Abstract
Background
Evidence of 24-months survival in the frame of prevention of mother-to-child transmission (PMTCT) cascade-care is scare from routine programs in sub-Saharan African (SSA) settings. Specifically, data on infant outcomes according to feeding options remain largely unknown by month-24, thus limiting its breath for public-health recommendations toward eliminating new pediatric HIV-1 infections and improving care. We sought to evaluate HIV-1 vertical transmission and infant survival rates according to feeding options.
Methods
A retrospective cohort-study conducted in Yaounde from April 2008 through December 2013 among 1086 infants born to HIV-infected women and followed-up throughout the PMTCT cascade-care until 24-months. Infants with documented feeding option during their first 3 months of life (408 on Exclusive Breastfeeding [EBF], 663 Exclusive Replacement feeding [ERF], 15 mixed feeding [MF]) and known HIV-status were enrolled. HIV-1 vertical transmission, survival and feeding options were analyzed using Kaplan Meier Survival Estimate, Cox model and Schoenfeld residuals tests, at 5% statistical significance.
Results
Overall HIV-1 vertical transmission was 3.59% (39), and varied by feeding options: EBF (2.70%), ERF (3.77%), MF (20%), p = 0.002; without significance between EBF and ERF (p = 0.34). As expected, HIV-1 transmission also varied with PMTCT-interventions: 1.7% (10/566) from ART-group, 1.9% (8/411) from AZT-group, and 19.2% (21/109) from ARV-naïve group, p < 0.0001. Overall mortality was 2.58% (28), higher in HIV-infected (10.25%) vs. uninfected (2.29%) infants (p = 0.016); with a survival cumulative probability of 89.3% [79.9%–99.8%] vs. 96.4% [94.8%–97.9% respectively], p = 0.024. Mortality also varied by feeding option: ERF (2.41%), EBF (2.45%), MF (13.33%), p = 0.03; with a survival cumulative probability of 96% [94%–98%] in ERF, 96.4% [94.1%–98.8%] in EBF, and 86.67% [71.06%–100%] in MF, p = 0.04. Using Schoenfeld residuals test, only HIV status was a predictor of survival at 24 months (hazard ratio 0.23 [0.072–0.72], p = 0.01).
Conclusion
Besides using ART for PMTCT-interventions, practice of MF also drives HIV-1 vertical transmission and mortality among HIV-infected children. Thus, throughout PMTCT option B+ cascade-care, continuous counseling on safer feeding options would to further eliminating new MTCT, optimizing response to care, and improving the life expectancy of these children in high-priority countries.
Keywords: HIV-1 vertical transmission, Survival, Feeding option, Infants, Cameroon
Background
During the last decade, the medical advancement and breakthrough in preventing HIV pediatric infections have been widely implemented, with prevention of mother-to-child transmission of HIV (PMTCT) option B+ emerging as a key intervention in current routine practices [1–3]. As a result, PMTCT is gradually moving towards eliminating MTCT (e-MTCT) due to efforts in the universal access to antiretroviral (ARV) drugs for HIV-infected pregnant women, especially those living in the 22 high-priority countries [3]. However, despite the global commitment in e-MTCT targets, achieving HIV vertical transmission rates ≤5% in breastfeeding and ≤2% less in non-breastfeeding populations remains challenging in most sub-Saharan Africa (SSA) countries [4, 5]. Pragmatic strategies to achieving the goal of e-MTCT include, but not limited to, generalized coverage of HIV screening amongst pregnant women through provider initiated counseling and testing, and implementation of option B+ (lifelong triple ARV therapy [ART] to all HIV-infected pregnant women regardless of clinical or immunological eligibility) [3, 6–8].
Cameroon falls amongst the 21 SSA countries that are part of 22 global countries prioritized for this fight against new pediatric infections [3, 9, 10]. Bottlenecks encountered throughout the PMTCT-cascade contribute in sustaining high rates of HIV vertical transmission in general [5], in spite of promising findings in some specific sites [11]. Tackling such challenges in the era of PMTCT option B+ cascade-care requires resolving issues around retention in care and suboptimal feeding option(s), while addressing related programmatic issues that include the decentralization process [12], distance between households and the nearest health facility [13], community engagement and male-partner involvement into the PMTCT cascade-care components [14–16].
Within our catchment area, the Djoungolo Health District of Yaoundé (capital city of Cameroon), PMTCT programme started in the early 2008 with promising outcomes recorded in both breastfeeding and non-breastfeeding populations during the first half of infancy [11]. In spite of the national recommendations for monitoring HIV-exposed infants until completion of PMTCT-cascade-care, retention in care is concerning, with persistent risks of HIV-vertical transmission around 24 months of infant age (above 8% nationwide) [17]. Faced with scarcity of thorough perinatal cohorts capable of providing 24-month outcomes in children within the PMTCT-cascade care in Cameroon, it becomes relevant to generate local evidence that may help in formulating policies supporting the optimal efficacy or effectiveness of PMTCT programs in resource limited settings (RLS) like SSA. Of note, in the era of option B+, whereby considerations to ARV interventions and infant feeding practices had earlier been addressed for PMTCT [18], advanced understanding of the effects of infant feeding options, on both HIV MTCT and infant survival potentials, becomes essential for eventually improving on targets of eMTCT in high priority countries [3].
Study objectives
We aimed to evaluate HIV-1 vertical transmission and infant survival rates according to feeding options, in a typical RLS with generalized HIV epidemiology, for possible knowledge generalizability to PMTCT high-priority countries with similar programmatic features.
Methods
Study design and populations
We conducted a retrospective cohort-study from April 2008 through December 2013 amongst infants born to HIV-infected women, and followed-up throughout the PMTCT cascade-care until 24-months at the Djoungolo Health District in Yaoundé-Cameroon.
Study procedures
Patients and their respective data were retrieved from the Djoungolo PMTCT cohort for the period 2008-2013. Characteristics of this perinatal cohort were extensively described elsewhere [11].
Briefly, PMTCT program was launched in 2008 at the Djoungolo Health District, a setting within the catchment area of the Essos Hospital Centre (EHC), classified as the area HIV reference treatment center. Routinely, pregnant women diagnosed positive for HIV in primary healthcare centers of Djoungolo were referred to EHC for HIV-related clinical assessment, CD4 cell count measurement, infant feeding counseling (IFC) and ART initiation following standard-of-care [11]. Routine antenatal care (ANC) and delivery were done in their respective primary clinics. After delivery, mothers were advised to register their babies at the EHC for ART provision, postnatal follow-up and monitoring of PMTCT-related outcomes. Postnatal care consisted of HIV-1 early infant diagnosis (EID) at 6 weeks of age, clinical visits, continuous counseling on and follow-up of feeding practices, administration of Cotrimoxazole and late serological testing. Routine immunizations could be done at EHC or at another recognized health facility within the Djoungolo Health District. Routine appointments were planned at week 6, month 9, month 12, and between months 15-24. EID, performed using either real time PCR or qualitative PCR, was done at week 6 and further confirmed after month 12, considering 6 weeks of post weaning period (i.e. for breastfeeding populations).
During the study period, changes in PMTCT recommended ARVs used for pregnant women were taken into account. Before 2010, women having a CD4 count above 350 cells/mm3 received zidovudine (AZT) from week 28 of pregnancy till birth. As from 2010, AZT was given from week 14, while women with CD4 count below 350 cells/mm3 or clinically classified at the WHO stage 3 or 4 were eligible for lifelong triple ART.
Choice of infant feeding options
Counseling for infant feeding options was part of ANC and postnatal care. Specifically, IFC was done during each ANC visit, and HIV positive women were referred to the infant feeding counselors for in-depth counseling purposes. During IFC, the two recommended exclusive options were either exclusive breastfeeding (EBF) or exclusive replacement feeding (ERF), with emphasis to avoid mixed feeding (MF) practice.
EBF was defined as breastfeeding with no added supplements except vitamins; ERF was defined as the administration of commercial formula feeding using bottles; while MF was described as a combination of both breastfeeding and formula feeding practices. Mothers opting to practice ERF were trained on the appropriate use of feeding bottles in terms of preparation, conservation and hygiene of feeding bottles and teens.
After IFC, mothers were all capable to freely make a choice of the appropriate feeding option for their babies. Additionally, supportive counseling was done during follow-up visits. EBF mothers were advised to EBF for 6 months, followed by weaning during a short period (i.e. 1 week). After 2009, the weaning period was extended to 1 month.
Infant eligibility criteria
Infants born alive, to an HIV-infected mother, were enrolled at their first postnatal clinic attendance, specifically in the frame of EID (i.e. around week 6). The reported feeding option of mothers was recorded and those with doubtful or missing feeding information were not included. Reported feeding options were then used to classify infants as EBF, ERF or MF. During follow-up, the conclusive HIV-free result was provided upon the criteria of one negative virological + negative serological testing ≥12 months assuming 6 weeks post weaning in case of breastfeeding. A confirmed HIV infection was based on two positive PCR at any moment of the follow-up irrespective of feeding option, or a positive HIV serology after 18 months. Children with indeterminate HIV serological result were excluded from the analysis.
Statistical analysis
Primary endpoints were HIV transmission and survival rates at 24 months of infant age. Kaplan Meier survival curves were used to estimate cumulative probabilities of survival overtime according to feeding option, and log-rank test was used to compare the curves between different feeding options. Multivariate Cox proportional hazards regression was used to estimate unadjusted and adjusted hazard ratios, adjusting for HIV serological status and birth weight. Schoenfeld residuals test which was used in assessing the proportional hazard assumption [19] and Cox-Snell residual was used to determine the goodness-of-fit. All statistical tests were performed at 5% level of significance and with 95% confidence interval. Statistical analyses were done using the package survival incorporated in R software version 3.1.3.
Ethical statements
Ethical clearance for the study was obtained from the National Ethics Committee for Research on Human Subjects in Cameroon (2013/02/027/L/CNER/SP) and the Institutional Review Board of EHC (2014/003/CE-CHE). All women participating with their infants in the IFC project provided a written informed consent. Data were processed using unique identifiers for purposes of privacy and confidentiality.
Results
Characteristics of the study population
A total of 1086 eligible infants born to HIV positive mothers (median of 399 [IQR: 260-540] CD4 cells/mm3) were enrolled (Fig. 1). Regarding maternal ARV experience for PMTCT-interventions, 566 (52.12%) received triple ART, 411 (37.85%) received AZT and 109 (10.04%) had no ARV exposure. Regarding infant feeding options during the first 3 months of life, 663 (61.05%) were on ERF, 408 (37.57%) on EBF and 15 (1.38%) on MF (Table 1).
Fig. 1.

Flow chart of HIV exposed infants included in the survival analysis according to the feeding mode
Table 1.
Baseline maternal and 24-months outcomes infant characteristics according to feeding mode in the HIV exposed infants of the Essos hospital center PMTCT program
| ERF N = 658 |
EBF N = 405 |
MF N = 14 |
p-value | |
|---|---|---|---|---|
| Maternal characteristics | ||||
| Age mean (SD) | 27.00 (5.35) | 27.53 (5.18) | 27.00 (4.88) | 0.30 |
| Marital status—n(%) | 0.48 | |||
| Single | 153 (36.51) | 96 (37.80) | 6 (54.55) | |
| In relationship | 266 (63.49) | 158 (62.20) | 5 (45.45) | |
| Parity—n(%) | 0.67 | |||
| Multiparous | 278 (66.99) | 176 (70.40) | 8 (72.73) | |
| Primiparous | 137 (33.01) | 74 (29.60) | 3 (27.27) | |
| CD4 cells count--mean(SD) | 402.60 (230.72) | 472.16 (397.74) | 534.17 (107.39) | 0.003 |
| OMS Stage—n(%) | 0.37 | |||
| 1 | 486 (96.05) | 312 (94.83) | 11 (100.00) | |
| 2 | 18 (3.56) | 11 (3.34) | 0 (0.00) | |
| 3 | 2 (0.40) | 5 (1.52) | 0 (0.00) | |
| 4 | 0 (0.00) | 1 (0.30) | 0 (0.00) | |
| Occupation—n(%) | 0.75 | |||
| Student | 35 (0.051) | 22 (0.032) | 2 (0.0029) | |
| Formal sector | 140 (8.37) | 82 (8.73) | 5 (18.18) | |
| Informal sector | 183 (33.49) | 116 (32.54) | 3 (45.45) | |
| Housewife | 60 (43.78) | 32 (46.03) | 1 (27.27) | |
| Infants characteristics | ||||
| Birth weight—n(%) | 0.93 | |||
| > =2500 g | 564 (89.81) | 350 (89.74) | 13 (92.86) | |
| < 2500 g | 64 (10.19) | 40 (10.26) | 1 (7.14) | |
| Survival state—n(%) | 0.29 | |||
| Died | 11 (1.67) | 7 (1.73) | 1 (7.16) | |
| Survivors | 647 (98.33) | 398 (98.27) | 13 (92.86) | |
| HIV Status—n(%) | 0.011 | |||
| Negative | 633 (96.20) | 394 (97.28) | 11 (78.57) | |
| Positive | 25 (3.80) | 11 (2.72) | 3 (21.43) | |
HIV status and associated-factors
Overall rate of HIV-vertical transmission was 3.59% (39/1086), and all infected children were enrolled for HIV care. According to feeding options, HIV transmission varied considerably: EBF (2.72%); ERF (3.80%); MF (21.43%), p = 0.011; without any significance (p = 0.34) between EBF and ERF (Table 1). Infants experiencing MF therefore had 5.3 and 7.4 folds higher risks of HIV MTCT compared to ERF and to EBF respectively.
As expected according to exposure to ARVs, HIV-vertical transmission rates were 1.7% (10/566) from ART-group, 1.9% (8/411) from AZT-group, and 19.2% (21/109) from ARV-naïve group, p < 0.0001.
According to HIV status, mortality rate was higher among HIV-infected (10.25%) vs. uninfected (2.29%) infants (p = 0.016), thus indicating about 4 folds increment for infected children. HIV negative children survived more than the positive ones (p = 0.024); the log-rank test also shows significant differences in the Kaplan Meier cumulative probability curves (Fig. 2). Similarly, the 24-month survival cumulative probability was varied considerably: 89.3% [79.9%-99.8%] vs. 96.4% [94.8%-97.9%] in infected vs. uninfected infants respectively, p = 0.024.
Fig. 2.
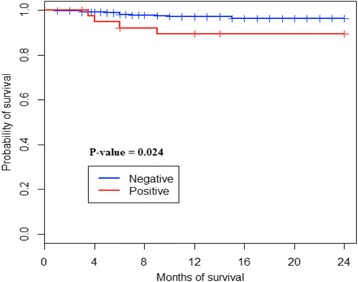
Kaplan-Meier cumulative probabilities curves of survival according to HIV status
Survival rates and associated-factors
Overall infant mortality in the study population was 2.58% (28), with varying trends according to feeding option: ERF (2.41%), EBF (2.45%), MF (13.33%), p = 0.032 (Table 2), indicating an increment of 5.4 and 5.5 folds in mortality for MF infants compared to EBF and ERF respectively. Similarly, the survival cumulative probability was 96% [94%-98%] in ERF, 96.4% [94.1%-98.8%] in EBF, and 86.67% [71.06%-100%] in MF, p = 0.04.
Table 2.
Unadjusted and adjusted Hazard Ratio (HRs) of survival at 24 months in the HIV exposed infants of the Essos hospital center PMTCT program
| Unadjusted HR | p-value | Adjusted HR | p-value | |
|---|---|---|---|---|
| Mode of feeding | ||||
| Exclusive breast feeding | 1.35 [0.52-3.49] | 0.54 | 1.16 [0.44-3.08] | 0.76 |
| Mixed feeding | 0.31 [0.04-2.42] | 0.26 | 0.44 [0.053-3.74] | 0.45 |
| Exclusive replacement feeding | Ref | Ref | Ref | Ref |
| HIV- Status | ||||
| Positive | 0.31 [0.11-0.90] | 0.032 | 0.30 [0.08-1.11] | 0.071 |
| Negative | Ref | Ref | Ref | Ref |
| Birth weight | ||||
| > =2500 g | 0.70 [0.16-2.96] | 0.63 | 0.93 [0.21-4.12] | 0.92 |
| < 2500 g | Ref | Ref | Ref | Ref |
| Global Schoenfeld residuals test | 0.23 | |||
Using the Log-rank test of survival (Fig. 3), a significant difference was observed in the Kaplan Meier curves according to feeding options (p = 0.04). Of note, the MF curve falls within the area under the curve and is distant from both the ERF and EBF curves. Specifically, the cumulative probability survival curve of MF compared those of EBF and EBF revealed p-values of 0.011 and 0.025 respectively. However, there was no significant difference of Kaplan Meier survival curves between EBF and ERF (p = 0.48). The 24-months survival cumulative probability was 96% [94%-98%] with ERF, 96.4% [94.1%-98.8%] with EBF, and 86.67% [71.06%-100%] with MF.
Fig. 3.

Kaplan-Meier cumulative probabilities curves of survival according to feeding option
Schoenfeld residuals test revealed a proportional hazard assumption with similar effects of EBF and ERF on survivals (unajusted HR 1.30 [0.59- 2.85]; adjusted HR 1.25 [0.56-2.79]). Of relevance, children in the MF arm appeared to survive less than those on ERF (unadjusted HR 0.22 [0.05-0.96]). However, after adjustment for children HIV status, the effect of MF disappeared (Adjusted HR 0.29 [0.063-1.34]), insinuating that HIV-status of children is an intermediate independent factor between infant feeding option and survival.
Discussion
In an attempt to ascertain the contributive effects of feeding options on HIV-1 vertical transmission and infant survival until 2 years of age, we demonstrated key outcomes of PMTCT programme performance after complete children follow-up throughout the PMTCT-cascade care in a high-priority country. In addition to the known impact of ARV [18, 20] within similar settings, feeding option appears as a contributive factor of infant clinical outcomes, thus paving the way for programmatic considerations [21, 22]. The present study therefore represents one of the few findings focusing on both vertical transmission and survival according to infant feeding options throughout the PMTCT-cascade care in a RLS. The findings of this study are likely to shift with the latest WHO recommendations which emphazise the practice of breastfeeding even after 12 months as recommended for the general population [21] and stresses the need not to interrupt breastfeeding in case of mixed feeding assuming maternal coverage of ARV.
The overall low rate of HIV-1 vertical transmission (3.59%) recorded in our study highlights the feasibility in achieving the national/global targets for virtual eMTCT (i.e. < 5%) [17, 18, 20], with better performance (i.e. < 2%) once PMTCT-interventions with ARV are effective [1–3]. In addition to previous knowledge, current findings underpin the significance of universal access to PMTCT option B+ [2, 6–9], with the potential of eMTCT globally [20].
Though practiced at a low rate (1.38%) in the study population, MF practice is still persistent in this RLS, indicated the need for advocacy towards continuous counseling of mothers for safe feeding options throughout the cascade of care, in order to mitigate the impact of unsafe feeding practice on PMTCT performance [21, 22]. In point of facts, beside ARV interventions, our observation places feeding option as a contributive factor for HIV vertical transmission, with potential impacts on the child overall health outcomes, including ERF in RLS [20–24].
In this urban RLS setting, higher rate of mortality was reported among HIV-positive children (compared to their negative counter parts) within the follow-up time of 24 months. This supports early pediatric ART initiation once diagnosed positive, to promote survival among infected children [25]. As the present evidence were generated in an urban setting, it is possible that mortality may be more burdened in rural settings whereby access to healthcare is more challenging in such SSA settings [26], thus suggesting wider or more representative assessments in varying geographical settings.
In the Cox model of multivariate analysis regarding feeding options and infant survival rates, MF appears as a significant contribution to poor survival events, thereby underlying the potential impact of MF on poor health outcomes of HIV-exposed infants [27, 28]. Thus, as safer feeding option, alongside ARVs, might serve as an additional weapon for both eMTCT while keeping the children alive, nutritional strategies to support maternal adherence to either ERF or EBF, using lessons of best feeding practitioners from successful PMTCT attendees, should be implemented for optimal outcomes [27–30].
Following the Schoenfeld residuals test of multivariate analysis, only HIV-infection was a predictor of infant mortality, with feeding option as a contributive factor. Thus, considering the reported strong association between feeding options and infant health outcomes (HIV MTCT and mortality events), it appears evident that MF contributes on both HIV MTCT and mortality among infants. Though the effect of MF is still being studied, this feeding option is assumed to impair the gut permeability, disturb the intestine microbiota, with exposure to many bacteria, microorganisms and antigens which may result in dysbiosis [31].
As EBF has better outcomes (though not significant) compared to ERF, the importance of EBF needs, in a context where access to potable water and other hygienic conditions are concerning, should be promoted extensively in RLS [32–36], for the overall health benefits of breast milk for the baby [36]. The practice of EBF over ERF has also been recommended by the WHO in their recent guidelines for RLS [20–22].
Overall strength of our findings relies on the association between survivals and the infant HIV status, with feeding option (i.e. MF) acting as an intermediary factor or vector of HIV transmission. Thus, considering generalizability within PMTCT high-priority countries, emphasis should be given to access to ART coupled to infant feeding counseling and support up to 2 years [21, 22]. The major strength of this study is the large sampling of our cohort coming from a SSA priority country, wherein fewer studies have reported on 2 years outcomes of HEI in routine settings. With over 70% retention in care, it would be relevant to investigate factors to improve retention also in HIV exposed uninfected infants, since they constitute a newly emerging epidemic group. Our analysis therefore demonstrates favorable outcomes at 24 months among HIV-exposed infants in both ERF and EBF arms, while those with MF showed the poorest outcomes.
A study limitation is the inability in ascertaining reasons justifying the reported cases of MF practices, which may be favoured by fear of rejection due to discrimination and stigma once HIV status is known. This stresses the role of health education, peer counselling, and male partner engagement as mitigating factors [37]. Also, lack of records for 6-months outcomes underscores the need to assess the impact of MF duration [38], as well as the infant nutritional status, on children health outcomes [39]. Furthermore, our study design did not give room for clinical follow-up, thus hindering the assessment of feeding practices at home, while missing data restricted the inclusion of some relevant factors in the survival analysis.
Conclusions
Alongside PMTCT-interventions using ARVs, the practice of MF appears as a contributive factor to HIV-1 transmission to children. Furthermore, beside the infant HIV status, the practice of MF also seems to contribute on mortality events among children. Specifically, the core role of HIV status for survival, added to the mitigating effect of feeding option, makes mandatory the infant counseling during the first 6 months of life. Therefore, in the era of option B+, continuous counseling on best feeding practices throughout the PMTCT-cascade needs to be strengthened in RLS. Such policy would help in further eliminating new MTCT while improving the life expectancy of children within PMTCT high-priority countries.
Acknowledgements
We are very appreciative to participating mother-baby pairs, for their consent throughout the study timeline, and to site staff for their cooperation during follow-up activities.
Funding
We are thankful to the French “Fondation GlaxoSmithKline (GSK)”, for the supportive grant allocated for the follow-up of this perinatal cohort.
Availability of data and materials
Data underlying these findings are provided in the manuscript tables and figures. Complete dataset could be provided upon reasonable request from the corresponding author. This dataset represents a core of the hospital database and may not be deposited in a public repository.
Abbreviations
- ANC
Antenatal care
- ART
Antiretroviral therapy
- ARV
Antiretroviral
- AZT
Zidovudine
- EBF
Exclusive breastfeeding
- EHC
Essos Hospital Centre
- eMTCT
Elimination of mother-to-child transmission of HIV
- ERF
Exclusive replacement feeding
- IFC
Infant feeding counseling
- MF
Mixed feeding
- PMTCT
Prevention of mother-to-child transmission of HIV
- RLS
Resource-limited settings
- SSA
Sub-Saharan Africa
Authors’ contributions
Designed the study and collected the data: AENN and ACNM. Analysed the data: AS. Interpreted the data: AENN and JF. Initiated the manuscript: AENN. Revised the manuscript: JF, ACNM, AS. All authors read and approved the final version of the manuscript.
Ethics approval and consent to participate
Ethical clearance for the study was obtained from the National Ethics Committee for Research on Human Subjects in Cameroon (2013/02/027/L/CNER/SP) and the Institutional Review Board of EHC (2014/003/CE-CHE). All women participating with their infants in this feeding counseling project provided a written informed consent. Data were processed using unique identifiers for purpose of privacy and confidentiality.
Consent for publication
N/A
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Anne Esther Njom Nlend, Phone: 237 677 70 40 06, Phone: 679 53 95 92, Email: anne.njom@gmail.com.
Annie Carole Nga Motaze, Email: anica123@yahoo.fr.
Arsene Sandie, Email: arsenesandie@gmail.com.
Joseph Fokam, Email: josephfokam@gmail.com.
References
- 1.World Health Organization . Antiretroviral drugs for treating pregnant women and preventing HIV infection in infants. Recommendations for a public health approach. Geneva: World Health Organization; 2010. [PubMed] [Google Scholar]
- 2.Chi BH, Stringer JS, Moodley D. Antiretroviral drug regimens to prevent mother-to-child transmission of HIV: a review of scientific, program, and policy advances for sub-Saharan Africa. Curr HIV/AIDS Rep. 2013;10(2):124–133. doi: 10.1007/s11904-013-0154-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Govender T, Coovadia H. Eliminating mother to child transmission of HIV-1 and keeping mothers alive: recent progress. J Inf Secur. 2014;68(Suppl 1):S57–S62. doi: 10.1016/j.jinf.2013.09.015. [DOI] [PubMed] [Google Scholar]
- 4.Luzuriaga K, Mofenson LM. Challenges in the elimination of pediatric HIV-1 infection. N Engl J Med. 2016;374(8):761–770. doi: 10.1056/NEJMra1505256. [DOI] [PubMed] [Google Scholar]
- 5.Gourlay A, Birdthistle I, Mburu G, Iorpenda K, Wringe A. Barriers and facilitating factors to the uptake of antiretroviral drugs for prevention of mother-to-child transmission of HIV in sub-Saharan Africa: a systematic review. J Int AIDS Soc. 2013;16:18588. doi: 10.7448/IAS.16.1.18588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.van Lettow M, Bedell R, Mayuni I, Mateyu G, Landes M, Chan AK, et al. Towards elimination of mother-to-child transmission of HIV: performance of different models of care for initiating lifelong antiretroviral therapy for pregnant women in Malawi (option B+) J Int AIDS Soc. 2014;17:18994. doi: 10.7448/IAS.17.1.18994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ahmed S, Kim MH, Abrams EJ. Risks and benefits of lifelong antiretroviral treatment for pregnant and breastfeeding women: a review of the evidence for the option B+ approach. Curr Opin HIV AIDS. 2013;8(5):474–489. doi: 10.1097/COH.0b013e328363a8f2. [DOI] [PubMed] [Google Scholar]
- 8.Coutsoudis A, Goga A, Desmond C, Barron P, Black V, Coovadia H. Is Option B+ the best choice? South Afr J HIV Med. 2013; 14(1):8–10
- 9.UNAIDS . Ambitious treatment targets: writing the final chapter of the AIDS epidemic. Reference discussion paper. Geneva: UNAIDS; 2013. [Google Scholar]
- 10.World Health Organization. HIV/AIDS: Global update on the health sector response to HIV, 2014. World Health Organization; 2014. ISBN: 978 92 4 150758 5. http://www.who.int/hiv/pub/progressreports/update2014/en/. Accessed 13 Oct 2016.
- 11.Nlend AEN, Ekobo CS, Bitoungui M, Ekani BB, Tchokoteu P, Lyeb S, et al. Early outcomes of HIV exposed children in the first district-wide programme using extended regimens for the prevention of mother-to-child transmission of HIV, in Yaounde, Cameroon. J Trop Pediatr. 2012;58(4):297–302. doi: 10.1093/tropej/fmr100. [DOI] [PubMed] [Google Scholar]
- 12.Edmonds A, Feinstein L, Okitolonda V, Thompson D, Kawende B, Behets F. Decentralization does not assure optimal delivery of PMTCT and HIV-exposed infant services in a low prevalence setting. J Acquir Immune Defic Syndr. 2015;70(4):e130–e139. doi: 10.1097/QAI.0000000000000781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Escamilla V, Chibwesha CJ, Gartland M, Chintu N, Mubiana-Mbewe M, Musokotwane K, et al. Distance from household to clinic and its association with the uptake of prevention of mother-to-child HIV transmission regimens in rural Zambia. J Acquir Immune Defic Syndr. 2015;70(3):e94–e101. doi: 10.1097/QAI.0000000000000739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Awungafac G, Njukeng PA, Ndasi JA, Mbuagbaw LT. Prevention of mother-to-child transmission of the human immunodeficiency virus: investigating the uptake and utilization of maternal and child health services in Tiko health district, Cameroon. Pan Afr Med J. 2015;20:20. doi: 10.11604/pamj.2015.20.20.5137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Osoti AO, John-Stewart G, Kiarie JN, Barbra R, Kinuthia J, Krakowiak D, Farquhar C. Home-based HIV testing for men preferred over clinic-based testing by pregnant women and their male partners, a nested cross-sectional study. BMC Infect Dis. 2015;15:298. doi: 10.1186/s12879-015-1053-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tilahun M, Mohamed S. Male partners’ involvement in the prevention of mother-to-child transmission of HIV and associated factors in Arba Minch town and Arba Minch Zuria Woreda, Southern Ethiopia. Biomed Res Int. 2015;2015:763876. doi: 10.1155/2015/763876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Republic of Cameroon, Ministry of Public Health, National AIDS Control Committee. Rapport annuel 2014 des activites de lute contre le VIH/SIDA et les IST au Cameroun. Yaounde: National AIDS Control Committee; 2015. www.cnls.cm/docs/Rapport_Annuel_CNLS_2014.pdf. Accessed 13 Oct 2016.
- 18.Saounde Temgoua EM, Nkenfou CN, Zoung-Kanyi Bissek AC, Fokam J, Billong SC, Sosso SM, et al. HIV-1 early infant diagnosis is an effective indicator of the prevention of mother-to-child transmission program performance: experience from Cameroon. Curr HIV Res. 2015;13(4):286–291. doi: 10.2174/1570162X13666150407143525. [DOI] [PubMed] [Google Scholar]
- 19.Schoenfeld D. The asymptotic properties of nonparametric tests for comparing survival distributions. Biometrika. 1981;68:316–319. doi: 10.1093/biomet/68.1.316. [DOI] [Google Scholar]
- 20.World Health Organization . Global plan towards the elimination of new HIV infections among children by 2015 and keeping their mothers alive 2011–2015. Geneva: UNAIDS; 2011. [Google Scholar]
- 21.The Academy of Nutrition and Dietetics . Systematic review of effectiveness of interventions to promote exclusive breastfeeding in women that are HIV (+) on anti-retroviral therapy living in areas that promote exclusive breastfeeding due to limited resources for safe replacement feeding. Geneva: World Health Organization; 2016. [Google Scholar]
- 22.World health organization . Guideline updates on HIV and infant feeding; the duration of breastfeeding and support from health services to improve feeding practices among mothers living with HIV. Geneva: World Health Organization; 2016. [PubMed] [Google Scholar]
- 23.Rollins NC, Becquet R, Bland RM, Coutsoudis A, Coovadia HM, Newell ML. Infant feeding, HIV transmission and mortality at 18 months: the need for appropriate choices by mothers and prioritization within programmes. AIDS. 2008;22(17):2349–2357. doi: 10.1097/QAD.0b013e328312c740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Leroy V, Sakarovitch C, Viho I, Becquet R, Ekouevi DK, Bequet L, et al. Acceptability of formula-feeding to prevent HIV postnatal transmission, Abidjan, cote d'Ivoire: ANRS 1201/1202 Ditrame plus study. J Acquir Immune Defic Syndr. 2007;44(1):77–86. doi: 10.1097/01.qai.0000243115.37035.97. [DOI] [PubMed] [Google Scholar]
- 25.Townsend CL, Byrne L, Cortina-Borja M, Thorne C, de Ruiter A, Lyall H, et al. Earlier initiation of ART and further decline in mother-to-child HIV transmission rates, 2000–2011. AIDS. 2014;28(7):1049–1057. doi: 10.1097/QAD.0000000000000212. [DOI] [PubMed] [Google Scholar]
- 26.Newell ML, Coovadia H, Cortina-Borja M, Rollins N, Gaillard P, Dabis F. Mortality of infected and uninfected infants born to HIV-infected mothers in Africa: a pooled analysis. Lancet. 2004;364(9441):1236–1243. doi: 10.1016/S0140-6736(04)17140-7. [DOI] [PubMed] [Google Scholar]
- 27.Shapiro RL, Kitch D, Ogwu A, Hughes MD, Lockman S, Powis K, et al. HIV transmission and 24-month survival in a randomized trial of HAART to prevent MTCT during pregnancy and breastfeeding in Botswana (the Mma Bana study) AIDS. 2013;27(12):1911. doi: 10.1097/QAD.0b013e32836158b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Becquet R, Bequet L, Ekouevi DK, Viho I, Sakarovitch C, Fassinou P, et al. Two-year morbidity–mortality and alternatives to prolonged breast-feeding among children born to HIV-infected mothers in Côte d'Ivoire. PLoS Med. 2007;4(1):e17. doi: 10.1371/journal.pmed.0040017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ciaranello AL, Leroy V, Rusibamayila A, Freedberg KA, Shapiro R, Engelsmann B, et al. Individualizing the WHO HIV and infant feeding guidelines: optimal breastfeeding duration to maximize infant HIV-free survival. AIDS. 2014;28(Suppl 3):S287–S299. doi: 10.1097/QAD.0000000000000337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.White AB, Mirjahangir JF, Horvath H, Anglemyer A, Read JS. Antiretroviral interventions for preventing breast milk transmission of HIV. Cochrane Database Syst Rev. 2014;10:CD011323. doi: 10.1002/14651858.CD011323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.O'Sullivan A, Farver M, Smilowitz JT. The influence of early infant-feeding practices on the intestinal microbiome and body composition in infants. Nutr Metab Insights. 2015;8(Suppl 1):1–9. doi: 10.4137/NMI.S29530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ngoma MS, Misir A, Mutale W, Rampakakis E, Sampalis JS, Elong A, et al. Efficacy of WHO recommendation for continued breastfeeding and maternal cART for prevention of perinatal and postnatal HIV transmission in Zambia. J Int AIDS Soc. 2015;18:19352. doi: 10.7448/IAS.18.1.19352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Anígilájé EA, Dabit OJ, Olutola A, Ageda B, Aderibigbe SA. HIV-free survival according to the early infant-feeding practices; a retrospective study in an anti-retroviral therapy programme in Makurdi, Nigeria. BMC Infect Dis. 2015;15:132. doi: 10.1186/s12879-015-0871-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chikhungu LC, Bispo S, Rollins N, Siegfried N, Newell ML. HIV-free survival at 12–24 months in breastfed infants of HIV-infected women on antiretroviral treatment. Tropical Med Int Health. 2016;21(7):820–828. doi: 10.1111/tmi.12710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cournil A, Van de Perre P, Cames C, de Vincenzi I, Read JS, Luchters S, et al. Early infant feeding patterns and HIV-free survival: findings from the Kesho-bora trial (Burkina Faso, Kenya, South Africa) Pediatr Infect Dis J. 2015;34(2):168–174. doi: 10.1097/INF.0000000000000512. [DOI] [PubMed] [Google Scholar]
- 36.Victora CG, Bahl R, Barros AJ, França GV, Horton S, Krasevec J, et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. 2016;387(10017):475–490. doi: 10.1016/S0140-6736(15)01024-7. [DOI] [PubMed] [Google Scholar]
- 37.Odeny BM, Pfeiffer J, Farquhar C, Igonya EK, Gatuguta A, Kagwaini F, Nduati R, Kiarie J, Bosire R. The stigma of exclusive breastfeeding among both HIV-positive and HIV-negative women in Nairobi, Kenya. Breastfeed Med. 2016;11:252–258. doi: 10.1089/bfm.2016.0014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kuhn L, Aldrovandi GM, Sinkala M, Kankasa C, Semrau K, Mwiya M, et al. Effects of early, abrupt weaning on HIV-free survival of children in Zambia. N Engl J Med. 2008;359(2):130–141. doi: 10.1056/NEJMoa073788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sint TT, Lovich R, Hammond W, Kim M, Melillo S, Lu L, et al. Challenges in infant and young child nutrition in the context of HIV the child survival working group of the interagency task team on the prevention and treatment of HIV infection in pregnant women, mothers and children. AIDS. 2013;27(Suppl 2):S169–S177. doi: 10.1097/QAD.0000000000000089. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data underlying these findings are provided in the manuscript tables and figures. Complete dataset could be provided upon reasonable request from the corresponding author. This dataset represents a core of the hospital database and may not be deposited in a public repository.


