case report. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. [Internet]. 2006 [cited 2015 Sep 16];102:e1–3. Available from: http://www.oooojournal.net/article/S1079-2104(06)00077-1/fulltext [DOI] [PubMed]
- 5.Kim HJ, Yum KW, Lee SS, Heo MS, Seo K. Effects of botulinum toxin type a on bilateral masseteric hypertrophy evaluated with computed tomographic measurement. Dermatologic Surg. 2003;29:484–489. doi: 10.1046/j.1524-4725.2003.29117.x. [DOI] [PubMed] [Google Scholar]
- 6.Serrat A, García-Cantera JM, Redondo LM. Isolated unilateral temporalis muscle hypertrophy. Int. J. Oral Maxillofac. Surg. [Internet]. Elsevier; 1998 [cited 2015 Sep 16];27:92–3. Available from: http://www.ijoms.com/article/S0901-5027(98)80302-0/fulltext [DOI] [PubMed]
- 7.Vordenbäumen S, Groiss SJ, Dihné M. Isolated unilateral temporal muscle hypertrophy: a rare cause of hemicranial headache. Headache [Internet]. 2009;49:779–82. Available from: 10.1111/j.1526-4610.2009.01393.x [DOI] [PubMed]
- 8.Arzul L, Corre P, Khonsari RH, Mercier JM, Piot B. Hypertrophie asym??trique des muscles masticateurs. Ann Chir Plast Esthet. 2012;57:286–291. doi: 10.1016/j.anplas.2012.02.014. [DOI] [PubMed] [Google Scholar]
- 9.Wilson PS, Brown AMS. Unilateral temporalis muscle hypertrophy: Case report. Int. J. Oral Maxillofac. Surg. [Internet]. 1990 [cited 2015 Sep 16];19:287–8. Available from: http://www.ijoms.com/article/S0901-5027(05)80422-9/pdf [DOI] [PubMed]
- 10.Graziano P, Dell’Aversana Orabona G, Astarita F, Ponzo LM, Nunziata R, Salzano G, et al. Bilateral hypertrophy of masseteric and temporalis muscles, our fifteen patients and review of literature. Eur. Rev. Med. Pharmacol. Sci. [Internet]. 2016 [cited 2016 Feb 5];20:7–11. Available from: http://www.europeanreview.org/article/10122. [PubMed]
- 11.Arzul L, Corre P, Khonsari RH, Mercier J-M, Piot B. [Asymmetric hypertrophy of the masticatory muscles]. Ann. Chir. Plast. esthétique [Internet]. 2012 [cited 2016 Feb 21];57:286–91. Available from: https://www.sciencedirect.com/science/article/pii/S0294126012000350?via%3Dihub. [DOI] [PubMed]
- 12.Straathof CSM, Doorenweerd N, Wokke BHA, Dumas EM, van den Bergen JC, van Buchem MA, et al. Temporalis muscle hypertrophy and reduced skull eccentricity in Duchenne muscular dystrophy. J. Child Neurol. [Internet]. 2014;29:1344–8. Available from: http://journals.sagepub.com/doi/abs/10.1177/0883073813518106?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub=pubmed [DOI] [PubMed]
- 13.Katsetos CD, Bianchi MA, Jaffery F, Koutzaki S, Zarella M, Slater R. Painful unilateral temporalis muscle enlargement: reactive masticatory muscle hypertrophy. Head Neck Pathol. [Internet]. 2014 [cited 2015 Sep 16];8:187–93. Available from: https://link.springer.com/article/10.1007%2Fs12105-013-0480-x [DOI] [PMC free article] [PubMed]
- 14.Harriman DG. The histochemistry of reactive masticatory muscle hypertrophy. Muscle Nerve. 1996;19:447–456. doi: 10.1002/(SICI)1097-4598(199611)19:11<1447::AID-MUS9>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- 15.Lowry TR, Helling E. Unilateral temporal muscle hypertrophy: a rare clinical entity. Ear. Nose. Throat J. [Internet]. 2003 [cited 2015 Sep 16];82:198–9. Available from: https://www.ncbi.nlm.nih.gov/pubmed/12696240. [PubMed]
- 16.Isaac AM. Unilateral Temporalis Muscle Hypertrophy Managed With Botulinum Toxin Type a. Br. J. Oral Maxillofac. Surg. [Internet]. 2000;38:571–2. Available from: http://www.bjoms.com/article/S0266-4356(00)90298-5/pdf [DOI] [PubMed]
- 17.Wang BH, Moon S-J, Wang H, Olivero WC. Isolated unilateral temporalis muscle hypertrophy. J. Neurosurg. Pediatr. [Internet]. American Association of Neurological Surgeons; 2013 [cited 2015 Sep 16];11:451–3. Available from: http://thejns.org/doi/abs/10.3171/2013.1.PEDS12534?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub=pubmed [DOI] [PubMed]
- 18.Prantl L, Heine N, Ulrich D, Eisenmann-Klein M. Recurrence of isolated unilateral temporalis muscle hypertrophy: case report. Aesthetic Plast. Surg. [Internet]. [cited 2015 Sep 16];29:574–5. Available from: https://link.springer.com/article/10.1007%2Fs00266-004-0122-5. [DOI] [PubMed]
- 19.Rokadiya S, Malden NJ. Variable presentation of temporalis hypertrophy--A case report with literature review. Br. Dent. J. [Internet]. Nature Publishing Group; 2006 [cited 2015 Sep 16];201:153–5; quiz 172. Available from: 10.1038/sj.bdj.4813850 [DOI] [PubMed]
- 20.von Lindern JJ, Niederhagen B, Appel T, Bergé S, Reich RH. Type A botulinum toxin for the treatment of hypertrophy of the masseter and temporal muscles: an alternative treatment. Plast. Reconstr. Surg. [internet]. 2001;107:327–32. Available from: https://journals.lww.com/plasreconsurg/pages/articleviewer.aspx?year=2001&issue=02000&article=00004&type=abstract. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Timeline of events. This data represents the time line of events carried out since diagnosis. It gives the dates and events in a chronological manner to date. (PDF 189 kb)
Data Availability Statement
The dataset supporting the conclusions of this article is included within the article.


